April Case Study Final
Diunggah oleh
api-265264098Deskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
April Case Study Final
Diunggah oleh
api-265264098Hak Cipta:
Format Tersedia
1
Michelle Rocque
Clinical Practicum I
April 2015
Invasive Ductal Carcinoma of the Right Breast Case Study
History of Present Illness: Patient MS is a 78 year-old Caucasian female who experienced an
abnormal mammogram of the right upper outer breast in early December 2014. A biopsy
completed two weeks later was confirmed positive. In January 2015, the patient was taken to
surgery after electing to have a mastectomy. The resulting pathology revealed a 1.5 cm grade 2
invasive ductal carcinoma without DCIS. Estrogen and progesterone receptors were both
positive. 16 axillary lymph nodes were taken and revealed 2 positive sentinel nodes and 14
negative axillary nodes. An Oncotype DX score was obtained and was 6 which is considered
low. This score, if available, makes a prediction for distal recurrence. It impacts the decision to
include adjuvant chemotherapy into the treatment regimen.1 MS was referred to radiation
oncology to consider post-mastectomy radiation therapy due to the confirmed nodal disease.
In late March 2015, the patient presented to the radiation oncology department for consultation
of radiation therapy to the right chest wall. Her diagnosis was malignant neoplasm of upperouter quadrant of female breast with an (Active) stage IIA, T1c, pN1a, M0. A detailed
description of the treatment plan was discussed with the patient. The risks, benefits, and side
effects of radiation therapy were discussed and she agreed to proceed with radiation therapy
treatments. An informed consent was signed by the patient and placed in the electronic medical
record.
Past Medical History: MS has a past medical history which consists of breast cancer, diabetes,
hypertension, lung problems, sinus cough, thyroid disease, urinary infections and she wears
glasses. Her past surgical history included an appendectomy, cholecystectomy, hysterectomy, a
right modified mastectomy and thyroidectomy. Also noted in her medical history was that the
patient has a pacemaker and has received no previous radiation therapy. MS also reported
known allergies as Penicillin, Codeine, Lisinopril, and Tramadol.
Social History: MS indicated that there was no family history of cancer. She stated that she
was married and not employed. She has one son, aged 61. She has no history of smoking and
has never drank alcohol.
Medications: MS indicated using the following medications: Neurontin, Claritin, Singulair,
Advair Diskus, Synthroid, Nexium, Micardis, Atorvastatin, Timolol, Astelin, and vitamin B12.
Diagnostic Imaging: In late November 2014, MS underwent a routine mammogram that
revealed a spiculated mass which measured 1.2 x 1.3 x 1.4 cm. Two weeks later, a right breast
ultrasound was completed. The findings from this exam were stated to be a right breast
spiculated mass highly suggestive of malignancy. Six days later, a right breast tissue biopsy was
performed. The pathology from this biopsy revealed ER/PR positive HER2 negative right
invasive ductal carcinoma.
Radiation Oncologist Recommendations: After review of MSs surgical history and pathology
report, the radiation oncologist recommended a 3-field technique to the right chest wall and right
supraclavicular fossa. Right chest wall tangents with the addition of bolus every other day would
be planned. Because of her 2 positive axillary lymph nodes, a supraclavicular treatment portal
would be needed.
The Plan (Precription): The radiation oncologists treatment prescription consisted of right
chest wall irradiation with conventional medial and lateral tangential beams. Bolus, .5 cm, every
other day would be added to the chest wall in order to pull the dose closer to the skin surface. A
right supraclavicular field would be used to treat the supraclavicular nodes. The prescription
dose was 50.4 Gray (Gy) to the chest wall and 50.4Gy to the right supraclavicular fossa.
Patient Setup/Immobilization: In late March 2015, MS underwent a computed tomography
(CT) simulation scan. The patient was placed in the supine position on the CT simulation couch
on a breast board with an immobilization device. Her right arm was positioned above her head
and left arm was left at her side (Figure 1). A cushion was placed under her knees for support.
