App Framework V 3
Diunggah oleh
api-251641757Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
App Framework V 3
Diunggah oleh
api-251641757Hak Cipta:
Format Tersedia
Benefits of Nutrition
Physical Wellbeing Weight Management Energy Bone strength Cardiovascular Health Social Wellbeing
Mental Wellbeing Improved self-esteem and confidence
Social involvement
Introduction:
It is well documented that obesity and physical inactivity are risk factors for cardiovascular disease, high blood pressure, and type-2 diabetes (National Heart, Lung, and Blood Institute, 2012). Unfortunately, individuals with developmental disabilities (IDD) are twice as likely to be overweight and obese (Stewart, Beange and Mackerras, 1994), making them more susceptible to diseases linked to obesity. For this population, contributing factors to obesity and physical inactivity were found to include feeding habits (Stewart, Beange and Mackerras, 1994), lifestyle choices (Messent, 1999, Robertson et al.2000), lack of education (Mikulovic et al., 2011), and low income (Links and Phelan, 1995). In addition to obesity, the prevalence of underweight IDD were four times higher than the general public, suggesting an overall limited understanding of healthy lifestyle choices (Bhaumik et al., 2008). Therefore, an accessible educational tool on nutrition and lifestyle for IDD would greatly benefit this population as a whole.
Nutrition
Lack of Education for IDD
Feeding Habits
Lack of Accessible resources
Lifestyle choices: People in the community with limited incomes are less likely to eat healthily or have opportunities to engage in physical activities - Bhaumik et al., 2008.
Many caregivers lack the education and support they need to improve the lifestyle of the IDD. As a result, some caregivers are pulled to their limits and overprotect by restricting involvement in community activities, followed by compensating behaviours such as overfeeding the individual in their care (Bhaumik et al, 2008). By applying changes to lifestyle and feeding behaviour, it is possible to address the preventable causes of obesity. For example, staying active in the house by sweeping, mopping, vacuuming, dusting, gardening, etc. (Villeneuve, 2013) can replace sedentary behaviour such as watching television and video games. Reducing these behaviour, that can occupy almost 4 hours a day for IDD (Mikulovic et al., 2011), enables this population to boost metabolism and cardiac function.
Feeding Habits: Although it has been reported that approximately 50% of IDD are within a normal body mass index (Mikulovic et al., 2011), these values are determined by weight alone, and may not be indicative of nutritional intake. As ratios of overweight and underweight IDD increase in comparison to the general public, the significance of informing IDD and their caregivers of nutritionally healthy and low calorie foods increases. Physical and mental improvements to a healthier feeding habit include more energy, increased knowledge, more confidence and selfesteem, and fewer serious health issues obesity, diabetes, and heart disease (Marks, Sisirak and Heller, 2010). With known factors such as physical inactivity as being one of the greatest limiting factors to a healthy lifestyle for individuals with disabilities (Messent, 1999; Robertson et al. 2000), educational information for IDD & caregivers should consider product mediums that allow access through a set of low barriers. Low-Income: It was observed that socioeconomic status (SES) of parents was linked to weight status, with a higher prevalence of overweight present in the lower SES category. Thus, obesity appears to be exacerbated by social inequalities, which are concomitant to health inequalities. - Mikulovic et al., 2011; pg.1 Studies for decades have shown that physical and mental wellbeing are linked and can be considered two aspects of the same component. The mental-physical conversation has effectively overshadowed the development of social wellbeing. Nevertheless, as Link and Phelan (1995; p.2) has pointed out, social conditions such as SES and social support significantly affect access to important resources that help individuals avoid lower life expectancy, higher overall mortality rates and higher rates of infant and perinatal mortality. For example, general nutritional information from credible organizations may be accessible to the public, but for IDD, there are significant gaps between this information and practical daily applications.
