Incidence of New Tumor Formation...
Diunggah oleh
romeoenny4154Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Incidence of New Tumor Formation...
Diunggah oleh
romeoenny4154Hak Cipta:
Format Tersedia
Incidence of New Tumor Formation in
Patients with Hereditary Retinoblastoma
Treated with Primary Systemic Chemotherapy:
Is There a Preventive Effect?
Matthew W. Wilson, MD, FACS,1,2,3 Barrett G. Haik, MD, FACS,1,2 Catherine A. Billups, MS,4
Carlos Rodriguez-Galindo, MD5,6
Purpose: To report the incidence of new tumor formation in hereditary retinoblastoma patients treated with
primary systemic chemotherapy.
Design: Noncomparative retrospective case series.
Participants: Fifty-eight consecutive patients with hereditary retinoblastoma treated with primary systemic
chemotherapy.
Methods: The charts of 58 consecutive patients with hereditary retinoblastoma treated between January 1996
and August 2005 were reviewed. Data extracted included gender, age at diagnosis, family history of retinoblastoma,
laterality of disease, tumors per eye, ReeseEllsworth grouping of affected eyes, starting and ending dates for
chemotherapy, number of cycles of chemotherapy, chemotherapy regimen, need for external beam radiotherapy
and/or enucleation, and development and location (macula, midzone, and periphery) of new tumors after the start of
systemic chemotherapy.
Main Outcome Measure: New tumor formation after treatment with primary systemic chemotherapy.
Results: Of the 58 patients, 48 had bilateral involvement at diagnosis. Median age at diagnosis was 6.6 months.
Thirteen patients had a positive family history. Of the eyes with tumor (n 106) at diagnosis, 52 (49%) were in
ReeseEllsworth groups I to III, whereas 54 (51%) were in group IV or V. Seven patients (12%) with a median age of
1.6 months at diagnosis formed 36 new tumors in 11 eyes after the start of chemotherapy. Median time from initiation
of chemotherapy to detection of the first new tumor was 3 months (range, 115). Cumulative incidence of new tumor
formation at 2 years was 103%. An age of 6 months at diagnosis, family history of retinoblastoma, and
ReeseEllsworth grouping of I to III were found to correlate significantly with an increased incidence of new tumor
formation (P0.001, P0.001, and P 0.021, respectively). Median follow-up for all patients was 5 years (range, 110.1).
Conclusion: New tumors continue to form in patients with hereditary retinoblastoma despite treatment with
primary systemic chemotherapy. Younger patients and those with a positive family history are more likely to have new
tumors formed. However, chemotherapy may impact small previously undetected lesions by slowing their growth and
facilitating later focal consolidation. Ophthalmology 2007;114:20772082 2007 by the American Academy of
Ophthalmology.
Retinoblastoma is the most common intraocular malignancy
of childhood.1 Approximately 1 in 20 000 live births is
affected annually, with 300 new cases being diagnosed in
the United States each year.1 One third of these children will
have bilateral/multifocal intraocular retinoblastoma. Such
patients are referred to as having hereditary retinoblastoma,
as they possess a germline mutation in one allele of the RB1
5
Originally received: November 8, 2006.
Final revision: February 13, 2007.
Accepted: March 7, 2007.
Available online: July 12, 2007.
Manuscript no. 2006-1295.
1
Department of Ophthalmology/Hamilton Eye Institute, University of
Tennessee Health Science Center, Memphis, Tennessee.
2
Division of Ophthalmology, Department of Surgery, St. Jude Childrens
Research Hospital, Memphis, Tennessee.
3
Department of Pathology, St. Jude Childrens Research Hospital, Memphis, Tennessee.
4
Department of Biostatistics, St. Jude Childrens Research Hospital, Memphis, Tennessee.
2007 by the American Academy of Ophthalmology
Published by Elsevier Inc.
Department of Pediatrics, University of Tennessee Health Science Center, Memphis, Tennessee.
6
Department of Oncology, St. Jude Childrens Research Hospital, Memphis, Tennessee.
Presented at: American Academy of Ophthalmology Annual Meeting,
November 13, 2006, Las Vegas, Nevada.
Supported by the National Cancer Institute, Bethesda, Maryland (grant nos.
CA 23099, 21765 [Cancer Center Support Grant]); American Lebanese Syrian
Associated Charities, Memphis, Tennessee; Research to Prevent Blindness,
New York, New York; and St. Giles Foundation, New York, New York.
Correspondence to Matthew W. Wilson, Hamilton Eye Institute, 930
Madison Avenue, Room 476, Memphis, TN 38163. E-mail:
mwilson5@utmem.edu.
