Ebpbpsummative
Diunggah oleh
api-252804976Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Ebpbpsummative
Diunggah oleh
api-252804976Hak Cipta:
Format Tersedia
Running head: DECREASING VAP
Decreasing Ventilator Associated Pneumonia in Critically Ill Patients
Brian Poirier
University of South Florida
DECREASING VAP
2
Abstract
Ventilator Associated Pneumonia (VAP) is the most common nosocomial infection in critically
ill, mechanically ventilated adult patients, resulting in increased hospital stays, healthcare costs
and mortality rates. The purpose of this paper is to develop an intervention to decrease the
prevalence of VAP. An EBP team was assembled to submit a proposal to act as a blueprint to
guide a team of EBP researchers and healthcare providers in a pilot study based on current
clinical guidelines and EBP research. Initially, a compilation of contemporary Randomized
Clinical Trials (RCTs) were analyzed and synthesized to develop an appropriate intervention.
The Cumulative Index to Nursing and Allied Health Literature (CINAHL) and the search engine
Pub Med were used to find potential RCTs; key words included: VAP, Chlorhexidine,
prevention, and oral care. A clinically significant intervention from the synthesis of three RCTs
was developed and implemented into a pilot study in critical care units over six months; the
incidence of VAP was compared to previous VAP incidence rates. Significant findings will be
applied to a new facility healthcare policy that will determine the standard care ordered for
mechanically ventilated patients.
DECREASING VAP
Decreasing Ventilator Associated Pneumonia in Critically Ill Patients
Ventilator Associated Pneumonia (VAP) is the most common nosocomial infection in
mechanically ventilated patients and results in increased hospital stays, healthcare costs and
mortality rates. Patients who acquire VAP are at risk for a 33% increase in mortality, increased
costs of $20,000-$40,000, and increased ICU time by up to 6 days (Kimberly Clark, 2013). Grap
et al. (2011) reported that up to 25% of ventilated patients acquire VAP during their admission
and VAP is responsible for 90% of nosocomial infections in this population. After reviewing
and synthesizing current Evidenced-Based Practice (EBP) literature, an intervention to decrease
the incidence of VAP was demonstrated in several Randomized Clinical Trials (RCTs) to
potentially be implemented in this facilitys healthcare policy. The EBP research team proposes
to implement an intervention after a pilot clinical trial to answer the following question: In
mechanically ventilated adult patients, how does the use of oral Chlorhexidine CHX treatments
compare to standard oral care in reducing the prevalence of VAP over a six month period?
To accomplish this proposal, the value of EBP research must be demonstrated to nurses,
physicians and healthcare providers to promote a culture of inquiry. Healthcare team members
will be offered membership to an EBP team and will have the opportunity to accept
responsibilities as EBP mentors; these mentors will increase EBP awareness throughout the
hospital through the use of multimedia projects, journal clubs, EBP training seminars, and
support in EBP research. Mentors will collaborate with facility administrators to ensure the
facility is equipped with the proper infrastructure to complete EBP research such as subscriptions
and access to current research and journals, access to databases (National Guideline
Clearinghouse and the Cochrane Library), and computer software and hardware (Melnyk &
Fineout-Overholt, 2011).
DECREASING VAP
4
Literature Search
Current (2009-present) literature was accessed and searched through the Cumulative
Index to Nursing and Allied Health Literature (CINAHL) and the search engine Pub Med. Key
words included in the search for relevant literature included: VAP, ICU, mechanically ventilated
patients, CHX, intubation and oral care.
Literature Review
The following RCTs were selected to synthesize and apply an intervention to a pilot
clinical trial based on their clinical significance, ease of implementation, and financial feasibility.
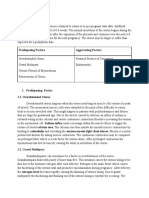
Table 1 contains an abbreviated list of included RCTs.
