MCQ Gynecological Cancer
Diunggah oleh
limaihwa1990Deskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
MCQ Gynecological Cancer
Diunggah oleh
limaihwa1990Hak Cipta:
Format Tersedia
Best Practice & Research Clinical Obstetrics and Gynaecology 26 (2012) A1A6
Contents lists available at SciVerse ScienceDirect
Best Practice & Research Clinical Obstetrics and Gynaecology
journal homepage: www.elsevier.com/locate/bpobgyn
Fertility Preservation in Gynaecological Cancer Multiple Choice Questions for Vol. 26, No. 3
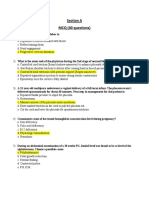
1. In the management of a woman of reproductive age with a diagnosis of epithelial ovarian cancer, balancing concerns of improving cancer outcomes and preserving the patients reproductive potential, prime ethical considerations underpinning the counselling and management would include: a) Autonomy. b) Benecence. c) Non-malecence. d) Justice. e) Truthfulness. 2. A 30-year old nulligravida has been referred to you with a 12-cm solid and cystic mass discovered on physical examination and conrmed by transvaginal ultrasound. She has a CA125 level of 350 IU/ml (normal less than 35 IU/ml). She and her husband are keen on starting a family soon and the couple is keen on fertility preservation. You describe the surgical objectives of fertility preserving surgery for epithelial ovarian cancer most appropriately as: a) Removal of all visible tumour. b) Retaining ovarian tissue and the uterus. c) Retaining only the uterus while ensuring that the staging procedure is minimally invasive. d) Accurately determining the extent of disease. e) Ensuring the removal of retroperitoneal nodes to improve outcomes. 3. During an exploratory laparotomy for a 29-year-old nulligravida with a solid-cystic adnexal mass who is keen on fertility preservation, gross disease seems to be conned only to the right ovary that has been removed intact for a frozen section diagnosis, which is reported as having features of a clear-cell carcinoma. The remainder of the intraperitoneal survey is grossly within normal limits. The most appropriate next steps might be to: a) Complete a total hysterectomy and a salpingo-oopherectomy of the remaining ovary and tube. b) Obtain a wedge biopsy of the remaining ovary. c) Carry out peritoneal biopsies. d) Carry out an omentectomy. e) A salpingo-oopherectomy of the remaining ovary. 4. A 28-year old woman with a diagnosis of FIGO stage IC grade 3 endometrioid adenocarcinoma of the ovary is pregnant at 9 weeks amenorrhea. She completed six cycles of adjuvant carboplatin and paclitaxel 9 months ago. Although she is t and has no functional complaints and in good general health, she is concerned about the possibility of congenital anomalies resulting from chemotherapy. The most appropriate next step in management is: a) Arrange for chorionic villus sampling to be carried out as soon as possible.
1521-6934/$ see front matter doi:10.1016/j.bpobgyn.2012.03.001
A2
Appendix / Best Practice & Research Clinical Obstetrics and Gynaecology 26 (2012) A1A6
b) c) d) e)
Arrange for amniocentesis at around 20 weeks gestation. Counsel the woman about the low likelihood of congenital anomalies. Arrange for this pregnancy to be terminated as soon as possible. Make an appointment for the woman with a genetics counsellor.