ISSN 0161-6420/07/$see front matter
doi:10.1016/j.ophtha.2007.03.015
2077
Ophthalmology Volume 114, Number 11, November 2007
gene. The median age at diagnosis for these patients is 1
year.1 During their course of treatment, new tumors will
form throughout the retina, most often peripheral to the
macula.2 The younger the patient is at diagnosis, the greater
the risk for new tumors to form.3 External beam radiotherapy (EBR) was the mainstay of treatment for these patients
until the 1990s. Although it would seem that radiation
would sterilize the entire retina and, thus, decrease the risk
for new tumor formation, retrospective studies have shown
differently, with the risk remaining unchanged.4 7
The risk of second malignancies from EBR led investigators to seek alternative treatment strategies in patients with
hereditary retinoblastoma.8 In the past decade, radiationsparing therapies that incorporate primary systemic chemotherapy and aggressive focal consolidation with cryotherapy, transpupillary thermotherapy, and brachytherapy have
evolved.9 19 The success of these approaches has been
extensively reported and additional benefits observed. Most
notable has been a decrease in the incidence of secondary
pineal tumors, suggesting a possible protective effect from
the chemotherapy.20 Further studies have examined the
impact of primary systemic chemotherapy on new tumor
formation in the eyes. These studies have shown that new
tumors continue to develop both during and after the completion of chemotherapy in up to 48% of treated eyes. New
tumors form most often within 5 months of the completion
of chemotherapy. Patients diagnosed at an earlier age remain at a greater risk for new tumors to form.2123 We have
studied the rate of new tumor formation in patients treated
with systemic chemotherapy and, herein, report our findings
in 116 eyes of 58 patients with hereditary retinoblastoma.
Materials and Methods
Approval was obtained from the institutional review board at St.
Jude Childrens Research Hospital to review retrospectively the
medical records of 58 consecutive patients with hereditary retinoblastoma treated with primary systemic chemotherapy between
January 1996 and August 2005. The following patient data were
extracted: gender, age at diagnosis, family history of retinoblastoma, laterality of disease, tumors per eye, ReeseEllsworth grouping of affected eyes, starting and ending dates for chemotherapy,
number of cycles of chemotherapy, chemotherapy regimen, need
for EBR and/or enucleation, and development and location (macula, midzone, and/or periphery) of new tumors after the start of
systemic chemotherapy. New tumors were defined as those lesions
that developed remote to another tumor. Tumors adjacent to a flat
chorioretinal scar from prior treatment were excluded. Multiple
grouped new tumors in the presence of overt vitreous and/or
subretinal seeds were recorded as implantations and not subject to
analysis in this study. The main outcome measured was the development of new tumors after the start of chemotherapy.
Statistical Methods
The association between ReeseEllsworth group at diagnosis (I/
II/III vs. IV/V) and number of tumors at diagnosis was investigated
using the exact Wilcoxon rank sum test. The Spearman correlation
coefficient was used to examine the association between age at
diagnosis and number of tumors. The cumulative incidence of new
tumor formation was estimated. Although interocular correlation
2078
may exist in patients with bilateral disease,24 the eye was chosen
as the unit of analysis. For eyes with multiple new tumors, the date
of first new tumor formation was used. Enucleation and EBR
before new tumor formation were considered as competing events
in this analysis. Eyes that did not develop new tumors and did not
have other events (enucleation or EBR) were censored at the date
of last follow-up. The Gray test was used to test whether youngness, ReeseEllsworth group, and family history impacted new
tumor formation.25 P values and test statistics (with corresponding
degrees of freedom) resulting from the Gray tests were reported.
This was an exploratory retrospective study, and P values should
be interpreted with caution; no adjustments were made for multiple
tests.
Results
All 58 patients were observed with serial examinations under
anesthesia inclusive of digital fundus photography based on age
and stability of disease. Of them, 34 were male and 13 had a family
history of retinoblastoma (Table 1). Patients median age at
diagnosis was 6.6 months (range, 0.237.3). Forty-eight patients presented with bilateral retinoblastoma. Of the 106 eyes
with retinoblastoma at diagnosis, 52 were classified as being in
ReeseEllsworth groups IIII and 54 were classified as being in
ReeseEllsworth group IV or V. Most eyes were in group V at
diagnosis (n 50 eyes [47%]). There were a total of 237 tumors
at diagnosis in 106 eyes in 58 children. For the 106 eyes with
tumors at diagnosis, the median number of tumors per eye was 2
(range, 19). There was no evidence of an association between
ReeseEllsworth group at diagnosis (I/II/III vs. IV/V) and number
of tumors at diagnosis (P 0.98). There was also no evidence of
an association between age at diagnosis and total number of
tumors in patients (P 0.55, 0.08).
