Endometriosis
Diunggah oleh
LokHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Endometriosis
Diunggah oleh
LokHak Cipta:
Format Tersedia
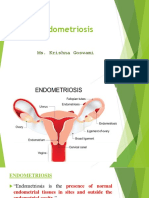
ENDOMETRIOSIS
Endometriosis is a benign condition in which endometrial glands and
stroma are present outside the uterine cavity and walls. Endometriosis
is important in gynecology because of its frequency, distressing
symptomatology, association with infertility, and potential for invasion
of adjacent organ systems, such as the gastrointestinal or urinary
tracts. Endometriosis often presents a difficult diagnostic challenge,
and few gynecologic conditions can require such difficult surgical
dissections.
INCIDENCE
The incidence of endometriosis in the general population is not known,
but it is estimated that 5% to 15% of women have some degree of the
disease. At least one-third of women with chronic pelvic pain have
visualized endometriosis, as do a significant number of infertile
women. Interestingly, endometriosis is noted in 5% to 15% of women
undergoing gynecologic laparotomies, and it is an unexpected finding
in approximately half of these cases.
The typical patient with endometriosis is in her 30s, nulliparous, and
infertile. However, in practice, many women with endometriosis do not
fit the classic picture. Occasionally, endometriosis may occur in
infancy, childhood, or adolescence, but at these early ages, it is usually
associated with obstructive genital anomalies. Although endometriosis
should regress following the menopause unless estrogens are
prescribed, 5% of new cases develop in that age group. In addition, the
scarifying involution from preexisting lesions may result in obstructive
problems, especially in the gastrointestinal and urinary tracts.
PATHOGENESIS
The pathogenesis of endometriosis is not understood. Genetic
predisposition clearly plays a role. The following three hypotheses have
been used to explain the various manifestations of endometriosis and
the different locations in which endometriotic implants can be found:
1. The retrograde menstruation theory of Sampson proposes that endometrial
fragments transported through the fallopian tubes at the time of
menstruation implant and grow in various intraabdominal sites.
1 By: Dr L.B. Shrestha, Dharan, Nepal
Endometrial tissue, which is normally shed at the time of menstruation, is
viable and capable of growth in vivo or in vitro. To explain some rare
examples of endometriosis in distant sites, such as the lung, forehead, or
axilla, it is necessary to postulate hematogenous spread.
2. The müllerian metaplasia theory of Meyer proposes that endometriosis
results from the metaplastic transformation of peritoneal mesothelium into
endometrium under the influence of certain, generally unidentified stimuli.
3. The lymphatic spread theory of Halban suggests that endometrial tissues
are taken up into the lymphatics draining the uterus and are transported to
the various pelvic sites where the tissue grows ectopically. Endometrial
tissue has been found in pelvic lymphatics in up to 20% of patients with the
disease.
Most authorities today believe that several factors are involved in the
initiation and spread of endometriosis, including retrograde
menstruation, coelomic metaplasia, immunologic changes and genetic
predisposition.
SITES OF OCCURRENCE
Endometriosis occurs most commonly in the dependent portions of the
pelvis. Specifically, implants can be found on the ovaries, the broad
ligament, the peritoneal surfaces of the cul-de-sac (including the
uterosacral ligaments and posterior cervix), and the rectovaginal
septum. Quite frequently, the rectosigmoid colon is involved, as is the
appendix and the vesicouterine fold of peritoneum. Endometriosis is
occasionally seen in laparotomy scars, developing especially after a
cesarean section or myomectomy when the endometrial cavity has
been entered. It is probable that endometrial tissue is seeded into the
surgical incision. Two out of three women with endometriosis have
ovarian involvement.
SYMPTOMS
The characteristic triad of symptoms associated with endometriosis is
dysmenorrhea, dyspareunia, and Dyschezia. Interestingly, there is no
clear relationship between the stage of endometriosis and the
frequency and severity of pain symptoms.
Dyspareunia is generally associated with deep-thrust penetration
during intercourse and occurs mainly when the cul-de-sac, uterosacral
ligaments, and portions of the posterior vaginal fornix are involved.
2 By: Dr L.B. Shrestha, Dharan, Nepal
Dyschezia is experienced with uterosacral, cul-de-sac, and
rectosigmoid colon involvement.
Premenstrual and postmenstrual spotting is a characteristic symptom
of endometriosis.