5. A 19-year-old woman presents to the emergency department with lower abdominal pain and increasing swelling that she has had for 4 days. Clinically, there is an irregular pelvi-abdominal mass about 15 cm in size. Her last menstrual period was 2 weeks ago. Transabdominal ultrasound scan shows features suggestive of ovarian neoplasm. Which of the following is/are true regarding this mass? a) This is most likely an ovarian germ-cell tumour. b) Most ovarian germ-cell tumours are benign. c) Her preoperative serum carcinoembryonic antigen and Ca19-9 levels should be assessed. d) Normal tumour marker levels do not preclude a malignant ovarian germ-cell tumour (MOGCT). e) Most immature teratomas are tumour marker negative. 6. The same woman described in the preceding question now undergoes a laparotomy for her pelvic mass. Her pre-operative tumour markers were all in the normal range. Intra-operatively there is a right ovarian solid-cystic mass 9-cm diameter with smooth intact capsule and 6-cm left ovarian solid-cystic mass also with a smooth intact capsule. The tubes and uterus are normal and the intraperitoneal survey is normal. Which of the following is/are true regarding her management? a) Ovarian dysgerminomas are usually bilateral. b) A contralateral dermoid cyst may be found in MOGCT. c) Bilateral oophorectomy and lymphadenectomy should be carried out. d) Bilateral ovarian cystectomy should be carried out initially. e) Chemotherapy may be required if the histology is malignant. 7. The same woman described above underwent a fertility-preserving surgery and complete surgical staging. Her histopathology report conrms a 9-cm diameter International Federation of Gynecology and Obstetrics stage 1A immature teratoma grade 3 in the right ovary and a 6-cm mature cystic teratoma in the left ovary. She was treated with three cycles of adjuvant bleomycin, etoposide and cisplatin chemotherapy. a) Chemotherapy effect on ovarian function includes decrease in serum gonadotrophins. b) Histologic changes in the ovaries of women receiving chemotherapy include a reduction in the number of follicles. c) She may become amenorrheic during chemotherapy. d) She has a 10% chance of infertility after chemotherapy. e) She will require fetal karyotyping in her rst pregnancy after chemotherapy. 8. Which of the following statement(s) about hydatidiform mole is/are true: a) Oxytocin is contra-indicated in uterine evacuation. b) Medical abortion should never be carried out because of the risk of tumour embolisation. c) Termination of pregnancy is not needed if the woman conceives within 6 months during the follow-up period. d) The risk of developing molar pregnancy in subsequent pregnancies is about 0.62%. e) Assisted reproductive techniques can increase the risk of gestational trophoblastic neoplasia (GTN). 9. Which of the following statements regarding GTN is true: a) Women who have a plateau of human chorionic gonadotropin (hCG) with at least four persistently elevated hCG values (day 1, 7, 14 and 21) after any pregnancy can be diagnosed as having GTN. b) Repeated uterine evacuation should be routinely carried out when the hCG is less than 1500 IU/ l to prevent the need for subsequent chemotherapy.
Appendix / Best Practice & Research Clinical Obstetrics and Gynaecology 26 (2012) A1A6
A3
c) Hysterectomy can be considered for women who do not desire to have children because it can reduce the risk of local invasion and distant metastasis. d) Women who conceive within 6 months after completing chemotherapy have a higher risk of abnormal pregnancies. e) Women may have earlier menopause after chemotherapy. 10. Which of the following statement(s) about choriocarcinoma, placental-site trophoblastic tumour and epithelioid trophoblastic tumour is/are true: a) Women with choriocarcinoma have worse pregnancy outcomes than the general population. b) There is proven value of fertility sparing treatment in placental-site trophoblastic tumour. c) The standard treatment for epithelioid trophoblastic tumour is hysterectomy. d) Women who conceive after being treated for choriocarcinoma have a higher risk of congenital abnormalities. e) Uterine embolisation can be considered in cases of heavy bleeding if the woman wishes to retain the uterus for future pregnancy. 11. A 28-year-old, nulliparous woman is diagnosed as having stage IB1 (2 cm) cervical cancer. She is 8 weeks pregnant at the time of diagnosis. She would like to keep her pregnancy if possible, but very keen to keep her fertility intact. The following are options of management: a) She should be advised to terminate the pregnancy. b) She should have a radical hysterectomy and pelvic lymph-node dissection, as it is the best treatment for her. c) She should have a radical trachelectomy and pelvic-node dissection after terminating her pregnancy. d) She should be advised to complete her family as soon as possible. e) Most authorities do not recommend waiting for more than 48 weeks before denitive treatment. 