Grap et al. (2011) conducted a randomized, controlled clinical trial to determine whether
a single early administration of CHX to the oral cavity and oropharynx would reduce the
incidence of VAP by decreasing the amount of oral microbial flora. Patients were randomly
assigned to either the intervention (5mL application of a 0.12% CHX solution) or the control
group (no CHX). Seventy-one patients were placed in the intervention group and 74 were placed
in the control group. The entire oral cavity was swabbed, including the anterior and posterior
pharynx, gums, teeth, tongue, and buccal mucosa within 12 hours of intubation to a total of 145
trauma patients requiring mechanical ventilation. VAP was evaluated on admission, 48, and 72
hours after intubation by using a Clinical Pulmonary Infection Score (CPIS). CPIS data
(temperature, white blood cell count, tracheal secretions, oxygenation [PAO2/FIO2], chest
radiograph, and tracheal aspirate culture) were compared using a random effects, repeatedmeasures analysis of covariance model. A significant treatment effect from admission to 48
hours (p = 0.020) and to 72 hours (p = 0.027) was found. 55.6% of the patients in the control
DECREASING VAP
group without pneumonia prior to intubation developed VAP by 48 or 72 hours compared to
only 33.3% of the intervention patients (Grap et al., 2011). Strengths of the trial include
randomization, a simple and low cost intervention, and the clinically significant results. A
possible weakness is the relatively small sample size; more evidence could be attained through a
larger sample.
Kusahara and colleagues (2012) conducted a randomized-controlled trial to test the
effectiveness of oral care with a 0.12% CHX gel in decreasing VAP in critically ill children. The
clinical trial was conducted in a pediatric critical care unit over a 36 month period. The study
sample was composed of 96 mechanically ventilated children, 50 were randomly assigned to a
placebo (control) group and 46 randomly assigned to a CHX (intervention) group. The
intervention group received twice daily oral care with a dental gel containing CHX while the
control group received twice daily oral care with a placebo dental gel. The primary outcome
measure was the development of VAP. Secondary outcomes included: length of ventilation in the
PICU, length of stay in the PICU, mortality, and oral and tracheal colonization with
microorganisms. Microbiological analyses of oropharyngeal and tracheal secretions were
performed 24, 48, and 96 hours after intubation. 32.6% of the intervention group were diagnosed
with VAP, while 32.0% of the control group were diagnosed (p = 0.949). While the use of 0.12%
CHX was found not to be a significant modifier of VAP incidence, CHX oral care was found to
be protective against VAP in children without pathogenic microorganisms in their oropharynx 24
hours after mechanical ventilation (p = 0.019). The intervention did not influence mortality (p =
0.425), length of stay (p = 0.143), or time spent in intensive care (p = 0.177) (Kusahara et al.,
2012). The strengths of this trial include: trial randomization, double-blindness, similarity of
demographics in each group, and baseline clinical variables. Weaknesses include the small
DECREASING VAP
sample size. Although this RCT examines a pediatric population and the outcomes observed may
be difficult to compare to adult patients, the findings of Kusahara et al. (2012) confirm the use of
CHX as a means of VAP prevention.
zaka et al. (2012) conducted a randomized double blind controlled trial in which 61
dentate patients admitted to a respiratory ICU and scheduled for invasive mechanical ventilation
for at least 48 hours were evaluated for the effectiveness of oral swabbing with a 0.2% CHX
gluconate (CHX) solution in decreasing the risk of acquiring VAP. Patients were divided into
two groups: twenty-nine patients were provided oral care by swabbing the oral cavity four times
a day with the CHX solution and 32 patients served as the control group, being swabbed with a
saline solution four times a day. Each swabbing session lasted one minute. Periodontal
measurements (probing depth and bleeding on probing were performed at six sites: mesiobuccal, mid-buccal, disto-buccal, mesiolingual, mid-lingual and disto-lingual on each tooth
present) were recorded on admission and lower-respiratory-tract specimens were obtained for
microbiological analysis on admission and at the suspicion of pneumonia. VAP development
time and mortality rates were also recorded. VAP rates were significantly higher in the control
group (68.8%) when compared to the CHX group (41.4%, p = 0.03) (zaka et al., 2012). There
were no significant differences in the periodontal measurements, VAP development time, or
mortality rate between groups. The finding that oral swabbing with a CHX solution drastically
reduces the development of VAP in ventilated patients supports its use in critically ill patients.
The strengths of the study include trial randomization, double-blindness, and the effectiveness of
the intervention. Although a 0.2% CHX solution strength is not approved by the FDA in the
United States, this trial still has demonstrated the effectiveness of the application of CHX in the
prevention of VAP and should be included.