SIGNS
Endometriosis presents with a wide variety of signs varying from the
presence of a small, exquisitely tender nodule in the cul-de-sac or on
the uterosacral ligaments to a huge, relatively nontender, cystic
abdominal mass. Occasionally, a small tender mulberry spot may be
seen in the posterior fornix of the vagina. Characteristically, a tender,
fixed adnexal mass is appreciated on bimanual examination. The
uterus is fixed and retroverted in a substantial number of women with
endometriosis. Occasionally, no signs at all are appreciated on physical
examination.
DIFFERENTIAL DIAGNOSIS
(1) Chronic pelvic inflammatory disease or recurrent acute salpingitis
(2) Hemorrhagic corpus luteum,
(3) Benign or malignant ovarian neoplasm, and, occasionally,
(4) Ectopic pregnancy.
DIAGNOSIS
The diagnosis of endometriosis should be suspected in an afebrile
patient with the characteristic triad of pelvic pain, a firm, fixed, tender
adnexal mass, and tender nodularity in the cul-de-sac and uterosacral
ligaments. The characteristic sharp, firm, exquisitely tender "barb"
(from barbed wire) felt in the uterosacral ligament is the diagnostic
sine qua non of endometriosis, but this finding is generally present
only in severe cases.
The definitive diagnosis is generally made by the characteristic gross
and histologic findings obtained at laparoscopy or laparotomy.
MANAGEMENT
3 By: Dr L.B. Shrestha, Dharan, Nepal
The management of endometriosis depends on certain key
considerations: (1) the certainty of the diagnosis, (2) the severity of
the symptoms, (3) the extent of the disease, (4) the desire for future
fertility, (5) the age of the patient, and (6) the threat to the
gastrointestinal or urinary tract or both.
Treatment is indicated for endometriosis associated pelvic pain,
dysmenorrhea, dyspareunia, abnormal bleeding, ovarian cysts, and
infertility due to gross distortion of tubal and ovarian anatomy.
There is no convincing evidence that treatment improves fertility in
women with mild endometriosis.
Surgical Treatments
The most comprehensive surgery includes total abdominal
hysterectomy, bilateral salpingo-oophorectomy with destruction of all
peritoneal implants, and dissection of all adhesions.
Nearly 25% of kidneys are lost when endometriosis blocks the ureter.
Often the desire for future fertility precludes this surgical option.
Large endometriomas (>3 cm) are amenable only to surgical resection.
Preoperative treatment with medical agents, such as gonadotropin-
releasing hormone (GnRH) agonists for 3 to 6 months can improve
surgical success.
There is a risk of recurrence of endometriosis throughout a woman's
life
Medical Treatments
Therapy should be targeted toward relieving the patient's individual
complaints and toward reducing the risk of disease progression.
Asymptomatic women found incidentally to have endometriosis may
not require any therapy.
For relief of pelvic pain, short-term treatment may be used, and either
a GnRH-agonist or danazol appears to be equally effective.
4 By: Dr L.B. Shrestha, Dharan, Nepal
Danazol is an androgenic derivative that may be used in a
"pseudomenopause" regimen to suppress symptoms of endometriosis
if fertility is not a present concern.
Three years after cessation of Danazol, 40% of patients will have
recurrence of endometriosis. After a full course of danazol therapy, use
of a cyclic oral contraceptive may help to delay or prevent such
recurrence.
GnRH-agonists effect a temporary medical castration, thereby bringing
about a marked, albeit temporary, regression of endometriosis.
Oral contraceptives and oral medroxyprogesterone acetate are more effective in
treating endometriosis-associated pelvic pain than placebos.