12. A 32-year old, gravida 2, para 1, at 10 weeks of amenorrhea, presents for routine antenatal check up. Clinical examination and pelvic ultrasound shows a viable intrauterine pregnancy corresponding to 10 weeks gestation and an incidental nding of a right ovarian cyst of about 8 cm with a complex appearance. The mass appears solid-cystic and no free uid is seen. a) She should have a computed tomography scan of the abdomen and pelvis to assess for metastatic disease. b) She should have blood taken to analyse for tumour markers (i.e. alpha fetoprotein, beta human chorionic gonadotropin and calcium 125). c) She should be advised to have an exploratory laparotomy at about 1214 weeks. d) The laparotomy should be done through a midline incision and a thorough assessment of the peritoneal cavity should be followed by unilateral salpingo-oophorectomy and the specimen sent for frozen section. e) If the frozen section showed a well-differentiated, mucinous adenocarcinoma, the surgeon should proceed with total hysterectomy, removal of the opposite ovary and omentectomy. 13. Which of the following statement(s) about gonadotoxicity of chemotherapeutic agents is/are true? a) It is highest for cyclophosphamide and lowest for vinblastin. b) It is highest for vinblastin and lowest for cyclophosphamide. c) It is highest for cyclophosphamide and lowest for vinblastin before the age of 30 years. d) It is highest for cyclophosphamide and lowest for vinblastin after the age of 30 years. e) For every gonadotoxic agent there is a direct age association. 14. Which of the following is/are true regarding the suggested methods for fertility preservation despite chemotherapy in young women? a) In-vitro fertilisation (IVF) and cryopreservation is applicable to every woman regardless of age.
A4
Appendix / Best Practice & Research Clinical Obstetrics and Gynaecology 26 (2012) A1A6
b) Cryopreservation of ovarian tissue is safe but the possible existence of malignant cells in the ovaries of women with leukaemia, Hodgkins lymphoma, and Ewings sarcoma have been reported. c) Gonadotropin-releasing hormones (GnRH)-agonists have been shown to interfere with the efciency of chemotherapy in hormone-receptor-positive breast carcinoma. d) It is not possible to combine IVF with cryopreservation of embryos (or ova); ovarian tissue cryopreservation; or GnRH-a administration for women before administration of gonadotoxic chemotherapy. e) IVF should be combined with cryopreservation of ova, ovarian tissue cryopreservation, and GnRH-a administration for prepubertal girls before administration of gonadotoxic chemotherapy. 15. Which of the following statements about methods for fertility preservation despite chemotherapy in young women is/are true? a) Cryopreservation of ovarian tissue and transplantation has generated by now at least 18 healthy neonates. b) Cryopreservation of ovarian tissue and transplantation has generated by now at least 100 healthy neonates. c) The administration of GnRH-a before and during gonadotoxic chemotherapy has been shown to be effective in preserving cyclic menstruation in survivors both in prospective randomisedcontrolled trials, case-control studies, and in several meta-analyses. d) IVF and cryopreservation of embryos is a clinically approved, unequivocally accepted, noninvestigational method for fertility preservation. e) GnRH-a co-treatment may be effective in cases of gonadotoxic chemotherapy but not in cases of radiotherapy. 16. Which statement about the gonadotoxicity of various chemotherapy regimens is/are correct? a) In Hodgkins lymphoma, the gonadotoxicity decreases in the following order: escalated BEACOPP, BEACOPP, ABVD. b) In Hodgkins lymphoma, the gonadotoxicity decreases in the following order: ABVD, MOPP ABVD, escalated BEACOPP, BEACOPP. c) In Hodgkins lymphoma, the gonadotoxicity decreases in the following order: BEACOPP, MOPP ABVD, ABVD, escalated BEACOPP. d) In Hodgkins lymphoma, the gonadotoxicity decreases in the following order: MOPPABVD, escalated BEACOPP, ABVD, BEACOPP. e) In Hodgkins lymphoma, the gonadotoxicity is very high and similar for all the above protocols after the age of 35 years and negligible before the age of 25 years. 17. A 29-year-old woman is being planned for adjuvant chemotherapy to treat breast cancer. The following is/are true regarding fertility preservation method(s): a) She may be offered cryopreservation of embryos. b) Cryopreservation of embryos is the most established option for preserving fertility. c) She may be offered cryopreservation of oocytes. d) Cryopreservation of oocytes requires gonadotropin stimulation. e) She may be offered cryopreservation of cortical ovarian tissue. 18. The following statement(s) is/are true about ovarian tissue cryopreservation for fertility preservation: a) This method should only be offered to pre-pubertal girls. b) This method may be offered to pre-pubertal girls and adolescents. c) This method may be offered to adult women of young reproductive age. d) This method can also be recommended to women of advanced reproductive age older than 40 years. e) If the procedure could not be performed before chemotherapy, it should not be offered afterwards.
