Retained Placenta
Diunggah oleh
Deddy AngHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Retained Placenta
Diunggah oleh
Deddy AngHak Cipta:
Format Tersedia
83
Agrawal A et al
Health Renaissance 2013; Vol. 11 No.1; 83-85
Retained placenta in patient with valvular heart disease
__________________________________________________
Address for correspondence
Dr Ajay Agrawal
Department of Gynecology and Obstetrics
BPKIHS, Dharan, Nepal
Email: drajayagrawal@yahoo.com
Case Report
Management of retained placenta in patient with valvular heart disease
with pulmonary edema
A Agrawal
1
, A Thakur
1
,
P Rijal
1
, P Basnet
1
, A Ghimire
2
, DK Uprety
1
1
Department of Gynecology and Obstetrics, BPKIHS, Dharan, Nepal
2
Department of Aesthesiology and Critical Care Medicine, BPKIHS, Dharan, Nepal
Abstract
A case of retained placenta following full-term vaginal delivery with an unscarred uterus
where surgical management of delivering the placenta was not attempted due to unfavorable
cardiac condition is presented. Although she was planned for hysterectomy, she was
successfully managed medically with injection methotrexate.
Introduction
Retained placentas affect 0.5%3% of women
following delivery, and is a major cause of maternal
death from postpartum haemorrhage (PPH) and
puerperal sepsis.
1, 2
After uterine atony, retained
placenta is the second major indication for blood
transfusion in the third stage of labour
3
. Independent
risk factors associated with retained placenta include
non-use of antenatal care, previous retained placenta,
previous caesarean section, maternal age 35 years
or more, grand multiparity, previous dilatation and
curettage, preterm delivery and placenta weight less
than 501 gm.
4
The ensuing complications may
include- severe post-partum haemorrhage with its
resultant coagulopathy, postpartum curettage, uterine
perforation, shock, infection, loss of fertility and even
death. The conventional treatment is manual removal
of placenta (MRP) under general anaesthesia(GA)
followed by hysterectomy if it fails. Not only does
this approach preclude future fertility, but it is also a
procedure synonymous with significant perioperative
risks. For women who wish to conserve their
reproductive function, other treatment options have
been described. In some settings, uterine conservation
(with the placenta left in situ) may be an alternative
strategy.
58
Adjuvant therapy with methotrexate has
also been used to expedite resorption of placental
tissue.
68
Case report
A lady, 21 years P
1
L
1
, reported at BPKIHS, 16
hours following vaginal delivery, with retained
placenta after failed attempt of MRP. She was
conscious, with normal vital signs, moderately pale,
with a diastolic murmur at aortic area. Uterus was
20-22 weeks size, well contracted with pelvic
examination showing moderate amount of bleeding
with patulous but closed cervical os and cord hanging
out of vagina
Her investigations read hemoglobin 10.9gm/dl, total
and differential counts within normal limits, with
normal readings of routine urine analysis, platelet
count, coagulation profile, hepatic and renal function
tests. There was prolonged QT interval and T wave
inversion in electrocardiography. Echocardiography
showed concentric left ventricular hypertrophy,
severe aortic stenosis, severe aortic regurgitation,
mild mitral regurgitation and tricuspid thickened AV
leaflets without pulmonary artery hypertension with
ejection fraction of 60%.
On 4th post partum day, she was planned for MRP.
However, before GA, after inserting epidural catheter
she developed severe pulmonary edema. MRP was
postponed and she was shifted to maternal intensive
care unit (MICU) for further management.
Considering the desire of the patient for retaining
her uterus, conservative management was planned.
84
Agrawal A et al
Health Renaissance 2013; Vol. 11 No.1; 83-85
Retained placenta in patient with valvular heart disease
On sixth postpartum day transabdominal sonography
revealed uterus of post partum size with endometrial
cavity showing an echogenic mass of dimensions
9.8cm x 8cm x 7cm, suggestive of placenta, with
vascularity on colour doppler confirming it to be
adherent to the uterine wall (placenta accreta), but
with no definite invasion (figure 1). Modality adopted
was: placenta left in-situ and injection methotrexate
given intramuscularly in the schedule of 1 mg/kg body
weight, weekly. Complete blood counts, liver and
renal function tests were done before giving each
dose of methotrexate which remained within limits.
