Ndep-Line-Winter 2014
Diunggah oleh
api-235820714Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Ndep-Line-Winter 2014
Diunggah oleh
api-235820714Hak Cipta:
Format Tersedia
NDEP-Line
From the Chair...
Rayane AbuSabha
Professor and Graduate Program Director
The Sage Colleges Nutrition Science Department
Troy, New York
abusar@sage.edu
Winter 2014
In this issue:
From the Chair .................1
From the Editor..................3
2015 Area Meeting
Save the Date .....3
Guidelines for Authors...4
NDEP Officers....................4
While I sadly watch another short and cool summer slip by, as the
incoming chair of NDEP I cannot help but be thrilled about all the
exciting projects NDEP is working on this year. Before I discuss FNCE,
let me highlight a few things NDEP accomplished this past year.
Off with the NDA
This past year was quite a busy year for our membership. The
surprising announcement of the NDA (Nutrition and Dietetic Associate)
designation at FNCE in Houston was a topic of much debate for us
educators. Educators took a stand and spoke out against the premature
decision for this new designation/credential which led the Academys
Board of Directors to appoint a Task Force to look more closely at
moving to multi-levels of practice. The Task force recommended
dropping the NDA and building on the DTR Pathway III following many
of the educators suggestions. Needless to say, thanks to the hard work
of the Task Force members (including our own NDEP Past-Chair Julie
O-Sullivan Maillet) and the BODs latest vote, our faith in the process
followed by our Academy leaders has been restored. For sure we hit a
few bumps, but we are facing a crisis and these snags may have been
necessary to arrive to the best solution for our students and the future
of the profession.
Utilization of NutritionFocused Physical
Assessment in Dietetic
Curriculum.........................5
Organizing an
Interprofessional
Service Learning
Event................................9
Application and
Student Perceptions
of a Flipped Teaching
Model in a Life Cycle
Nutrition Course ............12
If Nutrition Is Your
Profession, Then
Public Policy Is
Your Future? ...................15
Best Practices in
Food Systems
Management and
Quantity Foods
Production..................... 18
2 | NDEP-Line | Winter 2014
A New, Stronger NDEP
We are slowly but surely moving to a stronger
presence of educators in the dietetics field and
within the Academy. Last year, we had several of
our newly formed NDEP task forces hard at work
on education issues: They attended the
International Interprofessional Education
conference in Vancouver, Canada to represent
dietetic education, they sent out surveys and
collected data from members to begin sharing
best practices on simulations and ideas to serve
you better, they recommended DICAS updates
based on member input and they developed new
recommendations for the second round dietetic
internship match: kudos to all our task force
members! At the Academy level, NDEP was
invited to appoint a representative to sit on the
Council on Future Practice. Patti Landers has
kindly agreed to be our representative for the
2014-2015 year. BOD and CDR liaisons were
also appointed to the NDEP Council to provide
us with updates on their activities and represent
educators to their boards.
Plans for the Coming Year
For this coming year, our plans are to build the
solid base for the future of this new and stronger
NDEP. Enticing practitioners to become
preceptors is one of our priorities. In addition to
the Preceptor Recruitment Fair held at FNCE,
NDEP plans to begin a series of nutrition
webinars presented by educators and made
available free of charge to NDEP members and
preceptors. Further, I have developed a
webpage off my departments website
(sage.edu/nutrition) that provides preceptors with
a hub for courses and modules that award free
continuing professional education. Feel free to
share this page with your preceptors as one of
the many perks of serving as a great mentor. The
page can be accessed at:
www.sage.edu/nutrition-ceus. If you know of
other free CPEU opportunities please share them
with me and help me keep this page up-to-date.
Finally, this year I will be researching the matter
of providing educators with CPEs just for acting
as preceptors, as is the case
with the Occupational Therapy field supervisors
who are rewarded for mentoring students with 18
units every three years by their credentialing body
NBCOT.
Helping faculty is another priority of the NDEP
Council. We are currently collaborating with the
Informatics DPG to develop a toolkit for educators to
introduce informatics throughout the dietetics
curriculum. Likewise, my hope is that we will work to
develop similar educational toolkits on the topics of
public policy and advocacy, two challenging subjects
for most programs. These are only but a few of the
many plans your NDEP leadership has at work.
On to FNCE 2014
Your NDEP Council was very busy at the Food and
Nutrition Conference and Exhibition this October
2014. It was wonderful seeing so many of you at our
NDEP Member Breakfast and Meeting on Sunday
when we heard updates from ACEND and CDR. The
NDEP education session submitted by our IPE Task
Force for FNCE Using Teamwork to Promote
Improved Patient Outcomes was extremely well
attended and received rave reviews. The NDEP
Student Internship fair on Sunday was packed with
over 700 students attending. The room was smaller
than originally requested which led to a crowded
space. We are making every effort to ensure a larger
space for next year. Finally, NDEP arranged the
meeting with the Association of Nutrition
Departments and Programs (ANDP, also known as
the nutrition department chairs of research
institutions) and ACEND, CDR and CFP to improve
communications between the Academy groups and
ANDP. The meeting was an overall success with the
plan for NDEP to arrange such a meeting every year
at FNCE. Thanks to all our wonderful task force
members and our NDEP Council members for
volunteering their time so generously and ensuring
the success of the NDEP activities at FNCE 2014.
Have a wonderful and productive year!
Rayane
3 | NDEP-Line | Winter 2014
From the Editor...
Robyn Osborn, PhD, RD
robyn.osborn@va.gov
Greetings! Effective with this issue, I am your new NDEP-Line Editor. If you wish to submit articles or
announcements relevant to dietetic education to NDEP-Line, please send them to me. We are always
looking for announcements or articles of interest to other educators and preceptors, including program
innovations and best practices.
The photos from 2014 NDEP Breakfast at FNCE in Atlanta are available in the NDEP Portal. The link to
the portal is http://ndep.webauthor.com.
2015 Area Meetings - -Save the Date
Area 1 Sunday, March 15th Tuesday, March 17th
Location: Asilomar Conference Grounds, Pacific Grove, CA
Rates: $241.57/night plus tax for a single room or $156.96/night plus tax for a double room. Room cost includes three meals per
day and tourism and facility fees. Please click on the following link to book a room at Asilomar:
https://resweb.passkey.com/Resweb.do?mode=welcome_ei_new&eventID=12522214.
Regional Directors Contact Information: Miriam Ballejos - medlefsen@comcast.net and Anne Shovic - shovic@hawaii.edu
Area 2/5 March 26-27, 2015 in Minneapolis/St. Paul, Minnesota
Hotel: Hilton Minneapolis/St. Paul Hotel, 3800 American Blvd, Bloomington, MN - $149/night plus tax (currently 14.28%). For
reservations, please call 952-854-2100 and state you are attending the Academy of Nutrition and Dietetics NDEP meeting. Hotel
parking and Wi-Fi access are complimentary. Registration information to follow.
Additional Information: The meeting will start around 8:30am on Thursday, March 26 and end by 1pm on Friday, March 27.
Regional Directors Contact Information: Julie Kennel kennel.3@osu.edu and Laurie Kruzich - lkruzich@iastate.edu
nd
Area 3/4 Friday, May 1st Saturday May 2 in Denver, Colorado
Hotel: Sheraton Denver Downtown Hotel 1550 Court Place, Denver, CO - $159/night plus tax (currently 14.85%). To make a
reservation, please call 303-893-3333 and state that you are attending the NDEP Area 3/4 Meeting. Registration information to
follow.
Regional Directors Contact Information: Susan Miller - miller1@uab.edu and Kristy Becker - kristy.becker2@va.gov
th
Area 6/7 Thursday, April 9th Friday April 10 in State College, Pennsylvania
Hotel: The Penn State Conference Center Hotel - $119/night plus tax (currently 8.5%). Hotel shuttle to and from the airport and
downtown State College, Wi-Fi access, and parking are complimentary.
Additional Information: It is highly recommend to make your travel plans early especially if you plan to fly to the meeting.