DECREASING VAP
The Institute for Clinical Systems Improvement (2011) advocates for the use of a 0.2%
CHX oral care solution in conjunction with several additional interventions to form a bundle of
VAP prevention interventions. Ancillary interventions include: elevating the head of the patient,
inflating and maintaining the endotracheal tube cuff to 20-25 mm Hg, using a heated and
humidified air supply, removal of tracheal secretions, sedation vacations, peptic ulcer
prophylaxis, and deep vein thrombosis prevention (The Institute for Clinical Systems
Improvement, 2011). When compared to the three RCTs in this proposal, the current clinical
guidelines agree to the use of CHX as an essential intervention in VAP prevention, but the
minimum required strength of solution is ambiguous. The United States Food and Drug
Administration (FDA) has not approved a 0.2% strength CHX solution, but a 0.12% strength
solution has demonstrated comparable results.
Synthesis
It has been empirically demonstrated in several RCTs, which included diverse sample
populations, that the application of a CHX solution to critically ill, mechanically ventilated
patients decreases the associated risk of acquiring VAP. Although Kusahara and colleagues
(2012) were not able to demonstrate that a 0.12% CHX solution was able significantly modify
the VAP incidence in a sample of mechanically ventilated children, the use of CHX was found to
be protective against VAP in a subset of children in the trial who did not already have potentially
pathogenic micro flora in their oropharynx 24 hours after mechanical ventilation. The children in
this subset who were administered CHX were noted to have a significant decrease in the
incidence of VAP. Though this proposal is designed for adult patients, the results of Kusahara et
al. (2012) complement the findings of Grap et al. (2011) and zaka et al. (2012) in the use of
CHX as a means of VAP prevention in adult clients.
DECREASING VAP
Both Kusahara et al. (2012) and Grap et al. (2011) have utilized and demonstrated the
effectiveness of a CHX solution strength of 0.12% as zaka et al. (2012) used a solution
strength that has not been approved by the FDA, it must be excluded from this proposal. Time
from intubation until treatment with CHX may be an overlooked factor in the prevention of
VAP. Grap et al.s (2011) time from intubation to treatment was 12 hours, which demonstrated a
lower incidence of VAP with a weaker solution strength, fewer applications, and less CHX
solution used than zaka et al. (2012) and Kusahara et al (2012). Early use of a CHX oral care
solution followed by repeated daily use may be most beneficial to remove potentially pathogenic
micro flora, by initially removing pathogens and preventing their growth over time while
intubated.
Proposed Practice Change
To prevent the incidence and decrease the prevalence of VAP in critically ill,
mechanically ventilated adult patients, current research and clinical practice guidelines suggest
the inclusion of a Chlorhexidine oral care solution regiment. Synthesized from three distinct
RCT treatment modalities, this proposal recommends a 5 ml early application (within 12 hours
of intubation) of a 0.12% strength solution of Chlorhexidine administered by a respiratory
therapist or nurse present at the intubation, followed by a twice daily foam swab application by
the attending nurse. A pilot study will be conducted to determine if this intervention is effective
and a health policy change will be enacted based on those results. As this EBP project relies on
the current best evidence and valid data, any practice recommendations may change based on the
outcomes of this proposed pilot study.
DECREASING VAP
9
Change Strategy
As stated previously, to encourage an atmosphere of inquiry EBP mentors will provide
EBP seminars, hold journal clubs, encourage administrative and manager inclusion in EBP
projects, provide poster presentations and increase the recognition of healthcare team members
involved in EBP projects. To promote staff engagement in this proposal, it is also recommended
that posters and pamphlets describing the trial be distributed to work stations in the critical care
units conducting the pilot trail. Additionally, EBP clinical rounds can be scheduled bi-weekly to
involve healthcare team members (Melnyk & Fineout-Overholt, 2011).
To implement the EBP research proposal into this facility, the Iowa Model of EBP to
promote quality care will be used. The Iowa model is commonly utilized in healthcare facilities
and guides clinicians through the typically non-linear structure of EBP research (Melnyk &
Fineout-Overholt, 2011.)
Roll Out Plan
May 2014 - Identification of clinical problem: Elevated rates of VAP detected in
critically ill, mechanically ventilated adult patients. This was deemed a top
priority in this healthcare facility; an EBP research team was assembled to
research the pathology of, and factors related to VAP.
June 2014 - The EBP research team gathered relevant EBP research and RCTs
and synthesized an appropriate intervention to implement. A pilot study was
developed with suitable measures and outcomes to implement in critical care
units.
July - December 2014 - Six month implementation of the CHX solution
intervention in critical care units and subsequent data collection and compilation.