The radiation oncologist marked with wire and BBs the superior, inferior, medial and lateral
borders for field delineation. The opposite breast was outlined with wire. In addition, BBs were
placed on the chest to indicate the CT origin: long, lateral, vertical.
Anatomic Contouring: After completion of the CT simulation scan, the CT data set was
transferred in the Varian Eclipse 11.0 treatment planning system (TPS). The medical dosimetrist
contoured the field borders identified by the wires placed at the time of CT. Organs at risk were
also contoured by the medical dosimetrist. These included the right and left lungs, heart, spinal
canal and humeral head. An additional contour of the pacemaker was included in order for the
dose to be carried and shown on the dose-volume histogram.
Beam Isocenter/Arrangement: A Varian 6EX linear accelerator was used for treating this
patient. The medical dosimetrist chose a mono-isocentric technique for this treatment plan. The
isocenter was placed approximately 2.5cm inside the right chest wall along the superior border
marked by the radiation oncologist, which corresponded to the bottom of the clavicle (Figure 2).
The isocenter corresponded to the mid-plane depth of the medial and lateral tangential beams.
The field size chosen was half beamed on the superior Y axis and the X axis was half beamed at
the deep margin of the tangent. This created a quarter beam technique (Figure 2,3). The length
of the field encompassed the inferior border chosen by the oncologist. The width included
approximately 2cm of flash outside of the chest wall. The gantry was virtually rotated until the
appropriate amount of lung was included, as well as, visually avoiding the opposite breast
contour. A multi-leaf collimator (MLC) blocking pattern was created to block the lung that was
over 2cm. This also matched the medial field border that was contoured. This became the medial
tangent. This field was opposed for the lateral tangent. The medial and lateral photon beams
utilized gantry angles of 130 and 310 respectively. There were no collimator or table angles used
for these treatment fields. The dosimetrist returned to the isocenter to create a supraclavicular
field. The field was half beamed from the lower Y jaw. The gantry was rotated 10 degrees
toward the ipsilateral breast to angle off of the spinal cord. A custom MLC block was drawn to
cover the humeral head (Figure 3). The medical dosimetrist then entered the prescription
information into the TPS. A 6MV energy was used due to the location of the pacemaker in order
to keep the dose as low as possible.
Treatment Planning: The treatment planning system Eclipse version 11 was used. The
objective was to distribute a homogeneous dose throughout the treatment volume while keeping
the lung dose and pacemaker dose as low as possible. A calculation point was chosen and
adjusted in order to provide the dosimetrist with options to create a field in field technique for
lowering the hot spot in the tangential fields (Figure 2). The field weighting was also adjusted to
more effectively distribute the dose throughout the chest wall. A 15 degree wedge was inserted
into the lateral field to attenuate the dose and lower the hot spot of the plan. The patient received
a total of 180cGy per day to the tangential fields. The final field weighting was 35% to the
medial, 30% to the lateral, and 35% to the lateral field in field. The overall hotspot for the chest
wall was 108.4%. The treatment plan was then copied and .5cm bolus was added to cover the
chest wall. After the plan was recalculated for the addition of bolus, the monitor units indicated
a slight increase. Because bolus was used every other day, the prescribed dose to the non-bolus
tangents was 2520cGy and the bolus tangents received 2520cGy. The supraclavicular fossa was
planned after a calculation point was chosen. The calculation point was 3cm superior to the
isocenter and 2.5cm posterior to the patients skin surface (Figure 3). After initial calculation of
the field, it was determined that a wedge was needed to attenuate the dose from medial to lateral.
A 10 degree wedge was inserted and field weighting was adjusted to create a more homogeneous
dose distribution throughout the field. The overall hotspot for the supraclavicular portal was
108.2%. Once an acceptable treatment plan was achieved (Figures 4, 5), the dose volume
histogram (DVH) was reviewed for verification of treatment doses to organs at risk and the
pacemaker (Figure 6). The total lung volume at 20Gy (V20) was to be less than 30%. The V20
of this plan was 15%.
