Occupational Profile M Viveros Final
Diunggah oleh
api-293258738Deskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Occupational Profile M Viveros Final
Diunggah oleh
api-293258738Hak Cipta:
Format Tersedia
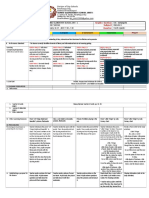
Running head: OCCUPATIONAL PROFILE AND INTERVENTION
Occupation Profile and Intervention Plan for Fieldwork
Mallory Viveros
Touro University Nevada
OCCUPATIONAL PROFILE AND INTERVENTION
Occupational Profile
Mr. Garcia is an 83 year old man retired from the United States Army and veteran of the
Korean War. He lives alone in a double wide trailer in Boulder City, Nevada and has done so
ever since he was honorably discharged from the army. He does not have a significant other and
does not have children, but does have three nephews and one niece. He is originally from
Michigan, and that is where all of his family is currently living. His sister is his power of
attorney, and makes all financial decisions for him. Mr. Garcia also has two brothers who call
him and converse with him quite often.
Although he chooses to live far from his family he values the time he gets to talk to them
on the phone because it is a significant part of his social interaction during the week. After
discharging from the army, he worked for Ford Motor Company as a parts assembler. He enjoyed
this job very much because he has a great interest in automobiles and putting together parts to
create a final product. Having been retired for a couple of decades now he enjoys participating in
the citys senior group, going to the park, and reading his newspaper. He is especially pleased
when the senior group has events involving games or fitness because he was an avid weight lifter
and athlete in his youth.
Mr. Garcia is seeking occupational therapy services due to experiencing days worth of
intolerable back pain, and undergoing a kyphoplasty due to a compression fracture at T9-T10. He
has a history of back pain, had a laminectomy at L4 nearly forty years ago, and has experienced
chronic back pain ever since then. Although he has been living with chronic lower back pain for
decades, last week he experienced acute middle back pain due to the compression fracture.
Following the kyphoplasty he is experiencing acute middle back pain, and would like to decrease
the amount of pain he is currently feeling. Due to his spinal surgery he must follow three spinal
OCCUPATIONAL PROFILE AND INTERVENTION
precautions for the next six weeks, and he is concerned this will affect his ability to perform selfcare activities at home.
In addition to his rehab diagnosis he has a medical history of chronic obstructive
pulmonary disease (COPD), lymphatic leukemia, and bronchiectasis. These three pulmonary
conditions greatly affect his ability to fully engage in meaningful occupations. He is dependent
on supplemental oxygen every day, but even with the support of supplemental oxygen he
frequently fatigues when engaging in activities of daily living (ADL). This concerns him because
he would like to be at home and enjoy his time without having to worry about his oxygen
saturation levels after participating in an activity.
At home Mr. Garcia gets frustrated with his decreased endurance levels and activity
tolerance because he quickly becomes short of breath. After attempting an activity or after
completion of an activity the client has to find a spot to sit so he can regain a normal breathing
pattern. He does this by resting and taking deep breaths through his mouth. Mr. Garcia is worried
that he will soon not be able to do any activities at home without the help of his caregiver. He has
a caregiver through the Visiting Angels caregiver program that visits him three days out of the
week. The caregiver is responsible for the clients shopping, meal preparation, and household
cleaning. He requires help for these three instrumental activities of daily living (IADL), but is
still able to drive and participate in self-care management.
Mr. Garcia is able to independently engage in grooming, showering, and dressing while
carrying his portable oxygen tank with him as he engages in each occupation. However, Mr.
Garcia becomes short of breath due to over exertion during occupational performance, which
requires him to frequently check his oxygen saturation levels. His dependence on supplemental
oxygen and lack of furniture to sit and rest on during activities is a current barrier affecting his
OCCUPATIONAL PROFILE AND INTERVENTION
ability to successfully participate in these self-care occupations. Back pain in addition to the
clients decreased endurance and shortness of breath is another main barrier that is preventing
him from being able to participate in IADLs and successfully complete ADLs from time to time.
The clients internal motivation to maintain independence in self-care, and endure the
difficulties of his pulmonary conditions supports his participation in occupations. Despite the
pain, fatigue, and trouble with breathing, he still desires to independently engage in self-care.
Even though he relies on his caregiver to shop and prepare meals for him he is able to heat up the
prepared meals independently when he is alone in his home. At times the clients external
environment becomes a barrier for him to complete ADLs such as showering and grooming. His
bathroom has a tub shower without grab bars or a shower chair. When the client becomes short
of breath or becomes fatigued from walking from the living room to the bathroom his activity
tolerance declines.