Appendix / Best Practice & Research Clinical Obstetrics and Gynaecology 26 (2012) A1A6
A5
19. The following statement(s) is/are true about ovarian tissue transplantation: a) Auto-transplantation of the ovarian tissue to regain fertility is suitable in all women who have preserved ovarian tissue for malignant diseases. b) Auto-transplantation of the ovarian tissue to regain fertility is suitable in women who have preserved ovarian tissue for benign diseases. c) Auto-transplantation of the ovarian tissue to regain fertility in women who have had a malignant disease is only suitable if the absence of malignant cells in the tissue is conrmed. d) Auto-transplantation of the ovarian tissue to regain fertility is suitable for women who have preserved ovarian tissue for leukaemia. e) Ovarian tissue transplantation should be carried out under institutional review board research protocols. 20. The following statement(s) is/are true about radical trachelectomy: a) A 30-year old woman with a squamous cervical cancer of 32 mm visible on MRI and no lymphovascular space involvement is a good candidate for radical trachelectomy if she desires childbearing. b) A trachelectomy procedure must be abandoned when positive pelvic lymph nodes are found. c) Radical trachelectomy has fewer postoperative complications than radical hysterectomy. d) The most frequent complication of the procedure is ureteral leak. e) In the abdominal approach the uterine artery is divided, and in the vaginal approach only the cervico-vaginal branch is divided. 21. Which of the following statement(s) is/are true about obstetrical outcomes in women undergoing radical trachelectomy? a) Subfertility after radical trachelectomy is similar to the general population. b) One of the main obstetrical problems after radical trachelectomy is preterm delivery. c) Severe prematurity occurs in over 10%. d) Women have to wait at least 1 year after surgery before attempting pregnancy. e) Obstetric visits have to be scheduled as for the rest of the population. 22. Which of the following about ovarian transposition and endometrial cancer is/are true? a) The rate of ovarian function preservation after pelvic radiation followed by brachytherapy after ovarian transposition is evaluated around 90%. b) During ovarian transposition, the quality of peritoneal dissection is essential to prevent a possible kinking of ovarian vessels. c) In cases of grade 1, stage 1A endometrial carcinoma, the general rate of occult ovarian tumour is around 10%. d) Macroscopic evaluation of normal ovaries correlates well with the absence of metastases. e) One per cent of endometrial carcinomas, diagnosed before the age of 50 years, are associated with Lynch syndrome. 23. Premenopausal well-differentiated endometrial cancer in a 40-year old woman wishing to retain fertility can be managed by: a) Endometrial resection. b) An intra-uterine progesterone coated device. c) Oral progestagens for 3 months. d) Metformin. e) Weight loss. 24. A woman aged 35 years, with one previous child by normal delivery, is diagnosed with a squamous cell cervical cancer 2-cm in diameter. The tumour is diagnosed by a deep punch biopsy and a magnetic resonance imaging (MRI) scan, and is found to be conned to the lower endo-cervical canal. It is staged as IBI, with no lymphadenopathy. Which of the following statements is/are true? a) Radical hysterectomy and pelvic lymph-node dissection is mandatory.