Meeting website link: http://sites.psu.edu/ndeparea6and7/
Please note that the webpage will be a work in progress. Information will be added as it becomes available.
Regional Directors Contact Information: Mary Dean Coleman - mdc15@psu.edu and Suzanne Neubauer
sneubauer@framingham.edu
Early bird meeting registration for all meetings will be $175 for NDEP members, $215 for Academy members, and $250 for nonAcademy members. Note: Fees increase by $30 to a standard rate. Fee schedules are determined by meeting and will be released
with registration information in January. Refer to the NDEP website at www.ndepnet.org for details, to be posted.
4 | NDEP-Line | Winter 2014
Guidelines for NDEP-Line
Authors
NDEP-Line features viewpoints,
statements, and information on
materials and products for the use of
Nutrition and Dietetic Educators and
Preceptors (NDEP) members. These
viewpoints, statements and information
do not imply endorsement by NDEP
and the Academy of Nutrition and
Dietetics. Articles may be reproduced
for educational purposes only. NDEPLine owns the copyright of all published
articles, unless prior agreement was
made.
NDEP Officers:
A submission may be returned to
the primary author for revision if it
does not conform to the style
requirements.
Copyright 2012 by Nutrition and
Dietetic Educators and Preceptors of
the Academy of Nutrition and Dietetics.
All rights reserved. No part of this
publication may be reproduced, stored
in a retrieval system or transmitted in
any form by any means without
permission of the publisher.
Article length
Article length is negotiated with the
editor for the issue in which it will
appear. Lead articles are usually
around 2,000 words. Other feature
articles are 1,000-1,500 words,
while book reviews and brief reports
are 500 words.
For authors in other
fields/disciplines:
Anthony T. Vicente, PhD, Director,
Nutrigenomics Laboratory,
American Human Nutrition
Research Center on Genetics at
American University
Text format
All articles, notices, and information
should be in Times New Roman
font, 12 point, single-spaced.
Tables and illustrations
Tables should be self-explanatory.
All diagrams, charts and figures
should be camera-ready. Each
illustration should be accompanied
by a brief caption that makes the
illustration intelligible by itself.
References
References should be cited in the
text in consecutive order
parenthetically. At the end of the
text, each reference should be
listed in order of citation. The format
should be the same as that of the
Journal of the Academy of Nutrition
and Dietetics.
Author(s)
List author with first name, initial (if
any) last name, professional suffix,
and affiliation (all in italics) below
the title of the article, i.e., For
NDEP members or other dietetic
educators:
Anne A. Anderson, PhD, RD, LD,
American University
Authors Contact Information
Before the article, give the primary
authors complete contact
information including program
affiliation, phone, fax and email
address.
Submission
All submissions for the publication
should be submitted to the editor as
an e-mail attachment as an MS
Word file. Indicate the number of
words after authors contact
information.
Rayane AbuSabha
Chair
abusar@sage.edu
Sylvia Escott-Stump
Chair-Elect
escottstumps@ecu.edu
Patti Landers
Past Chair
Patti-Landers@ouhsc.edu
Miriam Edlefsen Ballejos
Area 1 Regional Director
medlefsen@wsu.edu
Anne Shovic
Area 1 Regional Director
shovic@hawaii.edu
Laurie Kruzich
Area 2 Regional Director
lkruzich@iastate.edu
Susan Miller
Area 3 Regional Director Lead Director
Miller1@uab.edu
Kristy Becker
Area 4 Regional Director
Kristy.Becker2@va.gov
Julie A Kennel
Area 5 Regional Director
jkennel@ehe.osu.edu
Mary Dean Coleman
Area 6 Regional
Director
mdc15@psu.edu
Suzanne Neubauer
Area 7 Coordinator
sneubauer@framingham.edu
Renee Walker
Preceptor Director
Renee.walker2@va.gov
Submission Deadlines
Spring:
February 1
Summer:
May 1
Fall:
August 1
Winter:
November 1
Ruth Johnston
Portal Manager & HOD
Liaison
Ruth.Johnston@va.gov
Editor
Robyn Osborn, PhD, RD
VA San Diego Health care System
Phone: 858-552-8585 x 2407
Robyn.osborn@va.gov
Kathryn Hamilton
CDR Liaison
Reprint permissions request or
back issues:
Contact Robyn Osborn @
robyn.osborn@va.gov
Margaret Garner
BOD Liaison
mgarner@cchs.ua.edu
Julie Plasencia
Graduate Student Representative
Public Member
TBD
Dorothy Chen-Maynard
Journal Initiative Chair
dchen@csusb.edu
Robyn A Osborn
NDEP-Line Editor
Osborn_robyn@yahoo.com
Joan Frank
Applicant Guide Chair
jsfrank@ucdavis.edu
Lauren Florian
Academy Liaison
lflorian@eatright.org
5| NDEP-Line | Winter 2014
Utilization of Nutrition-Focused Physical
Assessment in Dietetic Curriculum
Dema Halasa-Esper MS, RDN, LD
Sue M. Leson, PhD, RDN, LD
Jeanine L. Mincher, PhD, RDN, LD
Rachael J. Pohle-Krauza, PhD, RDN
Zara C. Shah-Rowlands, PhD, RDN, LD
Youngstown State University, Department of Human Ecology, Food and Nutrition
dhesper@ysu.edu
330-941-3344
Background
New federal and state guidelines on the diagnosis
of malnutrition and reimbursement for related care,
requires that dietitians and other healthcare
providers become more vigilant and proactive in
providing successful interventions to prevent or
delay, reverse and limit malnutrition in care settings.
Physical assessment and examination skills are
needed to recognize the insidious effects of
malnutrition. Although physicians, nursing staff,
and other health professionals already perform
physical exams on patients, dietitians can utilize
Nutrition Focused Physical Assessment (NFPA) to
evaluate nutritional risk and determine more
effective nutrition interventions. NFPA techniques
assess for overt signs of nutritional deficiency, skin
integrity, organ function, and loss of muscle and
subcutaneous fat stores.
Healthcare reimbursement is scrutinized based on
clinical outcomes; therefore clinicians need to
exhibit care plans that show cost saving measures.
The Academy of Nutrition and Dietetics has
addressed this issue by asking the Council on
Future Practice (CFP) to project and plan for the
future needs of the dietetics profession by providing
guidance and recommendations on this topic in
their detailed report title Moving Forward A Vision
for the Continuum of Dietetic Education,
Credentialing and Practice. The impetus for our
Department to implement NFPA training through
the curriculum comes from parts of this report, as
well as preliminary data our colleagues have
collected over the past three years, which focus on
the incorporation of and training in NFPA in
undergraduate dietetic education.
Although the Accreditation Council for Education in
Nutrition and Dietetics (ACEND) has published
standards that allow currently accredited dietetics
programs to assimilate NFPA skill development into
coursework, Registered Dietitians Nutritionists
(RDNs) already in practice may have not yet been
trained in putting new assessment guidelines into
practice. In addition, all healthcare facilities have
not adopted new guidelines on malnutrition;
therefore, many have not made significant progress
toward training their dietetics staff on NFPA
techniques.1
Vision for Dietetics Education
Nutrition-related problems are best identified
through the Nutrition Care Process (NCP),
completed by RDs/RDNs. Here, objective and
subjective data are gathered in order to complete a
thorough nutrition assessment, which is the first
element of the NCP. Nutrition-focused physical
assessment is an important part of the fivecomponent approach to nutrition assessment, but
often not performed due to a lack of education and
training.2
Our ongoing goal is to incorporate more physical
assessment training into our CPD program at
Youngstown State University, along with
competency testing. It is our hope that such
training will reduce the reluctance of RDNs in
performing physical examinations. 3 Because of
this, a primary objective was to create and
6| NDEP-Line | Winter 2014
implement an educational program that would allow
preceptors, in addition to students, to be trained in
performing NFPA skills. This program will also
allow our department to further collaborate with
dietetic professionals who mentor our students
during their supervised practice experiences,
thereby, segueing classroom instruction into
supervised practices experiences. Currently, we
use case-based didactic approaches when applying
the NCP, but it is through hands-on training that
students will gain the self-assurance and skills set
necessary to perform NFPA as part of the NCP.