Injection folinic acid 0.1 milligram per kilogram body
weight was given twenty-four hours after
methotrexate.
uterus, after 18 days of hospitalization. On subsequent
follow-ups, for one month, patient remained afebrile
with no evidence of infection, and normal sonographic
and colour doppler findings after a fortnight.
Discussion
Presently, the only effective treatment of retained
placenta is MRP under GA. The role of systemic
oxytocics in the management of retained placentas
is controversial. Oxytocics given prophylactically at
the time of delivery increase the number of placental
deliveries at 20 and 40 minutes but have no effect
on the number of placentas that eventually need
manual removal
9
.Injection of oxytocin into the
umbilical vein has been suggested as an alternative.
Despite several placebo controlled trials of this
technique, no firm conclusions have been reached
regarding its efficacy.
10
Methotrexate has also been described an as adjuvant
therapy for the conservative management of placenta
accrete.
58, 11
It has been hypothesized that
methotrexate acts by inducing placental necrosis and
expediting a more rapid involution of the placenta
12
.
This contradicts the belief that methotrexate acts
only on rapidly dividing cells, given that trophoblast
proliferation is not felt to occur at term
13
. Thus, there
is controversy as to the effectiveness of methotrexate
as an adjuvant treatment. Also, there is a lack of
consensus regarding optimal dosing, frequency, or
route of administration. Dose in this particular case
was weekly 1 mg/kg body weight. In a recent review,
conservative management was utilized in 167 cases
of placenta accreta/percreta
14
.The failure rate was
22% and hysterectomy, either primary or delayed,
was required mostly for severe hemorrhage. Severe
maternal morbidity, including one maternal death,
occurred in 6% of cases. The death was attributed
to aplasia and nephrotoxicity secondary to
intraumbilical administration of methotrexate. This
case highlights the adverse effects that may occur
following even a single dose of adjuvant methotrexate.
Although conservative management of placenta
accrete appears to be successful at preventing
hysterectomy in most cases, there is still potential
for morbidity. If such an approach is used, intensive
monitoring for complications is required. Women may
continue to be at risk for weeks to months after
delivery. Sentilhes et al. reported a median period to
delayed hysterectomy of 22 weeks.
14
Figure 1: Placenta accreta
First dose of methotrexate was given on 6
th
post-
partum day after which she passed brownish vaginal
discharge along with bits of tissue. Broad spectrum
antibiotics and antiseptic vaginal douching was
continued. Size of the uterus decreased remarkably
and on 9
th
postpartum day it was 14-16 week size. 0n
13
th
day second dose was given and her trans-
abdominal sonography was repeated which revealed
decrease in placental size. However on 16
th
postpartum day, at night she started to have moderate
amount of vaginal bleeding, she was tachycadiac, with
normal blood pressure without evidence of pulmonary
edema. On abdominal examination, uterus was 14
weeks size, well contracted with pelvic examination
showing moderate amount of bleeding per vaginum
with patulous cervical os about two cm dilated. She
was planned for dilation and evacuation under
paracervical block which was successfully performed
and about 150gm of placental chunk was removed.
With this conservative strategy, vaginal bleeding
never became alarming and vaginal discharge never
purulent. Patient was discharged in a satisfactory
condition, fulfilling her initial desire of conserving the
85
Agrawal A et al
Health Renaissance 2013; Vol. 11 No.1; 83-85
Retained placenta in patient with valvular heart disease
Another controversy surrounding the use of
methotrexate in the management of placenta accreta
has been the utility of monitoring serum hCG. The
prognostic implications of decreasing hCG levels
following administration of methotrexate are better
described in the setting of ectopic pregnancy. For
placenta accrete, it is not clear whether decreasing
levels correlate with the rate of involution of placental
tissue. In one study, the serum hCG levels decreased
with a half-life of 5.2 days in women managed by
leaving the placenta in situ and did not vary with the
volume of remaining tissue.
15
So it was not monitored
in our patient.