All patients were alive at the time of analysis, with a median
follow-up from diagnosis of 5.0 years (range, 1.0 10.1). Seven
patients (12%) developed a total of 36 new tumors in 11 eyes
(Tables 2, 3 [available at http://aaojournal.org]); 6 tumors formed
in the macula, 16 in the midzone, and 14 in the periphery. The
median time from start of chemotherapy to detection of the first
new tumor was 3 months (range, 115); the latest time a new
tumor was noted to form was 24 months from the start of chemotherapy. One of these 7 patients had bilateral disease at diagnosis
and developed new tumors in both eyes approximately 1 month
after starting chemotherapy. The other 6 patients had unilateral
disease at diagnosis. Three of these 6 patients developed new
tumors in the opposite eye at approximately 3.0, 7.2, and 7.5
months after initiation of chemotherapy. The other 3 patients
developed new tumors in both eyes. Of note, none of these eyes
had EBR before development of new tumors. In addition, none of
these eyes were subsequently enucleated.
Cumulative incidences of new tumor formation at 1 and 2 years
were estimated to be 83% and 103%, respectively. Figure 1
shows the cumulative incidence of new tumor formation for all
eyes. Family history was a significant predictor of new tumor
formation (P0.001, 21 17.8). Eyes of patients with a family
history were more likely to develop new tumors than eyes of
patients without a family history; 2-year cumulative incidences
were 319% and 32% for eyes with and without family histories, respectively (Fig 2). Age at diagnosis was also a significant
predictor of new tumor formation (P0.001, 21 13.9). Eyes in
patients who were younger than 6 months at diagnosis were more
likely to develop new tumors (2-year cumulative incidence,
216%) than eyes in patients who were at least 6 months old at
diagnosis (2-year cumulative incidence, 00%) (Fig 3). All pa-
Wilson et al Incidence of New Tumor Formation after Systemic Chemotherapy
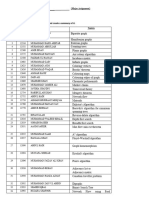
Table 1. Patient and Treatment Characteristics
Characteristic
retinoblastoma at diagnosis were studied. There was evidence that
the ReeseEllsworth grouping was a significant predictor of new
tumor formation (P 0.021, 21 5.3). All 5 eyes that had
retinoblastoma at diagnosis and later formed new tumors had a low
ReeseEllsworth classification, either group I (3 eyes) or group II
(2 eyes). The cumulative incidence of new tumor formation was
104% for ReeseEllsworth groups I to III, versus 00% for
ReeseEllsworth group IV or V (Fig 4).
N (%)
Gender
Male
Female
Age at diagnosis (mos)
Birth to 1
13
36
69
912
1215
1518
1821
2124
24
Unilateral
Bilateral
Family history
No
Yes
Chemotherapy
VC 4
VC 6
VC 7
VC 8
VC 8 VCE 3
VC 8 VT 3
VCE 6
ReeseEllsworth classification at diagnosis (n 106 eyes)
I
II
III
IV
V
34 (59%)
24 (41%)
6 (10%)
10 (17%)
11 (19%)
7 (12%)
10 (17%)
3 (5%)
0 (0%)
4 (7%)
3 (5%)
4 (7%)
10 (17%)
48 (83%)
Discussion
It has been estimated that hereditary retinoblastoma patients
will develop, on average, 2.7 tumors per eye.2 New tumors
will continue to form after initial diagnosis. Whether a
patients genetic predisposition to form new tumors can be
altered by treatment is unknown. We studied the impact of
primary systemic chemotherapy on the rate of new tumor
formation in a cohort of 58 patients with hereditary retinoblastoma. We found an overall cumulative incidence of 10%
at 2 years after the start of chemotherapy. Younger age at
diagnosis, family history of retinoblastoma, and lower
ReeseEllsworth classification were factors that significantly increased the likelihood of new tumor formation (P
0.001, P 0.001, and P 0.021, respectively). Eyes of
patients with a family history had a 31% incidence of new
tumor formation at 2 years, whereas those patients diagnosed before 6 months of age had a 21% incidence. Eyes
classified as ReeseEllsworth groups I to III had a 10%
incidence of new tumors. Each of these risk factors is intrinsically tied together. Patients with a family history are more
likely to be screened starting at birth and therefore diagnosed at
a younger age with less advanced intraocular disease.
We observed 36 new tumors in 11 eyes. Of these, 17%
(n 6) were in the macula, 44% (n 16) were in the
midzone, and 39% (n 14) were in the periphery. New
tumor formation in retinoblastoma appears to be closely tied
to retinal development. Immature retinal cells remain susceptible to second random mutations leading to inactivation
of the retinoblastoma protein and tumor development. As
the retina matures from the posterior pole towards the
45 (78%)
13 (22%)
1 (2%)
1 (2%)
5 (9%)
44 (76%)
2 (3%)
2 (3%)
3 (5%)
15 (14%)
24 (22%)
13 (12%)
4 (4%)
50 (47%)
C carboplatin; E etoposide; T topotecan; V vincristine.
tients who developed new tumors were younger than 5 months at
their initial diagnosis.