This will lead to confidence in using physical
assessment skills in their dietetic internship
experience and training, which will be translated
into future practice in nutrition and dietetics.
The interest in pursuing hands-on NFPA training in
dietetic education came from preliminary data
collected from a structured, internet-based survey
administered to RDs in the state of Ohio, who were
members of the American Dietetic Association. 4
The results of this survey revealed a significant
relationship between practitioner use of NFPA,
length of time in practice, and presence of
specialized certification. The RDs who used NFPA
received education and training mostly through a
conference/seminar and supervised practice. This
affirmed to our faculty that NFPA education should
be incorporated into the CPD curriculum. In
addition, we also gained insight into the necessity of
clinical preceptor involvement as part of the
ongoing effort to increase NFPAs emphasis in the
current curriculum.
Innovation in Dietetic Education with Expected
Outcomes
We have already seen the value of incorporating
NFPA training into the curriculum of supervised,
clinical practice for first year students in the CDP at
Youngstown State University. In 2011, we
conducted a pilot NPFA training in two four-hour
sessions as demonstration and simulation lectures
in each of the following subjects: body composition
(bioelectrical impedance and skinfold analysis,
muscle and subcutaneous fat assessment),
anthropometric indices (height, body weight, waist
circumference, arm span, and knee height), indirect
calorimetry (via Medgem), vital sign measurement
(temperature, pulse, respiration rate, blood
pressure, and blood glucose via finger stick), and
respiratory system assessment (review of thoracic
examination, breathing patterns and auscultation of
breath sounds). 4 All students ranked their interest
in NFPA as or greater based on a scale of 10, while
more than 90% of students ranked their likelihood
of using NFPA in future practice as a 7 or greater.
We concluded that the implementation of NFPA in
dietetic education might well have a prolonged and
favorable impact on students nutrition assessment
skills set and future dietetic practice. Our next step
is to incorporate these demonstration and
assimilation modules in NFPA into a course
curriculum for all dietetic students; however NFPA
skill assessment and competencies testing will be
completed with CPD students (junior and senior
years) and our preceptors in clinical, community,
maternal and child, and aging care practice settings
in order to ensure novice/beginner NFPA skills.
This will allow our dietetic program to further
expand our training to all students pursuing an
undergraduate degree in nutrition and dietetics at
Youngstown State University, both DPD and CPD
tracks.
Future Dietetics Education Plan with Expected
Outcomes
The diagnosis of malnutrition and reimbursement
for related care requires that dietitians become
more vigilant and proactive in identifying
malnutrition. The Academy of Nutrition and
Dietetics and the American Society for Parenteral
and Enteral Nutrition (ASPEN) have developed a
set of guidelines that, when used consistently and
accurately, can demonstrate the presence of
malnutrition, which can facilitate the physicians
ability to recognize and appropriately diagnose
malnourished patients.5 It is of note that four of six
criteria that should be used in order to generate this
diagnosis pertain to physical assessment of muscle
and fat mass, fluid accumulation, and grip strength.
And while malnutrition identifiers have always been
included to some degree in the nutrition
assessment process, linking them with current NCP
terminology (NCPT) may assist practitioners with
visualizing why and where NFPA fits into their
scope of practice and day-to-day provision of care
activities (Figure 1). Using NFPA will only enhance
7| NDEP-Line | Winter 2014
the dietitians ability to help to prevent, identify,
and/or delay the outcomes of malnutrition in
multiple care settings.
Dietetic educators can significantly contribute to the
building of didactic and skill development of
nutrition assessment; thus impacting RDNs role in
future practice. The benefit of and suggestions on
how to implement NFPA into dietetic curriculum are
detailed in Table 1. It is our recommendation to
program directors and educators to start small and
build gradually. The elements of NFPA skill
acquisition can be based on the novice and
beginner levels from the Career Development
Guide (CDG) as listed in the Academy Practice
Paper Critical Thinking Skills in Nutrition
Assessment and Diagnosis.7 Consider incorporating
elements of NFPA skills into several courses so
these concepts can be reinforced and addressed
through various dietetic settings (e.g. clinical,
community, maternal and child, and aging). This is
certainly an exciting time for our profession with
RDNs being recognized for professional skills,
knowledge, and the ability to impact healthcare
outcomes.
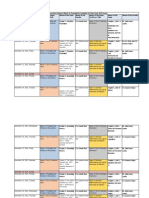
Figure 1: Nutrition Care Process Terminology and Malnutrition Characteristics. Adapted from (5) and (6).
Academy of Nutrition and Dietetics, Nutrition Care Process Terminology Reference Manual (eNCPT)
Copyright 2013. http://ncpt.webauthor.com
8| NDEP-Line | Winter 2014
Table 1: Benefits of and Suggestions for Implementation of NFPA into Dietetic Curriculum
Benefits
Provide cutting-edge educational
experiences can set your program apart.
Enable increased recognition of the
RDs/RDNs in the functioning of the health
care team.
Provide team experiences/collaboration for
students.
Increase the likelihood of future
reimbursement for nutrition services.
Students can develop novice level NFPA
skills prior to starting entry-level practice
Suggestions for Implementation
Faculty will need to engage in curriculum mapping to see
where and how NFPA can be incorporated into existing
courses.
Faculty will need to utilize resources already present:
- Colleagues on campus
- Already existing lab space and
equipment
- Shared simulation lab space
Faculty will need to obtain training and identify content experts
among the nutrition faculty.
Faculty will need to consider preceptors in the training as well
if supervised practice is part of the program.
Consider forming a joint Assessment Lab that is shared by
Allied Health Faculty and Students.
References:
1. Patel V, Romano M, Corkins MR, et al. Nutrition
screening and assessment in hospitalized
patients. A survey of current practice in United
States. Nut Clin Pract. 2014; 29:483- 490.
2. Cohen DA, Tougher-Decker R, Matheson P,
Byham-Gray J, OSullivan-Maillet. Physical
assessment knowledge and skills taught in dietetic
internships and coordinated programs. J Am Diet
Assoc. 2007; 107.
3. Halasa Esper D, Pohle-Krauza R. J., Leson S. M.
Nutrition Focused Physical Assessment:
Preceptors Education, Application and Perceived
Barriers. (Abstract). J AM Diet Assoc. 2010; 110
(9): A32.
4. Halasa-Esper D, Converse A, Yacovone ML,
Pohle-Krauza RJ. A Training Program in NutritionFocused Physical Assessment for Dietetics
Students. J Academy of Nutr Diet. 2012; 112 (9):
A27.
5. White J, Guenter P, Jenson G et al. Consensus
Statement of the Academy of Nutrition and
Dietetics/American Society for Parenteral and
Enteral Nutrition: Characteristics Recommended
for the Identifications and Document of Adult
Malnutrition (Undernutrition). J Acad Nutr Diet.
2012; 112:730-738.
6. Academy of Nutrition and Dietetics, Nutrition Care
Process Terminology Reference Manual (eNCPT).
Accessed December 1, 2014.
http://ncpt.webauthor.com
7. Practice Paper of Academy of Nutrition and
Dietetics: Critical Thinking of Nutrition Assessment
and Diagnosis. 2013.Accessed at
www.eatright.org/members/practicepapers
NDEP Website www.ndepnet.org
NDEP Portal http://ndep.webauthor.com
As an NDEP member, you are automatically entered into the portal and
have use of the EML system. Log in using your Academy log in and
password. To send a message to the NDEP EML, email
ndep@ndep.webauthor.com. To attach documents directly to your
message, you must send the message to this email address from your
email. Documents posted to messages submitted in the portal will not be
attached to the email message.