Conclusion
Our case demonstrates, conservative treatment of
persistent retained placenta can be successful. This
could have important public health implications where
facilities for manual removal are scarce or when
medical conditions of patient do not favor MRP under
GA. If an improvement in the conservative
management of placenta can be achieved, then
medical management of the retained placenta will
become the treatment of choice, even where theatre
facilities are available.
References
1. MacLeod J, Rhode R. Retrospective follow-up
of maternal deaths and their associated risk
factors in a rural district of Tanzania. Trop Med
Int Health 1998; 3:130-7.
2. Etuk SJ, Asuquo EE. Maternal mortality following
post-partum haemorrhage in Calabar a 6-year
review. West Afr J Med 1997;16:165-9.
3. Kamani, AA, McMorland GA, Wadsworth LD.
Utilization of red blood transfusion in an obstetric
setting. Am J Obstet Gynecol 1988; 159:1177-
1181.
4. Owolabi AT, Dare FO, Fasubaa OB, Ogunlola
IO, Kuti O, Bisiriyu LA. Risk factors for retained
placenta in southwestern Nigeria. Singapore Med
J 2008; 49(7): 532-537.
5. S. Y. P. Tong, K. H. Tay, and Y. C. K. Kwek,
Conservative management of placenta accreta:
review of three cases, Singapore Medical
Journal, vol. 49, no. 6, pp. e156e159, 2008.
6. S. Timmermans, A. C. Van Hof, and J. J.
Duvekot, Conservative management of
abnormally invasive placentation, Obstetrical
and Gynecological Survey, vol. 62, no. 8, pp. 529
539, 2007.
7. G. Kayem, C. Davy, F.Goffinet, C. Thomas,D.
Clement, andD. Cabrol, Conservative versus
extirpative management in cases of placenta
accreta, Obstetrics and Gynecology, vol. 104,
no. 3, pp. 531536, 2004.
8. F. Bretelle, B. Courbiere, C. Mazouni et al.,
Management of placenta accreta: morbidity and
outcome, European Journal of Obstetrics
Gynecology and Reproductive Biology, vol. 133,
no. 1, pp. 3439, 2007.
9. Prendivllle WJ, Elbourne D, McDonald S. Active
versus expectant management of the third stage
of labour (Cochrane Review). In :The Cochrane
Library, Issue 3. Update Software, Oxford, 1998.
10. Pipingas A, Hofmeyr GJ, Sese I KR. Umbilical
vessel oxytocin administration for retained
placenta: in-vitro study of various Infusion
techniques. Am J Obstet Gynecol 1993;168:793-
795.
11. Y. Oyelese and J. C. Smulian, Placenta previa,
placenta accreta, and vasa previa, Obstetrics
and Gynecology, vol. 107, no. 4, pp. 927941,
2006.
12. S. Arulkumaran, C. S. A. Ng, I. Ingemarsson,
and S. S. Ratnam, Medical treatment of
placenta accreta with methotrexate, Acta
Obstetricia et Gynecologica Scandinavica, vol.
65, no. 3, pp. 285286, 1986.
13. M. Winick, A. Coscia, and A. Noble, Cellular
growth in human placenta. I. Normal placental
growth, Pediatrics, vol. 39, no. 2, pp. 248251,
1967.
14. L. Sentilhes, C. Ambroselli, G. Kayem et al.,
Maternal outcome after conservative treatment
of placenta accreta, Obstetrics and Gynecology,
vol. 115, no. 3, pp. 526534, 2010.
15. N. Matsumura, T. Inoue, M. Fukuoka, N.
Sagawa, and S. Fujii, Changes in the serum
levels of human chorionic gonadotropin and the
pulsatility index of uterine arteries during
conservative management of retained adherent
placenta, Journal of Obstetrics and
Gynaecology Research, vol. 26, no. 2, pp. 81
87, 2000.
