Acute Viral Hepatitis B Anggita Nur Aziza
Diunggah oleh
Anggita Nur Aziza0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
27 tayangan28 halamanThis document describes a case of a 45-year-old male patient presenting with acute viral hepatitis B. The patient reports pain in the upper right abdomen, fever, nausea, vomiting, back and leg pain, loss of appetite, weight loss, and shortness of breath. A physical exam finds hepatomegaly and splenomegaly. Laboratory tests show elevated liver enzymes and the presence of HBsAg, consistent with acute hepatitis B. The patient is given IV fluids and medications to manage symptoms as the viral infection runs its course.
Deskripsi Asli:
Hepatitis B
Judul Asli
CASE 1
Hak Cipta
© © All Rights Reserved
Format Tersedia
PPT, PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniThis document describes a case of a 45-year-old male patient presenting with acute viral hepatitis B. The patient reports pain in the upper right abdomen, fever, nausea, vomiting, back and leg pain, loss of appetite, weight loss, and shortness of breath. A physical exam finds hepatomegaly and splenomegaly. Laboratory tests show elevated liver enzymes and the presence of HBsAg, consistent with acute hepatitis B. The patient is given IV fluids and medications to manage symptoms as the viral infection runs its course.
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PPT, PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
27 tayangan28 halamanAcute Viral Hepatitis B Anggita Nur Aziza
Diunggah oleh
Anggita Nur AzizaThis document describes a case of a 45-year-old male patient presenting with acute viral hepatitis B. The patient reports pain in the upper right abdomen, fever, nausea, vomiting, back and leg pain, loss of appetite, weight loss, and shortness of breath. A physical exam finds hepatomegaly and splenomegaly. Laboratory tests show elevated liver enzymes and the presence of HBsAg, consistent with acute hepatitis B. The patient is given IV fluids and medications to manage symptoms as the viral infection runs its course.
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PPT, PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 28
ACUTE VIRAL HEPATITIS B
Anggita Nur Aziza
*
*
Name : Mr. Y
Age : 45 y.o
Sex : Male
Address : Sukajaya Kampung
Pinayungan RT 14 RW 06
Kecamatan Teluk Jambe Timur
Kabupaten Karawang
Occupation : Computer Labour
Religion : Muslim
Marital status : Married
Date of addmision : October 23
rd
2011
Taken from : Rengasdengklok
Pain in upper right abdomen
since 2 days before
hospitalized
Chief
complaint
Fever
Nausea and vomitting
Aches from back waist to
feet
Hasnt been defecated for 2
days
Additional
complaint
*
*Patient came with pain in upper right abdomen
since 2 days before hospitalized. It felt sharp,
continously, not radiating and day by day is
getting worse especially when the patient lying
down.
*Beside the pain, the patient also felt aches
from back waist to feet, nausea and vomitting,
and fever.
*Fever starts from 2 days before hospitalized, intermittent.
*Nausea and vomitting starts from 2 days before hospitalized,
vomitted about 2 times, food in its contain, blood (-)
*The aches from back waist felt since 1 days before
hospitalized, sharp, continously, worsened when the patient
is walking and sit down.
*Theres no pain and no dripping when he is urinating. The
patient hasnt been defecated since 2 days before
hospitalized. He also loss his appetite and loss weight since a
month ago.
*Dizziness, fatigue, cough, pain in chest are denied.
*Lately, patient said that the pain in abdomen and back waist
is decreased. But the patient feel shortness of breath since
last night, and swollen in his feet.