Questions email ndep@eatright.org
9| NDEP-Line | Winter 2014
Organizing an Interprofessional Service
Learning Event
Nina Roofe, PhD, RDN, LD, FAND
Assistant Professor & Dietetic Internship Director
Department of Family & Consumer Sciences
University of Central Arkansas
nroofe@uca.edu
501-450-5950
Purpose and Rationale
Development of interprofessional skills is a
critical component in didactic and supervised
practice educational programs. The World
Health Organization defines Interprofessional
Education (IPE) as when students from two or
more professions learn about, from and with each
other to enable effective collaboration and
improve health outcomes. The expectation of a
patient-centered health care team starts at the
undergraduate level.1 Didactic programs in
dietetics promote IPE and teamwork while
addressing barriers and challenges.2
Competencies for IPE programs encompass four
domains including values and ethics; roles and
responsibilities; interprofessional communication;
and teams and teamwork.3-5 All team members
should be trained with a community-oriented,
patient centered mindset (see Figure 1).
Figure 1: Interprofessional Collaborative Practice Domains
Interprofessional Communication Practices
Roles and Responsibilities for Collaborative
Practice
Community Oriented
Patient Centered
Interprofessional Teamwork and Team-Based
Practice
Values / Ethics for Interprofessional Practice
10| NDEP-Line | Winter 2014
Faculty Involvement
Developing a culture for IPE requires faculty from
multiple disciplines who are trained in and value
IPE and are willing to work together to co-create
a shared vision, common goals, and
experiences.6-8 The event described here is a
campus-wide health fair for faculty, staff, and
students. This IPE event is one section of the
health fair. Two faculty members were assigned
to each of the four areas of health information
regarding obesity (definition, screening,
prevention, or treatment) to oversee and assist
student efforts. Prior to the health fair, faculty
from multiple disciplines provided education and
instruction to their respective students. This
education and training focused on
interprofessional health care collaboration, scope
of practice of various health care providers, and
applicable licensure laws.
Student Involvement
The students were challenged with the task of
creating education and screening materials
focused on obesity prevention and treatment.
Four sections were identified for organizational
purposes including (1) Definitions/Risk Factors,
(2) Screening, (3) Prevention, and (4) Treatment.
Students from eight departments collaborated on
each content area section of the health fair. The
eight departments were Health Sciences,
Kinesiology, Nursing, Nutrition, Occupational
Therapy, Physical Therapy, Psychology, and
Speech Language Pathology. A true
interdisciplinary model was used with all
departments represented in each content area as
opposed to a multidisciplinary model. The goal
was not to have a nutrition section, nursing
section, physical therapy section, etc., but rather
to provide a venue for students from each
department to collaborate on a given content
area.
Students created informational displays using
criteria from the CDC, USDA, and the Academy
regarding body mass index categories as well as
obesity risk factors and comorbidities. These
displays provided specific information regarding
definitions and screening criteria for obesity.
Screenings were conducted at the next section
including measurements of body mass index,
waist to hip ratio, body composition, and a family
health history. The third section was focused on
prevention and provided information on lifestyle
assessment, strategy development, goal setting
and local resources to support nutrition, exercise,
and stress management. The final section
showcased evidence-based treatment options for
obesity including prescription medications,
bariatric surgery, and weight management
programs.
Steps in event planning are outlined below to
serve as a guide for implementation and can be
adapted to fit specific department or college
parameters.
1. Secure administrative and faculty support.
a. College Dean established one day during
the term as IPE Day for students to
participate in the event. This was
communicated to all faculty in the college
to allow students involved to be excused
from class for the purpose of the event. If
students were enrolled in courses outside
the college, a letter from an IPE faculty
member was written to request the
student be excused for this event.
b. Department Chairs encouraged faculty to
support the event and to tie participation
to course objectives in appropriate
classes. In this case, the event is part of
the capstone Nutrition Senior Seminar
course.
c. Faculty planned ahead for this event
when writing their course syllabi and
course schedule. Additionally the course
content included education and training
on IPE as well as a reflection assignment
for points in the course.
2. Identify assessment/record-keeping
needs.
a. Attendance records to report level of
participation for university, college, and
departmental outcome measures
b. Follow-up surveys or focus groups to
identify what worked well and areas for
improvement for future events.
3. Identify the number of students in each
department who would participate in the
event.
a. Each department compiled a list of
students and their preferred email
addresses
b. The number of students in each
department was equally (as much as
possiblesome departments did not have
an even number of students) divided
among the areas of the health fair.
4. Determine topics for each section and
divide students evenly in each section.
a. Each group looked at the scope of each
discipline involved in relation to their
assigned section of the health fair.
11| NDEP-Line | Winter 2014
b. Areas of overlap were identified as well as
areas of delineation, e.g. nursing staff
administer medications while nursing,
nutrition, and health science staff address
food drug interaction education.
c. The students met several times before the
event to plan, review scope of practice
and licensure laws, delineate roles, and
collaborate on how to address their
assigned areas.
d. Once assigned areas were identified,
each group created the content for their
displays and interactive booths:
i.
Definition/Screening Criteria:
informational displays using criteria
from the CDC, USDA, etc. regarding
BMI definitions, risk factors, and comorbidities.
ii.
Screening: performed BMI
calculations, waist to hip ratio, body
composition analysis, and a family
health history.
iii.
Prevention: conducted a lifestyle
assessment and provided information
on goal-setting, local resources and
strategy development, e.g. nutrition,
exercise, stress management,
awareness of risk factors, and
genetics.
iv.
Treatment: showcase of current
treatments with scientific evidence
base and local resources, e.g. Rx
meds, bariatric surgery, weight
management programs.
5. Assess and Debrief
a. Administered surveys and conducted
focus groups as planned.
b. Determined impact on students in terms
of teamwork, communication, and comfort
with health care collaborations through
student reflection.
c. Shared information on attendance and
impact with interested stakeholders:
students, faculty, and staff.
Discussion
The ability of healthcare providers to work as a
team is crucial for optimal patient care. In fact,
the Interprofessional Education Collaborative
(IPEC) has established interprofessional
teamwork and team based practice as one of the
four interprofessional collaborative practice
domains. 3 Creating experiences that allow for
interaction with multiple disciplines in the health
sciences provides a context for practicing
communication and teamwork skills.9
Participation gives students an opportunity to
begin to understand the necessity of
communication and how to function as a team in
order to provide optimal patient care. These
events can be documented on a students
resume which may be of interest to prospective
employers and graduate education programs.
Faculty involvement is critically important for
student training and modeling of collaboration
with faculty from other departments.10 Looking
ahead to actual practice settings, we can
anticipate that teamwork and collaboration can
decrease error and enhance quality of care. It
stands to reason that learning these skills during
academic and clinical training will increase the
possibility that graduates will be skilled at
collaboration and teamwork, leading to improved
patient outcomes.
References
1. World Health Organization. Framework for action
on interprofessional education & collaborative
practice [internet]. Geneva (Switzerland): World
Health Organization; 2010.
Available from:
http://www.who.int/hrh/resources/framework_actio
n/en/
2. Heiss CJ, Goldberg LR, Brady H. Service-learning
in dietetics courses: A benefit to the community
and an opportunity for students to gain dieteticsrelated experience. J Acad Nutr Diet. 2012;
112(10): 1524-7.
3. Bainbridge L, Nasmith L, Orchard C, Wood V.
Competencies for interprofessional collaboration.
JOPTE. 2010; 24(1): 6-11.
4. Bridges DR, Abel MS, Carlson J, Tomkowiak J.
Service learning in interprofessional education: A
case study. JOPTE. 2010; 24(1): 44-50.
5. Interprofessional Education Collaborative. Core
competencies for interprofessional collaborative
practice: Report of an expert panel [Internet].
Washington DC: Interprofessional Collaborative;
2011 May. 56 p. Available from:
http://www.aacn.nche.edu/educationresources/ipecreport.pdf
6. Bringle RG, Hatcher JA. Innovative practices in
service-learning and curricular engagement. New
Directions for Higher Education. 2009 Fall; 147:
37-46.