Anda mungkin juga menyukai
- Pituitary Tumors: A Clinical CasebookDari EverandPituitary Tumors: A Clinical CasebookLisa B. NachtigallBelum ada peringkat
- Conservative Management of Placenta Accreta in A Multiparous WomanDokumen10 halamanConservative Management of Placenta Accreta in A Multiparous WomanRobel Mae Lagos MontañoBelum ada peringkat
- Placenta Percreta Dan Ligasi Arteri Internal IlliakaDokumen4 halamanPlacenta Percreta Dan Ligasi Arteri Internal IlliakaNyoman TapayanaBelum ada peringkat
- A Cornual Ectopic Pregnancy Case: Diagnosis, Etiology and Its ManagementDokumen5 halamanA Cornual Ectopic Pregnancy Case: Diagnosis, Etiology and Its ManagementparkfishyBelum ada peringkat
- Gynecology and Minimally Invasive Therapy: Shahul Hameed Mohamed Siraj, Bernard Su Min ChernDokumen3 halamanGynecology and Minimally Invasive Therapy: Shahul Hameed Mohamed Siraj, Bernard Su Min ChernIrvin MarcelBelum ada peringkat
- Uterine AtonyDokumen4 halamanUterine AtonyJohn Cenas100% (1)
- Adenomyosis Excision Followed by Successful Live Birth After Three Consecutive IVFDokumen5 halamanAdenomyosis Excision Followed by Successful Live Birth After Three Consecutive IVFPyuzz RemakeBelum ada peringkat
- AkretaDokumen7 halamanAkretaInna SeraLaratBelum ada peringkat
- Anesthetic implications of uterine rupture in a primigravid patientDokumen4 halamanAnesthetic implications of uterine rupture in a primigravid patientYahia AhmadBelum ada peringkat
- A Rare Case of Morbidly Adherent Placenta in A Young - 2024 - International JouDokumen4 halamanA Rare Case of Morbidly Adherent Placenta in A Young - 2024 - International JouRonald QuezadaBelum ada peringkat
- RM 08008Dokumen6 halamanRM 08008Manoj ChoudharyBelum ada peringkat
- Early Pregnancy Problems: Presented byDokumen28 halamanEarly Pregnancy Problems: Presented byMalk OmryBelum ada peringkat
- Ojog 2013020415273326Dokumen6 halamanOjog 2013020415273326Achmad Safi'iBelum ada peringkat
- Cesarean Scar Ectopic Pregnancy Case ReportDokumen6 halamanCesarean Scar Ectopic Pregnancy Case ReportMominah MayamBelum ada peringkat
- Cesarean Scar Pregnancies and Their ManagementDokumen7 halamanCesarean Scar Pregnancies and Their ManagementClinton SitanggangBelum ada peringkat
- New Options for Managing Adherent PlacentaDokumen6 halamanNew Options for Managing Adherent PlacentaAngelique Ramos PascuaBelum ada peringkat
- Managment of Scar PregnancyDokumen43 halamanManagment of Scar Pregnancyvacha sardarBelum ada peringkat
- Minakshi S. Neglected Puerperal Inversion of The Uterus Ignorance Makes Acute A Chronic FormDokumen4 halamanMinakshi S. Neglected Puerperal Inversion of The Uterus Ignorance Makes Acute A Chronic FormJulius Albert SBelum ada peringkat
- An Interesting Case of Intramyometrial Pregnancy: Rare DiseaseDokumen5 halamanAn Interesting Case of Intramyometrial Pregnancy: Rare DiseaseDinorah MarcelaBelum ada peringkat
- Yan 2007Dokumen3 halamanYan 2007Agustin LindaBelum ada peringkat
- JurnalDokumen4 halamanJurnalMigumi YoshugaraBelum ada peringkat
- CCD - Ectopic Pregnancy HafyzDokumen29 halamanCCD - Ectopic Pregnancy HafyzHanif GandohBelum ada peringkat
- Ectopic Pregnancy: Causes, Symptoms and Treatment OptionsDokumen12 halamanEctopic Pregnancy: Causes, Symptoms and Treatment OptionsAnni BarbaBelum ada peringkat