Quality Assurance/Physics Check: A monitor unit (MU) check was independently performed
using the RadCalc program. The expected tolerance between the TPS and RadCalc is 5% for
each treatment field. All fields fell within the acceptable range. In addition, the physics
department performed a diode reading on the patient to check the pacemaker dose. This was
completed once the patient began treatment. Three readings were taken with the diode placed
superior, over, and inferior to the pacemaker (Figure 7). These readings all fell within acceptable
limits and was calculated to be approximately 18.6cGy (Figure 8). According to the AAPM TG
34, contemporary cardiac pacemakers can fail from radiation damage at doses as low as 10Gy
and can exhibit functional changes at doses as low as 2Gy.2
Conclusion: The mono- isocentric technique is becoming more frequently used in our
department. The advantage is that there is a shorter treatment time because there is no movement
of the patient once the isocenter is established. Ive learned that this technique cannot be used in
every situation because you have field length and overall anatomic limitations. When a half
beam is used for the tangential fields there is no need to over rotate the gantry in order to
eliminate beam divergence. I also learned that by using a half beam on the tangential fields there
was less dose to the patients pacemaker. I saw through the planning of this case how changing
the calculation point brings a real change to the isodose lines and can change the hot spot of the
plan. I initially struggled with finding a calculation point which gave me desired coverage
inferiorly and superiorly. The concepts I learned from this case study will help me to plan chest
wall treatments more effectively and efficiently in the future.
References
1. Nguyen MT, Stessin A, Nagar H, et al. Impact of oncotype DX recurrence score in the
management of breast cancer cases. Clinical Breast Cancer. 2014; 14(3): 182-190.
http://dx.doi.org/10.1016/j.clbc.2013.12.002.
2. Marbach JR, Sontag MR, Van Dyk J, Wolbarst AB. Management of radiation oncology
patients with implanted cardiac pacemakers: report of AAPM task group no. 34. Med Phys.
1994; 21(1): 85. http://dx.doi.org/10.1118/1.597259.
Figure 1: Patient position from with borders shown from CT simulation.
Figure 2: Medial digitally reconstructed radiograph (DRR) with calculation point defined.
Figure 3: AP DRR with calculation point defined.
Figure 4: Axial (upper view) and sagittal slices of RT chest wall.
10
Figure 5: Axial (upper view) and sagittal slices of RT supraclavicular fossa.
11
Figure 6: Plan Summary of RT Chest Wall and Supraclavicular fossa DVH
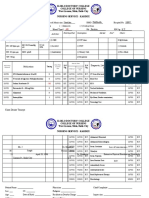
Figure 7: Diode placement and measured dose
12
Figure 8: Special physics consult showing estimated dose from Eclipse
Anda mungkin juga menyukai
- Resume 1 2016Dokumen4 halamanResume 1 2016api-265264098Belum ada peringkat
- Fall Case Log TotalsDokumen2 halamanFall Case Log TotalsBen LemieuxBelum ada peringkat
- Typhon Group Easi - Evaluation Survey InstrumentDokumen3 halamanTyphon Group Easi - Evaluation Survey Instrumentapi-265264098Belum ada peringkat
- Oct 15Dokumen3 halamanOct 15api-265264098Belum ada peringkat