A6
Appendix / Best Practice & Research Clinical Obstetrics and Gynaecology 26 (2012) A1A6
b) Trachelectomy is contra-indicated as the woman is a primipara over 35 years. c) Trachelectomy may be considered, provided that complete removal of the cervix up to and including the internal orice at the isthmus is carried out. d) Trachelectomy needs to ensure a clear margin of at least 1 cm. e) The woman should be counselled that radical hysterectomy or chemo-radiotherapy offers her the best chance of cure still with a 1015% chance of recurrence. 25. A nulliparous woman, aged 29 years, undergoes radical vaginal trachelectomy for a stage 1BI cervical cancer with no adverse prognostic factors in the nal pathology. The margins of resection are clear by a good centimetre. The tumour is well differentiated with no lympho-vasculature space invasion and negative pelvic nodes. Which of the following statement(s) is/are true regarding future care? a) She may conceive as soon as she wishes. b) She needs no follow up cytology as there is no cervix remaining. c) She needs to be discharged to the care of a General Practitioner. d) She should have regular smears 6 monthly, then yearly for at least 10 years. e) Endometrial cells on smears can make interpretation difcult. 26. After radical vaginal trachelectomy, a woman conceives spontaneously for the rst time and reaches the second trimester with no apparent problems. Which of the following is/are true? a) She can have shared antenatal care with her General Practitioner. b) She is at increased risk of premature rupture of the membranes. c) She should have the cerclage removed to allow labour to ensue at 38 weeks. d) She may be expected to labour spontaneously near term and deliver vaginally. e) She should have a planned classical caesarean section if and when she labours. 27. The following is/are true about cervical cancer: a) It is decreasing in incidence worldwide as the natural history is better and more clearly understood. b) It is decreasing in mortality worldwide. c) Adenocarcinoma is increasing in countries with a screening programme. d) Cervical cancer can occur in monogamous relationships. e) Cervical cancer is so rare in women under 25 years that screening is not necessary before this age. 28. The correct proportion of borderline tumours affecting women of reproductive age is? a) 20%. b) 25%. c) 33%. d) 50%. e) 65%. 29. Which adjuvant chemotherapy drugs have been shown to be benecial in advanced-stage borderline disease? a) Cisplatin. b) Carboplatin. c) Paclitaxel. d) Paclitaxel plus carboplatin. e) No proven benet from any adjuvant therapy. 30. Which mutation(s) are associated with low-grade serous ovarian carcinoma? a) BRAF and KRAS. b) TP53. c) HLA-G expression. d) BRCA1 and BRCA2. e) CA125.
Anda mungkin juga menyukai
- Patient's Medical Chart SummaryDokumen32 halamanPatient's Medical Chart SummaryAira Gene MenesesBelum ada peringkat
- Novartis Glivec Case StudyDokumen7 halamanNovartis Glivec Case StudyGarima ParakhBelum ada peringkat
- OB-GYN - MCQ - 2012 - 5th-Year - Mu - TahDokumen16 halamanOB-GYN - MCQ - 2012 - 5th-Year - Mu - TahHalah100% (1)
- Gyn 9 - All Gynecology 5 2021Dokumen22 halamanGyn 9 - All Gynecology 5 2021Menna Kamal100% (2)
- Obstetrics MCQDokumen8 halamanObstetrics MCQSandip Patil100% (6)
- Blueprints Obstetrics and Gynecology 5th Edition MCQDokumen30 halamanBlueprints Obstetrics and Gynecology 5th Edition MCQsinglez100% (1)