7. DEon M. A blueprint for interprofessional learning.
Medical Teacher [Internet]. 2004. 26(7): 604-9.
Available from:
http://informahealthcare.com/doi/abs/10.1080/014
21590400004924.
8. Institute of Medicine. Health professions
education: A bridge to quality. Washington DC:
The National Academies Press; 2003 Apr 18,
p.176.
12| NDEP-Line | Winter 2014
9. Institute of Medicine. Educating for the health
team: Report of the conference on the
interrelationships of educational programs for
health professionals. Washington DC: The
National Academies Press; 1972 Oct., p39.
10. Solomon P, King S. Online interprofessional
education: Perceptions of faculty facilitators.
JOPTE. 2010; 24(1): 3.
Application and Student Perceptions of a
Flipped Teaching Model in a Life Cycle
Nutrition Course
Renee D. Barrile, PhD, RD, LDN
Lecturer, Clinical Laboratory and Nutritional Science
University of Massachusetts Lowell
Renee_Barrile@uml.edu
978-934-4457
Flipping a class refers to a model of teaching that
reverses the traditional classroom lecture to
something that students do at home before coming
to class. In other words, students learn the material
on their own time by watching pre-taped lectures
and/or assigned readings and during class time
they participate in activities to enhance learning.
There are many potential benefits to this model.
One is that students come to class prepared with
the basic information, allowing class time to be
dedicated to hands-on learning activities. Students
can then apply knowledge under the guidance of
their instructor while working collaboratively with
their peers.1
The idea of a flipped classroom has been gaining in
popularity since articles about the model have
appeared in a range of publications from the NY
Times2 to the scholarly journal Science.3 While
limited, there is some quantitative data to suggest
students do learn material to a greater extent when
being taught in this manner. In one example, a
physics class was taught in a traditional manner at
the start of the semester. Later, one section used
reading assignments and quizzes to introduce
material, and class time was used for small group
discussion and questions delivered through clickers
and written responses. At the end of the course,
grades on a multiple choice test were significantly
higher from the section taught with the flipped
model compared to the control section. The flipped
class also scored higher on student engagement as
assessed by trained observers.4 Another University
used a flipped model in a challenging engineering
course. This flipped model required students to
watch lecture videos from the Massachusetts
Institute of Technology and used class time for
discussion. Initial data show the method is leading
to higher test scores compared to sections taught in
a traditional lecture only format.5
There are several ideas and suggestions to ensure
students are learning the material in a flipped class.
This is important because the material is being
introduced outside normal class time so that the
time used for in class activities is productive.
Initially, instructional materials like pre-taped
lectures or targeted readings with some type of
incentive to use these materials before coming to
class is critical to introduce material that is to be
learned. Secondly, students must be evaluated to
ensure learning is taking place. Lastly, the activities
that take place during the class time should allow
students to apply what they have learned in the
taped lectures or readings and enhance critical
thinking and problem solving skills.6
In the Spring of 2014, I used a flipped teaching
model in a Life Cycle nutrition course. To do this,
assigned readings, quizzes, and in class group
activities were utilized for selected topics
throughout the semester. The objective of making
some classes flipped was to better engage
students, foster more critical thinking and problem
13| NDEP-Line | Winter 2014
solving skills and encourage collaborative learning.
For the flipped topics, the start of class included an
open note quiz to ensure students had completed
the reading assignment and came to class
prepared. The rest of class was dedicated to small
group activities that allowed students to apply what
they had learned in the readings. Short quizzes
provided incentive for preparing for class, and
points were awarded for turning in a finished
product from the small group activities. The material
the students were quizzed on was the more basic
material and was taken directly from the assigned
reading. All of the in-class activities were completed
in small groups and required some type of
documentation that was submitted at the end of the
class. The activities did require some background
information, which was covered in the reading, and
were planned to help achieve overall course
objectives. The effectiveness of the flipped model
was assessed with a brief, voluntary, and
anonymous survey given on the last day of class.
Of the 41 students enrolled in the course, 35
provided informed consent and completed the
survey on the last day of class. The survey
included 5 questions pertaining to student learning,
student engagement, critical thinking and problem
solving skills, and class preparedness. These
questions were asked using a Likert scale from 1-5
with 1 indicating the student liked the flipped model
much better than the traditional model, 2 indicating
the student liked it better than the traditional model,
3 indicating they thought flipped vs. traditional were
the same, 4 indicated the flipped model was worse
than traditional, and 5 indicating the flipped model
was much worse. The average score for all 5
questions using the Likert scale was around 2,
indicating most students preferred the flipped model
over the traditional model. The highest average
score was for student engagement where 91% of
students felt the flipped model was much better or
better than the traditional model. The majority of
students (83%) also felt the flipped model was
much better or better at fostering critical thinking
skills, 77% felt it was much better or better at
helping them come prepared for class, and 74% felt
it was much better or better at fostering problem
solving skills.
The survey also included open ended questions
that were intended to elicit feedback that could be
used for future planning purposes. The responses
echoed the responses to the Likert scale questions
in that comments were generally positive about the
flipped model, and many students reported that
they found the flipped classes more interesting and
engaging than a normal lecture. A few also noted
that they enjoyed being able to apply knowledge,
get up and move during class, and interact with
their classmates. Some also cited benefits in their
critical thinking and communication skills. A few
students also found the assigned reading and
quizzes made studying for regular exams easier.
When asked what they did NOT like about the
flipped classes, the majority of those that
responded made reference to the quizzes on the
assigned reading given at the start of the flipped
classes. There were many reasons for not liking
the quizzes including the general stress and extra
work of having to read and take a quiz and more
specific critiques about the quizzes themselves.
For example, one student felt that the quizzes were
inconsistent and another noted they didnt know
how to prepare for them. Others do not like
learning by reading and would prefer taped lectures
and a few did not feel like the reading prepared
them for the in-class activities enough. There were
also some comments about the activities
themselves. One student commented that they did
not like working in groups and two students noted
they liked certain activities better than others.
The last open ended question asked what could be
done to make the flipped classes better. While
many chose to leave this question blank, the most
common written response was wanting more time
to complete the in-class activities. A few students
also suggested that more of the classes be flipped.
Others made suggestions to improve the seemingly
least favorite aspect of the flipped class, the
quizzes. Ideas included not having them, not
grading them, giving more guidance on what would
be on them, and making them worth extra credit. A
few students commented on the activities. One
student requested more interesting activities and
three others wanted more information on what the
activity would be before coming to class.
Analysis of the survey results was valuable in
planning for future sections of this course. First
and foremost, I will continue to utilize the flipped
model in place of some of the traditional lectures. I
will also make specific changes based on the
feedback. For example, I will include a brief
description of the in-class activity in the syllabus so
14| NDEP-Line | Winter 2014
students will feel more prepared for class. I will
change the requirements of some of the activities
so students will have enough time to fully complete
the in-class assignments. Although the open note
quizzes were clearly the least desirable aspect of
the flipped class, I will continue to include them and
grade them because it was an efficient and effective
way to ensure students prepared for class.
However, I will add specific learning objectives for
each class in the syllabus, which can help guide
students to important concepts to prepare for
quizzes and the in class activities.
The initial workload to plan and prepare flipped
classes is certainly greater for both student and
instructor. However, some students noted
preparing for the flipped classes made studying for
regular exams easier. I expect my workload to
decrease moving forward since the in-class
activities and quizzes are established and only
need moderate refining. Another important
consideration is class size. One of the great
benefits of the flipped model is being able to
interact with the students, but the number of
instructors/teaching assistants that are available to
assist the students during the learning activities
limits this. A major weakness of this project was
the absence of data to evaluate if the flipped model
improved student performance. While I do have
information about grades on exams and case
studies from previous semesters when the course
was not flipped, informed consent was not given for
past sections so data cannot be reported.
Additionally, the composition of the students from
semester to semester has great variability, which
greatly limits comparability.