- Final PaperDokumen12 halamanFinal Paperapi-282901112Belum ada peringkat
- Oct 15Dokumen3 halamanOct 15api-265264098Belum ada peringkat
- Final Project SubmissionDokumen10 halamanFinal Project Submissionapi-265264098Belum ada peringkat
- ImrtDokumen3 halamanImrtapi-265264098Belum ada peringkat
- BrachycompDokumen2 halamanBrachycompapi-265264098Belum ada peringkat
- Oct 15Dokumen3 halamanOct 15api-265264098Belum ada peringkat
- Case Study Operational IssuesDokumen2 halamanCase Study Operational Issuesapi-265264098Belum ada peringkat
- Final PaperDokumen12 halamanFinal Paperapi-282901112Belum ada peringkat
- Oct 15Dokumen3 halamanOct 15api-265264098Belum ada peringkat
- Budget ActivityDokumen2 halamanBudget Activityapi-247490129Belum ada peringkat
- Flow 20chart 2012 2010 2015Dokumen2 halamanFlow 20chart 2012 2010 2015api-265264098Belum ada peringkat
- Qa Tolerance Tables FinalDokumen12 halamanQa Tolerance Tables Finalapi-265264098Belum ada peringkat
- CitationsDokumen1 halamanCitationsapi-265264098Belum ada peringkat
- Qa Checklist 2015Dokumen1 halamanQa Checklist 2015api-269666683Belum ada peringkat
- Research Draft 2Dokumen22 halamanResearch Draft 2api-269666683Belum ada peringkat
- Photon PDFDokumen3 halamanPhoton PDFapi-265264098Belum ada peringkat
- Imrt PDFDokumen3 halamanImrt PDFapi-265264098Belum ada peringkat
- Effective Mentoring in Medical DosimetryDokumen6 halamanEffective Mentoring in Medical Dosimetryapi-265264098Belum ada peringkat
- ElectronpdfDokumen2 halamanElectronpdfapi-265264098Belum ada peringkat
- Procedures SummerDokumen2 halamanProcedures Summerapi-265264098Belum ada peringkat
- Clinical Practicum II Clinical Lab AssignmentDokumen3 halamanClinical Practicum II Clinical Lab Assignmentapi-264047496Belum ada peringkat
- JuneDokumen3 halamanJuneapi-265264098Belum ada peringkat
- JulypdfDokumen3 halamanJulypdfapi-265264098Belum ada peringkat
- JulypdfDokumen3 halamanJulypdfapi-265264098Belum ada peringkat
- CaselogsDokumen2 halamanCaselogsapi-265264098Belum ada peringkat
- Cns AssignmentDokumen1 halamanCns Assignmentapi-286145993Belum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5782)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Family Nursing Problem Lack of Inability of Immunization The ParentsDokumen2 halamanFamily Nursing Problem Lack of Inability of Immunization The Parentsscarletblue100% (1)
- RespimirrorDokumen10 halamanRespimirrorsukantaenvBelum ada peringkat
- Spleen - Function, Location & Problems - Live SciencebjkDokumen13 halamanSpleen - Function, Location & Problems - Live SciencebjkImtiax LaghariBelum ada peringkat
- Safety and Effectiveness of Lurasidone in Adolescents With Schizophrenia: Results of A 2-Year, Open-Label Extension StudyDokumen11 halamanSafety and Effectiveness of Lurasidone in Adolescents With Schizophrenia: Results of A 2-Year, Open-Label Extension StudyNaiana PaulaBelum ada peringkat
- Esbl Producing eDokumen45 halamanEsbl Producing eapi-205355237Belum ada peringkat
- Multiple Mini Interview (MMI) For The Mind BookDokumen13 halamanMultiple Mini Interview (MMI) For The Mind Bookbravek20161% (18)
- Hubungan Kadar Leukosit, Monosit, Dan Prokalsitonin Dengan Kejadian Infeksi Dan Luaran Fungsional Pada Stroke AkutDokumen7 halamanHubungan Kadar Leukosit, Monosit, Dan Prokalsitonin Dengan Kejadian Infeksi Dan Luaran Fungsional Pada Stroke AkutDiayanti TentiBelum ada peringkat