*
Same
condition (+)
Hypertension
(-)
Diabetes
mellitus (-)
Cardiovasular
(-)
Kidney (-) Allergy (-)
*
Same
condition (-)
Hypertension
(-)
Diabetes
mellitus (-)
Cardiovasular
(-)
Kidney (-) Allergy (-)
Had gone to puskesmas
2 days before
hospitalized and get
medicated
Herbal medicine (-)
Blood transfusion (+)
PAST MEDICAL
HISTORY
*
Smoke (-)
Alcohol (-
)
Tattoo (-)
Free sex
(-)
Narcotics
(-)
Injection
drugs (-)
He didnt
exercise
regularly
*
Severely ill
General
appearance
Compos
mentis
Conciousness
Vital
Sign
BP:
130/70
mmHg
RR:
24x/min
Temp:
37,5
0
c
HR:
120x/min
*
Head
Normocephaly
Eyes
Conjunctiva anemic -/-
Sclera icteric -/-
Ears
Normotia
Secret -/-
Serumen -/-
Nose
Sepeum deviation -
Secret -/-
Concha normal
Mouth
Dirty mouth -
Dry mouth -
Dry tongue -
Throat
Tonsils T1/T1
Faring hiperemis (-)
Neck
Lymph gland is not palpable
Thyroid gland is not palpable
JVP 5+2 cm
Inspection:
Symmetrical
Palpation:
Equal vocal fremitus
Percusion:
Sonor in both lung
Auscultation:
Vesicular breath sound in both
lung, no ronchi and wheezing
Inspection:
Ictus cordis is invisible, spider
nevi (-)
Palpation:
Ictus cordis is palpable at 5
th
ICS
LMCS
Percution:
no enlargment
Auscultation:
Regular I - II heart sound no
murmur and gallop
*
*
Inspection
Brown skin, bulging abdomen, icteric (-), caput meducae (-)
Palpation
Pain present on palpation at right hypochondrium region
Liver palpable 3 fingers under arcus costae, soft consistency, sharp
edge, flat surface, tenderness (-)
Spleen palpable at Schuffner 4, soft consistency, sharp edge, flat
surface, tenderness (-)
Shifting dullness (-)
Percussion
No pain present on abdominal percussion
Dullness
CVA (-)
Auscultation
Bowel sound (+). Arterial bruit (-), venous hum (-)
*
*Warm acrals
*Oedema
+ +
+ +
+ -
+ +
*
October 23rd 2011 Patient result Normal range
Hb 8.00 % 12 17 g%
Leukocyte 5.100/uL 5000-10.000/uL
Trombocyte 227.000 150.000-450.000
Ht 24 % 37-48 %
HbsAg + -
GDS 105 mg/dl 80-140 mg/dl
Ureum 66,2 mg/dl 10-45 mg/dl
Creatinine 1.39 mg/dl 0.4-1.5 mg/dl
Albumin 3,10 3.5-5.0 mg %
SGOT 56 < 40 u/l
SGPT 36 < 40 u/l
*
October 24th 2011 Patient result Normal range
Protein total 6,05 mg% 6.5 8.5 mg%
Albumin 3,22 mg% 3.5 5 mg%
Globulin 2,83 mg% 2.6 3.6 mg%
Total Bilirubin 0,68 mg/dl < 1.1 mg/dl
Direct Bilirubin 0,37 mg/dl < 0.6 mg/dl
Indirect Bilirubin 0,31 mg/dl < 0.5 mg/dl
SGOT 650 u/l < 40 u/l
SGPT 429 u/l < 40 u/l
*
October 25th
2011
Patient result Normal range
Ureum 33.3 10-45 mg/dl
Creatinin 1.30 0.4-1.5 mg/dl
*
Symptoms Signs Laboratory and others
Pain in upper right
abdomen
Fever
Nausea and vomitting
Aches form back waist
untill feet
Hasnt been defecated
for 2 days
Loss of appetite
Weight loss
Shortness of breath
Swollen in feet
Vital sign:
BP: 130/70 mmHg
HR: 120 x/min
RR: 24 x/min
T: 37.5
0
c
Abdomen:
Bulging abdomen
Hepatomegali and
splenomegali
sounds dull
Hb: 8.0 g%
Ht: 24 %
HbsAg: +
Ureum: 69 mg/dl
Creatinine: 1.94 mg/dl
Protein total : 6.05 %
Albumin: 3.10 mg%
Globulin: 2.83 mg%
Total bilirubin: 0.68 mg/dl
Direct bilirubin: 0.37
mg/dl
Indirect bilirubin: 0.31
mg/dl
SGOT: 650 u/l