- Gynecology & Obstetrics MCQ Revision GuideDokumen49 halamanGynecology & Obstetrics MCQ Revision Guidedeepak12290% (41)
- Dewhurst's Textbook of Obstetrics & GynaecologyDari EverandDewhurst's Textbook of Obstetrics & GynaecologyChristoph LeesPenilaian: 2 dari 5 bintang2/5 (1)
- The Unofficial Guide to Obstetrics and Gynaecology: Core O&G Curriculum Covered: 300 Multiple Choice Questions with Detailed Explanations and Key Subject SummariesDari EverandThe Unofficial Guide to Obstetrics and Gynaecology: Core O&G Curriculum Covered: 300 Multiple Choice Questions with Detailed Explanations and Key Subject SummariesPenilaian: 1.5 dari 5 bintang1.5/5 (3)
- OBS and Gynaecology MCQ ReviewDokumen11 halamanOBS and Gynaecology MCQ ReviewnoblefxBelum ada peringkat
- 01.williams Obstetrics - Combined QuestionsDokumen23 halaman01.williams Obstetrics - Combined QuestionschristinejoanBelum ada peringkat
- Board Exams Ob Gyn 2009Dokumen12 halamanBoard Exams Ob Gyn 2009filchibuff50% (2)
- Gyn MCQs PRIMEsDokumen40 halamanGyn MCQs PRIMEssk100% (2)
- MCQ On MenopauseDokumen4 halamanMCQ On Menopausesalamred100% (3)
- Multiple Choice Questions in Paediatric SurgeryDari EverandMultiple Choice Questions in Paediatric SurgeryPenilaian: 1 dari 5 bintang1/5 (1)
- Comprehensive Handbook Obstetrics & Gynecology 3rd EdDari EverandComprehensive Handbook Obstetrics & Gynecology 3rd EdPenilaian: 5 dari 5 bintang5/5 (1)
- Gynecology & Obstetrics MCQDokumen49 halamanGynecology & Obstetrics MCQOmar AhmedBelum ada peringkat
- Obs and Gyne Final All PDFDokumen268 halamanObs and Gyne Final All PDFملك عيسى100% (2)
- Revision in Obstetrics&Gynecology Revision in Obstetrics&GynecologyDokumen136 halamanRevision in Obstetrics&Gynecology Revision in Obstetrics&GynecologySiam Weng Loong100% (4)
- MCQ - On Obstetrics and Gynaecology PART 2Dokumen78 halamanMCQ - On Obstetrics and Gynaecology PART 2Kripa Susan100% (3)
- OB-GYNE 2 Batch 2017 Ratio PDFDokumen13 halamanOB-GYNE 2 Batch 2017 Ratio PDFAdrianBelum ada peringkat
- Method Statement - Fire Rated Duct Insulation.Dokumen16 halamanMethod Statement - Fire Rated Duct Insulation.suhail kalody100% (2)
- MCQ'S FOR Obstetrics and GynaecologyDokumen330 halamanMCQ'S FOR Obstetrics and Gynaecologywhoosh200887% (108)
- MCQDokumen99 halamanMCQhemazzzz80% (5)
- Recommended Books For MRCOG Part 2 ExaminationsDokumen9 halamanRecommended Books For MRCOG Part 2 Examinationssaqii67% (6)
- MCQs Gynaec 2 - ObGynDokumen10 halamanMCQs Gynaec 2 - ObGynbmhsh100% (3)
- Grade 10 Worksheet on Reproductive Health LawsDokumen7 halamanGrade 10 Worksheet on Reproductive Health LawsLeode Joy Tulang100% (1)
- Instruction Manual in Obstetrics: Volume OneDari EverandInstruction Manual in Obstetrics: Volume OneBelum ada peringkat
- Accounting for Partnership and Corporation ModuleDokumen32 halamanAccounting for Partnership and Corporation ModuleMary Lynn Dela PeñaBelum ada peringkat
- OBGYN ultrasound exam questionsDokumen19 halamanOBGYN ultrasound exam questionssalamred100% (2)
- Obst 5 - All Obstetrics 1 2021Dokumen22 halamanObst 5 - All Obstetrics 1 2021Menna KamalBelum ada peringkat
- Ob &gyDokumen6 halamanOb &gyThumz ThuminBelum ada peringkat
- Obstetrics and Gynecology Mock ReviewDokumen14 halamanObstetrics and Gynecology Mock ReviewokurimkuriBelum ada peringkat
- Ectopic Pregnancy MCQDokumen2 halamanEctopic Pregnancy MCQIniyaval Ravindran100% (2)