- 10 1016@j Ijscr 2020 01 020Dokumen4 halaman10 1016@j Ijscr 2020 01 020ari naBelum ada peringkat
- Practice Bulletin: Medical Management of Ectopic PregnancyDokumen7 halamanPractice Bulletin: Medical Management of Ectopic PregnancyChangBelum ada peringkat
- Placenta Previa 1Dokumen2 halamanPlacenta Previa 1Gunther MirandaBelum ada peringkat
- Laparoscopy During PregnancyDokumen6 halamanLaparoscopy During PregnancyTrần Ngọc TúBelum ada peringkat
- Blighted Ovum: A Case ReportDokumen2 halamanBlighted Ovum: A Case Reportakhmad ikhwanBelum ada peringkat
- Ectopic Pregnancy Diagnosis and TreatmentDokumen39 halamanEctopic Pregnancy Diagnosis and TreatmentFecky Fihayatul IchsanBelum ada peringkat
- Endometrial Adenocarcinoma and Polycystic Ovary Syndrome: Risk Factors, Management, and PrognosisDokumen4 halamanEndometrial Adenocarcinoma and Polycystic Ovary Syndrome: Risk Factors, Management, and PrognosisDikie MustofadijayaBelum ada peringkat
- Clinical Study: Nitroglycerin For Management of Retained Placenta: A Multicenter StudyDokumen7 halamanClinical Study: Nitroglycerin For Management of Retained Placenta: A Multicenter StudyTri Anna FitrianiBelum ada peringkat
- Effectiveness of Per Rectal Misoprostol Versus Intramuscular Oxytocin For Prevention of Primary Postpartum HaemorrhageDokumen5 halamanEffectiveness of Per Rectal Misoprostol Versus Intramuscular Oxytocin For Prevention of Primary Postpartum HaemorrhageFuad HasanBelum ada peringkat
- Artículo Nefro 2Dokumen6 halamanArtículo Nefro 2Stephani RobinsonBelum ada peringkat
- An Alternative To Hysterectomy: Manchester RepairDokumen0 halamanAn Alternative To Hysterectomy: Manchester RepairDwi WicaksonoBelum ada peringkat
- Hemorragia y EmbrazoDokumen6 halamanHemorragia y Embrazoana catalinaBelum ada peringkat
- Conservative Management of Ectopic Pregnancy: A Provincial Hospital Case Series of Medically Managed Ectopic PregnanciesDokumen5 halamanConservative Management of Ectopic Pregnancy: A Provincial Hospital Case Series of Medically Managed Ectopic PregnanciesSandy JusiBelum ada peringkat
- Imafuku 2019Dokumen5 halamanImafuku 2019Rizki FebriyaniBelum ada peringkat
- Hetero TopicDokumen3 halamanHetero TopicDONNYBelum ada peringkat
- tmp7DB6 TMPDokumen78 halamantmp7DB6 TMPFrontiersBelum ada peringkat
- Clinical Presentation of Ectopic Pregnancy Turned Out to Be Ectopic PregnancyDokumen33 halamanClinical Presentation of Ectopic Pregnancy Turned Out to Be Ectopic PregnancyRosiBelum ada peringkat
- Willmott Et Al-2008-BJOG An International Journal of Obstetrics & GynaecologyDokumen3 halamanWillmott Et Al-2008-BJOG An International Journal of Obstetrics & GynaecologyganangahimsaBelum ada peringkat
- Best modality for diagnosing ectopic pregnancyDokumen31 halamanBest modality for diagnosing ectopic pregnancyantonio91uBelum ada peringkat
- Acute Abdomen in PregnancyDokumen6 halamanAcute Abdomen in PregnancydkasisBelum ada peringkat
- Managing Placenta Accreta: Medical vs Surgical OptionsDokumen9 halamanManaging Placenta Accreta: Medical vs Surgical OptionsAslesa Wangpathi PagehgiriBelum ada peringkat