References
1. EDUCAUSE Learning Initiative. Things you should
know about Flipped Classrooms. Educause
Learning Initiative website. Available at:
www.educause.edu. Published February 2013.
Accessed April 11, 2014.
2. Fitzpatrick M. Classroom lectures go digital. The
New York Times; June 24, 2012.
3. DesLauriers L, Schelew E, and Wieman C. Improved
learning in a large-enrollment physics class. Science
2011; 332: 862-864.
4. Walvoord BE, and Anderson VJ. Effective grading: A
tool for learning and assessment. San Francisco,
CA: Jossey-Bass; 1998.
5. Mazur E. Farewell, Lecture? Science 2009; 23: 5051.
6. Berrett D. How flipping the classroom can improve
the traditional lecture. Chronicle of Higher Education
website. Available at:
http://chronicle.com/article/How-Flipping-theClassroom/130857/. Published 2012. Accessed
April 12, 2014.
15 | NDEP-Line | Winter 2014
If Nutrition Is Your profession, Then Public
Policy Is Your Future?
Wendy Phillips, MS, RDN, CNSC, CLE, FAND
President, Virginia Academy of Nutrition and Dietetics
Angie Hasemann, MS, RDN, CSP
Dietetic Internship Director, University of Virginia Health System
wp4b@virginia.edu
434-982-2522
Public policy training for nutrition students
and interns
If nutrition is your profession then public policy is
your business. As dietetic students, interns, and
registered dietitian nutritionists (RDNs), we hear
this slogan frequently, yet so few actually
become involved in public policy at the
grassroots level. Only about 7% of members of
the Academy of Nutrition and Dietetics
(abbreviated as the Academy) responded to the
Call to Action for the Treat and Reduce Obesity
Act, and less than 10% of state affiliate members
vote in state or national elections for board
positions of these organizations. Most state
affiliates of the Academy report that only three to
four percent of their members participate in the
annual Legislative Day held in the capitol of each
state. If we say public policy is our business, we
do a poor job of showing our business skills.
Barriers to involvement
Many describe hesitancy to become involved in
new activities as fear of the unknown, including
public policy. Students receiving primary
education in the United States are often required
to take a Civics class in eighth grade and
sometimes have refresher classes in high school
and possibly college. However, the information
may seem insignificant to them and their future
careers, and many students do not remember
specifics by the time they enter the workforce. In
addition, students may not complete their
internships or accept employment in the same
state (or even the same country!) as their primary
education, and, therefore, need to learn public
policy specific to the state in which they are now
living and working. Walking in to a legislators
office can be an intimidating task, especially if the
person does not comfortably understand the
structure of government or policies related to
nutrition and healthcare in their area.
Another reason dietitians report not becoming
involved in public policy is being unconvinced
that the rewards would be worth the time
invested. Due to the realities of healthcare
budgets, most dietitians do not have time built
into their daily activities at work to participate in
public policy, and even taking one day off to
attend state affiliate Legislative Days may prove
challenging, especially if the state capitol is a
long distance to travel. Low numbers of dietitians
responding to calls to action and organized
legislative activity may indicate that supervisors
arent fully supporting legislative activity by their
RDN staff and, furthermore, may not be setting
an example of being active in public policy.
Therefore, it is important to help dietitians
understand how public policy impacts their day to
day work, their patients, and their profession. In
addition, reducing the fear of the unknown
through mentoring is an effective way to increase
participation in public policy activities. Preparing
dietitians to enjoy and succeed in public policy
matters begins long before they make their way
into a legislators office and, preferably, long
before becoming a RDN.
Starting early
Just as dietetic students and interns are learning
medical nutrition therapy and foodservice
management, it is beneficial to learn the basics of
public policy during their education. A best
practice from the University of Virginia Health
System Dietetic Internship features a seasoned
RDN public policy leader hosting a Mock
General Assembly. In this creative activity,
interns learn about the legislative priorities
established by the Academy, and then draft mock
nutrition bills to be introduced in the mock
General Assembly (GA). They introduce the bills
16 | NDEP-Line | Winter 2014
into the mock Virginia House of Delegates, and
advocate for these bills, which they then debate.
As members of the mock subcommittees in the
House of Delegates or Senate, they ultimately
vote on the proposed bills, and present 2 final
choices to the mock Governor. The Governor
(usually impersonated by the Internship Director)
then approves one bill and the team of interns
who drafted that bill wins a prize. This lesson not
only shows how public policy can be fun and
relevant, it introduces the structure of the GA and
legislative process in a relaxed setting. This
makes the perfect practice session just before
the state affiliates Legislative Day at the state
capitol.
Making it easier/taking away the barriers
Mentoring
An informal poll of current and past board
members for the Virginia Academy of Nutrition
and Dietetics (VAND) stated the most important
factor for getting them involved in leadership
positions for the state affiliate or in public policy
activities was mentoring. Dietitians, nutrition
students, and interns were more likely to make
the first visit with an elected representative to
discuss nutrition-related public policy if they were
accompanied by a dietitian who was familiar with
the process. Anecdotal evidence supports that
witnessing an RDN skilled in public policy
casually converse with a legislator whom they
knew well helps to not only educate but, also,
inspire others. State capitols may be distant from
the dietitians hometown, and legislators are often
very busy when the GA is actually in session.
Therefore, it is helpful for the first visit to be
conducted in the legislators home district office
when the GA is not in session. This may also be
a less intimidating environment for someone new
to the experience.
These visits do not need to be heavily scripted or
focused on specific legislation. In fact, the first
meeting with a legislator should take place when
there is no nutrition-related legislation being
considered because this helps to establish a
relationship outside of the specific request to vote
for the legislation. This serves as a great
opportunity to introduce the dietetics field, the
path to becoming an RDN, and the patients or
clients helped by RDNs on a daily basis.
Providing a base understanding of the field and
the many roles an RDN can play will help
reinforce the importance of the profession and
how RDNs serve the constituents in the
legislators area. For someone new to public
policy, it may be helpful to provide a simple
notecard with talking points to cover, including
the number of dietitians in the state and
legislative district, the wide variety of fields in
which RDNs work, and a reminder to offer to be
expert reviewers for nutrition-related bills. The
message is simple, but helping to coach and
mentor others until they are comfortable is
essential to training future public policy leaders.
Making it personal
Above all, it is important to remember that politics
is still personal. While statistics about the impact
of obesity on chronic health diseases like
diabetes and cardiovascular disease are
important to have available, a story about a
patient who suffered from obesity and its
resultant diseases and was subsequently helped
by an RDN to improve their quality of life and
medical conditions will be more powerful. While
people may struggle to recall the statistics you
shared, they will remember the stories you tell.
Use these stories to paint a picture for the
legislator, just as you would for a friend or
colleague. People, including legislators, make
decisions with their emotional brain, not their
rational brain.1 It is important to help legislators
see the human connection in the nutrition-related
policy efforts for which we are advocating.
In addition to personal stories, a picture is worth
a thousand words. Bringing pictures of RDNs,
dietetic interns, and nutrition students working in
a variety of settings and with a variety of people,
such as pregnant women, children, elderly,
hospitalized, athletes, and other healthy people
can help legislators understand the magnitude of
impact that RDNs can have in the lives of their
constituents. These pictures can speak louder
than words when used on posters, websites, and
social media sites as well.2 Encouraging RDs,
students, and interns to begin capturing the work
they do in the community in photos early on in
the career will lend itself to more engaging career
portfolios, as well as more intriguing evidence
when advocating for the profession in the public
policy arena.
17 | NDEP-Line | Winter 2014
Practical (and easy!) steps to become
involved
Tell your story
Our legislators are elected by us, to represent us.
They care about their constituents as much as
we care about our patients and for the same
reason! Most RDNs become dietitians to make a
difference in the lives of patients. Most
legislators entered the profession because they
want to make a difference in their county, state,
and/or country. In the same way that dietitians
need to hear a patients story in order to help
him/her, the legislators need to hear how they
can help us. During the 2014 Lobby Day for the
Virginia Academy of Nutrition and Dietetics, two
state legislators spoke to the dietitians and
interns in attendance. Both of these Delegates
stressed the importance of telling success stories
of dietitians working with patients.