ReeseEllsworth classification was also investigated as a predictor of new tumor formation. Because many new tumors formed
in eyes with no disease at diagnosis, only the 106 eyes with
0.20
0.15
0.10
0.05
0.00
0
10
12
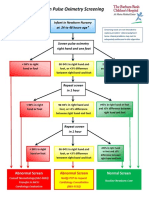
Figure 1. Cumulative incidence estimates of new tumor formation for all eyes (n 116). X-axis, years.
2079
Ophthalmology Volume 114, Number 11, November 2007
Figure 2. Cumulative incidence estimates of new tumor formation by family history (yes [solid line] vs. no [dashed line]) (P0.001, 21 17.8). X-axis,
years.
periphery, the majority of new tumors form outside the
macula closer to the midzone and periphery.
Whether these new tumors developed before, during, or
after chemotherapy is uncertain. One hypothesis is that each
new tumor represents a new mutation that occurred after the
start of chemotherapy and the tumor grew unimpeded. Alternatively, these small tumor foci may have preceded the
start of chemotherapy and not been detected. Their poorly
developed intrinsic vascularity may not have allowed cytotoxic levels of the chemotherapeutic agents to be achieved.
In these instances, the tumors growth may have been
blunted, but it continued to grow either at the completion of
chemotherapy or once resistance had been developed. This
hypothesis is in keeping with the finding of Gombos et al
that tumors 2 mm in diameter are less likely to respond to
chemotherapy.26 They concluded that the poorly developed
0.35
0.30
0.25
0.20
0.15
0.10
0.05
0.00
0
10
12
Figure 3. Cumulative incidence estimates of new tumor formation by age at diagnosis (6 months [solid line] vs. 6 months [dashed line]) (P0.001,
21 13.9). X-axis, years.
2080
Wilson et al Incidence of New Tumor Formation after Systemic Chemotherapy
0.20
0.15
0.10
0.05
0.00
0
10
12
Figure 4. Cumulative incidence estimates of new tumor formation by ReeseEllsworth classification (I/II/III [solid line] vs. IV/V [dashed line]) (P 0.021,
21 5.3). X-axis, years.
vasculature of small tumors did not allow adequate delivery
of the systemic chemotherapy. We believe that both of these
hypotheses account for tumors detected after the administration of systemic chemotherapy in our patients.
Ours was not the first study to address the impact of
treatment on the new tumor formation in patients with
hereditary retinoblastoma. Initial reports pertained to those
patients treated with EBR. Salmonsen et al reported that
11% of eyes with retinoblastoma treated with EBR developed new tumors at a mean of 3.5 months after treatment.4
Of the 61 tumors documented, 90% were in the periphery of
the retina. Their findings led them to hypothesize that
retinoblastoma has the propensity to develop in the immature retina, and thus, tumor development follows the
progression of retinal development from the posterior
pole to the ora serrata. Later, Merrill et al reported similar
findings over a 10-year study period, with an overall 13%
incidence of new tumor formation after EBR.5 However,
when patients were stratified by age, a 25% risk for those
patients diagnosed before 6 months of age was found.
Other studies have shown similar rates of new tumor
formation after EBR.6,7
Abramson et al studied 355 eyes from 325 patients with
bilateral retinoblastoma treated with modalities other than
enucleation, inclusive of EBR, intraarterial chemotherapy,
plaque brachytherapy, photocoagulation, and cryotherapy.
New tumors formed in 25% of the eyes.3 Patients diagnosed
before 6 months of age had a 45% chance of developing
new tumors, as compared with a 14% chance in those
patients diagnosed after 6 months of age. Patients diagnosed
before 2 years of age were noted to develop tumors up to 4.5
years after treatment, whereas those patients diagnosed after
2 years of age developed tumors up to 1.5 years later. A
later study by the same authors focused on new intraocular
tumors after treatment in patients with unilateral retinoblastoma.27 In contrast to their previous study, those patients
treated with enucleation were included. Overall, 6% of the
patients developed at least one new tumor in either the
treated or the untreated eye. Patients with a family history of
retinoblastoma and those patients diagnosed before 6
months of age had the greatest risk: 35% and 16%, respectively. In that study, the mean time to new tumor formation
after treatment was 0.74 years; no new tumors developed
after 7.7 years of age.