- Obg MCQSDokumen11 halamanObg MCQSShriyansh ChaharBelum ada peringkat
- C. Anovulation: C. Dysfunctional Uterine BleedingDokumen18 halamanC. Anovulation: C. Dysfunctional Uterine BleedingJan Mikhail Frasco100% (1)
- Gyna Full QDokumen43 halamanGyna Full QMohammed Isa HomidatBelum ada peringkat
- OBS & GYN MCQsDokumen10 halamanOBS & GYN MCQsmaximBelum ada peringkat
- PG Neet Obg Mcqs 90 - Malpresentation and Obstructed Labour - 1Dokumen15 halamanPG Neet Obg Mcqs 90 - Malpresentation and Obstructed Labour - 1أ.م.د. ايناس جليل حسينBelum ada peringkat
- PROLOG: Gynecology and SurgeryDari EverandPROLOG: Gynecology and SurgeryPenilaian: 5 dari 5 bintang5/5 (2)
- PROLOG: Obstetrics, Eighth Edition (Assessment & Critique)Dari EverandPROLOG: Obstetrics, Eighth Edition (Assessment & Critique)Penilaian: 5 dari 5 bintang5/5 (2)
- Will Obstetri 2-8 Maret 2018Dokumen16 halamanWill Obstetri 2-8 Maret 2018Shandy Suwanto Putra100% (2)
- Obstetrics and Gynecology Question PapersDokumen22 halamanObstetrics and Gynecology Question Papersprinceej83% (18)
- كامل نساءDokumen181 halamanكامل نساءYasser ArefBelum ada peringkat
- Basic Geriatric Nursing 6th Edition Williams Test BankDokumen24 halamanBasic Geriatric Nursing 6th Edition Williams Test BankJimmyHaynessfmg100% (47)
- The ERAS® Society Handbook for Obstetrics & GynecologyDari EverandThe ERAS® Society Handbook for Obstetrics & GynecologyGregg NelsonBelum ada peringkat
- Obstetrics MCQs Ten TeachersDokumen11 halamanObstetrics MCQs Ten TeachersSuhaila Ahmed100% (5)
- DR Khaled Final Exam MCQ 2012 - 2013Dokumen89 halamanDR Khaled Final Exam MCQ 2012 - 2013ﻣﻠﻚ عيسى100% (2)
- Operative Gyn MCQ PDFDokumen10 halamanOperative Gyn MCQ PDFFentahun TadesseBelum ada peringkat
- OBGYN 1st Round 2021 AnsweredDokumen14 halamanOBGYN 1st Round 2021 AnsweredMuhammed Mostafa100% (4)
- DNB Obgy McqsDokumen5 halamanDNB Obgy McqsSandip PatilBelum ada peringkat
- Question 3Dokumen19 halamanQuestion 3Anonymous LF9aizGhaBelum ada peringkat
- ObstetricsDokumen8 halamanObstetricsrevathidadam55555100% (1)
- Gyne 2018 5th year exam محلول PDFDokumen27 halamanGyne 2018 5th year exam محلول PDFMohammad HereshBelum ada peringkat
- Paper 2 (OBS) Jan 2018 RecallsDokumen19 halamanPaper 2 (OBS) Jan 2018 RecallshummaBelum ada peringkat
- MCQ For PG Entrance Obstetrics and Gynaecology PDFDokumen2 halamanMCQ For PG Entrance Obstetrics and Gynaecology PDFdraymanonline.com100% (1)
- PROLOG: Patient Management in the Office, Eighth EditionDari EverandPROLOG: Patient Management in the Office, Eighth EditionBelum ada peringkat
- Obstetrics mcqs pdf: The ultimate study guideDokumen2 halamanObstetrics mcqs pdf: The ultimate study guiderevathidadam5555588% (8)
- Essay Q's Obs and Gyn 2Dokumen2 halamanEssay Q's Obs and Gyn 2whoosh200886% (7)
- MCQ GynecologyDokumen25 halamanMCQ GynecologyAli Alhaddi80% (5)
- Soal MCQ UI 2009Dokumen14 halamanSoal MCQ UI 2009Suzette100% (1)
- Flow Cytometry in Clinical DiagnosisDokumen16 halamanFlow Cytometry in Clinical DiagnosisRaj Cella0% (1)
- Gynaemcq 120602094722 Phpapp02Dokumen7 halamanGynaemcq 120602094722 Phpapp02Melissa Aina Mohd Yusof100% (1)
- Obstetrics Mcqs PDFDokumen2 halamanObstetrics Mcqs PDFJennifer47% (17)
- MCQ sample questions on mechanisms of labour and pregnancy complicationsDokumen11 halamanMCQ sample questions on mechanisms of labour and pregnancy complicationsMuhammad Bilal100% (2)
- Soal Usulan UnHas Juli 2019Dokumen25 halamanSoal Usulan UnHas Juli 2019Ibnu SinaBelum ada peringkat