SGPT: 429 u/l
*
1. Acute viral hepatitis B
2. Chronic hepatitis B
3. Acute non viral hepatitis B
4. Cirrhosis hepatis
5. Cholelithiasis
*
Acute viral hepatitis B
*
*Imunoserologic examination
*USG
*Urinalysis
*Liver biopsy
*
*IVFD RL 20 tpm
*IVFD Aminofusin hepar
*Ranitidin 2 x 1 amp
*Curcuma 3 x 1 tab
*Meloxicam 1 x 15 mg
*Alprazolam 1 x 0.5 mg
*Neurodex 2 x 1 tab
*Laxadin 2 x C II
*
Ad
fungsionam
: dubia ad
malam
Ad sanationam
: dubia ad
malam
Ad vitam :
dubia ad
bonam
Anda mungkin juga menyukai
- How I Use The Evidence in Dysphagia Management (2) : A Question of TasteDokumen3 halamanHow I Use The Evidence in Dysphagia Management (2) : A Question of TasteSpeech & Language Therapy in Practice100% (3)
- Acu-Stim For RecoveryDokumen4 halamanAcu-Stim For Recoverycare_e_genBelum ada peringkat
- 2714 - Peripheral Venous Catheter Care Policy For AdultsDokumen10 halaman2714 - Peripheral Venous Catheter Care Policy For AdultssofiinhaptBelum ada peringkat
- American Board of Family Medicine: TTT SAMPLE TTTDokumen148 halamanAmerican Board of Family Medicine: TTT SAMPLE TTTAbdulrhman AlruwiliBelum ada peringkat
- Assisting Arterial Blood Gas: Lesson PlanDokumen2 halamanAssisting Arterial Blood Gas: Lesson PlanSwapnil MahapureBelum ada peringkat
- Focus Diagnosis Action Response Subjective: "I Hate Water and I Don't Drink It Much " DXDokumen2 halamanFocus Diagnosis Action Response Subjective: "I Hate Water and I Don't Drink It Much " DXGrape Juice100% (1)
- Amc Recall 2Dokumen18 halamanAmc Recall 2vivekmoBelum ada peringkat
- DMDFDokumen22 halamanDMDFsujal177402100% (1)
- Duty Report Er 23 07 2015Dokumen25 halamanDuty Report Er 23 07 2015Auditya WidyasariBelum ada peringkat
- MR GoutyDokumen25 halamanMR GoutyArvindan SubramaniamBelum ada peringkat
- Janiar, Female, 74 Yo, HCU 12Dokumen11 halamanJaniar, Female, 74 Yo, HCU 12Melsa AprimaBelum ada peringkat
- Apriyanto Lifandy Desmy FadillahDokumen38 halamanApriyanto Lifandy Desmy FadillahdesmyyBelum ada peringkat
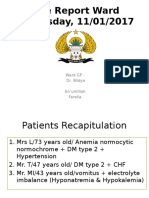
- Case Report Ward Wednesday, 11/01/2017: Ward GP: Dr. Widya An'umillah FarellaDokumen39 halamanCase Report Ward Wednesday, 11/01/2017: Ward GP: Dr. Widya An'umillah FarellaFarella KartikaBelum ada peringkat
- Duty Report - Rosni (DR - Gari)Dokumen9 halamanDuty Report - Rosni (DR - Gari)RudiErwinKurniawanBelum ada peringkat
- Duty Report - Rosni (DR - Gari)Dokumen9 halamanDuty Report - Rosni (DR - Gari)RudiErwinKurniawanBelum ada peringkat
- English Case JaundiceDokumen38 halamanEnglish Case JaundiceCavin HandokoBelum ada peringkat
- Diploma in Medical and Health Science Case ClerkingDokumen11 halamanDiploma in Medical and Health Science Case ClerkingWan AmeeramirulzamanBelum ada peringkat
- Anamnesis: Autoanamnesis On March 22 ND 2017 Chief Complaint General Weekness 1 Day AgoDokumen25 halamanAnamnesis: Autoanamnesis On March 22 ND 2017 Chief Complaint General Weekness 1 Day AgoTebeBelum ada peringkat
- Yulnova, Acute On CKD and Thrombocytopenia, Duty HannaDokumen18 halamanYulnova, Acute On CKD and Thrombocytopenia, Duty HannaHanna GustinBelum ada peringkat