To address nutritional needs for IDD, it is important to identify the social positions that experience the greatest effects. In 2011, the government of Canada found that 23.5% (Financial Security, 2011) of people with disabilities were below the poverty line based on after-tax Low-
income cut offs (LICO). This percentage was second, behind only unattached individuals aged 45-64 (34.8%), of which, 18.3% (Population with a disability, 2007) documented at least one disability, representing large margins of overlap with populations with disabilities. Therefore, the production of relevant educational content must be packaged and presented to apply scientifically proven information specifically towards daily uses. Providing accessible functional resources will educate IDD & their caregivers, improving nutritional health and subsequently reducing cases of obesity, diabetes, dependence on medication, and overall poor physical wellbeing. Specifically, the Canadas Food Guide may be re-introduced to mitigate nutritional concerns for low-income IDD. Utilizing existing tools such as the food guide as the foundation for nutrition education allows for familiar and consistent language recognitions, assisting the application of general knowledge. Since 1977, Canada has adopted the following four basic food groups: 4 food groups: 1. Vegetables [vej-tuh-buh ] and Fruit Green leafy vegetables Rich in Iron! broccoli, cauliflower, spinach, kale Coloured vegetables Vitamin A! carrots, tomatoes, beets Apricot, Grapefruit, Bananas, Watermelon, Kiwi 2. Grain products bread, cooked pasta, cooked rice, cereal 3. Milk and Alternatives [awl-tur-nuh-tiv, al-] milk, soy, yogurt, cheese 4. Meat and Alternatives Protein and Iron! cooked fish, lean meat, tofu, eggs, cooked legumes To maintain a healthy lifestyle, it is also important to stay hydrated: Get Hydrated: Water, Tea, Coffee,
Milk or Soups Avoid: juice, pop, sugary drinks - half a cup or more of sugary drinks can increase risk of diabetes and excess weight gain. Infant: Ages 1-3: Ages 4-8: 9-13: 14-18: Men 18+: Women 18+: BENEFITS! keeps blood pressure normal *Green Tea is affordable and has proven anti-obesity effects! (Wolfram, Wang and Thielecke, 2006). TIPS! flavour water with lemon juice, mint leaves or sweeteners such as Crystal Light if not a fan of water. Following the four food groups extends into a balanced intake. Portion Sizes: For a balanced diet, Healthy plate portions should be: 1/2 vegetables, 1/4 whole grains, 1/4 meat or protein. (maybe a picture) Even when food choices are unchanged, healthy portions can help manage weight! For adults: Fruit and vegetable: 7-8 servings/day Meat: 3 ounce per serving 3 cups a day 4 cups 5 cups 7 cups 7 cups 3L or 12 cups 2.2L or 9 cups
Most importantly, to apply the nutritional content to low-income populations: Eating healthy on a budget! Frozen vegetables are very affordable--try different types to mix up the varieties and nutrients - full of Vitamins A, B, C & fibre! Canned beans and legumes: chickpeas, kidney beans, bean medleys.
TIPS: purchase food in season! Fall - apples, Summer - berries, pineapple Year Round bananas, oranges. Freeze fruits purchased when they're cheaper to have later on can also reduce costs. Milk is typically pretty affordable, but if it's not, dried skim milk powder works too
Meats: Affordable Cuts of Meat: Beef: ground, mince, chuck, blade, brisket Lamb: Shoulder, neck, gigot, chop Chicken: Thigh Pork: Belly, Shoulder, Gigot, chop Fish: drum fish, herring, sardines, atlantic mackerel, tilapia, trout, pollock. Frozen or Canned fish also tend to be lower cost. *Sardines are one of the most nutritionally dense foods! TIP: Buy in bulk, freeze for later!
References: Bhaumik, S., Watson, J. M., Thorp, C. F., Tyrer, F., & McGrother, C. W. (2008). Body mass index in adults with intellectual disability: distribution, associations and service implications: a populationbased prevalence study. Journal of Intellectual Disability Research, 52(4), 287-298. Department of Health (2003). Tackling Health Inequalities. A Programme for Action. Her Majestys Stationery Office, London. Disability Rights Commission (2006). Equal Treatment: Closing the Gap. A Formal Investigation into Physical Health Inequalities Experienced by People with Learning Disabilities and/or Mental Health Problems. Disability Rights Commission, London. Financial Security, (2011). Government of Canada employment and social development. Accessed http://www4.hrsdc.gc.ca/.3ndic.1t.4r@-eng.jsp?iid=23#M_4 Fishbein, D., & Meduski, J. (1987). Nutritional biochemistry and behavioral disabilities. Journal of learning disabilities, 20(8), 505-512.
Four food groups, (2007). Health Canada, Accessed: http://www.hc-sc.gc.ca/fn-an/food-guidealiment/context/fg_history-histoire_ga-eng.php Villeneuve. (2013). Staying Active as You Age Workbook. Link, B. G., & Phelan, J. (1995). Social conditions as fundamental causes of disease. Journal of health and social behavior, 80-94. Marks, B., Sisirak, J., & Heller, T. (2010). Health Matters: The Exercise and Nutrition Health Education Curriculum for People with Developmental Disabilities. Brookes Publishing Company. Messent, R., Cooke, C.B., Long, J.P. (1999). Primary and secondary barriers to physically active healthy lifestyles for adults with learning disabilities. Disability & Rehabilitation, 21(9), 409419. Mikulovic, J., Marcellini, A., Compte, R., Duchateau, G., Vanhelst, J., Fardy, P. S., & Bui-Xuan, G. (2011). Prevalence of overweight in adolescents with intellectual deficiency. Differences in socio-educative context, physical activity and dietary habits. Appetite, 56(2), 403-407. National Audit Office (2001) Tackling Obesity in England. Report by the Comptroller and Auditor General. Her Majestys Stationary Office, London. National Heart, Lung, and Blood Institute, 2012. Accessed: http://www.nhlbi.nih.gov/health/health-topics/topics/obe/risks.html Population with a disability, (2007). Government of Canada employment and social development. Accessed: http://www4.hrsdc.gc.ca/.3ndic.1t.4r@-eng.jsp?iid=40 Robertson, J., Emerson, E., Gregory, N., Hatton, C., Turner, S., Kessissoglou, S., & Hallam, A. (2000). Lifestyle related risk factors for poor health in residential settings for people with intellectual disabilities. Research in developmental disabilities, 21(6), 469-486. Stewart, L., Beange, H., & Mackerras, D. (1994). A survey of dietary problems of adults with learning disabilities in the community. Mental Handicap Research, 7(1), 41-50. Wolfram, S., Wang, Y., & Thielecke, F. (2006). Antiobesity effects of green tea: From bedside to bench. Molecular nutrition & food research, 50(2), 176-187.