Knowing what stories to tell and how to introduce
them can be challenging for someone who is new
to public policy. This is worth practicing on the
car ride to the legislators office or even at district
or state dietetic meetings. Asking fellow RDs
some pointed questions can help to guide this.
What do you love most about your job? Can you
tell me about a patient whose progress you were
most proud to be a part of? Have you had a
patient or client express appreciation to you
recently? What did he/she say?
Often, the story will come out without rehearsal.
Simply in talking to a person and mentioning
nutrition, they likely have a comment, question, or
story themselves. Whether it is that their neighbor
is an RDN, they want to know more about sports
nutrition, or theyve had their own weight loss
journey, listen. Use nutrition counseling skills to
engage and ask open-ended questions. Learn
more about the background of the story. This
may seem challenging, but training in
motivational interviewing often takes over, and it
becomes a conversation. Find ways in this
conversation to get to know the legislator better
and to emphasize the vital role RDNs play in
healthcare. Often, conversations with a legislator
have quite a few similarities to conversations with
clients or patients, just with a different but equally
important purpose.
By finding ways to tell stories and make public
policy personal, this intimidating topic can not
only be easier, but also more fun. Engage a few
colleagues to help mentor, and you are
guaranteed to have a great time at your
representatives home office, state Legislative
Day, or even on Capitol Hill. Do you have
creative ideas on how you make public policy
your business? Please share them with us at
vand.president@gmail.com.
References:
1. Damsio A. Descartes' Error: Emotion,
Reason, and the Human Brain. Putnam
Publishing; 1994.
2. Just a Handful of Social Media Comments
Can Grab the Attention of Congress, Study
Shows. CQ Roll Calls Website.
http://connectivity.cqrollcall.com/just-ahandful-of-social-media-comments-can-grabattention-of-congress-study-shows/. Updated
October 27, 2014. Accessed November 25,
2014.
Mark Your Calendars
Certificate of Training in Adult Weight
Management:
March 20-22, 2015, New Brunswick, NJ
June 4-6, 2015, New Orleans, LA
Certificate of Training in Childhood and
Adolescent Weight Management:
March 12-14, 2015, Charlotte, NC
Coding and Billing Webinar
Spring 2015: Upcoming NDEP Webinar on
Coding and Billing presented by Jessie Pavlinac
to provide directions on using the new
Academy Coding and Billing Handbook: A Guide
for Program Directors and Preceptors. More
information will be sent through the NDEP EML.
18 | NDEP-Line | Winter 2014
Best Practices in Food Systems
Management and Quantity Foods
Production
Jeanie Subach, EdD, RD, CSSD, LDN
Assistant Professor, Department of Nutrition
West Chester University of Pennsylvania
rsubach@wcupa.edu
610 436-2762
The May 2012 supplement of the Journal of the
Academy of Nutrition and Dietetics titled
Management Is a Multifaceted Component
Essential to the Skill Set of Successful Dietetics
Practitioners1 stresses the need for inclusion of the
development of managerial skills in didactic and
supervised practice curriculum for future
practitioners. The supplement explains the
inclusion should not be limited to foodservice
management courses and experience, rather
woven throughout all parts of curricula and
practices. It further discusses the need to remove
the question of Are you management or clinical
from the conversations of the dietetic profession,
stating Management should be inculcated in the
members of our profession in a variety of
contexts.1
Most dietetic educators would agree that food
systems management and quantity food production
are not the most popular courses in the didactic
curriculum. As faculty in a DPG program, teaching
both Quantity Foods Production and Food Systems
and Nutrition Management, I am faced with the task
of engaging students in the concepts of both
courses. The challenge lays in increasing the
understanding of the importance of the role of the
registered dietitian in food systems management
and quantity foods production.
The initial assignment given to students in the
Quantity Food Production class at West Chester
University of Pennsylvania is the completion of a
self-assessment used to survey their experience
and interest of the food service industry. The final
question of the assessment asks the likelihood that
they will pursue a career in food service post
baccalaureate. The majority of the responses from
the 130+ students indicated a preference to pursue
a career that is more clinical or communityoriented. I respond each year by sharing the
journal supplement, reinforcing that the success in
clinical and community nutrition cannot be achieved
without quality quantity food production, which
cannot be achieved without strong managerial
skills. A goal of the course is to dispel the
perception of mean foodservice directors and lunch
ladies in hair nets, educating on the value, scope,
and depth of the area of management and food
service as a support system to clinical and
community endeavors/operations.
As a compliment to course content, students plan
and execute a quantity foods production project.
Using the concepts of the systems theory model,
students plan the menu and are assigned different
task as part of management and production teams.
The audiences of the productions are organizations
within and outside the University, which adds a
service learning component to the course. At the
completion of the events, students write a reflection
paper and conduct a production analysis in class.
One function was the production of a dinner meal
for 165 persons. Meal recipients were students and
families of the Universitys Adapted Physical
Education program (APE). The program provides
physical education to children ages 6-18 with
intellectual and developmental disabilities. The gym
of the College of Health Sciences served as the
dining room, and the foods lab was the quantity
foods kitchen. The less than ideal setting posed
many obstacles requiring the students to work as a
team and use their problem solving abilities.
The menu was designed, distributed, and returned
prior to the event. Students executed all aspects of
procurement, production, and service, upholding
their obligations as ServSafe Managers.
Purchasing and production modifications were
made to accommodate allergens and special
feeding needs. At the completion of the event,
customer and employee satisfaction and financial
accountably, all desired outputs of the Food
Systems Model, were all successfully obtained.
19 | NDEP-Line | Winter 2014
While this may seem like a typical quantity food
class production, the event was actually a tipping
point, allowing students to view foodservice through
a different lens. At the end of the event, the
director of the APE program called the nutrition
students together informing them of a
breakthrough that occurred during service. An 11year-old boy with autism took a bite of an apple for
the first time in his life. His mother, coach, and
program director cried at the sight. The APE
director told them that through the design of the
menu, service, and positive interaction between the
nutrition majors, students, and families, that healthy
food was served and accepted in a safe, friendly
environment. The director explained that this
enabled the child to feel safe and comfortable
enough to do something he had never done before.
She told them they did more than just serve food,
that they made a difference in the life of a young
boy with autism. The next day in class discussion,
although pleased with the successful execution of
the event, the students were more excited with
making a difference in the life of a child with autism.
The statement made at the start of the semester
that success in clinical and community nutrition
cannot be achieved without quality quantity food
production was repeated, and this time the students
understood.
Exposing students to various populations and food
services experiences allows them to see first-hand
the importance of food systems management and
foodservice as a vehicle to provide healthy food to
the public in the quest of decreasing incidences of
obesity and other diet-related chronic diseases.
References
1. Canter, DD, Sauer, KL, Shanklin, CW.
Management Is a Multifaceted Component
Essential to the Skill Set of Successful
Dietetics Practitioners. J Acad Nutr Diet,
2012, 112(5), S5.
