Carbetocin For The Prevention of Postpartum Hemorrhage: D. Cordovani, J. C. A. Carvalho, M. Boucher and D. Farine
Diunggah oleh
Kartika AnggakusumaJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Carbetocin For The Prevention of Postpartum Hemorrhage: D. Cordovani, J. C. A. Carvalho, M. Boucher and D. Farine
Diunggah oleh
Kartika AnggakusumaHak Cipta:
Format Tersedia
44
Carbetocin for the Prevention of Postpartum
Hemorrhage
D. Cordovani, J. C. A. Carvalho, M. Boucher and D. Farine
INTRODUCTION
Considering the physical and emotional costs of
postpartum hemorrhage (PPH) worldwide, it is not
surprising that institutions as diverse as the World
Health Organization, the International Confederation
of Midwives (ICM) and the International Federation
of Gynecology and Obstetrics (FIGO) all recommend
active management of the third stage of labor
(AMTSL) even for patients with low risk for PPH
1,2
(see Chapters 14 and 15). Their consensus is under-
standable given that numerically more women with-
out risk factors for PPH suffer from it than do women
with obvious risk factors
2
.
The administration of a uterotonic medication soon
after the delivery of the fetus is an essential part of the
AMTSL
2
that is capable of decreasing the incidence of
PPH by 40%
3,4
. However, these medications pose
some challenges, in that individually and collectively
they have side-effects, contraindications and problems
with storage and administration. As such, the search
for the ideal uterotonic continues, and today the
main uterotonic agents are oxytocin, ergonovine,
carboprost, carbetocin and misoprostol. This chapter
focuses on carbetocin.
Oxytocin is the most widely available and used
uterotonic agent
3,5
(see Chapter 43). It binds to the
myometrial oxytocin receptors and stimulates contrac-
tion of the uterine muscle by increasing the intra-
cellular concentration of calcium
6,7
. However, its use
is not without some limitations. Oxytocin has a short
half-life of 317 minutes, and a continuous intra-
venous (IV) infusion is necessary to achieve sustained
uterotonic activity
3,5,7
. Moreover, large doses or
boluses of oxytocin are associated with adverse
effects in the form of hypotension, nausea, vomiting,
dysrhythmias, ST-T changes, pulmonary edema and
severe water intoxication with convulsions
3,8,9
.
In contrast, carbetocin (1-deamino-1-carba-2-
tyrosine(O-methyl)-oxytocin) is a synthetic oxytocin
analogue that binds to the same oxytocin receptors
in the myometrium with an affinity similar to that
of oxytocin
6,7
. Its main advantage over oxytocin
is a four-fold longer uterotonic activity, a fact
which precludes the necessity of a continuous
infusion
10,11
.
PHARMACOLOGY
As noted above, carbetocin is a synthetic oxytocin
analogue that binds to the same myometrium recep-
tors as oxytocin with similar affinity
7,12
. Despite a sim-
ilar affinity, its potency in animal models is about
one-tenth that of oxytocin on a mole per mole basis
13
.
At the same time, its plasma half-life is approximately
40 minutes after IV injection, which is 410 times
longer than that of oxytocin
10
. Similarly to oxytocin,
it causes an increase in the intracellular concentration
of calcium that promotes uterine contractility, through
the generation of inositol phosphates
14
.
Oxytocin and vasopressin are neurohypophysial
hormones with a short half-life in plasma. By remov-
ing the primary amino group from the vasopressin
molecule, a prolongation of the half-life was achieved,
something which did not happen when the same alter-
ation was made in the oxytocin molecule. A further
alteration of the molecule was necessary in order to
achieve this same goal. The disulfide bond had been
proven not to be important in the mechanism of
action of oxytocin
6
. By removing the amino group
(1-deamino), and replacing the sulfur atom at position
1 with a carba group (CH
2
), a prolonged myo-
metrial action was observed
6,7
. Carbetocin is the carba
analogue being used clinically in order to prevent
and/or treat PPH. The deamination protects carbe-
tocin from aminopeptidase cleavage, and the replace-
ment of the disulfide bond by CH
2
S protects the
analogue from disulfidase cleavage
15
(Figure 1). This is
the suggested explanation for the protracted half-life of
carbetocin in plasma. Another suggested explanation
for the prolonged activity of carbetocin is its higher
lipophilicity that can alter its tissue distribution
7,13
.
Atke et al. suggested that this increased lipophilicity
was responsible for an increased half-life in the
receptor compartment
7
.
The structural differences between the molecules
of oxytocin and carbetocin could also explain the
decreased potency of the latter when compared with
the former. The current recommended dose of
carbetocin for the prevention of PPH is 100 g, which
is roughly equivalent to 10 g (5 IU) of oxytocin
13
.
However, it is important to highlight that these figures
are derived from animal data. Human myometrium
361
receptors might have higher affinity to carbetocin than
rat receptors; therefore, it is not clear if the decreased
potency found in animal models can be extrapolated
to humans
7,13
.
In a study, performed on 40 women, carbetocin
was administered either IV in doses varying from 8 to
30 g or intramuscularly (IM) in doses varying from
10 to 70 g, 2448 h postpartum. After IV administra-
tion, tetanic contraction was achieved in a mean time
( SD) of 1.2 0.5 min. Uterine tetany lasted for
6.9 2.1 min followed by rhythmic contraction for
60 18 min. After IM administration, the onset was
1.9 0.6 min, with tetanic contractions lasting for
11.3 3 min, followed by rhythmic contractions that
lasted for 119 69 min
13
. According to these findings,
the onset is not affected by the route of administration,
but the uterotonic activity is significant longer
(two-fold) after IM injection when compared with IV.
After IM injection, carbetocin reaches peak plasma
levels in 30 min and its bioavailability is 80%
5,10,16,17
.
Small amounts of carbetocin can cross over from
plasma to breast milk, with a mean peak concentration
in breast milk that is 50 times lower than in plasma
11
.
This small amount is not of clinical concern, as
carbetocin would be rapidly degraded by peptidases in
the infants gastrointestinal tract.
CARBETOCIN AT CESAREAN DELIVERY
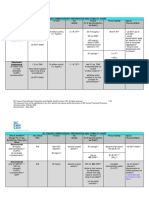
To the best of our knowledge, only nine studies have
used carbetocin for prevention of PPH after cesarean
delivery. These are presented in Table 1 in chronolog-
ical order.
The first study was published in abstract form. It
was a dose-finding study with a total of 18 patients
who underwent elective cesarean section under
epidural anesthesia. This study established the recom-
mended dose of 100 g. There was a 0% response in
terms of uterine contractility with doses below 60 g,
and 83% (5 out of 6) response with a dose of 100 g
18
.
Barton et al. published in abstract form their find-
ings comparing carbetocin 100 g versus placebo
19
.
Although carbetocin is in fact more efficient than
placebo, 28% of the women in the placebo group did
not require any uterotonic therapy.
Boucher et al. conducted a double-blind random-
ized control trial to compare carbetocin 100 g IV
bolus after placental delivery with oxytocin 2.5 IU IV
bolus followed by a 16 h infusion of oxytocin for a
total of 30 IU
20
. Their primary outcome was blood
loss as calculated by means of aspiration from the surgi-
cal field from the time the study drug was administered
until skin closure. Although not statistically significant,
women in the carbetocin group bled 29 ml less
(p = 0.3). More important, significantly fewer women
had blood loss greater than 200 ml with carbetocin
(p = 0.0041). In addition, the three study participants
that required additional uterotonic intervention were
all in the oxytocin group.
Similarly, Dansereau et al. also compared carbetocin
as a single 100 g bolus IV with oxytocin IV bolus fol-
lowed by 8 h infusion of oxytocin after cesarean deliv-
ery for women with low risk for PPH
9
. This Canadian
multicenter double-blind randomized controlled trial
is the largest study to date, with 694 participants. The
major finding was a 50% decrease in the necessity of
additional uterotonic therapy in patients treated with
carbetocin when compared with oxytocin.
Del Angel-Garcia et al. published in abstract form
their findings comparing carbetocin 100 g IV with
oxytocin 5 IU IV after elective cesarean delivery in
patients with at least one risk factor for PPH
21
. Uterine
atony was reported in 8% of the patients in the
carbetocin group versus 19% in the oxytocin arm.
This Mexican study included a cost analysis. Accord-
ing to the authors, allocation of patients to carbetocin
therapy resulted in lower cost than those treated with
oxytocin (US dollars 3525 vs. US dollars 4054).
Borruto et al. also compared carbetocin as a single
IV bolus with oxytocin infusion. Their study included
both elective and emergency cesarean delivery among
patients who had at least one risk factor for PPH
22
.
Similar to the previous studies, the odds ratio (OR) for
uterotonic intervention was 1.83 (95% CI 0.92.6)
times higher in the oxytocin group compared with the
carbetocin group.
Attilakos et al., in a double-blind randomized con-
trolled trial compared carbetocin 100 g single IV
bolus with oxytocin 5 IU single IV bolus after low risk
cesarean deliveries
23
. Additional uterotonics were nec-
essary in 33.5% of patients in the carbetocin group
patients compared with 45.5% in the oxytocin group
(p = 0.023). This study included 377 patients.
Although the need for additional uterotonics was
decreased, not dissimilar to other studies mentioned
above, this study did not demonstrate a decrease in
blood loss or in the incidence of PPH. Of interest,
both arms of the study had a high failure rate.