- Sirosis HepatisDokumen29 halamanSirosis HepatisXaverius da CunhaBelum ada peringkat
- A Case On Periampullary Carcinoma.: Presented by DR Sumaiya Tasnim TanimaDokumen34 halamanA Case On Periampullary Carcinoma.: Presented by DR Sumaiya Tasnim TanimaJobaer MahmudBelum ada peringkat
- Case Illustration: TH THDokumen6 halamanCase Illustration: TH THdigimon666Belum ada peringkat
- Heri Sunoto, CKD CHF, Duty HannaDokumen17 halamanHeri Sunoto, CKD CHF, Duty HannaHanna GustinBelum ada peringkat
- CR Piopneumothoraks Nicky FIXdDokumen62 halamanCR Piopneumothoraks Nicky FIXdPutri RahmawatiBelum ada peringkat
- Upper GI BleedingDokumen70 halamanUpper GI BleedingMia MusBelum ada peringkat
- Morning Report RakaDokumen19 halamanMorning Report Rakaraka widhiartaBelum ada peringkat
- Case PresentationDokumen20 halamanCase PresentationMohamad HafyfyBelum ada peringkat
- Duty Report Chronic Kidney Diseases, DM and GERD: Approach of Complexity ProblemDokumen15 halamanDuty Report Chronic Kidney Diseases, DM and GERD: Approach of Complexity ProblemGiovina FajarBelum ada peringkat
- CFGVDokumen28 halamanCFGVmyolie wuBelum ada peringkat
- Bedah 21 Nov 2022 + FU 19 Nov 22 + Patof.Dokumen28 halamanBedah 21 Nov 2022 + FU 19 Nov 22 + Patof.maya_rosmariaBelum ada peringkat
- Sri Pertiwi, Syok Sepsis CAPDokumen14 halamanSri Pertiwi, Syok Sepsis CAPLukman NurhakimBelum ada peringkat
- Imed Case 5Dokumen11 halamanImed Case 5Shakshi RainaBelum ada peringkat
- Case Base DiscussionDokumen19 halamanCase Base DiscussionNu JoeBelum ada peringkat
- NCP An - MVDokumen7 halamanNCP An - MVMahendri Deayu PutriBelum ada peringkat
- LeptospirosisDokumen19 halamanLeptospirosisFelicia adeline ChristianBelum ada peringkat
- Mastoera, Female, 87 Yo, HCU 8Dokumen10 halamanMastoera, Female, 87 Yo, HCU 8Melsa AprimaBelum ada peringkat
- Case Conference February 1st 2018Dokumen26 halamanCase Conference February 1st 2018Efan StiawanBelum ada peringkat
- Presentasi Kasus Dokter Arif Cynthia NataliaDokumen26 halamanPresentasi Kasus Dokter Arif Cynthia NataliaIntan SorayaBelum ada peringkat
- Yetti, CAP Hipoxia, Duty HannaDokumen18 halamanYetti, CAP Hipoxia, Duty HannaHanna GustinBelum ada peringkat
- Baru Titi Sumarni, Melena Uremic Bleeding, CKD Stage V, Oa GenuDokumen15 halamanBaru Titi Sumarni, Melena Uremic Bleeding, CKD Stage V, Oa GenuherdianBelum ada peringkat
- Neli Pastinar, Penkes UE, RPGN, SLE, Duty HannaDokumen19 halamanNeli Pastinar, Penkes UE, RPGN, SLE, Duty HannaHanna GustinBelum ada peringkat
- Ca StomachDokumen33 halamanCa StomachAdvaith DevanandBelum ada peringkat
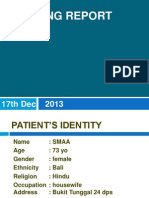
- Morning Report Case: 17th Dec 2013Dokumen22 halamanMorning Report Case: 17th Dec 2013SunardiasihBelum ada peringkat
- Vier Marleiny, Melena Gastropathy Nsaid, Duty HannaDokumen19 halamanVier Marleiny, Melena Gastropathy Nsaid, Duty HannaHanna GustinBelum ada peringkat
- Syafrudin, Male, 58 Yo, MW 11: Chief Complaint: (Autoanamnesis and Alloanamnesis) Present Illness HistoryDokumen14 halamanSyafrudin, Male, 58 Yo, MW 11: Chief Complaint: (Autoanamnesis and Alloanamnesis) Present Illness HistoryLukman NurhakimBelum ada peringkat