Happy Holidays
From Your
NDEP Council
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- A Strategic Management PaperDokumen7 halamanA Strategic Management PaperKarll Brendon SalubreBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- American Literature TimelineDokumen2 halamanAmerican Literature TimelineJoanna Dandasan100% (1)
- 05 Askeland ChapDokumen10 halaman05 Askeland ChapWeihanZhang100% (1)
- VV016042 Service Manual OS4 PDFDokumen141 halamanVV016042 Service Manual OS4 PDFCamilo Andres Uribe Lopez100% (1)
- Adhd Nutrition Considerations ChecklistDokumen1 halamanAdhd Nutrition Considerations Checklistapi-235820714Belum ada peringkat
- Adhdreferences 2016Dokumen4 halamanAdhdreferences 2016api-235820714Belum ada peringkat
- Nutrition Screening Acute Care Setting Newsletter Winter 2017 Phillips DoleyDokumen8 halamanNutrition Screening Acute Care Setting Newsletter Winter 2017 Phillips Doleyapi-235820714Belum ada peringkat
- Fnce 2017 LTC Productivity Benchmarks AbstractDokumen1 halamanFnce 2017 LTC Productivity Benchmarks Abstractapi-235820714Belum ada peringkat
- Granting Owps To Rdns Can Decrease Costs Andj Phillips DoleyDokumen8 halamanGranting Owps To Rdns Can Decrease Costs Andj Phillips Doleyapi-235820714Belum ada peringkat
- Western Hemisphere ProfileDokumen1 halamanWestern Hemisphere Profileapi-235820714Belum ada peringkat
- Beastarsept 2016Dokumen1 halamanBeastarsept 2016api-235820714Belum ada peringkat
- 2201 October p1 DK 13 17Dokumen5 halaman2201 October p1 DK 13 17api-235820714Belum ada peringkat
- Pine View Invitational Deca 2nd Place Jan 2016Dokumen1 halamanPine View Invitational Deca 2nd Place Jan 2016api-235820714Belum ada peringkat
- Braden Scale Jan 2017 JandDokumen6 halamanBraden Scale Jan 2017 Jandapi-235820714Belum ada peringkat
- Tyler Phillips CVDokumen1 halamanTyler Phillips CVapi-235820714Belum ada peringkat
- Minimizing False-Positive Nutrition Referrals From The MSTDokumen5 halamanMinimizing False-Positive Nutrition Referrals From The MSTapi-235820714Belum ada peringkat
- Parrish Dec 15 UpdatedDokumen8 halamanParrish Dec 15 UpdatedRhod Bernaldez EstaBelum ada peringkat
- td10 2015Dokumen6 halamantd10 2015api-235820714Belum ada peringkat
- PhillipsproductivityarticleDokumen3 halamanPhillipsproductivityarticleapi-235820714Belum ada peringkat
- Benchmarkingfeb 2015Dokumen7 halamanBenchmarkingfeb 2015api-235820714Belum ada peringkat
- Brandjuly 2014Dokumen6 halamanBrandjuly 2014api-235820714Belum ada peringkat
- Phillips NCP June 2015 Malnutrition Coding For NSTDokumen5 halamanPhillips NCP June 2015 Malnutrition Coding For NSTapi-235820714Belum ada peringkat
- Fnce 2014 AbstractmstzechariahphillipsDokumen1 halamanFnce 2014 Abstractmstzechariahphillipsapi-235820714Belum ada peringkat
- Newsletter Fall 2014costbasedaccountingarticleDokumen18 halamanNewsletter Fall 2014costbasedaccountingarticleapi-235820714Belum ada peringkat
- Matters Nov14 PhillipsDokumen1 halamanMatters Nov14 Phillipsapi-235820714Belum ada peringkat
- Lobbydaynewsletter 2014Dokumen7 halamanLobbydaynewsletter 2014api-235820714Belum ada peringkat
- Katch-Up Mhfs November 12 2012rcnmawardDokumen2 halamanKatch-Up Mhfs November 12 2012rcnmawardapi-235820714Belum ada peringkat
- PG Malnutritioncoding Sept 14Dokumen7 halamanPG Malnutritioncoding Sept 14api-235820714Belum ada peringkat
- Brandnewsletterapril 2014Dokumen9 halamanBrandnewsletterapril 2014api-235820714Belum ada peringkat
- Esphlsummaryaug 2014Dokumen1 halamanEsphlsummaryaug 2014api-235820714Belum ada peringkat
- 1pageprofile PhillipsDokumen1 halaman1pageprofile Phillipsapi-235820714Belum ada peringkat
- Dyk October 2012Dokumen2 halamanDyk October 2012api-235820714Belum ada peringkat
- Newsletter Spring 2014 - Icd10Dokumen20 halamanNewsletter Spring 2014 - Icd10api-235820714Belum ada peringkat
- Rostam's Seven LaboursDokumen3 halamanRostam's Seven LaboursArifin SohagBelum ada peringkat
- CANAVAN' and VESCOVI - 2004 - CMJ X SJ Evaluation of Power Prediction Equations Peak Vertical Jumping Power in WomenDokumen6 halamanCANAVAN' and VESCOVI - 2004 - CMJ X SJ Evaluation of Power Prediction Equations Peak Vertical Jumping Power in WomenIsmenia HelenaBelum ada peringkat
- ALT Company Introduction 20170524.1Dokumen51 halamanALT Company Introduction 20170524.1Terence WoonBelum ada peringkat
- RRLDokumen4 halamanRRLTiltshifter ViBelum ada peringkat
- PremiumpaymentReceipt 10663358Dokumen1 halamanPremiumpaymentReceipt 10663358Kartheek ChandraBelum ada peringkat
- GDcorrespondencecourselessons 165Dokumen8 halamanGDcorrespondencecourselessons 165olly rathboneBelum ada peringkat
- Volume 4-6Dokumen757 halamanVolume 4-6AKBelum ada peringkat
- Hope 03 21 22Dokumen3 halamanHope 03 21 22Shaina AgravanteBelum ada peringkat
- Good Evil EssayDokumen2 halamanGood Evil EssayuniquebythemillionsBelum ada peringkat
- Split Plot Design GuideDokumen25 halamanSplit Plot Design GuidefrawatBelum ada peringkat
- Adjustment and Impulse Control DisordersDokumen19 halamanAdjustment and Impulse Control DisordersArchana50% (4)
- Booklet English 2016Dokumen17 halamanBooklet English 2016Noranita ZakariaBelum ada peringkat
- Food 8 - Part 2Dokumen7 halamanFood 8 - Part 2Mónica MaiaBelum ada peringkat
- Datasheet AD549Dokumen14 halamanDatasheet AD549Trần Hồng VănBelum ada peringkat
- 2000 T.R. Higgins Award Paper - A Practical Look at Frame Analysis, Stability and Leaning ColumnsDokumen15 halaman2000 T.R. Higgins Award Paper - A Practical Look at Frame Analysis, Stability and Leaning ColumnsSamuel PintoBelum ada peringkat
- Beuys Begleitheft en ScreenDokumen18 halamanBeuys Begleitheft en Screensofijawt0% (1)
- IT Technician CVDokumen3 halamanIT Technician CVRavi KumarBelum ada peringkat
- APA - 7thed - UCW Student Paper TemplateDokumen4 halamanAPA - 7thed - UCW Student Paper Templatesimerpreet3Belum ada peringkat
- Understanding Urbanization & Urban Community DevelopmentDokumen44 halamanUnderstanding Urbanization & Urban Community DevelopmentS.Rengasamy89% (28)
- Lesson Plan Garbage Gym GameDokumen3 halamanLesson Plan Garbage Gym Gameapi-272479731Belum ada peringkat
- Yayasan Pendidikan Ramadanthy Milad Anniversary SpeechDokumen6 halamanYayasan Pendidikan Ramadanthy Milad Anniversary SpeechDina Meyraniza SariBelum ada peringkat
- Vee 2003Dokumen14 halamanVee 2003Syed faizan Ali zaidiBelum ada peringkat
- Armitage Tutorial for Cyber Attack ManagementDokumen54 halamanArmitage Tutorial for Cyber Attack Managementworkmumbai3870Belum ada peringkat
- Material Safety Data Sheet: Development Associates, IncDokumen3 halamanMaterial Safety Data Sheet: Development Associates, IncDedi MulyadiBelum ada peringkat
- Chapter 1-The Indian Contract Act, 1872, Unit 1-Nature of ContractsDokumen10 halamanChapter 1-The Indian Contract Act, 1872, Unit 1-Nature of ContractsALANKRIT TRIPATHIBelum ada peringkat
- SPH3U Formula SheetDokumen2 halamanSPH3U Formula SheetJSBelum ada peringkat