5 By: Dr L.B. Shrestha, Dharan, Nepal
Anda mungkin juga menyukai
- Endometriosis: OccurrenceDokumen6 halamanEndometriosis: Occurrencewea xczBelum ada peringkat
- EndometrisisDokumen10 halamanEndometrisisAmmarBelum ada peringkat
- EndometriosisDokumen46 halamanEndometriosisManoj Ranadive0% (1)
- Kocakoc 2008Dokumen16 halamanKocakoc 20087dc2s9tdrwBelum ada peringkat
- Endometriosis Adenomyosis Dr-IrabonDokumen67 halamanEndometriosis Adenomyosis Dr-IrabonAbegail IbañezBelum ada peringkat
- Endometriosis - Clinical Features - Diangosis - TeachMeObGynDokumen3 halamanEndometriosis - Clinical Features - Diangosis - TeachMeObGynLiridon SopajBelum ada peringkat
- Department of Prasuti Tantra and Striroga Dayanand Ayurvedic College, Jalandhar SESSION 2016-17Dokumen40 halamanDepartment of Prasuti Tantra and Striroga Dayanand Ayurvedic College, Jalandhar SESSION 2016-17jyothiBelum ada peringkat
- Endometriosis - Pathogenesis, Clinical Features, and Diagnosis - UpToDateDokumen42 halamanEndometriosis - Pathogenesis, Clinical Features, and Diagnosis - UpToDateOrlando GuerraBelum ada peringkat
- En DoDokumen8 halamanEn DoJair EnriquezBelum ada peringkat
- Deep Infiltrating Endometriosis: Symptoms and Diagnostic Procedures. The Symptoms As Well As Clinical FindingsDokumen5 halamanDeep Infiltrating Endometriosis: Symptoms and Diagnostic Procedures. The Symptoms As Well As Clinical FindingsBunga JuwitaBelum ada peringkat
- Endometriosis - Pathogenesis, Clinical Features, and Diagnosis - UpToDateDokumen39 halamanEndometriosis - Pathogenesis, Clinical Features, and Diagnosis - UpToDatefujimeisterBelum ada peringkat
- EndometriomaDokumen7 halamanEndometriomaErick Rafael AncaBelum ada peringkat
- ENDOMETRIOSISDokumen17 halamanENDOMETRIOSISPeterson Wachira HscBelum ada peringkat
- Endo Metros IsDokumen24 halamanEndo Metros IsPatel NenshiBelum ada peringkat
- EndometriosisDokumen15 halamanEndometriosispalohe1277Belum ada peringkat
- EndometriosisDokumen17 halamanEndometriosisIngrid HerreraBelum ada peringkat
- ADENOMYOSISDokumen5 halamanADENOMYOSISdoddydrBelum ada peringkat
- The Association Between Endometriomas and Ovarian Cancer: Preventive Effect of Inhibiting Ovulation and Menstruation During Reproductive LifeDokumen10 halamanThe Association Between Endometriomas and Ovarian Cancer: Preventive Effect of Inhibiting Ovulation and Menstruation During Reproductive LifeMohamad Syaikhul IslamBelum ada peringkat
- Endometri Osis: Par Khmermedical StudyDokumen18 halamanEndometri Osis: Par Khmermedical StudyLeang KarichakBelum ada peringkat
- Impey Obs and Gynae Revision Notes PDFDokumen9 halamanImpey Obs and Gynae Revision Notes PDFRoiseBelum ada peringkat
- Womb Gynecological Endometrial Cells Uterine Cavity: Endometriosis (From Endo, "Inside", and Metra, "Dokumen3 halamanWomb Gynecological Endometrial Cells Uterine Cavity: Endometriosis (From Endo, "Inside", and Metra, "remyavarghese25Belum ada peringkat
- Die 1Dokumen18 halamanDie 1juan carlos pradaBelum ada peringkat
- TTEA BrochureDokumen2 halamanTTEA BrochureSteve MaximayBelum ada peringkat
- Benign Lesions of The OvariesDokumen12 halamanBenign Lesions of The OvariesdocjosmaBelum ada peringkat
- Myoma Uteri/Fibroids/ Leiomyomata: Symptoms of Uterine Myoma May IncludeDokumen3 halamanMyoma Uteri/Fibroids/ Leiomyomata: Symptoms of Uterine Myoma May IncludeDiane MargretBelum ada peringkat
- Associate Professor:Ivan Bonet. Obstetric and Gynecology Associate Professor:Ivan Bonet. Obstetric and GynecologyDokumen31 halamanAssociate Professor:Ivan Bonet. Obstetric and Gynecology Associate Professor:Ivan Bonet. Obstetric and Gynecologyivan0% (1)
- ENDOMETRIOSISsDokumen27 halamanENDOMETRIOSISsNouman HameedBelum ada peringkat