- Self-Monitoring of Blood Glucose Among Patients With Type I Diabetes Mellitus in Buraidah CityDokumen7 halamanSelf-Monitoring of Blood Glucose Among Patients With Type I Diabetes Mellitus in Buraidah CityInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Psychological Profiles Among Women With Vulvar Vestibulitis Syndrome: A Chart ReviewDokumen9 halamanPsychological Profiles Among Women With Vulvar Vestibulitis Syndrome: A Chart ReviewHeriberto Escobar SamaniegoBelum ada peringkat
- Pharmacology For Nursing Care 6th Edition Lehne Test BankDokumen2 halamanPharmacology For Nursing Care 6th Edition Lehne Test BankStuartCarrsBelum ada peringkat
- Cholelithiasis N C P BY BHERU LALDokumen1 halamanCholelithiasis N C P BY BHERU LALBheru LalBelum ada peringkat
- LiposuctionDokumen35 halamanLiposuctionprkscribdBelum ada peringkat
- Diabetes Mellitus Type 2Dokumen19 halamanDiabetes Mellitus Type 2anandbro093100% (1)
- Living Will TemplateDokumen2 halamanLiving Will Templatesaucolcous50% (4)
- 5 Different Ways To Consume Cannabis For Better HealthDokumen3 halaman5 Different Ways To Consume Cannabis For Better HealthPrakhar Singh PundhirBelum ada peringkat
- Inglês Médico - Aula 01Dokumen26 halamanInglês Médico - Aula 01Leandro Teixeira dos SantosBelum ada peringkat
- 10.1038@s41569 020 00451 XDokumen16 halaman10.1038@s41569 020 00451 XAldo González SalinasBelum ada peringkat
- Iloilo Doctors' College Nursing Service KardexDokumen4 halamanIloilo Doctors' College Nursing Service KardexKiara Denise TamayoBelum ada peringkat
- Care of Clients With Gastrointestinal Disorders Copy 1Dokumen7 halamanCare of Clients With Gastrointestinal Disorders Copy 1Mr. whiteBelum ada peringkat
- West Visayas State University Medical Center E. Lopez St. Jaro Iloilo CityDokumen7 halamanWest Visayas State University Medical Center E. Lopez St. Jaro Iloilo CityRegine Marie EspañaBelum ada peringkat
- The 29 Pulses in Chinese Medicine (TCM) Pulse DiagnosisDokumen7 halamanThe 29 Pulses in Chinese Medicine (TCM) Pulse Diagnosispromo21Belum ada peringkat
- Instructions For Use Epogen (Ee-Po-Jen) (Epoetin Alfa)Dokumen10 halamanInstructions For Use Epogen (Ee-Po-Jen) (Epoetin Alfa)Francis LucenarioBelum ada peringkat
- Physician Statement Form ETPDokumen2 halamanPhysician Statement Form ETPKpi BrazilTwoBelum ada peringkat
- Approach To Loss of AppetiteDokumen6 halamanApproach To Loss of AppetitePrithvi RameshBelum ada peringkat
- ممارسه صيدلانيه رقم ١ PDFDokumen31 halamanممارسه صيدلانيه رقم ١ PDFMustafa PhBelum ada peringkat
- Mental Health Nursing Techniques and DisordersDokumen3 halamanMental Health Nursing Techniques and DisordersRuchika Kaushal100% (1)
- CPR by Using SimulationDokumen5 halamanCPR by Using SimulationAnusha VergheseBelum ada peringkat
- 2020 Using Sildenafilto Treata Dogwithidiopathic MegaesophagusDokumen7 halaman2020 Using Sildenafilto Treata Dogwithidiopathic MegaesophagusEduardo SantamaríaBelum ada peringkat
- Sales Rep. / Sales ManagerDokumen3 halamanSales Rep. / Sales Managerapi-121455688Belum ada peringkat
- Crash Course Psychiatry Xiu 5 Ed 2019Dokumen355 halamanCrash Course Psychiatry Xiu 5 Ed 2019Shang100% (5)