- Case Conference Sunday Night Shift, October 14 2018Dokumen26 halamanCase Conference Sunday Night Shift, October 14 2018Hendra WardhanaBelum ada peringkat
- Liver Function Test FinalDokumen98 halamanLiver Function Test FinalHussain AzharBelum ada peringkat
- Wa0008.Dokumen14 halamanWa0008.Mahendra NitharwalBelum ada peringkat
- Muhammad Nur, Penkes Ec SAE DD Hypoxia, Duty HannaDokumen16 halamanMuhammad Nur, Penkes Ec SAE DD Hypoxia, Duty HannaHanna GustinBelum ada peringkat
- MburiDokumen11 halamanMburirahmaBelum ada peringkat
- Lapjag 10 Feb 2016 - AnemiaDokumen25 halamanLapjag 10 Feb 2016 - AnemiamyoganoBelum ada peringkat
- Case DR SigitDokumen71 halamanCase DR SigitandreBelum ada peringkat
- Intraoperatively Inadequate BlockMORBIDITY ProtocolDokumen9 halamanIntraoperatively Inadequate BlockMORBIDITY Protocoldocv526Belum ada peringkat
- Rheumatoid Arthritis LapsusDokumen37 halamanRheumatoid Arthritis Lapsusderahmat dedyBelum ada peringkat
- Case CHF, Cap, DM Tipe 2 - Dr. Ruddy, SP - PDDokumen34 halamanCase CHF, Cap, DM Tipe 2 - Dr. Ruddy, SP - PDMelisaBelum ada peringkat
- LAPORAN TUTORIAL Case 1 Kelompok B5 - Hepatitis SirosisDokumen35 halamanLAPORAN TUTORIAL Case 1 Kelompok B5 - Hepatitis SirosisTutde SedanaBelum ada peringkat
- Morning Report YusmustiDokumen9 halamanMorning Report YusmustiAfdhol FalahBelum ada peringkat
- Uterine Myoma With Cystic DegenertionDokumen17 halamanUterine Myoma With Cystic DegenertionMeizaBelum ada peringkat
- Duty DewiDokumen13 halamanDuty DewiLukman NurhakimBelum ada peringkat
- AfrinalDokumen15 halamanAfrinalLiya AnjelinaBelum ada peringkat
- MR BP Dan AsphyxiaDokumen29 halamanMR BP Dan AsphyxiaRizky FajriBelum ada peringkat
- CC 22 Sept Pneumonia KolestasisDokumen60 halamanCC 22 Sept Pneumonia KolestasisIka Juli2018Belum ada peringkat
- Ny.T PEB Eng Tim Dinas 2Dokumen23 halamanNy.T PEB Eng Tim Dinas 2arifsandroBelum ada peringkat
- Death Case: DR Levina DR Muhammad Fauzan AssegafDokumen45 halamanDeath Case: DR Levina DR Muhammad Fauzan AssegafWiwik Puji LestariBelum ada peringkat
- Febrianto, Sepsis Ec HAP, PIS, Duty HannaDokumen17 halamanFebrianto, Sepsis Ec HAP, PIS, Duty HannaHanna GustinBelum ada peringkat
- Case GNApsDokumen47 halamanCase GNApsAndhika Hadi WirawanBelum ada peringkat
- JurnalDokumen5 halamanJurnalAnggita Nur AzizaBelum ada peringkat
- PottDokumen14 halamanPottAnggita Nur AzizaBelum ada peringkat
- Presentasi HapDokumen33 halamanPresentasi HapAnggita Nur AzizaBelum ada peringkat
- Is Case DR Nur NoviDokumen36 halamanIs Case DR Nur NoviAnggita Nur AzizaBelum ada peringkat
- Is Case DR Nur NoviDokumen36 halamanIs Case DR Nur NoviAnggita Nur AzizaBelum ada peringkat
- Is Case DR Nur NoviDokumen36 halamanIs Case DR Nur NoviAnggita Nur AzizaBelum ada peringkat
- Is Case DR Nur NoviDokumen36 halamanIs Case DR Nur NoviAnggita Nur AzizaBelum ada peringkat
- Bercak Darah ReferatDokumen35 halamanBercak Darah ReferatAnggita Nur AzizaBelum ada peringkat