DECREASING VAP
10
January 2015 Data collected from the pilot study will be analyzed and
evaluated; if a decrease in the incidence of VAP is clinically significant, the
intervention will be synthesized into a new health policy that can be tailored to
provide best practice care to patients at this facility. Results will be disseminated
within the healthcare facility by a practice change. Regionally, findings will be
presented by EBP mentors at future EBP conferences.
Project Evaluation
In order to determine the effects of a CHX solution on the incidence of VAP and compare
the intervention against current standard oral care, the EBP research team will review the
incidence rate of VAP in critically ill, mechanically ventilated adult patients before and after the
completion of the six month trial implementation of a 0.12% CHX oral care solution regimen.
RCTs cited in this proposal have recorded a decrease in the incidence of VAP in the
intervention groups ranging from 22.3% to 41.7% compared to control groups. Success of this
intervention will be confirmed by a minimum decrease in the incidence of VAP by 20%.
Diagnoses of VAP by infectious disease physicians will be recorded in a database by critical care
nurses. VAP diagnoses from previous standard oral care will be compared to the six month
implementation of the CHX oral care intervention by the EBP team members and mentors.
Dissemination of EBP
Clinically significant findings will be disseminated regionally by EBP mentors and
include poster viewings, oral presentations at EBP conferences, EBP research presentations in
regional hospitals, and hospital/organization-based professional committee meetings. As this
intervention is specific to mechanically ventilated adult patients, its implementation is restricted
to critical care units. EBP mentors may also provide Evidenced-Based Clinical Rounds in critical
DECREASING VAP
11
care units to include critical staff. In the event of publication, journal clubs may also review the
findings in healthcare facilities across the country and world (Melnyk & Fineout-Overholt,
2011).
DECREASING VAP
12
References
Grap, M., Munro, C. L., Hamilton, V., Elswick, R. K., Sessler, C. N., & Ward, K. R. (2011).
Early, single chlorhexidine application reduces ventilator-associated pneumonia in
trauma patients. Heart & lung, 40(5), e115-22. doi:10.1016/j.hrtlng.2011.01.006.
Institute for Clinical Systems Improvement (ICSI). (2011 Nov. 29). Prevention of ventilatorassociated pneumonia. Health care protocol. Bloomington (MN): Institute for Clinical
Systems Improvement (ICSI). Retrieved from
http://www.guideline.gov/content.aspx?id=36063&search=preventing+vap
Kimberly Clark. (2011). Ventilator associated pneumonia. Retrieved from
http://www.kchealthcare.com/hai-watch/hai-threats-solutions/ventilator-associatedpneumonia.aspx
Kusahara, D., Peterlini, M., & Pedreira, M. (2012). Oral care with 0.12% chlorhexidine for the
prevention of ventilator-associated pneumonia in critically ill children: Randomised,
controlled and double blind trial. International Journal of Nursing Studies, 49(11), 13541363. doi:10.1016/j.ijnurstu.2012.06.005.
Melnyk, B. M., Fineout-Overholt, E. (2011). Evidenced-based practice in nursing & healthcare.
Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins.
zaka, . ., Baolu, . K., Buduneli, N. N., Tabakan, M. S., Bacakolu, F. F., & Kinane,
D. F. (2012). Chlorhexidine decreases the risk of ventilator-associated pneumonia in
intensive care unit patients: a randomized clinical trial. Journal of Periodontal Research,
47(5), 584-592. doi:10.1111/j.1600-0765.2012.01470.x
DECREASING VAP
13
Table 1
Literature Review
Reference
Aims
Grap, M., Munro, C. L.,
Hamilton, V., Elswick,
R. K., Sessler, C. N., &
Ward, K. R. (2011).
Early, single
chlorhexidine
application reduces
ventilator-associated
pneumonia in trauma
patients. Heart & lung,
40(5), e115-22.
doi:10.1016/j.hrtlng.201
1.01.006.
Determine
whether a single
early
administration of
CHX would
reduce the
incidence of
VAP in critically
ill adults.
Kusahara, D., Peterlini,
M., & Pedreira, M.
(2012). Oral care with
0.12% chlorhexidine for
the prevention of
ventilator-associated
pneumonia in critically
ill children:
Randomised, controlled
and double blind trial.
International Journal of
Nursing Studies, 49(11),
1354-1363.
doi:10.1016/j.ijnurstu.20
12.06.005.