- CV3038 Stair Tower Bracing JSEA REV.ADokumen13 halamanCV3038 Stair Tower Bracing JSEA REV.ADavid ThomasBelum ada peringkat
- M2: Quiz No. 1: Attempt HistoryDokumen10 halamanM2: Quiz No. 1: Attempt History수지Belum ada peringkat
- Midstream Clean Catch Urine CollectionDokumen1 halamanMidstream Clean Catch Urine CollectionChristian Jewel GambolBelum ada peringkat
- Angat Buhay:: Partnerships Against PovertyDokumen15 halamanAngat Buhay:: Partnerships Against PovertyMeg TorresBelum ada peringkat
- Pedro Velazquez - Blood Vessels WorksheetDokumen4 halamanPedro Velazquez - Blood Vessels Worksheetapi-391255953Belum ada peringkat
- CPS 2 ToxicologyDokumen31 halamanCPS 2 ToxicologyNgọc Hà NguyễnBelum ada peringkat
- Jane Doe, Et Al., v. Dr. Paul Jones, Et Al.Dokumen17 halamanJane Doe, Et Al., v. Dr. Paul Jones, Et Al.Michael_Roberts2019Belum ada peringkat
- Allianz Health Silver SingleDokumen17 halamanAllianz Health Silver SingleBrayan Willian Ferreira RodriguesBelum ada peringkat
- Ielts Speaking Transcript 1 3Dokumen3 halamanIelts Speaking Transcript 1 3Hồng NhiBelum ada peringkat
- CAD-CAM Milled Versus Rapidly Prototyped (3d-Printed) Complete Dentures: An in Vitro Evaluation of TruenessDokumen7 halamanCAD-CAM Milled Versus Rapidly Prototyped (3d-Printed) Complete Dentures: An in Vitro Evaluation of TruenessAkshayaa BalajiBelum ada peringkat
- Consult - Quality Qualite Eng PDFDokumen44 halamanConsult - Quality Qualite Eng PDFFaisal AbbasBelum ada peringkat
- Webinar - I-WPS OfficeDokumen31 halamanWebinar - I-WPS OfficeGayathri sundarajanBelum ada peringkat
- Molecular identification of cystic echinococcosis risk factors in MongoliaDokumen19 halamanMolecular identification of cystic echinococcosis risk factors in MongoliaBảo NgọcBelum ada peringkat
- Brokenshire College Socsksargen, Inc.: NCM 100-Theorerical Foundations in NursingDokumen8 halamanBrokenshire College Socsksargen, Inc.: NCM 100-Theorerical Foundations in NursingKeren Happuch EspirituBelum ada peringkat
- QR Chapter 1 3 SilorioDokumen19 halamanQR Chapter 1 3 SilorioAnton GoBelum ada peringkat
- Chapter Three The Components of Child Protection: A Brief Overview of Specific Child Protection IssuesDokumen10 halamanChapter Three The Components of Child Protection: A Brief Overview of Specific Child Protection IssuesButa DenisBelum ada peringkat
- CHN FNCP IdbDokumen8 halamanCHN FNCP IdbKaren AngelBelum ada peringkat
- Sabri T. Shuker - Maxillofacial Air-Containing Cavities, Blast Implosion Injuries, and ManagementDokumen8 halamanSabri T. Shuker - Maxillofacial Air-Containing Cavities, Blast Implosion Injuries, and ManagementYamveaBelum ada peringkat
- Pubpol 511Dokumen12 halamanPubpol 511Joshua WhiteBelum ada peringkat
- Pointers To Review in Discipline Ideas in The Applied Social SciencesDokumen3 halamanPointers To Review in Discipline Ideas in The Applied Social SciencesAngelo Jose De GuiaBelum ada peringkat
- Sample Patient ProfileDokumen7 halamanSample Patient ProfileElisabeth CampbellBelum ada peringkat
- Biology: Cambridge International Examinations International General Certificate of Secondary EducationDokumen20 halamanBiology: Cambridge International Examinations International General Certificate of Secondary Educationmath magicBelum ada peringkat
- Medical Surgical Nursing 3 BulletsDokumen4 halamanMedical Surgical Nursing 3 BulletsQueen ElizabethBelum ada peringkat