In the era of primary systemic chemotherapy for the
treatment of intraocular retinoblastoma, Scott et al were the
first to report the occurrence of new tumors.28 Four children
were found to develop 9 new tumors in 6 eyes either during
or after the completion of chemotherapy. The small series
did not permit statistical analysis but did alert us to the need
for continued close surveillance both during and after the
completion of chemotherapy. Lee et al later reported their
findings in 57 eyes of 34 patients with hereditary retinoblastoma treated initially with systemic carboplatin.21
They observed 63 new tumors in 27 eyes (47%). Of the
new tumors noted, 57% formed within months of carboplatin treatment. As in previous studies, children diagnosed before 6 months of age were at a greater risk for
new tumor formation in comparison to those diagnosed
later: 60% and 31%, respectively. The majority of new
tumors formed before 1 year of age and were detected
within 4 months of chemotherapy. Shields et al also
studied the impact of systemic chemotherapy on new
tumor formation in 162 eyes of 106 patients.22 According
to KaplanMeyer analysis, new tumors formed in 23% of
patients treated with 6 cycles of carboplatin, vincristine,
and etoposide within 1-year follow-up and in 24% by
5-year follow-up. The mean interval for new tumor formation was 5 months after diagnosis. Familial history
and younger age at diagnosis were the most important
risk factors by multivariate analysis. More recently,
Schueler et al have published their findings on 50 eyes of
32 patients with hereditary retinoblastoma treated with a
mean of 6 cycles of triple-agent chemotherapy (vincristine, etoposide, carboplatin, or cyclophosphamide).23
New tumors occurred in 48% of the eyes treated either
during or within 7 months after completion of chemotherapy. Children who developed new tumors were significantly younger at the time of diagnosis and had a
significantly lower number of tumors per eye at diagnosis. In our own study as well as those cited above, not all
patients were treated with the same chemotherapeutic
regimens. Therefore, we can only discuss the effects of
primary systemic chemotherapy in a general context
without regard to specific chemotherapeutic agents.
Even though the reported risk for new tumor formation
varies in each of the aforementioned studies, we believe the
findings are similar to ours. Incidences of new tumor for-
2081
Ophthalmology Volume 114, Number 11, November 2007
mation among the eyes treated with systemic chemotherapy,
EBR, or focal therapies do not differ. Thus, it would appear
that neither chemotherapy nor radiation alters a hereditary
retinoblastoma patients predisposition to form new tumors.
In theory, only therapies that specifically targeted retinal
development would be able to prevent new tumors from
occurring. Nonetheless, we do believe systemic chemotherapy impacts the growth of small undetected lesions by
slowing their growth and facilitating later focal consolidation. Close surveillance with serial examinations under anesthesia with meticulous attention to the developing peripheral retina remains mandatory.
References
1. Ellsworth RM. The practical management of retinoblastoma.
Trans Am Ophthalmol Soc 1969;67:462534.
2. Abramson DH, Gombos DS. The topography of bilateral
retinoblastoma lesions. Retina 1996;16:2329.
3. Abramson DH, Greenfield DS, Ellsworth RM. Bilateral
retinoblastoma: correlations between age at diagnosis and time
course for new intraocular tumors. Ophthalmic Paediatr Genet
1992;13:17.
4. Salmonsen PC, Ellsworth RM, Kitchin FD. The occurrence of
new retinoblastoma after treatment. Ophthalmology 1979;86:
837 43.
5. Merrill PT, Buckley EG, Halperin EC. New and recurrent
tumors in germinal retinoblastoma: is there a treatment effect?
Ophthalmic Genet 1996;17:115 8.
6. Hernandez JC, Brady LW, Shields JA, et al. External beam
radiation for retinoblastoma: results, patterns of failure and a
proposal for treatment guidelines. Int J Radiat Oncol Biol
Phys 1996;35:12532.
7. Messmer EP, Sauerwein W, Heinrich T, et al. New and recurrent
tumor foci following local treatment as well as external beam
radiation in eyes of patients with hereditary retinoblastoma.
Graefes Arch Exp Clin Exp Ophthalmol 1990;228:426 31.
8. Abramson DH, Frank CM. Second nonocular tumors in survivors of bilateral retinoblastoma: a possible age effect on
radiation-related risk. Ophthalmology 1998;105:5739.
9. Wilson MW, Rodriguez-Galindo C, Haik BG, et al. Multiagent chemotherapy as neoadjuvant treatment for multifocal
intraocular retinoblastoma. Ophthalmology 2001;108:2106
14, discussion 2114 5.
10. Rodriguez-Galindo C, Wilson MW, Haik BG, et al. Treatment
of intraocular retinoblastoma with vincristine and carboplatin.
J Clin Oncol 2003;21:2019 25.
11. Shields CL, De Potter P, Himelstein B, et al. Chemoreduction
in the initial management of intraocular retinoblastoma. Arch
Ophthalmol 1996;114:1330 8.
12. Friedman DL, Himelstein B, Shields CL, et al. Chemoreduction and local ophthalmic therapy for intraocular retinoblastoma. J Clin Oncol 2000;18:127.
2082
13. Gallie BL, Budning A, DeBoer G, et al. Chemotherapy with
focal therapy can cure intraocular retinoblastoma without radiotherapy. Arch Ophthalmol 1996;114:1321 8.
14. Murphree AL, Villablanca JG, Deegan WF III, et al. Chemotherapy plus local treatment in the management of intraocular
retinoblastoma. Arch Ophthalmol 1996;114:1348 56.