Test the
effectiveness of
oral care with a
0.12% CHX gel
in decreasing
VAP in critically
ill children.
Design and
Measures
RCT. VAP
evaluated on
admission, 48,
and 72 hours
after intubation
by using a
Clinical
Pulmonary
Infection Score
(CPIS).
RCT. The
primary
outcome
measure was
development
of VAP.
Secondary
measures
included:
length of
ventilation in
the PICU,
length of stay
in the PICU,
mortality, and
oral and
tracheal
colonization
with
microorganism
s.
Sample
145 trauma
patients
requiring
mechanical
ventilation.
Seventy-one
patients were
randomly
placed in the
intervention
(CHX) group
and 74 were
randomly
placed in the
control group.
Ninety-six
mechanically
ventilated
children, 50 of
which were
randomly
assigned to a
placebo
(control) group
and 46
randomly
assigned to a
CHX
(intervention)
group.
Outcomes /
statistics
A significant
treatment effect
from admission to
48 hours (p =
0.020) and to 72
hours (p = 0.027).
55.6% of the
patients in the
control group
developed VAP
compared to
33.3% of the
intervention
patients.
Study results
indicated a
diagnosis of VAP
in 32.6% of
patients in the
intervention group,
and 32.0% of
patients in the
control group (p =
0.949). While the
use of 0.12% CHX
was found to not
significantly
modify the VAP
incidence in a
sample of
mechanically
ventilated children,
CHX use was
found to be
protective against
VAP in children
without potentially
pathogenic micro
flora in their
DECREASING VAP
zaka, . ., Baolu,
. K., Buduneli, N. N.,
Tabakan, M. S.,
Bacakolu, F. F., &
Kinane, D. F. (2012).
Chlorhexidine decreases
the risk of ventilatorassociated pneumonia in
intensive care unit
patients: a randomized
clinical trial. Journal of
Periodontal Research,
47(5), 584-592.
doi:10.1111/j.16000765.2012.01470.x
14
Evaluate the
effectiveness of
oral swabbing
with a 0.2%
CHX gluconate
(CHX) solution
in decreasing the
risk of acquiring
VAP. VAP
development
time and
mortality rates
were also
recorded.
RCT. VAP
development,
periodontal
measurements,
lowerrespiratorytract specimens
sampling, and
mortality rates.
Sixty-one
dentate
patients
admitted to a
respiratory
ICU and
scheduled for
invasive
mechanical
ventilation for
at least 48
hours. Twentynine patients
were randomly
assigned to
intervention
(CHX) group,
and 32 patients
randomly were
assigned to the
control group.
oropharynx 24
hours after
mechanical
ventilation (p =
0.019). The
intervention did
not influence
pediatric intensive
care unit mortality
(p = 0.425),
hospital length of
stay (p = 0.143), or
pediatric intensive
care unit length of
stay (p = 0.177).
VAP rates were
significantly
higher in the
control group
when compared to
the CHX group
(68.8% vs. 41.4%,
p = 0.03). There
were no significant
differences in the
periodontal
measurements,
VAP development
time, or mortality
rate between
groups.
Anda mungkin juga menyukai
- Pat FinalDokumen24 halamanPat Finalapi-252804976Belum ada peringkat
- Pat I MsiDokumen28 halamanPat I Msiapi-252804976Belum ada peringkat
- Brian Poirier: His Certificate Is Awarded ToDokumen1 halamanBrian Poirier: His Certificate Is Awarded Toapi-252804976Belum ada peringkat
- Brian Poirier ResumeDokumen2 halamanBrian Poirier Resumeapi-252804976Belum ada peringkat
- TMH Cover LetterDokumen1 halamanTMH Cover Letterapi-252804976Belum ada peringkat
- Cert AspDokumen1 halamanCert Aspapi-252804976Belum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Josh Fose Standards Web PDFDokumen44 halamanJosh Fose Standards Web PDFYasir QureshiBelum ada peringkat
- A. Classification and Characteristics of Diabetes MellitusDokumen6 halamanA. Classification and Characteristics of Diabetes MellitusNicole Villanueva, BSN - Level 3ABelum ada peringkat