Triopon et al., in a French two-phase observational
study
24
, compared the outcomes of a cohort of
155 patients who received oxytocin with the out-
comes of a subsequent cohort of 155 patients who
received carbetocin after cesarean delivery (after the
362
POSTPARTUM HEMORRHAGE
Figure 1 Oxytocin molecule. The amino group and the disulfide
bond, which were altered in order to create carbetocin, are
indicated. The amino group was removed and the sulfur atom was
replaced by a carba group
363
Carbetocin for the Prevention of Postpartum Hemorrhage
A
u
t
h
o
r
Y
e
a
r
T
y
p
e
o
f
s
t
u
d
y
P
o
p
u
l
a
t
i
o
n
I
n
t
e
r
v
e
n
t
i
o
n
O
u
t
c
o
m
e
s
B
o
u
c
h
e
r
e
t
a
l
.
1
8
1
9
9
1
D
o
s
e
-
r
a
n
g
i
n
g
L
o
w
-
r
i
s
k
,
e
l
e
c
t
i
v
e
C
/
S
u
n
d
e
r
e
p
i
d
u
r
a
l
(
n
=
1
8
)
C
a
r
b
e
t
o
c
i
n
I
V
r
a
n
g
i
n
g
f
r
o
m
1
0
t
o
1
0
0
g
a
f
t
e
r
d
e
l
i
v
e
r
y
o
f
p
l
a
c
e
n
t
a
0
%
r
e
s
p
o
n
s
e
w
i
t
h
d
o
s
e
s
6
0
g
8
3
%
(
5
/
6
)
w
i
t
h
t
e
t
a
n
i
c
c
o
n
t
r
a
c
t
i
o
n
w
i
t
h
1
0
0
g
B
a
r
t
o
n
e
t
a
l
.
1
9
(
a
b
s
t
r
a
c
t
)
1
9
9
6
D
o
u
b
l
e
-
b
l
i
n
d
R
C
T
L
o
w
-
r
i
s
k
e
l
e
c
t
i
v
e
C
/
S
u
n
d
e
r
r
e
g
i
o
n
a
l
a
n
e
s
t
h
e
s
i
a
(
n
=
1
1
9
)
1
0
0
g
c
a
r
b
e
t
o
c
i
n
(
n
=
6
2
)
v
s
.
s
a
l
i
n
e
(
n
=
5
7
)
U
t
e
r
i
n
e
t
o
n
e
s
i
g
n
i
f
i
c
a
n
t
l
y
i
n
c
r
e
a
s
e
d
i
n
c
a
r
b
e
t
o
c
i
n
t
r
e
a
t
e
d
w
o
m
e
n
(
p
<
0
.
0
5
)
U
s
e
o
f
a
d
d
i
t
i
o
n
a
l
u
t
e
r
o
t
o
n
i
c
t
h
e
r
a
p
y
8
/
6
2
v
s
.
4
1
/
5
7
,
R
R
0
.
1
8
(
C
I
9
5
%
0
.
0
9
0
.
3
5
)
B
o
u
c
h
e
r
e
t
a
l
.
2
0
1
9
9
8
D
o
u
b
l
e
-
b
l
i
n
d
R
C
T
L
o
w
-
r
i
s
k
,
e
l
e
c
t
i
v
e
C
/
S
u
n
d
e
r
e
p
i
d
u
r
a
l
(
n
=
5
7
)
C
a
r
b
e
t
o
c
i
n
1
0
0
g
I
V
(
n
=
2
9
)
v
s
.
o
x
y
t
o
c
i
n
2
.
5
I
U
I
V
b
o
l
u
s
+
1
6
h
i
n
f
u
s
i
o
n
o
f
3
0
I
U
a
f
t
e
r
d
e
l
i
v
e
r
y
o
f
p
l
a
c
e
n
t
a
M
e
a
n
i
n
t
r
a
o
p
e
r
a
t
i
v
e
b
l
o
o
d
l
o
s
s
w
a
s
1
5
9
v
s
.
1
8
8
m
l
(
p
=
0
.
3
)
S
i
g
n
i
f
i
c
a
n
t
l
y
f
e
w
e
r
w
o
m
e
n
h
a
d
b
l
o
o
d
l
o
s
s
2
0
0
m
l
w
i
t
h
c
a
r
b
e
t
o
c
i
n
(
3
3
%
)
v
s
.
o
x
y
t
o
c
i
n
(
7
9
%
)
(
p
=
0
.
0
0
4
1
)
C
o
m
p
a
r
a
b
l
e
v
i
t
a
l
s
i
g
n
s
a
n
d
h
e
m
a
t
o
l
o
g
i
c
v
a
l
u
e
s
D
a
n
s
e
r
e
a
u
e
t
a
l
.
9
1
9
9
9
C
a
n
a
d
i
a
n
m
u
l
t
i
c
e
n
t
e
r
d
o
u
b
l
e
-
b
l
i
n
d
R
C
T
L
o
w
-
r
i
s
k
e
l
e
c
t
i
v
e
C
/
S
u
n
d
e
r
r
e
g
i
o
n
a
l
a
n
e
s
t
h
e
s
i
a
(
n
=
6
9
4
)
C
a
r
b
e
t
o
c
i
n
1
0
0
g
I
V
(
n
=
3
1
7
)
v
s
.
o
x
y
t
o
c
i
n
5
I
U
I
V
b
o
l
u
s
8
h
i
n
f
u
s
i
o
n
o
f
2
0
I
U
(
n
=
3
1
8
)
A
d
d
i
t
i
o
n
a
l
o
x
y
t
o
c
i
c
i
n
t
e
r
v
e
n
t
i
o
n
w
a
s
4
.
7
%
v
s
.
1
0
.
1
%
(
p
<
0
.
0
5
)
O
R
f
o
r
t
r
e
a
t
m
e
n
t
f
a
i
l
u
r
e
w
a
s
2
.
0
3
t
i
m
e
s
h
i
g
h
e
r
w
i
t
h
o
x
y
t
o
c
i
n
v
s
.
c
a
r
b
e
t
o
c
i
n
(
9
5
%
C
I
1
.
1
2
.
8
)
S
i
m
i
l
a
r
s
a
f
e
t
y
p
r
o
f
i
l
e
D
e
l
A
n
g
e
l
-
G
a
r
c
i
a
e
t
a
l
.
2
1
(
a
b
s
t
r
a
c
t
)
2
0
0
6
R
a
n
d
o
m
i
z
e
d
p
r
a
g
m
a
t
i
c
c
l
i
n
i
c
a
l
t
r
i
a
l
A
t
l
e
a
s
t
1
r
i
s
k
f
a
c
t
o
r
f
o
r
P
P
H
,
e
l
e
c
t
i
v
e
C
/
S
(
n
=
1
5
2
)
C
a
r
b
e
t
o
c
i
n
1
0
0
g
I
V
(
n
=
7
7
)
v
s
.
o
x
y
t
o
c
i
n
5
I
U
I
V
(
n
=
7
5
)
U
t
e
r
i
n
e
a
t
o
n
y
i
n
8
%
v
s
.
1
9
%
(
p
<
0
.
0
0
0
1
)
B
l
o
o
d
l
o
s
s
5
0
0
m
l
o
n
l
y
o
b
s
e
r
v
e
d
w
i
t
h
o
x
y
t
o
c
i
n
C
h
e
a
p
e
r
m
e
a
n
c
o
s
t
p
e
r
p
a
t
i
e
n
t
t
r
e
a
t
e
d
w
i
t
h
c
a
r
b
e
t
o
c
i
n
(
U
S
D
3
5
2
5
v
s
.
U
S
D
4
0
5
4
)
B
o
r
r
u
t
o
e
t
a
l
.
2
2
2
0
0
9
R
a
n
d
o
m
i
z
e
d
c
o
n
t
r
o
l
l
e
d
c
l
i
n
i
c
a
l
t
r
i
a
l
S
i
n
g
l
e
t
o
n
,
a
t
l
e
a
s
t
1
r
i
s
k
f
a
c
t
o
r
f
o
r
P
P
H
,
e
l
e
c
t
i
v
e
o
r
e
m
e
r
g
e
n
c
y
C
/
S
(
n
=
1
0
4
)
C
a
r
b
e
t
o
c
i
n
1
0
0
g
(
n
=
5
2
)
v
s
.
o
x
y
t
o
c
i
n
2
h
i
n
f
u
s
i
o
n
o
f
1
0
I
U
(
n
=
5
2
)
a
f
t
e
r
p
l
a
c
e
n
t
a
l
d
e
l
i
v
e
r
y
U
t
e
r
o
t
o
n
i
c
i
n
t
e
r
v
e
n
t
i
o
n
i
n
3
.
8
%
v
s
.
9
.
6
%
(
p
<
0
.
0
1
)
O
R
f
o
r
t
r
e
a
t
m
e
n
t
f
a
i
l
u
r
e
w
a
s
1
.
8
3
(
9
5
%
C
I
0
.
9
2
.
6
)
M
e
a
n
b
l
o
o
d
l
o
s
s
3
0
m
l
l
e
s
s
w
i
t
h
c
a
r
b
e
t
o
c
i
n
(
p
=
0
.
0
5
)
A
t
t
i
l
a
k
o
s
e
t
a
l
.
2
3
2
0
1
0
D
o
u
b
l
e
-
b
l
i
n
d
R
C
T
L
o
w
-
r
i
s
k
,
e
l
e
c
t
i
v
e
o
r
e
m
e
r
g
e
n
c
y
C
/
S
(
n
=
3
7
7
)
C
a
r
b
e
t
o
c
i
n
1
0
0
g
I
V
(
n
=
1
8
8
)
v
s
.
o
x
y
t
o
c
i
n
5
I
U
I
V
(
n
=
1
8
9
)
A
d
d
i
t
i
o
n
a
l
o
x
y
t
o
c
i
c
3
3
.