- Mifepristone and Misoprostol For Early Pregnancy Failure: A Cohort AnalysisDokumen6 halamanMifepristone and Misoprostol For Early Pregnancy Failure: A Cohort AnalysisBobby SetiawanBelum ada peringkat
- Embarazo EctópicoDokumen7 halamanEmbarazo EctópicomariBelum ada peringkat
- Nama: Zaimah Shalsabilla Kelas: Alpha NIM: 04011181520071Dokumen11 halamanNama: Zaimah Shalsabilla Kelas: Alpha NIM: 04011181520071shalsaBelum ada peringkat
- W 3 e WDDokumen6 halamanW 3 e WDsupaidi97Belum ada peringkat
- UC Irvine: Clinical Practice and Cases in Emergency MedicineDokumen6 halamanUC Irvine: Clinical Practice and Cases in Emergency MedicinePatrick NunsioBelum ada peringkat
- Journal Gyn KETDokumen8 halamanJournal Gyn KETImaylani S. SitanggangBelum ada peringkat
- Uterine Inversion: A Life-Threatening Obstetric Emergency: Dawn R. Hostetler, MD, and Michael Bosworth, DODokumen4 halamanUterine Inversion: A Life-Threatening Obstetric Emergency: Dawn R. Hostetler, MD, and Michael Bosworth, DOAndi Farras WatyBelum ada peringkat
- 1 s2.0 S2211419X13000578 MainDokumen4 halaman1 s2.0 S2211419X13000578 Mainindra040293Belum ada peringkat
- Csii-Pregnancy in Patients With Mechanical Prosthetic ValvesDokumen6 halamanCsii-Pregnancy in Patients With Mechanical Prosthetic Valvesapi-205989841Belum ada peringkat
- Hioerplasia Mamaria GestacionalDokumen9 halamanHioerplasia Mamaria GestacionalOctavio LeyvaBelum ada peringkat
- Aderoba 2016Dokumen8 halamanAderoba 2016DONNYBelum ada peringkat
- Uog 14728Dokumen25 halamanUog 14728Stanley PhanBelum ada peringkat
- Women's Health Case: Methotrexate vs Laparoscopic SalpingostomyDokumen9 halamanWomen's Health Case: Methotrexate vs Laparoscopic SalpingostomyWong Chui YeeBelum ada peringkat
- tmpC705 TMPDokumen3 halamantmpC705 TMPFrontiersBelum ada peringkat
- tmpB9EA TMPDokumen3 halamantmpB9EA TMPFrontiersBelum ada peringkat
- Tugas English Lesson 12-14 FIXDokumen1 halamanTugas English Lesson 12-14 FIXDeddy AngBelum ada peringkat
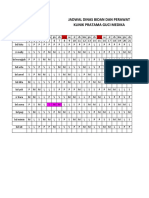
- Jadwal Dinas Bidan Dan Perawat Klinik Pratama Guci MedikaDokumen5 halamanJadwal Dinas Bidan Dan Perawat Klinik Pratama Guci MedikaDeddy AngBelum ada peringkat
- AdvBiomedRes2120-8335885 230918Dokumen4 halamanAdvBiomedRes2120-8335885 230918Deddy AngBelum ada peringkat
- Acute Necrotizing Ulcerative GingivitisDokumen9 halamanAcute Necrotizing Ulcerative GingivitisDeddy AngBelum ada peringkat
- Daftar PustakaDokumen3 halamanDaftar PustakaDeddy AngBelum ada peringkat
- Presentation1 DaraDokumen20 halamanPresentation1 DaraDeddy AngBelum ada peringkat
- LTE EPC Technical OverviewDokumen320 halamanLTE EPC Technical OverviewCristian GuleiBelum ada peringkat
- 3GPP TS 36.306Dokumen131 halaman3GPP TS 36.306Tuan DaoBelum ada peringkat
- Theoretical and Actual CombustionDokumen14 halamanTheoretical and Actual CombustionErma Sulistyo R100% (1)
- Project Binder 2Dokumen23 halamanProject Binder 2Singh DhirendraBelum ada peringkat
- TIA Selection Tool: Release Notes V2022.05Dokumen10 halamanTIA Selection Tool: Release Notes V2022.05Patil Amol PandurangBelum ada peringkat
- Datasheet PDFDokumen6 halamanDatasheet PDFAhmed ElShoraBelum ada peringkat
- Flowing Gas Material BalanceDokumen4 halamanFlowing Gas Material BalanceVladimir PriescuBelum ada peringkat