15. Kingston JE, Hungerford JL, Madreperla SA, Plowman PN.
Results of combined chemotherapy and radiotherapy for advanced intraocular retinoblastoma. Arch Ophthalmol 1996;
114:1339 43.
16. Greenwald MJ, Strauss LC. Treatment of intraocular retinoblastoma with carboplatin and etoposide chemotherapy. Ophthalmology 1996;103:1989 97.
17. Shields CL, Shields JA, Needle M, et al. Combined chemoreduction and adjuvant treatment for intraocular retinoblastoma.
Ophthalmology 1997;104:210111.
18. Beck MN, Balmer A, Dessing C, et al. First-line chemotherapy with local treatment can prevent external-beam irradiation
and enucleation in low-stage intraocular retinoblastoma. J Clin
Oncol 2000;18:28817.
19. Brichard B, De Bruycker JJ, De Potter P, et al. Combined
chemotherapy and local treatment in the management of
intraocular retinoblastoma. Med Pediatr Oncol 2002;38:
4115.
20. Shields CL, Meadows AT, Shields JA, et al. Chemotherapy
for retinoblastoma may prevent intracranial neuroblastic malignancy (trilateral retinoblastoma). Arch Ophthalmol 2001;
119:1269 72.
21. Lee TC, Hayashi NI, Dunkel IJ, et al. New retinoblastoma
tumor formation in children initially treated with systemic
carboplatin. Ophthalmology 2003;110:1989 94.
22. Shields CL, Shelil A, Cater J, et al. Development of new
retinoblastoma after 6 cycles of chemoreduction for retinoblastoma in 162 eyes of 106 consecutive patients. Arch Ophthalmol 2003;121:1571 6.
23. Schueler AO, Anastassiou G, Jurklies C, et al. De novo
intraocular retinoblastoma development after chemotherapy
in patients with hereditary retinoblastoma. Retina 2006;26:
42531.
24. Chaum E, Ellsworth RM, Abramson DH, et al. Cytogenetic
analysis of retinoblastoma: evidence for multifocal origin and
in vivo gene amplification. Cytogenet Cell Genet 1984;38:
8291.
25. Gray RJ. A class of K-sample tests for comparing the cumulative
incidence of a competing risk. Ann Stat 1988;16:114154.
26. Gombos DS, Kelly A, Coen PG, et al. Retinoblastoma treated
with primary chemotherapy alone: the significance of tumour
size, location and age. Br J Ophthalmol 2002:86:80 3.
27. Abramson DH, Gamell LS, Ellsworth RM, et al. Unilateral
retinoblastoma: new intraocular tumours after treatment. Br J
Ophthalmol 1994;78:698 701.
28. Scott IU, Murray TG, Toledano S, OBrien JM. New retinoblastoma tumors in children undergoing systemic chemotherapy [letter]. Arch Ophthalmol 1998;116:1685 6.
Wilson et al Incidence of New Tumor Formation after Systemic Chemotherapy
Table 2. Patients with New Tumor Formation after the Start of Chemotherapy
Patient
Gender
Age at Diagnosis (mos)
Laterality
Family History
Duration of Chemotherapy (mos)
Chemotherapy Agents
1
2
3
4
5
6
7
M
F
F
M
M
M
F
4.8
1.5
0.3
1.6
0.2
2.8
2.8
Unilateral
Unilateral
Unilateral
Unilateral
Unilateral
Bilateral
Unilateral
No
No
Yes
Yes
Yes
Yes
No
5.8
5.1
11.0
9.5
5.0
9.5
6.4
VC 8
VC 8
VC 8 VT 3
VC 8 VCE 3
VC 8
VC 8 VT 3
VC 8
C carboplatin; E etoposide; F female; M male; T topotecan; V vincristine.