5
%
v
s
.
4
5
.
5
%
(
R
R
0
.
7
4
,
9
5
%
C
I
0
.
5
7
0
.
9
5
,
p
=
0
.
0
2
3
)
N
o
d
i
f
f
e
r
e
n
c
e
i
n
e
s
t
i
m
a
t
e
d
b
l
o
o
d
l
o
s
s
,
s
i
d
e
-
e
f
f
e
c
t
s
,
o
r
h
e
m
a
t
o
l
o
g
i
c
v
a
l
u
e
s
T
r
i
o
p
o
n
e
t
a
l
.
2
4
2
0
1
0
T
w
o
-
p
h
a
s
e
o
b
s
e
r
v
a
t
i
o
n
a
l
s
t
u
d
y
E
l
e
c
t
i
v
e
o
r
e
m
e
r
g
e
n
c
y
C
/
S
(
n
=
3
1
0
)
U
s
e
o
f
c
a
r
b
e
t
o
c
i
n
a
s
a
s
e
n
t
i
n
e
l
e
v
e
n
t
s
e
p
a
r
a
t
i
n
g
t
h
e
2
g
r
o
u
p
s
.
D
a
t
a
f
r
o
m
1
5
5
w
h
o
r
e
c
e
i
v
e
d
o
x
y
t
o
c
i
n
5
I
U
c
o
m
p
a
r
e
d
w
i
t
h
1
5
5
w
o
m
e
n
w
h
o
r
e
c
e
i
v
e
d
c
a
r
b
e
t
o
c
i
n
1
0
0
g
a
f
t
e
r
f
e
t
a
l
d
e
l
i
v
e
r
y
S
i
g
n
i
f
i
c
a
n
t
d
e
c
r
e
a
s
e
i
n
p
o
s
t
o
p
e
r
a
t
i
v
e
I
V
i
r
o
n
a
d
m
i
n
i
s
t
r
a
t
i
o
n
i
n
t
h
e
c
a
r
b
e
t
o
c
i
n
g
r
o
u
p
(
6
.
5
%
v
s
.
1
4
.
5
%
,
p
=
0
.
0
3
)
F
e
w
e
r
c
o
m
p
r
e
s
s
i
o
n
s
u
t
u
r
e
s
(
a
l
t
h
o
u
g
h
n
o
t
s
i
g
n
i
f
i
c
a
n
t
)
i
n
t
h
e
c
a
r
b
e
t
o
c
i
n
g
r
o
u
p
(
0
.
6
%
v
s
.
4
.
5
%
,
p
=
0
.
0
6
)
N
o
d
i
f
f
e
r
e
n
c
e
i
n
t
h
e
i
n
c
i
d
e
n
c
e
o
f
v
a
s
c
u
l
a
r
s
u
t
u
r
e
s
,
n
e
c
e
s
s
i
t
y
o
f
a
d
d
i
t
i
o
n
a
l
u
t
e
r
o
t
o
n
i
c
,
a
n
d
b
l
o
o
d
t
r
a
n
s
f
u
s
i
o
n
C
o
r
d
o
v
a
n
i
e
t
a
l
.
2
5
2
0
1
2
D
o
u
b
l
e
-
b
l
i
n
d
,
r
a
n
d
o
m
i
z
e
d
d
o
s
e
-
f
i
n
d
i
n
g
s
t
u
d
y
L
o
w
-
r
i
s
k
,
e
l
e
c
t
i
v
e
C
/
S
u
n
d
e
r
s
p
i
n
a
l
a
n
e
s
t
h
e
s
i
a
(
n
=
8
0
)
C
a
r
b
e
t
o
c
i
n
8
0
,
9
0
,
1
0
0
,
1
1
0
o
r
1
2
0
g
I
V
a
f
t
e
r
f
e
t
a
l
d
e
l
i
v
e
r
y
S
i
m
i
l
a
r
f
a
i
l
u
r
e
r
a
t
e
a
m
o
n
g
a
l
l
d
o
s
e
g
r
o
u
p
s
.
N
o
t
p
o
s
s
i
b
l
e
t
o
c
a
l
c
u
l
a
t
e
E
D
9
5
S
i
m
i
l
a
r
i
n
c
i
d
e
n
c
e
o
f
s
i
d
e
-
e
f
f
e
c
t
s
a
n
d
b
l
o
o
d
l
o
s
s
i
n
a
l
l
g
r
o
u
p
s
O
v
e
r
a
l
l
,
u
t
e
r
u
s
w
a
s
b
o
g
g
y
a
t
2
m
i
n
i
n
1
0
/
8
0
(
1
2
.
5
%
)
A
d
d
i
t
i
o
n
a
l
u
t
e
r
o
t
o
n
i
c
g
i
v
e
n
t
o
9
/
8
0
(
1
1
.
2
5
%
)
6
/
1
0
(
6
0
%
)
w
i
t
h
b
o
g
g
y
u
t
e
r
u
s
a
t
2
m
i
n
3
/
7
0
(
4
.
3
%
)
w
i
t
h
f
i
r
m
u
t
e
r
u
s
a
t
2
m
i
n
R
C
T
,
r
a
n
d
o
m
i
z
e
d
c
o
n
t
r
o
l
l
e
d
t
r
i
a
l
;
C
/
S
,
c
e
s
a
r
e
a
n
s
e
c
t
i
o
n
;
U
S
D
,
U
S
d
o
l
l
a
r
s
T
a
b
l
e
1
S
t
u
d
i
e
s
w
i
t
h
c
a
r
b
e
t
o
c
i
n
a
f
t
e
r
c
e
s
a
r
e
a
n
d
e
l
i
v
e
r
y
departments drug of choice for prevention of PPH
was converted from oxytocin to carbetocin). In con-
trast to the previous studies, there was no significant
decrease in the need for additional uterotonics. On the
other hand, there was a significant decrease in postop-
erative IV iron administration in the carbetocin group
(6.5% vs. 14.5%, p = 0.03) and fewer compression
sutures were necessary (although not significant) in the
carbetocin group (0.6% vs. 4.5%, p = 0.06).
A recent dose-finding study performed by
Cordovani et al. attempted to calculate the ED95 of
carbetocin for elective cesarean delivery in low-risk
patients for PPH
25
. The authors were unable to calcu-
late the ED95 of carbetocin, as the failure rate was
evenly distributed across all dose groups (80, 90, 100,
110 and 120 g). Overall, 12.5% of patients failed to
present a firm uterus after 2 min of drug administra-
tion, and 11.25% of women required additional
uterotonic therapy within 4 h. It is important to point
out that, three of the women requiring additional
uterotonics in fact had a firm uterus after 2 min of
carbetocin administration.
In general, the studies on cesarean deliveries have
shown a decrease in the necessity of additional
uterotonic intervention, although none demonstrated
a decrease in either the incidence of PPH or the mean
blood volume loss, as the study design practically elim-
inated such end points. At the same time, fewer
patients in the carbetocin arms of the studies lost larger
amounts of blood
21,22
. The optimal dose of carbetocin
is yet to be determined, but recent data suggest that
doses as low as 80 g are as effective as the current
recommended dose of 100 g
25
.
CARBETOCIN IN VAGINAL DELIVERY
Six studies on carbetocin therapy used in vaginal
deliveries are presented in Table 2 in chronological
order.
Van Dongen et al. performed an ascending dose-
tolerance study with IM carbetocin administered after
low risk vaginal deliveries
10
. Their findings revealed a
maximum tolerated dose of 200 g due to the pres-
ence of limiting side-effects, namely retained placenta,
blood loss of 1000 ml or more and blood transfusion.
Optimal results were within the 75125 g dose range
in keeping with the 100 g dose determined in the
original dose-finding study
19
.
Boucher et al., in a double-blind randomized con-
trolled trial involving 160 patients with at least one risk
factor for PPH, compared carbetocin 100 g IM with
oxytocin 10 IU IV infusion over a 2 h period
26
. Their
findings showed no difference in the requirement of
additional uterotonics or in the presence of PPH.
However, significantly fewer women in the carbe-
tocin arm required uterine massage compared with in
the oxytocin arm.
Leung et al. compared carbetocin 100 g IM
(n = 165) with Syntometrine
, a combination of oxy-
tocin and ergometrine, IM (n = 164) given after low
risk vaginal deliveries
17
. No significant difference was
observed in hemoglobin drop or use of additional
uterotonics, but women treated with Syntometrine
had a significantly higher incidence of nausea, vomit-
ing and hypertension.
Ngan et al., in a retrospective study involving 118
low risk patients, found that carbetocin was associated
with less blood loss compared with a combination of
oxytocin and ergometrine
27
.
Nirmala et al. studied 120 women at high risk for
PPH who delivered vaginally in another randomized
controlled trial which compared carbetocin 100 g
IM with Syntometrine IM
16
. In contrast to the find-
ings observed in a low risk population
17
, these authors
found a significant decrease in the mean blood loss as
well as a significant smaller decrease in hemoglobin
drop in the carbetocin group. However, there was no
difference in the necessity of additional uterotonic
agents or blood transfusion. Interestingly, also in
contrast to the findings of Leung et al.
17
, there was
no difference in the incidence of side-effects.
Su et al. performed yet another comparison of
carbetocin with Syntometrine
28
evaluating 370
women with low risk for PPH. Similar to previous
findings
17
, no differences were found in the require-
ments for additional uterotonic agents, in blood loss
or in the incidence of PPH. On the other hand,
side-effects were noticeably more prevalent in the
Syntometrine group.