Recently the clients physician informed him that his prognosis for leukemia would only
allow him close to six more months of life. His religious values and deep spirituality has helped
him cope with the updated prognosis and reality of his declining health. He is experiencing
symptoms of frustration with his prognosis because he dedicated most of his life to staying fit by
weight training and eating healthy. He is able to overcome these feelings of frustration by
continuing to attend senior community group meetings and going to the park. He is interested in
these two things because he has a passion for sports and fitness.
Before attending group meetings or going to the park he follows a morning routine
involving retrieving the newspaper from the driveway, eating, then grooming. One constant in
his daily routine is checking his oxygen tubes making sure there are no tangles and monitoring
the level of liters every morning. Since being diagnosed with COPD and leukemia his routines
OCCUPATIONAL PROFILE AND INTERVENTION
have changed and revolves around how much energy he has at the moment. The clients main
priority since his updated prognosis is to decrease his back pain and improve his quality of life.
He would like to continue participating in his senior group, become more independent in meal
preparation, and reduce the incidences of becoming easily fatigued during self-care activities.
Occupational Analysis
Mr. Garcia participated in a 60 minute occupational therapy initial evaluation two days
after his kyphoplasty. The evaluation involved obtaining information necessary to create an
occupational profile. The information gathered by the therapist involved: occupational and
medical history, roles, leisure, routines, and current concerns of the client. After providing
information for the occupational profile the client participated in total body dressing to assess his
range of motion and level of independence.
Context /Setting
The evaluation took place in both the clients hospital room and in the ADL room on the
acute rehabilitation unit of Valley Hospital. The ADL room is fully equipped with a full
functioning kitchen, bathroom with shower, and a bed. The evaluation took place immediately
after the client returned to his room from eating breakfast in the dining hall. The client was
informed of the evaluation at his bedside in his hospital room. The hospital room is used so the
therapist can assess the clients bed and functional mobility.
Activity and Performance
Mr. Garcia was supervised in a sit to stand transfer from bed to wheelchair in order to
participate in functional mobility from his room to the ADL room to complete the initial
evaluation. He was able to get out of bed without grabbing the bedrails, and only required
assistance from the therapist to switch out his oxygen from the hospital wall to the portable tank.
OCCUPATIONAL PROFILE AND INTERVENTION
Mr. Garcia was able to wheel himself to the ADL room in the wheelchair. Once in the
room and finished discussing his medical history with the therapist the client participated in total
body dressing activities. He was asked to don and doff his pants as well as a pair of socks. Due to
the clients recent kyphoplasty he was educated on the importance of maintaining three spinal
precautions: no bending, lifting, or twisting. The client was provided with adaptive equipment
including a reacher, dressing stick, sock aid, and long handled shoehorn to increase independence
in lower body dressing while maintain spinal precautions. He has never used adaptive equipment
before, so he was instructed how to operate each device prior to starting the dressing activities.
Mr. Garcia expressed that he did not need to use the adaptive equipment because he is
capable of dressing without it. He demonstrated how he has been dressing with his chronic back
pain and spinal precautions. Although he was able to don and doff his pants, he became short of
breath and quickly fatigued. After explanation of how the adaptive equipment could help to
conserve energy and maintain spinal precautions the client tried lower body dressing with the hip
kit. He was able to successfully don and doff his pants using the reacher and dressing stick with
minimal tactile and verbal cuing. He did experience some fatigue when standing to pull up his
pants, and rushed to complete the task causing him to become more fatigued as he expended
more energy while hurrying. He was able to successfully don and doff a pair of socks with three
verbal cues involving instructions on how to use the sock aid.
Key Observations
During the activity the client required three reminders to maintain spinal precautions
while dressing. He also required steadying assistance when standing to pull up his pants around
his waist due to poor balance. The client is seeking occupational therapy services due to living
with chronic back pain and acute middle back pain as a result of his kyphoplasty. Although he
OCCUPATIONAL PROFILE AND INTERVENTION
has been referred because of his spinal surgery, he is also having difficulty engaging in
occupations both ADLs and IADLs due to COPD and lymphocytic leukemia.