Table 3. Eyes with New Tumor Formation
ReeseEllsworth
Group
Age at
Diagnosis (mos)
Age at First
New Tumor (mos)
Total No. of New
Tumors
Identified
Ia
4.8
1.5
0.3
0.3
1.6
12
9
3
6
3
1
1
1
2
9
1.6
15
Right
0.2
5
6
Left
Right
1
3
Ia
IIa
0.2
2.8
15
4
1
10
Left
IIa
2.8
Right
2.8
Patient
Eye
Tumors at
Diagnosis
1
2
3
3
4
Left
Right
Right
Left
Right
0
0
1
0
1
Left
Ia
New Tumor
Location
Periphery, 1
Macula, 1
Midzone, 1
Macula, 2
Macula, 1;
midzone, 4;
periphery, 4
Macula, 1;
midzone, 3;
periphery, 1
Macula, 1;
midzone, 1
Midzone, 1
Midzone, 4;
periphery, 6
Midzone, 2;
periphery, 1
Periphery, 1
Time from
Chemotherapy
Start to First New
Tumor (mos)
7
7
2
5
1
13
3
15
1
1
3
2082.e1
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- PolyarthritisDokumen6 halamanPolyarthritisromeoenny4154Belum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- 51 Allergens Set: Sr. No. Patch Test Allergen Price (RS.)Dokumen2 halaman51 Allergens Set: Sr. No. Patch Test Allergen Price (RS.)romeoenny4154Belum ada peringkat
- Dizziness in PaedDokumen7 halamanDizziness in Paedromeoenny4154Belum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Contoh ReviewDokumen6 halamanContoh Reviewromeoenny4154Belum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Pneumonia and Respiratory Tract Infections in ChildrenDokumen37 halamanPneumonia and Respiratory Tract Infections in ChildrenjayasiinputBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- List of Allergens: Skin Prick Test Allergens 01/29/2016Dokumen3 halamanList of Allergens: Skin Prick Test Allergens 01/29/2016romeoenny4154Belum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Acute Fever in Children and InfantDokumen26 halamanAcute Fever in Children and Infantromeoenny4154Belum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- HemophiliaDokumen2 halamanHemophiliaromeoenny4154Belum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Ulceration Slides 090331Dokumen62 halamanUlceration Slides 090331mumutdwsBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Clinical Reasoning Handout: URI Symptoms Sore Throat 1) Pearls BackgroundDokumen5 halamanClinical Reasoning Handout: URI Symptoms Sore Throat 1) Pearls Backgroundromeoenny4154Belum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Febrile Seizure GuidelineDokumen1 halamanFebrile Seizure GuidelinesmileyginaaBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Adhd Scoring ParentDokumen3 halamanAdhd Scoring Parentromeoenny4154Belum ada peringkat
- DD Viral ExantemDokumen4 halamanDD Viral Exantemsiska_mariannaBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Febrile Neonate Clinical Practice Guideline: CatheterizedDokumen1 halamanFebrile Neonate Clinical Practice Guideline: Catheterizedromeoenny4154Belum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Afebrile SeizuresDokumen11 halamanAfebrile SeizuresMai Hunny100% (1)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Congenital Heart Disease 2014Dokumen1 halamanCongenital Heart Disease 2014romeoenny4154Belum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Children Perio DiseasesDokumen9 halamanChildren Perio Diseasesdr parveen bathlaBelum ada peringkat
- Acute Stridor Diagnostic Challenges in Different Age Groups Presented To The Emergency Department 2165 7548.1000125Dokumen4 halamanAcute Stridor Diagnostic Challenges in Different Age Groups Presented To The Emergency Department 2165 7548.1000125romeoenny4154Belum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Calvin K.W. Tong Approach To A Child With A Cough: General PresentationDokumen5 halamanCalvin K.W. Tong Approach To A Child With A Cough: General Presentationromeoenny4154Belum ada peringkat
- Bronchiolitis Clinical Guideline2014Dokumen2 halamanBronchiolitis Clinical Guideline2014romeoenny4154Belum ada peringkat
- Common Anemia in Pediatric BRM - PM - V1P4 - 03Dokumen12 halamanCommon Anemia in Pediatric BRM - PM - V1P4 - 03romeoenny4154Belum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Guidelines Clinical Management Chikungunya WHODokumen26 halamanGuidelines Clinical Management Chikungunya WHOFábio CantonBelum ada peringkat
- Clinical Reasoning Handout: URI Symptoms Sore Throat 1) Pearls BackgroundDokumen5 halamanClinical Reasoning Handout: URI Symptoms Sore Throat 1) Pearls Backgroundromeoenny4154Belum ada peringkat
- Common Anemia in Pediatric BRM - PM - V1P4 - 03Dokumen12 halamanCommon Anemia in Pediatric BRM - PM - V1P4 - 03romeoenny4154Belum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Approach To Acute Arthritis in Kids: Allyson Mcdonough, MD Baylor Scott & White Health Department of RheumatologyDokumen35 halamanApproach To Acute Arthritis in Kids: Allyson Mcdonough, MD Baylor Scott & White Health Department of Rheumatologyromeoenny4154Belum ada peringkat
- DD Viral ExantemDokumen4 halamanDD Viral Exantemsiska_mariannaBelum ada peringkat
- Common Anemia in Pediatric BRM - PM - V1P4 - 03Dokumen12 halamanCommon Anemia in Pediatric BRM - PM - V1P4 - 03romeoenny4154Belum ada peringkat