In general, studies of vaginal deliveries found no
difference in the requirement for additional uterotonic
medication when compared with oxytocin or with a
combination of oxytocin and ergometrine. However,
when compared with oxytocin alone, carbetocin-
treated patients with at least one risk factor for PPH
required less uterine massage. The findings regarding
decrease in blood loss are conflicting. The most con-
sistent finding was a decrease in the incidence of nau-
sea and vomiting when compared with a combination
of oxytocin and ergometrine.
SIDE-EFFECTS AND CONTRAINDICATIONS
Oxytocin and carbetocin are without differences
regarding either the types of side-effects or their
frequency
9,20,22,23
. The incidence of side-effects in
three reports is presented in Table 3
9,20,22
. Although
not shown in the table, Borruto et al. described
28.8% of arrhythmias after oxytocin injection, but
none for carbetocin
22
. Similarly, Boucher et al. found a
3.6% incidence of premature ventricular contraction
after oxytocin administration, but none after
carbetocin
20
. The safety of carbetocin in patients
with severe cardiovascular disease has not yet been
determined.
As carbetocin should not be administered prior to
fetal delivery, under no circumstances should it be
used for induction of labor or labor augmentation. It
should be administered as an IM injection or slow IV
bolus over 1 min after fetal or placental delivery
1,11
.
The following is an extract from the product leaflet
provided by its manufacturer:
364
POSTPARTUM HEMORRHAGE
365
Carbetocin for the Prevention of Postpartum Hemorrhage
A
u
t
h
o
r
Y
e
a
r
T
y
p
e
o
f
s
t
u
d
y
P
o
p
u
l
a
t
i
o
n
I
n
t
e
r
v
e
n
t
i
o
n
O
u
t
c
o
m
e
s
V
a
n
D
o
n
g
e
n
e
t
a
l
.
1
0
1
9
9
8
A
s
c
e
n
d
i
n
g
d
o
s
e
t
o
l
e
r
a
n
c
e
L
o
w
-
r
i
s
k
,
v
a
g
i
n
a
l
d
e
l
i
v
e
r
y
(
n
=
4
5
)
C
a
r
b
e
t
o
c
i
n
I
M
(
1
5
,
3
0
,
5
0
,
7
5
,
1
0
0
,
1
2
5
,
1
5
0
,
1
7
5
,
2
0
0
g
)
i
m
m
e
d
i
a
t
e
l
y
a
f
t
e
r
b
i
r
t
h
o
f
i
n
f
a
n
t
M
a
x
i
m
u
m
b
l
o
o
d
l
o
s
s
a
t
t
h
e
u
p
p
e
r
a
n
d
l
o
w
e
r
d
o
s
e
l
e
v
e
l
s
.
L
o
w
e
s
t
i
n
t
h
e
7
0
1
2
5
g
r
a
n
g
e
M
a
x
i
m
u
m
t
o
l
e
r
a
t
e
d
d
o
s
e
c
a
l
c
u
l
a
t
e
d
t
o
b
e
2
0
0
g
(
4
/
1
8
r
e
t
a
i
n
e
d
p
l
a
c
e
n
t
a
,
3
/
1
8
b
l
o
o
d
t
r
a
n
s
f
u
s
i
o
n
,
4
/
1
8
a
d
d
i
t
i
o
n
a
l
o
x
y
t
o
c
i
c
s
)
B
o
u
c
h
e
r
e
t
a
l
.
2
6
2
0
0
4
D
o
u
b
l
e
-
b
l
i
n
d
R
C
T
A
t
l
e
a
s
t
1
r
i
s
k
f
a
c
t
o
r
f
o
r
P
P
H
(
n
=
1
6
0
)
C
a
r
b
e
t
o
c
i
n
1
0
0
g
I
M
+
I
V
p
l
a
c
e
b
o
(
n
=
8
3
)
v
s
.
p
l
a
c
e
b
o
I
M
+
o
x
y
t
o
c
i
n
1
0
I
U
2
h
I
V
i
n
f
u
s
i
o
n
(
n
=
7
7
)
a
f
t
e
r
d
e
l
i
v
e
r
y
o
f
p
l
a
c
e
n
t
a
N
o
d
i
f
f
e
r
e
n
c
e
i
n
r
e
q
u
i
r
e
m
e
n
t
f
o
r
a
d
d
i
t
i
o
n
a
l
u
t
e
r
o
t
o
n
i
c
m
e
d
i
c
a
t
i
o
n
,
n
o
r
i
n
l
a
b
o
r
a
t
o
r
y
P
P
H
i
n
d
i
c
a
t
o
r
s
U
t
e
r
i
n
e
m
a
s
s
a
g
e
r
e
q
u
i
r
e
d
i
n
4
3
.
4
%
v
s
.
6
2
.
3
%
(
p
<
0
.
0
2
5
)
L
e
u
n
g
e
t
a
l
.
1
7
2
0
0
6
D
o
u
b
l
e
-
b
l
i
n
d
R
C
T
L
o
w
-
r
i
s
k
,
v
a
g
i
n
a
l
d
e
l
i
v
e
r
y
(
n
=
3
2
9
)
C
a
r
b
e
t
o
c
i
n
1
0
0
g
I
M
(
n
=
1
6
5
)
v
s
.
S
y
n
t
o
m
e
t
r
i
n
e
I
M
(
n
=
1
6
4
)
a
f
t
e
r
d
e
l
i
v
e
r
y
o
f
i
n
f
a
n
t
N
o
d
i
f
f
e
r
e
n
c
e
i
n
d
r
o
p
o
f
h
e
m
o
g
l
o
b
i
n
(
1
.
4
v
s
.
1
.
5
g
/
d
l
)
,
o
r
a
d
d
i
t
i
o
n
a
l
u
t
e
r
o
t
o
n
i
c
a
g
e
n
t
s
(
8
.
7
%
v
s
.
6
.
7
%
)
S
i
g
n
i
f
i
c
a
n
t
l
o
w
e
r
i
n
c
i
d
e
n
c
e
o
f
n
a
u
s
e
a
(
R
R
0
.
1
8
,
9
5
%
C
I
0
.
0
4
0
.
7
8
)
,
v
o
m
i
t
i
n
g
(
R
R
0
.
1
,
9
5
%
C
I
0
.
0
1
0
.
7
4
)
,
h
y
p
e
r
t
e
n
s
i
o
n
a
t
3
0
m
i
n
(
p
<
0
.
0
1
)
a
n
d
6
0
m
i
n
(
p
<
0
.
0
5
)
H
i
g
h
e
r
i
n
c
i
d
e
n
c
e
o
f
t
a
c
h
y
c
a
r
d
i
a
(
R
R
1
.
6
8
,
9
5
%
C
I
1
.
0
3
3
.
5
7
)
N
g
a
n
e
t
a
l
.
2
7
2
0
0
7
R
e
t
r
o
s
p
e
c
t
i
v
e
s
t
u
d
y
L
o
w
-
r
i
s
k
,
v
a
g
i
n
a
l
d
e
l
i
v
e
r
y
(
n
=
1
1
8
)
C
a
r
b
e
t
o
c
i
n
1
0
0
g
I
M
v
s
.
I
M
c
o
m
b
i
n
a
t
i
o
n
o
f
o
x
y
t
o
c
i
n
5
I
U
a
n
d
e
r
g
o
m
e
t
r
i
n
e
0
.
2
m
g
i
m
m
e
d
i
a
t
e
l
y
a
f
t
e
r
i
n
f
a
n
t
d
e
l
i
v
e
r
y
M
e
a
n
b
l
o
o
d
l
o
s
s
3
8
8
v
s
.
5
5
1
(
p
=
0
.
0
1
)
B
l
o
o
d
l
o
s
s
5
0
0
m
l
w
a
s
2
1
.
4
%
v
s
.
4
3
.
5
%
(
p
=
0
.
0
1
)
a
n
d
b
l
o
o
d
l
o
s
s
1
0
0
0
m
l
w
a
s
1
.
8
%
v
s
.
1
4
.
5
%
(
p
=
0
.
0
2
)
N
i
r
m
a
l
a
e
t
a
l
.
1
6
2
0
0
9
R
a
n
d
o
m
i
z
e
d
c
o
n
t
r
o
l
l
e
d
s
t
u
d
y
H
i
g
h
-
r
i
s
k
f
o
r
P
P
H
,
v
a
g
i
n
a
l
d
e
l
i
v
e
r
y
(
n
=
1
2
0
)
C
a
r
b
e
t
o
c
i
n
1
0
0
g
I
M
(
n
=
6
0
)
v
s
.
S
y
n
t
o
m
e
t
r
i
n
e
I
M
(
n
=
6
0
)
i
m
m
e
d
i
a
t
e
l
y
a
f
t
e
r
i
n
f
a
n
t
d
e
l
i
v
e
r
y
N
o
d
i
f
f
e
r
e
n
c
e
i
n
r
e
q
u
i
r
e
m
e
n
t
f
o
r
a
d
d
i
t
i
o
n
a
l
o
x
y
t
o
c
i
c
a
g
e
n
t
,
t
i
m
e
i
n
t
e
r
v
a
l
t
o
w
e
l
l
c
o
n
t
r
a
c
t
e
d
u
t
e
r
u
s
,
b
l
o
o
d
t
r
a
n
s
f
u
s
i
o
n
,
a
d
v
e
r
s
e
e
f
f
e
c
t
o
r
c
o
m
p
l
i
c
a
t
i
o
n
s
S
i
g
n
i
f
i
c
a
n
t
l
y
l
o
w
e
r
m
e
a
n
b
l
o
o
d
l
o
s
s
i
n
c
a
r
b
e
t
o
c
i
n
g
r
o
u
p
(
2
4
4
1
1
4
m
l
v
s
.