- Endometriosis at Caesarian Section Scar: Khalifa Al-JabriDokumen2 halamanEndometriosis at Caesarian Section Scar: Khalifa Al-JabriJuan SetiajiBelum ada peringkat
- DR Sankalpa R WankhedeDokumen76 halamanDR Sankalpa R Wankhedechaitanya suryawanshiBelum ada peringkat
- Female Genital Cysts Tract PDFDokumen6 halamanFemale Genital Cysts Tract PDFRaraBelum ada peringkat
- 2.1gyne Endometriosis PDFDokumen9 halaman2.1gyne Endometriosis PDFFAtty ACidsBelum ada peringkat
- Endometriosis: Pathogenesis, Clinical Features, and Diagnosis - UpToDateDokumen41 halamanEndometriosis: Pathogenesis, Clinical Features, and Diagnosis - UpToDateRafael Vilano AvelarBelum ada peringkat
- 1 GYNE 7 - EndometriosisDokumen6 halaman1 GYNE 7 - EndometriosisIrene FranzBelum ada peringkat
- Benign Gynecological LesionsDokumen9 halamanBenign Gynecological LesionsLanceBelum ada peringkat
- Ahmed Ali - AdenomyosisDokumen6 halamanAhmed Ali - AdenomyosisAhmed AliBelum ada peringkat
- EndometriosisDokumen4 halamanEndometriosisAno DzamelashviliBelum ada peringkat
- Jurnal Polip EndometriumDokumen4 halamanJurnal Polip EndometriumNamira AmmarinBelum ada peringkat
- Role of Laparoscopic Surgery in Endometriosis Associated Infertility - Literature ReviewDokumen7 halamanRole of Laparoscopic Surgery in Endometriosis Associated Infertility - Literature ReviewFaza KahfiBelum ada peringkat
- Endometriosis Is A Common Disease in Women of Reproductive Age and IsDokumen45 halamanEndometriosis Is A Common Disease in Women of Reproductive Age and IsSreekanth reddyBelum ada peringkat
- Endometriosis and AdenomyosisDokumen49 halamanEndometriosis and AdenomyosisOmar HamwiBelum ada peringkat
- AdenomyosisDokumen16 halamanAdenomyosisWiwik'RatnaSariPratiwi'100% (2)
- From The Archives of The AFIP: Endometriosis: Radiologic-Pathologic CorrelationDokumen24 halamanFrom The Archives of The AFIP: Endometriosis: Radiologic-Pathologic Correlation104022432 104a-Belum ada peringkat
- Ndometriosis: A Guide For PatientsDokumen16 halamanNdometriosis: A Guide For PatientsYusran AchmadBelum ada peringkat
- Swatilekha Das (RN, MSN)Dokumen20 halamanSwatilekha Das (RN, MSN)sandeepv08Belum ada peringkat
- EndometriosisDokumen2 halamanEndometriosiswhatisendometriosisBelum ada peringkat
- Adeno Related LitDokumen2 halamanAdeno Related Litflorence zemogBelum ada peringkat
- Kista Ovarium 21906150Dokumen43 halamanKista Ovarium 21906150NUR ATHIFAHBelum ada peringkat
- Abdominal Wall Incision Scar Endometriosis: Olgu SunumuDokumen3 halamanAbdominal Wall Incision Scar Endometriosis: Olgu SunumuwererewwerwerBelum ada peringkat
- Presentation 1Dokumen20 halamanPresentation 1Mohamad HafyfyBelum ada peringkat
- Endometriosis O&g PresentationDokumen31 halamanEndometriosis O&g PresentationChauthiran Agamudaiyar100% (1)
- An Unusual Localization of Leiomyoma: Vaginal LeiomyomaDokumen4 halamanAn Unusual Localization of Leiomyoma: Vaginal Leiomyomaistiana sariBelum ada peringkat
- Endometriosis: by Jane LyttletonDokumen8 halamanEndometriosis: by Jane Lyttletonitsik12886Belum ada peringkat
- EndometriosisDokumen10 halamanEndometriosisSivaram Shanmugha VilasBelum ada peringkat
- Disgerminom OvarianDokumen7 halamanDisgerminom OvarianIfrim MihaelaBelum ada peringkat
- EndometriosisDokumen50 halamanEndometriosisHannah Eloise MagsinoBelum ada peringkat
- EndometriozaDokumen17 halamanEndometriozaLoredanaBelum ada peringkat
- Keperwatan DasarDokumen14 halamanKeperwatan DasarAdiva LidiyaBelum ada peringkat
- Swatilekha Das (RN, MSN)Dokumen20 halamanSwatilekha Das (RN, MSN)sandeepv08Belum ada peringkat
- Umbilical Endometriosis: A Case ReportDokumen5 halamanUmbilical Endometriosis: A Case ReportIJAR JOURNALBelum ada peringkat