- How To Interpret An EcgDokumen57 halamanHow To Interpret An EcgAnggita Nur AzizaBelum ada peringkat
- Pre - Operative SurgeryDokumen3 halamanPre - Operative SurgeryFan Eli100% (5)
- DermatologyDokumen30 halamanDermatologyCarlos HernándezBelum ada peringkat
- Bowel EliminationDokumen5 halamanBowel EliminationDimple Castañeto CalloBelum ada peringkat
- Group 1 PWC and Group 2 PWC No Power OptionsDokumen3 halamanGroup 1 PWC and Group 2 PWC No Power OptionslisamaurerBelum ada peringkat
- Azide Dextrose BrothDokumen1 halamanAzide Dextrose BrothJHOSELINE KHATERINE RAMIREZ BARBARANBelum ada peringkat
- Clinical Experience With Surgical Debridement and Simultaneous Meshed Skin Grafts in Treating Biofilm-Associated Infection: An Exploratory Retrospective Pilot StudyDokumen9 halamanClinical Experience With Surgical Debridement and Simultaneous Meshed Skin Grafts in Treating Biofilm-Associated Infection: An Exploratory Retrospective Pilot StudyAsmat BurhanBelum ada peringkat
- Critical Study On Gulma and It's Surgical Aspects in AyurvedaDokumen24 halamanCritical Study On Gulma and It's Surgical Aspects in AyurvedaPREM277272Belum ada peringkat
- Endotracheal Intubation Management RPAH PC2022 014Dokumen15 halamanEndotracheal Intubation Management RPAH PC2022 014sinasinaaiBelum ada peringkat
- 4 2 HomeworkDokumen8 halaman4 2 HomeworkShawntel IsordiaBelum ada peringkat
- Herpes Zoster: Shingles Acute Posterior GanglionitisDokumen23 halamanHerpes Zoster: Shingles Acute Posterior GanglionitisHannah Clarisse Monge IgniBelum ada peringkat
- Laboratory Test Result Reference Value Description Unit Molecular and GenomicsDokumen1 halamanLaboratory Test Result Reference Value Description Unit Molecular and GenomicsFajar Reza LaksanaBelum ada peringkat
- Anatomi Sistem Lakrimal: - SekresiDokumen13 halamanAnatomi Sistem Lakrimal: - SekresiPutri PurwanthiBelum ada peringkat
- Insulin Resistance and PCOS-dr. Hilma Final 11 Juli 2021 FIXDokumen48 halamanInsulin Resistance and PCOS-dr. Hilma Final 11 Juli 2021 FIXputrihealthirezaBelum ada peringkat
- Non Communicable DiseasesDokumen13 halamanNon Communicable Diseaseszzzsubedi100% (1)
- Askep CKDDokumen55 halamanAskep CKDyuli ariyantiBelum ada peringkat
- Chapter 6-Family Nursing Care PlanDokumen3 halamanChapter 6-Family Nursing Care PlanBi B BelleBelum ada peringkat
- Fraser Health: Health Authority Redesign AccomplishmentsDokumen13 halamanFraser Health: Health Authority Redesign AccomplishmentsStephen OlsonBelum ada peringkat
- Activity On Lesson 2 Common Injuries in DanceDokumen10 halamanActivity On Lesson 2 Common Injuries in DancePammy AlivenBelum ada peringkat
- Personal Notes Excpetional StuffDokumen352 halamanPersonal Notes Excpetional StuffYagyeshBelum ada peringkat
- Tablet PCR Cheat SheetDokumen4 halamanTablet PCR Cheat Sheetapi-253658656Belum ada peringkat
- Humoral Imune Respon: SuhermanDokumen62 halamanHumoral Imune Respon: SuhermansuhermanBelum ada peringkat
- Referat AppendicitisDokumen28 halamanReferat AppendicitisFerio Joelian ChandraBelum ada peringkat
- IgA NephrophathyDokumen4 halamanIgA NephrophathyyousifBelum ada peringkat