3
4
3
1
4
3
m
l
,
9
5
%
C
I
5
2
1
4
6
m
l
)
S
i
g
n
i
f
i
c
a
n
t
r
e
d
u
c
e
d
d
r
o
p
i
n
h
e
m
o
g
l
o
b
i
n
i
n
c
a
r
b
e
t
o
c
i
n
g
r
o
u
p
(
0
.
3
0
.
2
g
/
d
l
v
s
.
0
.
4
0
.
2
g
/
d
l
,
9
5
%
C
I
0
.
1
0
.
2
)
S
u
e
t
a
l
.
+
2
8
2
0
0
9
D
o
u
b
l
e
-
b
l
i
n
d
R
C
T
L
o
w
-
r
i
s
k
,
v
a
g
i
n
a
l
d
e
l
i
v
e
r
y
(
n
=
3
7
0
)
C
a
r
b
e
t
o
c
i
n
1
0
0
g
I
M
(
n
=
1
8
5
)
v
s
.
S
y
n
t
o
m
e
t
r
i
n
e
I
M
(
n
=
1
8
5
)
i
m
m
e
d
i
a
t
e
l
y
a
f
t
e
r
i
n
f
a
n
t
d
e
l
i
v
e
r
y
N
o
d
i
f
f
e
r
e
n
c
e
i
n
r
e
q
u
i
r
e
m
e
n
t
f
o
r
a
d
d
i
t
i
o
n
a
l
o
x
y
t
o
c
i
c
a
g
e
n
t
,
b
l
o
o
d
l
o
s
s
o
r
i
n
c
i
d
e
n
c
e
o
f
P
P
H
W
o
m
e
n
w
h
o
h
a
d
S
y
n
t
o
m
e
t
r
i
n
e
w
e
r
e
f
o
u
r
t
i
m
e
s
m
o
r
e
l
i
k
e
l
y
t
o
e
x
p
e
r
i
e
n
c
e
n
a
u
s
e
a
(
R
R
4
.
2
,
9
5
%
C
I
2
.
2
7
.
8
)
a
n
d
v
o
m
i
t
i
n
g
(
R
R
4
.
3
,
9
5
%
C
I
1
.
9
9
.
5
)
.
T
r
e
m
o
r
,
s
w
e
a
t
i
n
g
,
r
e
t
c
h
i
n
g
a
n
d
u
t
e
r
i
n
e
p
a
i
n
w
e
r
e
a
l
s
o
m
o
r
e
l
i
k
e
l
y
i
n
t
h
e
S
y
n
t
o
m
e
t
r
i
n
e
g
r
o
u
p
(
p
<
0
.
0
5
)
R
C
T
,
r
a
n
d
o
m
i
z
e
d
c
o
n
t
r
o
l
l
e
d
t
r
i
a
l
T
a
b
l
e
2
S
t
u
d
i
e
s
w
i
t
h
c
a
r
b
e
t
o
c
i
n
a
f
t
e
r
v
a
g
i
n
a
l
d
e
l
i
v
e
r
y
Because of its long duration of action relative to oxytocin,
uterine contractions produced by carbetocin cannot be
stopped by simply discontinuing the medication. Therefore,
carbetocin should not be administered prior to delivery of the
infant for any reason, including elective or medical induction
of labour. Inappropriate use of carbetocin during pregnancy
could theoretically mimic the symptoms of oxytocin over-
dosage, including hyperstimulation of the uterus with strong
(hypertonic) or prolonged (tetanic) contractions, tumultuous
labour, uterine rupture, cervical and vaginal lacerations,
postpartum hemorrhage, utero-placental hypoperfusion and
variable deceleration of fetal heart, fetal hypoxia, hypercapnia,
or death. Carbetocin should not be used in patients with a
history of hypersensitivity to oxytocin or carbetocin.
Carbetocin should not be used in patients with vascular dis-
ease, especially coronary artery disease, except with extreme
caution. Carbetocin is not intended for use in children.
CARBETOCIN TODAY
In email correspondence with Ferring Pharmaceuticals
in July 2011, the authors were informed that carbe-
tocin has been available for clinical use since the year
of 2000. Today, carbetocin is approved in 23 countries
for the prevention or treatment of uterine atony
5
.
Of these, Canada has undertaken a leading role in
carbetocin research, including the largest randomized
controlled trial executed to date
9
. As a consequence,
the Society of Obstetricians and Gynaecologists of
Canada (SOGC) in their 2009 guidelines on the active
management of the third stage of labor
1
, released the
following recommendations:
6. Carbetocin, 100 g given as an IV bolus over 1 minute,
should be used instead of continuous oxytocin infusion in
elective Caesarean section for the prevention of PPH and to
decrease the need for therapeutic uterotonics. (I-B)
7. For women delivering vaginally with 1 risk factor for PPH,
carbetocin 100 g IM decreases the need for uterine massage
to prevent PPH when compared with continuous infusion of
oxytocin. (I-B)
This means that, for cesarean delivery performed in
Canada under regional anesthesia, carbetocin is the
first choice as a uterotonic agent. It is also recom-
mended for vaginal deliveries with increased risk for
PPH. How frequent these recommendations are being
followed is yet to be assessed, as it is recognized that
the practice varies across the country.
COST-EFFECTIVENESS
British data from 2010 states that one ampoule of
carbetocin 100 g costs 17.64, whereas one ampoule
of oxytocin 10 IU costs 0.86
23
. Although it is
significantly more expensive, other factors must be
considered. Among these, only one ampoule of
carbetocin would be used in a successfully treated
patient, whereas an average of 24 ampoules of
oxytocin would be necessary to supply a continuous
infusion.
A Mexican study from 2006 analysed the overall
cost to treat women with carbetocin compared with
oxytocin
21
. The use of resources was obtained from a
clinical trial involving 152 women with high risk for
PPH who underwent cesarean delivery. The cost was
calculated using the financial information provided by
the Mexican Institute of Social Security, which is
the third party payer. Their finding was that women
treated with carbetocin cost less to the health care sys-
tem than those treated with oxytocin (US dollars 3525
vs. US dollars 4054)
21
. One could infer that this is due
to a decrease in the necessity for additional uterotonic,
blood products and faster hospital discharge. How-
ever, at this point this inference cannot be confirmed.
These data were accurate for Mexico at the time of the
study, but a similar benefit with carbetocin in other
settings could be expected.
The ease of administration and the potentially
lower overall cost with a greater efficacy could
become the basis of a wider use of carbetocin for the
prevention of PPH, especially in low-resource areas.
However, because the manufacturer recommends
carbetocin to be stored at temperatures of 28C, this
requirement may preclude its more widespread use in
poorly resourced areas where 24 h access to reliable
sources of electricity is problematic. Carbetocin in a
room temperature formulation would potentially
increase its usefulness in such countries. To date, no
data have been published on drug stability at room
temperature
REMAINING QUESTIONS
Although current data suggest that carbetocin can be
more effective than oxytocin in the prevention of
PPH, studies to date have not focused on the
hemodynamic effects of this agent. The practice of
administering oxytocin as a bolus has been discouraged
due to its hemodynamic effects
3,8,9
. At the same time,
current recommendations of carbetocin, which is an
oxytocin analogue with agonistic properties at the
same receptors, state that this drug should be given as a
single IV bolus. The only caveat is that the recommen-
dation is for a slow IV bolus administered over a 1 min
duration. This is not based on clinical data, but
presumably on extrapolation from findings with
oxytocin
29,30
.
The safety of carbetocin for use in patients with
vascular disease as well as coronary disease has not
been tested. Similarly, no studies were performed on
patients under general anesthesia. Although there is no
clear reason that would preclude the use of carbetocin
in women under a general anesthetic, the lack of
clinical trials accounts for the manufacturers
366
POSTPARTUM HEMORRHAGE
>20% <20% and >10% <10% and >5% <5%
Abdominal pain
Nausea
Flushing
Feeling of warmth
Headache
Tremors
Pruritus
Shortness of breath
Vomiting
Metalic taste
Back pain
Sweating
Dizziness
Table 3 Side-effects associated with carbetocin and frequency of
occurence
recommendation of using this drug only in women
who are not anesthetized or who are only under
regional or local anesthesia
11
.
Further analysis is warranted to assess the cost-
effectiveness of carbetocin. Should the Mexican study
findings
21
be replicated in different settings, this will
further justify the use of carbetocin as a first choice of
uterotonic agent. In addition, the drug stability at
room temperature remains unclear.
Finally, the optimal dose of carbetocin is still to be
determined. In the case of oxytocin, initial IV doses as
low as 0.5 IU are effective in providing adequate uter-
ine contractility at elective cesarean delivery
31
. Extrap-
olating the findings for carbetocin, it is reasonable to
assume that 100 g, which is equivalent to 5 IU of
oxytocin according to animal data
13
, is considerably
more than the minimum necessary. This is especially
true if the suggestions that the human uterus is more
sensitive to carbetocin than the rat myometrium are
accurate
7,13
. In addition, similarly to oxytocin,
carbetocin will have to be evaluated in different clini-
cal scenarios, namely non-laboring elective cesarean
section, urgent/emergent cesarean section on laboring
women and vaginal delivery. Its usefulness in the area
of medical interruptions of pregnancy remains to be
investigated.
CONCLUSIONS
Carbetocin is a synthetic oxytocin analogue. It com-
bines the quick onset of oxytocin with the long-acting
effect of ergometrine. Compared with oxytocin, it
reduces the necessity of uterotonic intervention with
similar incidence of side-effects; compared with a
combination of oxytocin and ergometrine, it is as
effective with fewer side-effects, namely nausea, vom-
iting and hypertension. According to the Society of
Obstetricians and Gynaecologists of Canada, it should
be the first choice of uterotonic agent to prevent PPH
at elective cesarean delivery under regional anesthesia.