- Asthma ED Clinical Guideline2014Dokumen5 halamanAsthma ED Clinical Guideline2014romeoenny4154Belum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (120)
- GinggivostomatitisDokumen6 halamanGinggivostomatitisromeoenny4154Belum ada peringkat
- Croup GuidelineDokumen17 halamanCroup Guidelineromeoenny4154Belum ada peringkat
- Subliminal Perception and Extrasensory PerceptionDokumen19 halamanSubliminal Perception and Extrasensory PerceptionAnne Jenette CastilloBelum ada peringkat
- Fabrication of Mortar Mixer and CHB Filler PumpDokumen15 halamanFabrication of Mortar Mixer and CHB Filler PumpRenjo Kim VenusBelum ada peringkat
- Dos and DontsDokumen1 halamanDos and DontsLeah GlickBelum ada peringkat
- Percentage Grade5Dokumen24 halamanPercentage Grade5marissa menesesBelum ada peringkat
- Graph Theory (B)Dokumen2 halamanGraph Theory (B)Waqar RoyBelum ada peringkat
- Fundamentals of Physics Sixth Edition: Halliday Resnick WalkerDokumen3 halamanFundamentals of Physics Sixth Edition: Halliday Resnick WalkerAhmar KhanBelum ada peringkat
- 9th Computer Notes Full BookDokumen14 halaman9th Computer Notes Full BookKot Abdul Malik High SchoolBelum ada peringkat
- It'S Not A Lie If You Believe It: LyingDokumen2 halamanIt'S Not A Lie If You Believe It: LyingNoel ll SorianoBelum ada peringkat
- Gender Differences in Self-ConceptDokumen13 halamanGender Differences in Self-Conceptmaasai_maraBelum ada peringkat
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Ebook PDF Elementary Algebra 4th Edition by Michael III SullivanDokumen41 halamanEbook PDF Elementary Algebra 4th Edition by Michael III Sullivansean.cunningham518Belum ada peringkat
- Sentence Cont. ExerciseDokumen6 halamanSentence Cont. ExerciseKim Thy Trần PhạmBelum ada peringkat
- Attachment 4A Security Classification GuideDokumen42 halamanAttachment 4A Security Classification GuidepingBelum ada peringkat
- Sap 47n WF TablesDokumen56 halamanSap 47n WF TablesjkfunmaityBelum ada peringkat
- Qualifications Recruitment Promotions Scheme - University AcademicsDokumen10 halamanQualifications Recruitment Promotions Scheme - University Academicsuteachers_slBelum ada peringkat
- Catalogo Molas PratoDokumen176 halamanCatalogo Molas Pratocassio_tecdrawBelum ada peringkat
- 16 Degrees ScorpioDokumen21 halaman16 Degrees Scorpiostrength17Belum ada peringkat
- Reflection and Refraction of LightDokumen34 halamanReflection and Refraction of Lightseunnuga93Belum ada peringkat
- Transportation Impact Handbook 2010Dokumen246 halamanTransportation Impact Handbook 2010Enrique Márquez100% (1)
- Chap 4 - Shallow Ult PDFDokumen58 halamanChap 4 - Shallow Ult PDFChiến Lê100% (2)
- Jump in A Teachers BookDokumen129 halamanJump in A Teachers BookShei QuinterosBelum ada peringkat
- Sample PREP-31 Standard Sample Preparation Package For Rock and Drill SamplesDokumen1 halamanSample PREP-31 Standard Sample Preparation Package For Rock and Drill SampleshBelum ada peringkat
- Ascc Catalog 2014-2016Dokumen157 halamanAscc Catalog 2014-2016api-261615090Belum ada peringkat
- Chapter 4Dokumen21 halamanChapter 4Ahmad KhooryBelum ada peringkat
- NBA AwarenessDokumen39 halamanNBA AwarenessRaja SekarBelum ada peringkat
- EI in NegotiationsDokumen22 halamanEI in NegotiationspranajiBelum ada peringkat
- MAX31865 RTD-to-Digital Converter: General Description FeaturesDokumen25 halamanMAX31865 RTD-to-Digital Converter: General Description FeaturespaKoSTe1Belum ada peringkat
- Function, Roles, and Skills of A Manager: Lesson 3Dokumen12 halamanFunction, Roles, and Skills of A Manager: Lesson 3Christine Joy ResponteBelum ada peringkat
- Mann Whitney U: Aim: To Be Able To Apply The Mann Whitney U Test Data and Evaluate Its EffectivenessDokumen16 halamanMann Whitney U: Aim: To Be Able To Apply The Mann Whitney U Test Data and Evaluate Its EffectivenessAshish ThakkarBelum ada peringkat
- Xaviers Institute of Social Service: Assignment On Quantitative TechniquesDokumen20 halamanXaviers Institute of Social Service: Assignment On Quantitative Techniquesravi kumarBelum ada peringkat
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDari EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BePenilaian: 2 dari 5 bintang2/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDari EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsBelum ada peringkat
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDari EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisPenilaian: 4.5 dari 5 bintang4.5/5 (42)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDari EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityPenilaian: 4 dari 5 bintang4/5 (24)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDari EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityPenilaian: 4 dari 5 bintang4/5 (3)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDari EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedPenilaian: 5 dari 5 bintang5/5 (80)