- CH 23 Infectious Diseases Skill WSDokumen2 halamanCH 23 Infectious Diseases Skill WSChing Man TamBelum ada peringkat
- Essential Care of Newborn at BirthDokumen32 halamanEssential Care of Newborn at Birthastha singh100% (1)
- What Is Subinvolution?Dokumen5 halamanWhat Is Subinvolution?Xierl BarreraBelum ada peringkat
- Pediatrics 2013 Kapadia E1488 96Dokumen11 halamanPediatrics 2013 Kapadia E1488 96M Aprial DarmawanBelum ada peringkat
- Fdar Samples PresentationDokumen29 halamanFdar Samples PresentationKewkew Azilear92% (37)
- Managerial Epidemiology Concepts and Case, 2d Ed.: Full TextDokumen2 halamanManagerial Epidemiology Concepts and Case, 2d Ed.: Full TextlovesunsetBelum ada peringkat
- Irene Gee Regidor BSED-English Conditions of Developmental Delay 1. Mental RetardationDokumen3 halamanIrene Gee Regidor BSED-English Conditions of Developmental Delay 1. Mental RetardationAliana CabalunaBelum ada peringkat
- Pengaruh Penambahan Kayu Manis TerhadapDokumen8 halamanPengaruh Penambahan Kayu Manis TerhadapIbnu SetyawanBelum ada peringkat
- DM Infectious DiseasesDokumen20 halamanDM Infectious DiseasesVasishta NadellaBelum ada peringkat
- Power of Plants 1Dokumen14 halamanPower of Plants 1api-399048965Belum ada peringkat
- Coronary Drug Eluting Stents Nonclinical and Clinical StudiesDokumen89 halamanCoronary Drug Eluting Stents Nonclinical and Clinical Studiesdudde niranjanBelum ada peringkat
- Summary - Hyaline Membrane DiseaseDokumen1 halamanSummary - Hyaline Membrane DiseaseJet BautistaBelum ada peringkat
- Luka Bakar: Nama: Melvin Andrean NIM: 112018161 Pembimbing: Kpt. Dr. Anwar Lewa, SP - BP-RE, M.BiomedDokumen47 halamanLuka Bakar: Nama: Melvin Andrean NIM: 112018161 Pembimbing: Kpt. Dr. Anwar Lewa, SP - BP-RE, M.BiomedIpd CengkarengBelum ada peringkat
- Jan 5, 2021 TDIR Worksheet (COG 2)Dokumen122 halamanJan 5, 2021 TDIR Worksheet (COG 2)Clarabelle Mae Dela RosaBelum ada peringkat
- Asuhan Keperawatan DiareDokumen32 halamanAsuhan Keperawatan Diareandreas winda adityaBelum ada peringkat
- Comprehensive Pharmacy Review 3rd EditionDokumen5 halamanComprehensive Pharmacy Review 3rd EditionAllidañac Luap0% (1)
- Introduction of Air Ambulance Services in IndiaDokumen5 halamanIntroduction of Air Ambulance Services in Indiaprithvinatarajan100% (1)
- Primitive ReflexesDokumen10 halamanPrimitive Reflexesbun_yulianaBelum ada peringkat
- HematuriaDokumen15 halamanHematurianisaw_2Belum ada peringkat
- 4th Year MBBS Batches & GroupsDokumen2 halaman4th Year MBBS Batches & GroupsSohail Abbas KhanBelum ada peringkat
- Letter of Support Template - 0 PDFDokumen2 halamanLetter of Support Template - 0 PDFselamitspBelum ada peringkat
- Intro To MED-SurgDokumen47 halamanIntro To MED-SurgMarites Santos AquinoBelum ada peringkat
- Understanding Osteoarthritis and Its ManagementDokumen160 halamanUnderstanding Osteoarthritis and Its ManagementPedro GouveiaBelum ada peringkat
- Effectiveness of Ergonomic Intervention inDokumen10 halamanEffectiveness of Ergonomic Intervention inTania SánchezBelum ada peringkat
- Literature Review On UTIDokumen31 halamanLiterature Review On UTINishchal Dhakal0% (1)
- A Time Motion Study To Measure and Analysis Clinical Nursing Workload in One of The Leading Hospitals in BangaloreDokumen4 halamanA Time Motion Study To Measure and Analysis Clinical Nursing Workload in One of The Leading Hospitals in BangaloreInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Sehatvan Fellowship ProgramDokumen8 halamanSehatvan Fellowship ProgramShivam KumarBelum ada peringkat
- Nepheline Syenite - Various Grades (A200-A270)Dokumen5 halamanNepheline Syenite - Various Grades (A200-A270)Lynne MarrBelum ada peringkat