It is also suggested that it should be used in women at
risk for PPH after vaginal delivery.
References
1. Leduc D, Senikas V, Lalonde A, et al. Active management of
the third stage of labour: prevention and treatment of post-
partum hemorrhage. J Obstet Gynaecol Can 2009;31:98093
2. World Health Organization. Recommendations for the Pre-
vention of Postpartum Haemorrhage. WHO/MPS/07.06.
Geneva: WHO, 2007
3. Peters NCJ, Duvekot JJ. Carbetocin for the prevention of
postpartum hemorrhage: a systematic review. Obstet Gynecol
Surv 2009;64:12935
4. Vercauteren M, Palit S, Soetens F, Jacquemyn Y, Alahuhta S.
Anaesthesiological considerations on tocolytic and uterotonic
therapy in obstetrics. Acta Anaesthesiol Scand 2009;53:7019
5. Rath W. Prevention of postpartum haemorrhage with the
oxytocin analogue carbetocin. Eur J Obstet Gynecol Reprod
Biol 2009;147:1520
6. Barth T, Krejci I, Kupkova B, Jost K. Pharmacology of cyclic
analogues of deamino-oxytocin not containing a disulphide
bond (carba analogues). Eur J Pharmacol 1973;24:1838
7. Atke A, Vilhardt H. Uterotonic activity and myometrial
receptor affinity of 1-deamino-1-carba-2-tyrosine(O-
methyl)-oxytocin. Acta Endocrinol (Copenh) 1987;115:
15560
8. Moran C, Ni Bhuinneain M, Geary M, Cunningham S,
McKenna P, Gardiner J. Myocardial ischaemia in normal
patients undergoing elective Caesarean section: a peripartum
assessment. Anaesthesia 2001;56:10518
9. Dansereau J, Joshi K, Helewa ME, et al. Double-blind com-
parison of carbetocin versus oxytocin in prevention of uterine
atony after cesarean section. Am J Obstet Gynecol 1999;180:
6706
10. van Dongen PWJ, Verbruggen MM, Groot AN de,
Roosmalen J van, Sporken JM, Schulz M. Ascending dose
tolerance study of intramuscular carbetocin administered after
normal vaginal birth. Eur J Obstet Gynecol Reprod Biol
1998;77:1817
11. Ferring Inc. Product monograph: Duratocin (Carbetocin
Injection). 2006
12. Dyer RA, Dyk D van, Dresner A. The use of uterotonic
drugs during caesarean section. Int J Obstet Anesth 2010;19:
3139
13. Hunter DJS, Schulz P, Wassenaar W. Effect of carbetocin , a
long-acting oxytocin analog on the postpartum uterus. Clin
Pharmacol Ther 1992;52:607
14. Engstrm T, Barth T, Melin P, Vilhardt H. Oxytocin
receptor binding and uterotonic activity of carbetocin
and its metabolites following enzymatic degradation. Eur J
Pharmacol 1998;355:20310
15. Sweeney G, Holbrook AM, Levine M, et al. Pharma-
cokinetics of carbetocin, a long-acting oxytocin analogue, in
nonpregnant women. Curr Ther Res 1990;47:52840
16. Nirmala K, Zainuddin AA, Ghani NAA, Zulkifli S,
Jamil MA. Carbetocin versus syntometrine in prevention of
post-partum hemorrhage following vaginal delivery. J Obstet
Gynaecol Res 2009;35:4854
17. Leung SW, Ng PS, Wong WY, Cheung TH. A randomised
trial of carbetocin versus syntometrine in the management of
the third stage of labour. BJOG 2006;113:145964
18. Boucher M, Durocher F, Schulz P, Wassenaar W. Carbetocin
to produce uterine contraction during Cesarean-section. A
dose-ranging study. Proceedings of the 11th Annual Meeting
- Society of Perinatal Obstetricians; 1991 Jan 28-Feb 02; San
Francisco, CA, USA. Abstract #556
19. Barton SR, Jackson A. The safety and efficiency of carbetocin
to control uterine bleeding following caesarean section.
Prenat Neonat Med 1996;1:185
20. Boucher M, Horbay GL, Griffin P, et al. Double-blind, ran-
domized comparison of the effect of carbetocin and oxytocin
on intraoperative blood loss and uterine tone of patients
undergoing cesarean section. J Perinatol 1998;18:2027
21. Del Angel-Garcia G, Garcia-Contreras F, Constantino-Casas
P. Economic evaluation of carbetocine for the prevention of
uterine atony in patients with risk factors in Mexico. Value
Health 2006;9:A254
22. Borruto F, Treisser A, Comparetto C. Utilization of
carbetocin for prevention of postpartum hemorrhage after
cesarean section: a randomized clinical trial. Arch Gynecol
Obstet 2009;280:70712
23. Attilakos G, Psaroudakis D, Ash J, et al. Carbetocin versus
oxytocin for the prevention of postpartum haemorrhage
following caesarean section: the results of a double-blind
randomised trial. BJOG 2010;117:92936
24. Triopon G, Goron A, Agenor J, et al. Use of carbetocin in
prevention of uterine atony during cesarean section. Compar-
ison with oxytocin. Gynecol Obstet Fertil 2010;38:72934
25. Cordovani D, Balki M, Seaward G, Farine G, Carvalho JCA.
Carbetocin at elective cesarean delivery: a randomized con-
trolled trial to determine the effective dose. Can J Anesth
2012;in press
26. Boucher M, Nimrod CA, Tawagi GF, Meeker TA, Rennicks
White RE, Varin J. Comparison of carbetocin and oxytocin
for the prevention of postpartum hemorrhage following
367
Carbetocin for the Prevention of Postpartum Hemorrhage
vaginal delivery: a double-blind randomized trial. J Obstet
Gynaecol Can 2004;26:4818
27. Ngan L, Keong W, Martins R. Carbetocin versus a combina-
tion of oxytocin and ergometrine in control of postpartum
blood loss. Int J Gynaecol Obstet 2007;97:1523
28. Su LL, Rauff M, Chan YH, et al. Carbetocin versus
syntometrine for the third stage of labour following vaginal
deliverya double-blind randomised controlled trial. BJOG
2009;116:14616
29. Thomas JS, Koh SH, Cooper GM. Haemodynamic effects of
oxytocin given as i.v. bolus or infusion on women undergo-
ing Caesarean section. Br J Anaesth 2007;98:1169
30. Tsen LC, Balki M. Oxytocin protocols during cesarean deliv-
ery: time to acknowledge the risk/benefit ratio? Int J Obstet
Anesth 2010;19:2435
31. Carvalho JC, Balki M, Kingdom J, Windrim R. Oxytocin
requirements at elective cesarean delivery: a dose-finding
study. Obstet Gynecol 2004;104:100510
368
POSTPARTUM HEMORRHAGE
Anda mungkin juga menyukai
- Absolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationDari EverandAbsolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationBelum ada peringkat
- Carbetocin For The Prevention of Postpartum HemorrhageDokumen8 halamanCarbetocin For The Prevention of Postpartum HemorrhageLeslie GuzmanBelum ada peringkat
- Esophageal Preservation and Replacement in ChildrenDari EverandEsophageal Preservation and Replacement in ChildrenAshwin PimpalwarBelum ada peringkat
- Carbetocin For The Prevention of Postpartum Hemorrhage A Systematic ReviewDokumen7 halamanCarbetocin For The Prevention of Postpartum Hemorrhage A Systematic ReviewOscar Gregorio Coronado MacdanielBelum ada peringkat
- CarbetocinDokumen9 halamanCarbetocinNovii NoviiBelum ada peringkat
- Tabl 2018Dokumen7 halamanTabl 2018Mega Restia 2016Belum ada peringkat
- CarbetocinDokumen23 halamanCarbetocinAulia RahmaBelum ada peringkat
- Carbetocin Versus Oxytocin For The Prevention of Postpartum Haemorrhage Following Caesarean Section: The Results of A Double-Blind Randomised TrialDokumen8 halamanCarbetocin Versus Oxytocin For The Prevention of Postpartum Haemorrhage Following Caesarean Section: The Results of A Double-Blind Randomised TrialNawis WibowoBelum ada peringkat
- Effective uterotonics for postpartum hemorrhage preventionDokumen13 halamanEffective uterotonics for postpartum hemorrhage preventionNicole Andrea Silva GaeteBelum ada peringkat
- Update On The New Modalities On The Prevention and PDFDokumen20 halamanUpdate On The New Modalities On The Prevention and PDFSamuel SammyBelum ada peringkat
- Regla de Los Tres Algoritmo Vs Infusion Continua de Oxitocina Durante Cesarea Electiva-3 - 537Dokumen9 halamanRegla de Los Tres Algoritmo Vs Infusion Continua de Oxitocina Durante Cesarea Electiva-3 - 537Ailed HerediaBelum ada peringkat
- 12-Uterotonic and Tocolytic Drugs (R Dyer) PDFDokumen6 halaman12-Uterotonic and Tocolytic Drugs (R Dyer) PDFJTBelum ada peringkat
- The Prevention and Treatment of Postpartum Haemorrhage: What Do We Know, and Where Do We Go To Next?Dokumen9 halamanThe Prevention and Treatment of Postpartum Haemorrhage: What Do We Know, and Where Do We Go To Next?Adipta KurniawanBelum ada peringkat
- Utero Toni CosDokumen13 halamanUtero Toni CosPedro PachecoBelum ada peringkat
- Jurnal Maternitas 3 EnglishDokumen5 halamanJurnal Maternitas 3 EnglishmesiBelum ada peringkat
- Higher-Dose Oxytocin for Postpartum HemorrhageDokumen13 halamanHigher-Dose Oxytocin for Postpartum HemorrhageBella DirkBelum ada peringkat