Anda mungkin juga menyukai
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Gamify Your Classroom - A Field Guide To Game-Based Learning, Revised EditionDokumen372 halamanGamify Your Classroom - A Field Guide To Game-Based Learning, Revised EditionCuong Tran VietBelum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Carcinoma of PenisDokumen13 halamanCarcinoma of Penisalejandro fernandezBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
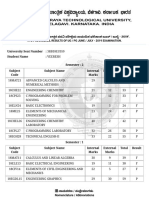
- VTU Result PDFDokumen2 halamanVTU Result PDFVaibhavBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Conflict Management Strategy ThesisDokumen16 halamanConflict Management Strategy ThesisKrizna Dingding DotillosBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Monograph SeismicSafetyDokumen63 halamanMonograph SeismicSafetyAlket DhamiBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- scn615 Classroomgroupactionplan SarahltDokumen3 halamanscn615 Classroomgroupactionplan Sarahltapi-644817377Belum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- A Review of Cassiterite Beneficiation PraticesDokumen23 halamanA Review of Cassiterite Beneficiation PraticesLevent ErgunBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- MMW CH4 L2Dokumen20 halamanMMW CH4 L2Charles Patrick GarciaBelum ada peringkat
- Ila 0306Dokumen11 halamanIla 0306Hong ChenBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Edgardo Macabulos - FS1-Activity-1Dokumen8 halamanEdgardo Macabulos - FS1-Activity-1Macabulos Edgardo SableBelum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Doloran Auxilliary PrayersDokumen4 halamanDoloran Auxilliary PrayersJosh A.Belum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Crim Pro Exam Sheet at A Glance.Dokumen5 halamanCrim Pro Exam Sheet at A Glance.Heather Kinsaul Foster80% (5)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Jackson Et Al 2019 Using The Analytical Target Profile To Drive The Analytical Method LifecycleDokumen9 halamanJackson Et Al 2019 Using The Analytical Target Profile To Drive The Analytical Method LifecyclerbmoureBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- CBSE Class11 Maths Notes 13 Limits and DerivativesDokumen7 halamanCBSE Class11 Maths Notes 13 Limits and DerivativesRoy0% (1)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Ramin Shamshiri Risk Analysis Exam2 PDFDokumen8 halamanRamin Shamshiri Risk Analysis Exam2 PDFRedmond R. ShamshiriBelum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Exercise On Relative ClausesDokumen5 halamanExercise On Relative ClausesSAmuel QuinteroBelum ada peringkat
- De Villa vs. Court of AppealsDokumen1 halamanDe Villa vs. Court of AppealsValerie Aileen AnceroBelum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- LESSON 1: What Is Social Studies?: ObjectivesDokumen15 halamanLESSON 1: What Is Social Studies?: ObjectivesRexson Dela Cruz Taguba100% (1)
- ABC of Effective WritingDokumen4 halamanABC of Effective Writingprada85Belum ada peringkat
- D78846GC20 sg2Dokumen356 halamanD78846GC20 sg2hilordBelum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- What Is Art?Dokumen14 halamanWhat Is Art?Sarvenaaz QaffariBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Theory of Interpersonal RelationsDokumen2 halamanTheory of Interpersonal RelationsAra Gayares Gallo100% (1)
- Chapter 1Dokumen16 halamanChapter 1MulugetaBelum ada peringkat
- (These Are Taken From The Hics Infectious Disease Incident Response Guide Available atDokumen2 halaman(These Are Taken From The Hics Infectious Disease Incident Response Guide Available atDavid MitchellBelum ada peringkat
- Electronic Check ProcessingDokumen1 halamanElectronic Check Processingaaes2Belum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- 5909 East Kaviland AvenueDokumen1 halaman5909 East Kaviland Avenueapi-309853346Belum ada peringkat
- Lee Gwan Cheung Resume WeeblyDokumen1 halamanLee Gwan Cheung Resume Weeblyapi-445443446Belum ada peringkat
- Far 1 - Activity 1 - Sept. 09, 2020 - Answer SheetDokumen4 halamanFar 1 - Activity 1 - Sept. 09, 2020 - Answer SheetAnonn100% (1)
- History Paper 2 IB Study GuideDokumen6 halamanHistory Paper 2 IB Study Guidersuresh1995100% (4)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)