- Sradham ChecklistDokumen9 halamanSradham ChecklistpswaminathanBelum ada peringkat
- Religion in Space Science FictionDokumen23 halamanReligion in Space Science FictionjasonbattBelum ada peringkat
- Emerson EPC48150 1800 FA1EPC48300 3200 FA1 V PDFDokumen26 halamanEmerson EPC48150 1800 FA1EPC48300 3200 FA1 V PDFRicardo Andrés Soto Salinas RassBelum ada peringkat
- A Fossil Hunting Guide To The Tertiary Formations of Qatar, Middle-EastDokumen82 halamanA Fossil Hunting Guide To The Tertiary Formations of Qatar, Middle-EastJacques LeBlanc100% (18)
- Survey Report on Status of Chemical and Microbiological Laboratories in NepalDokumen38 halamanSurvey Report on Status of Chemical and Microbiological Laboratories in NepalGautam0% (1)
- Reflection 2: WHAT DOES It Mean To Be A Pacific Islander Today and in The Future To Me?Dokumen5 halamanReflection 2: WHAT DOES It Mean To Be A Pacific Islander Today and in The Future To Me?Trishika NamrataBelum ada peringkat
- 1989 GMC Light Duty Truck Fuel and Emissions Including Driveability PDFDokumen274 halaman1989 GMC Light Duty Truck Fuel and Emissions Including Driveability PDFRobert Klitzing100% (1)
- Tds G. Beslux Komplex Alfa II (25.10.19)Dokumen3 halamanTds G. Beslux Komplex Alfa II (25.10.19)Iulian BarbuBelum ada peringkat
- 7890 Parts-Guide APDokumen4 halaman7890 Parts-Guide APZia HaqBelum ada peringkat
- Fundermax Exterior Technic 2011gb WebDokumen88 halamanFundermax Exterior Technic 2011gb WebarchpavlovicBelum ada peringkat
- g4 - Stress Analysis of Operating Gas Pipeline Installed by HorizontalDokumen144 halamang4 - Stress Analysis of Operating Gas Pipeline Installed by HorizontalDevin DickenBelum ada peringkat
- Reflective Essay 4Dokumen1 halamanReflective Essay 4Thirdy AngelesBelum ada peringkat
- 1.2 - Sewing Machine and Special AttachmentsDokumen3 halaman1.2 - Sewing Machine and Special Attachmentsmaya_muth0% (1)
- Are Hypomineralized Primary Molars and Canines Associated With Molar-Incisor HypomineralizationDokumen5 halamanAre Hypomineralized Primary Molars and Canines Associated With Molar-Incisor HypomineralizationDr Chevyndra100% (1)
- Daftar Spesifikasi Teknis Pembangunan Gedung Kantor BPN BojonegoroDokumen6 halamanDaftar Spesifikasi Teknis Pembangunan Gedung Kantor BPN BojonegoroIrwin DarmansyahBelum ada peringkat
- Telco XPOL MIMO Industrial Class Solid Dish AntennaDokumen4 halamanTelco XPOL MIMO Industrial Class Solid Dish AntennaOmar PerezBelum ada peringkat
- WOOD Investor Presentation 3Q21Dokumen65 halamanWOOD Investor Presentation 3Q21Koko HadiwanaBelum ada peringkat
- Organizing Small Items with Glass Bottle OrganizersDokumen70 halamanOrganizing Small Items with Glass Bottle OrganizersDy SaiBelum ada peringkat
- A Compilation of Thread Size InformationDokumen9 halamanA Compilation of Thread Size Informationdim059100% (2)
- CP 343-1Dokumen23 halamanCP 343-1Yahya AdamBelum ada peringkat
- BCP-8000 User's ManualDokumen36 halamanBCP-8000 User's ManualAsad PatelBelum ada peringkat
- Baseline Program Rev 3A Presentation 25 July 2020Dokumen24 halamanBaseline Program Rev 3A Presentation 25 July 2020Shakti Sourava RautrayaBelum ada peringkat
- ML AiDokumen2 halamanML AiSUYASH SHARTHIBelum ada peringkat