- Standardization of Chemotherapy and Individual Dosing of Platinum CompoundsDokumen6 halamanStandardization of Chemotherapy and Individual Dosing of Platinum CompoundsJesse Helmut Hansen-BartelBelum ada peringkat
- Paracetamol A Review of Three Routes of AdministrationDokumen3 halamanParacetamol A Review of Three Routes of AdministrationMohd MiqdamBelum ada peringkat
- Preventing Postpartum Hemorrhage with CarbetocinDokumen4 halamanPreventing Postpartum Hemorrhage with CarbetocinNadeem AlamgirBelum ada peringkat
- Harmancrowell2019 1Dokumen6 halamanHarmancrowell2019 1enggarBelum ada peringkat
- Hum. Reprod.-2005-Homburg-2043-51 (CC End of An Era)Dokumen9 halamanHum. Reprod.-2005-Homburg-2043-51 (CC End of An Era)Kinjal ShahBelum ada peringkat
- Oxytocin Protocols for Cesarean DeliveryDokumen19 halamanOxytocin Protocols for Cesarean DeliveryJuragoma100% (1)
- W 3 e WDDokumen6 halamanW 3 e WDsupaidi97Belum ada peringkat
- 2015 Article 20Dokumen7 halaman2015 Article 20ardianBelum ada peringkat
- Peska 2020Dokumen6 halamanPeska 2020Abraham MedinaBelum ada peringkat
- Anesthetizing The Obese.1Dokumen3 halamanAnesthetizing The Obese.1SoniJfreeBelum ada peringkat
- Obstetrics 2Dokumen6 halamanObstetrics 2Kartika AnggakusumaBelum ada peringkat
- Evidence Based NursingDokumen7 halamanEvidence Based NursingLloyd Adrian GaffudBelum ada peringkat
- Fluid Overload in Children With Severe Sepsis and Septic ShockDokumen3 halamanFluid Overload in Children With Severe Sepsis and Septic Shockaaron tabernaBelum ada peringkat
- AntepartumDokumen2 halamanAntepartumchel_0520Belum ada peringkat
- Multiple-Dose Acetaminophen Pharmacokinetics: Ayres"Dokumen6 halamanMultiple-Dose Acetaminophen Pharmacokinetics: Ayres"did youBelum ada peringkat
- Evaluates Administration of Oxytocin Drug in Maternity and Its Implications: Short Article ReviewDokumen7 halamanEvaluates Administration of Oxytocin Drug in Maternity and Its Implications: Short Article Reviewindex PubBelum ada peringkat
- Clinical Study: Effects of A New Patient Safety-Driven Oxytocin Dosing Protocol On Postpartum HemorrhageDokumen5 halamanClinical Study: Effects of A New Patient Safety-Driven Oxytocin Dosing Protocol On Postpartum HemorrhageRatih Kusuma DewiBelum ada peringkat
- Introduction: Intravenous Ibuprofen May Offer Advantages Over Ketorolac For Postoperative Pain ControlDokumen6 halamanIntroduction: Intravenous Ibuprofen May Offer Advantages Over Ketorolac For Postoperative Pain ControlnadaBelum ada peringkat
- Current Controversies With Oral Emergency Contraception: A ReviewDokumen19 halamanCurrent Controversies With Oral Emergency Contraception: A ReviewNEHEMIAS PAYARESBelum ada peringkat
- 2020, Ibrahim, Carbetocin Versus Oxytocin For Prevention of Postpartum Hemorrhage in Hypertensive Women Undergoing Elective Cesarean SectionDokumen8 halaman2020, Ibrahim, Carbetocin Versus Oxytocin For Prevention of Postpartum Hemorrhage in Hypertensive Women Undergoing Elective Cesarean SectionHAVIZ YUADBelum ada peringkat
- 10 1097@ftd 0b013e3181898b6f PDFDokumen8 halaman10 1097@ftd 0b013e3181898b6f PDFintan wahyuBelum ada peringkat
- Oxytocin Use in Labor: Legal ImplicationsDokumen9 halamanOxytocin Use in Labor: Legal ImplicationsGustavo flores quispeBelum ada peringkat
- Aogs 95 501 PDFDokumen4 halamanAogs 95 501 PDFIrfanBelum ada peringkat
- Retained PlacentaDokumen4 halamanRetained PlacentaNinanu Nida-nnBelum ada peringkat
- Jurnalll MisoDokumen5 halamanJurnalll MisoBayu WijanarkoBelum ada peringkat
- Current Trends in ObstetricsDokumen6 halamanCurrent Trends in ObstetricsShyrra Edades Pinder100% (1)
- Tocolisis Aguda PDFDokumen6 halamanTocolisis Aguda PDFRolando DiazBelum ada peringkat
- Postpartum Hemorrhage in The Developed World: Whither Misoprostol?Dokumen3 halamanPostpartum Hemorrhage in The Developed World: Whither Misoprostol?Tracy VillegasBelum ada peringkat
- Evidence-Based Labor Management 05Dokumen12 halamanEvidence-Based Labor Management 05Samir CastilloBelum ada peringkat
- Refractory Uterine Atony-Still A Problem After All These YearsDokumen9 halamanRefractory Uterine Atony-Still A Problem After All These YearsIndah 15Belum ada peringkat
- Albumin Delivery Improves Breast Cancer TherapyDokumen3 halamanAlbumin Delivery Improves Breast Cancer TherapyAnjum AfzalBelum ada peringkat
- Reply From The Authors - Bja - 16Dokumen2 halamanReply From The Authors - Bja - 16RENAULTBelum ada peringkat
- Anesthesia For The Pregnant Cat and DogDokumen5 halamanAnesthesia For The Pregnant Cat and DogDiajeng Galuh RiesantiBelum ada peringkat
- Intravenous Infusion of Paracetamol For Intrapartum AnalgesiaDokumen6 halamanIntravenous Infusion of Paracetamol For Intrapartum AnalgesiaDaniel Rincón VillateBelum ada peringkat
- Caesarean DeliveryDokumen207 halamanCaesarean Deliverynsaid007Belum ada peringkat
- Aromatase Inhibitors For Ovulation Induction and Ovarian StimulationDokumen13 halamanAromatase Inhibitors For Ovulation Induction and Ovarian StimulationGinecologia Aseptică 1Belum ada peringkat
- Case ReportDokumen5 halamanCase ReportMira WardhaniBelum ada peringkat
- Clinical Study: Safety and Efficacy of Misoprostol Versus Oxytocin For The Prevention of Postpartum HemorrhageDokumen5 halamanClinical Study: Safety and Efficacy of Misoprostol Versus Oxytocin For The Prevention of Postpartum HemorrhageTasya Arsy LiyanaBelum ada peringkat
- Clinical Study: Safety and Efficacy of Misoprostol Versus Oxytocin For The Prevention of Postpartum HemorrhageDokumen5 halamanClinical Study: Safety and Efficacy of Misoprostol Versus Oxytocin For The Prevention of Postpartum HemorrhageMuhammad Ghifari RifanshaBelum ada peringkat
- Acute TocolysisDokumen6 halamanAcute Tocolysisverogalung100% (1)
- B85. gui235CPG0910Dokumen7 halamanB85. gui235CPG0910jhon heriansyahBelum ada peringkat
- fsrh-ceu-statement-response-to-edelman-2022-aug22Dokumen3 halamanfsrh-ceu-statement-response-to-edelman-2022-aug22mirunahorgaBelum ada peringkat
- Randomized Controlled Multicentre Study of Albumin Replacement Therapy in Septic Shock (ARISS) : Protocol For A Randomized Controlled TrialDokumen13 halamanRandomized Controlled Multicentre Study of Albumin Replacement Therapy in Septic Shock (ARISS) : Protocol For A Randomized Controlled TrialntnquynhproBelum ada peringkat
- Report of A Case Treated With Acetylbetah (Ethylcholine Broi IdeDokumen8 halamanReport of A Case Treated With Acetylbetah (Ethylcholine Broi IdeKartika AnggakusumaBelum ada peringkat
- Osteoporosis: Pathophysiology and Clinical ManagementDokumen628 halamanOsteoporosis: Pathophysiology and Clinical ManagementKartika AnggakusumaBelum ada peringkat
- Selective Serotonin Reuptake Inhibitor Poisoning: An Evidence-Based Consensus Guideline For Out-Ofhospital Management.Dokumen19 halamanSelective Serotonin Reuptake Inhibitor Poisoning: An Evidence-Based Consensus Guideline For Out-Ofhospital Management.Kartika AnggakusumaBelum ada peringkat
- Final Indonesia Adult ImmunizationRecommendation 2013Dokumen3 halamanFinal Indonesia Adult ImmunizationRecommendation 2013Monica ZhangBelum ada peringkat
- Comparison of Renal Function Between Cyanotic and Acyanotic Congenital Heart Disease in Children and AdolescentDokumen9 halamanComparison of Renal Function Between Cyanotic and Acyanotic Congenital Heart Disease in Children and AdolescentKartika AnggakusumaBelum ada peringkat
- Obstetrics 2Dokumen6 halamanObstetrics 2Kartika AnggakusumaBelum ada peringkat
- Fascial PalsyDokumen65 halamanFascial PalsyKartika AnggakusumaBelum ada peringkat
- Hirschsprung's DiseaseDokumen7 halamanHirschsprung's DiseaseKartika AnggakusumaBelum ada peringkat
- Age Ageing 2014 Ngo Ageing Afu143Dokumen9 halamanAge Ageing 2014 Ngo Ageing Afu143Kartika AnggakusumaBelum ada peringkat
- Treatment of Depression in Patients With EpilepsyDokumen9 halamanTreatment of Depression in Patients With EpilepsyKartika AnggakusumaBelum ada peringkat
- Carbetocin for Prevention of Postpartum HaemorrhageDokumen6 halamanCarbetocin for Prevention of Postpartum HaemorrhageKartika AnggakusumaBelum ada peringkat
- Decreased CD4 1 Lymphocytes and Innateimmune Responses in Adults With Previousextrapulmonary TuberculosisDokumen8 halamanDecreased CD4 1 Lymphocytes and Innateimmune Responses in Adults With Previousextrapulmonary TuberculosisKartika AnggakusumaBelum ada peringkat
- Cholinesterase Inhibitory of XanthoneDokumen5 halamanCholinesterase Inhibitory of XanthoneKartika AnggakusumaBelum ada peringkat
- Carbetocin in The Prevention of Postpartum HaemorrhageDokumen5 halamanCarbetocin in The Prevention of Postpartum HaemorrhageKartika AnggakusumaBelum ada peringkat
- Pharmalogical of Xanthones As CardiovascularDokumen12 halamanPharmalogical of Xanthones As CardiovascularKartika AnggakusumaBelum ada peringkat
- Posyandu LansiaDokumen9 halamanPosyandu LansiaKartika AnggakusumaBelum ada peringkat
- Pharmacological Effects of MangiferinDokumen6 halamanPharmacological Effects of MangiferinKartika AnggakusumaBelum ada peringkat
- Ada, 2007Dokumen6 halamanAda, 2007shinigamigirl69Belum ada peringkat
- 17 FullDokumen8 halaman17 FullKartika AnggakusumaBelum ada peringkat
- Pharmacological Effects of MangiferinDokumen6 halamanPharmacological Effects of MangiferinKartika AnggakusumaBelum ada peringkat
- Ballard ScoreDokumen1 halamanBallard ScoreFikriyah FuadiyahBelum ada peringkat
- Daftar PustakaDokumen3 halamanDaftar PustakaKartika AnggakusumaBelum ada peringkat
- Malaria AlgorithmDokumen1 halamanMalaria AlgorithmKartika AnggakusumaBelum ada peringkat
- PCOS InsulineDokumen14 halamanPCOS Insulinet3klaBelum ada peringkat
- WHO Grow Chart TB+U Girl 5-19Dokumen1 halamanWHO Grow Chart TB+U Girl 5-19Kartika AnggakusumaBelum ada peringkat
- AbstractDokumen18 halamanAbstractKartika AnggakusumaBelum ada peringkat
- Dubowitz ScoreDokumen3 halamanDubowitz ScorentadudulBelum ada peringkat
- Teva PharmaceuticalDokumen17 halamanTeva PharmaceuticalGanesh VedhachalamBelum ada peringkat
- Moist Heat Sterilization Validation and Requalification STERISDokumen4 halamanMoist Heat Sterilization Validation and Requalification STERISDany RobinBelum ada peringkat
- Loxapine PDFDokumen2 halamanLoxapine PDFDavid AdamsBelum ada peringkat
- PEBC Pharmacist Evaluation ExamDokumen238 halamanPEBC Pharmacist Evaluation ExamHerodotus100% (4)
- Sulphite SensitivityDokumen3 halamanSulphite SensitivityKrishan BhanotBelum ada peringkat
- Drugs Med-SurgTest 3Dokumen6 halamanDrugs Med-SurgTest 3Sarah PlunkettBelum ada peringkat
- Ayurvedic medicine for renal stonesDokumen3 halamanAyurvedic medicine for renal stoneshk_scribdBelum ada peringkat
- Cosmetic Vite hplc-4 PDFDokumen14 halamanCosmetic Vite hplc-4 PDFZahiroh Maulida A NBelum ada peringkat
- Evidence-based Injection Practice: To Aspirate or NotDokumen1 halamanEvidence-based Injection Practice: To Aspirate or NotElsion Goleci0% (1)
- CREW: Department of Health and Human Services: Public Affairs Firms Documents: 11/16/06 HHS/CMS FOIA Response 2 of 3Dokumen513 halamanCREW: Department of Health and Human Services: Public Affairs Firms Documents: 11/16/06 HHS/CMS FOIA Response 2 of 3CREWBelum ada peringkat
- Project Synopsis 123Dokumen3 halamanProject Synopsis 123Goutham KulkarniBelum ada peringkat
- CYMBALTA (Duloxetine HCL) Product Monograph For CanadaDokumen49 halamanCYMBALTA (Duloxetine HCL) Product Monograph For Canadajennabush100% (10)
- AnnexD.2 CertificationOfServiceDeliverySupport (Medicines)Dokumen3 halamanAnnexD.2 CertificationOfServiceDeliverySupport (Medicines)Arlyn DapulaBelum ada peringkat
- Various Drugs Used in Paediatric DentistryDokumen56 halamanVarious Drugs Used in Paediatric DentistryPo PowBelum ada peringkat
- Tapasya Product CatalogueDokumen104 halamanTapasya Product Cataloguethaonguyendc100% (1)
- Empr Prescriber's EditionDokumen420 halamanEmpr Prescriber's EditionPatel Pratyk100% (1)
- The High Cost of Prescription Drugs CausesDokumen5 halamanThe High Cost of Prescription Drugs Causesjuddy avottBelum ada peringkat
- Camphor WaterDokumen19 halamanCamphor WaterChristine RanoaBelum ada peringkat
- Guaiphenesin Insert SAMPLEDokumen4 halamanGuaiphenesin Insert SAMPLENj M. ZaraBelum ada peringkat
- Addii Biotech Third Party List - 2Dokumen2 halamanAddii Biotech Third Party List - 2Vicky VPNBelum ada peringkat
- Chemo Stability Chart - AtoKDokumen59 halamanChemo Stability Chart - AtoKAfifah Nur Diana PutriBelum ada peringkat
- ReferensiDokumen4 halamanReferensirinasiahaanBelum ada peringkat
- CyclosporineDokumen25 halamanCyclosporineraki9999Belum ada peringkat
- TTTTDokumen26 halamanTTTTMoataz TrabehBelum ada peringkat
- Metabical Harvard Case StudyDokumen56 halamanMetabical Harvard Case StudyVaibhav Singh100% (3)
- Essential Drug Concept and Its Implication in NepalDokumen5 halamanEssential Drug Concept and Its Implication in NepalB.pharm 16th BatchBelum ada peringkat
- Pharmaceutical Analysis I - TheoryDokumen3 halamanPharmaceutical Analysis I - TheoryHarit0% (1)
- Unwrapping LazarusDokumen24 halamanUnwrapping LazarusChosen Books100% (1)
- EtosuksimidDokumen14 halamanEtosuksimidMaharani IndriatyBelum ada peringkat
- As The CEO of Teva, Which Markets Would You Concentrate On Developing Going Forward?Dokumen12 halamanAs The CEO of Teva, Which Markets Would You Concentrate On Developing Going Forward?mGD1993Belum ada peringkat
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDari EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionPenilaian: 4 dari 5 bintang4/5 (402)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDari EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityPenilaian: 3.5 dari 5 bintang3.5/5 (2)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDari EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisPenilaian: 4 dari 5 bintang4/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDari EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedPenilaian: 5 dari 5 bintang5/5 (78)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDari EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityPenilaian: 4 dari 5 bintang4/5 (13)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDari EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBelum ada peringkat
- The Comfort of Crows: A Backyard YearDari EverandThe Comfort of Crows: A Backyard YearPenilaian: 4.5 dari 5 bintang4.5/5 (23)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDari EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsPenilaian: 3.5 dari 5 bintang3.5/5 (3)
- Techniques Exercises And Tricks For Memory ImprovementDari EverandTechniques Exercises And Tricks For Memory ImprovementPenilaian: 4.5 dari 5 bintang4.5/5 (40)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDari EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsPenilaian: 5 dari 5 bintang5/5 (1)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDari EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsPenilaian: 4.5 dari 5 bintang4.5/5 (169)
- The Obesity Code: Unlocking the Secrets of Weight LossDari EverandThe Obesity Code: Unlocking the Secrets of Weight LossPenilaian: 5 dari 5 bintang5/5 (4)
- The Ultimate Guide To Memory Improvement TechniquesDari EverandThe Ultimate Guide To Memory Improvement TechniquesPenilaian: 5 dari 5 bintang5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingDari EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingPenilaian: 5 dari 5 bintang5/5 (4)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDari EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDari EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsBelum ada peringkat
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisDari EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisPenilaian: 5 dari 5 bintang5/5 (8)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingDari EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingPenilaian: 3.5 dari 5 bintang3.5/5 (33)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Dari EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Penilaian: 4.5 dari 5 bintang4.5/5 (110)
- Summary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisDari EverandSummary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisPenilaian: 3 dari 5 bintang3/5 (2)
- The Happiness Trap: How to Stop Struggling and Start LivingDari EverandThe Happiness Trap: How to Stop Struggling and Start LivingPenilaian: 4 dari 5 bintang4/5 (1)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDari EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifePenilaian: 4.5 dari 5 bintang4.5/5 (253)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsDari EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsBelum ada peringkat
- The Tennis Partner: A Doctor's Story of Friendship and LossDari EverandThe Tennis Partner: A Doctor's Story of Friendship and LossPenilaian: 4.5 dari 5 bintang4.5/5 (4)