Impacted Domains
The domains of occupational therapy that are significantly impacting the clients ability
to successfully engage in occupations are client factors, performance patterns, and context and
environments. Currently dressing, functional mobility, shopping, meal preparation, and cleaning
are impacted by his symptoms of back pain and shortness of breath. According to the
Occupational Therapy Practice Framework Third Edition (American Occupational Therapy
Association [AOTA], 2014), Client factors include (1) values, beliefs, and spirituality; (2) body
functions; and (3) body structures that reside within the client that influence the clients
performance in occupations (p. s22). Mr. Garcias client factors of back pain and respiratory
dysfunction greatly inhibit his successful completion of occupations because he has difficulty
enduring during ADLs and IADLs because his respiratory diseases causes shortness of breath
and fatigue.
The clients routines for total body dressing, grooming, and showering are making it
somewhat difficult for him to follow spinal precautions while engaging these activities. He
expressed frustration with being provided with adaptive equipment to perform occupations such
as dressing, something he has done by himself for several decades. His temporal context of two
days status post kyphoplasty and physical environment of being in a hospital is altering the way
he normally performs dressing, thus the reason why his independence level has decreased since
being admitted to the hospital.
Problem List
OCCUPATIONAL PROFILE AND INTERVENTION
1.
2.
3.
4.
5.
Client requires Min A for lower body dressing due to spinal precautions.
Client requires Min A in showering 10/10 body parts due to spinal precautions.
Client requires frequent rest breaks for functional mobility due to back pain.
Client requires Min A with toileting due to spinal precautions.
Client requires min verbal cues for grooming due to noncompliance of spinal
precautions.
Reasoning of Prioritization
The clients problem list is ordered from most significant to the client to least significant.
The client has actively expressed his frustration with becoming short of breath and easily
fatigued when dressing his lower body due to his pulmonary disorders. Now the client is also
experiencing acute middle back pain and has to maintain spinal precautions when dressing his
lower body. This increased his frustration with his decreased level of independence, so it is
incredibly important to provide the client with the tools and education to increase his
independence in this activity as soon as possible.
Maintenance of spinal precautions added on to his already existing fatigue has also
negatively impacted his ability independently shower. Dressing is a higher priority for the client
because he has to be able to dress before and after showering. The third problem is that the
client requires frequent rest breaks in between functional transfer, which directly impacts his
independence level with toileting because it may take him longer to transfer on to the toilet. The
hospital rooms all have a bathroom in each room, but client must notify hospital staff anytime
they need to use the restroom. The client expressed frustration with this policy because it takes
him longer to get to the toilet, and waiting on staff increases the amount of time he has to wait
until he can use the toilet.
The fifth problem and least significant to the client is grooming with supervision
assistance. Currently the client is unable to engage in grooming tasks without supervision
OCCUPATIONAL PROFILE AND INTERVENTION
because he needs reminders to follow and maintain all three spinal precautions. Grooming is
important to the client, but he values showering more so because he no longer shaves and has
easy accessibility to the sink in his hospital room. Before the clients compression fracture and
kyphoplasty he was independent in total body dressing, showering, functional mobility, and
grooming. Although he would fatigue and at times become short of breath, he was always able to
participate in these occupations and wishes to soon be able to do them independently sooner
rather than later.
Intervention Plan and Outcomes
Long Term Goal 1
Client will perform lower body dressing with Modified Independence within 2 weeks.
Short Term Goal 1a. Client will safely retrieve and transport clothing from closet
maintain 3/3 spinal precautions.
Intervention. The client will participate in a standing meal preparation activity in order
to promote balance, functional mobility, and maintenance of 3/3 spinal precautions. This
intervention utilizes occupation as a means Meal preparation is an occupation that the client
wishes he could have more active participation in. The client currently does no more than heat up
meals that have already been prepared for him by his caregiver, and hope to be able to have a
bigger part in the process. The standing meal preparation activity will help organize the clients
movement when following spinal precautions.
Instruction to maintain 3/3 spinal precautions and use of reacher for meal preparation will
be provided to the client before starting the activity. The client will perform a sit to stand transfer
from his wheelchair to stand at the kitchen countertop, then begin preparing macaroni and cheese
from a box. All kitchenware and food items are placed more than arms reach to facilitate use of
OCCUPATIONAL PROFILE AND INTERVENTION
10
the reacher. The client will use a walker with a basket to prevent fatigue and shortness of breath
during the activity.
Approach. The occupational therapist should utilize the modify approach for this
intervention to support the clients performance in meal preparation. The inhibiting factors that
have been preventing the client to engage in meal preparation can be combated with the use of
adaptive equipment. During the intervention the client will be provided with a front wheel
walker with a basket accessory, and a reacher to help maintain 3/3 spinal precautions. This
approach will afford the client the opportunity to safely participate in meal preparation in his
own home again.
Grading. To meet the needs of the client and provide an appropriate level of challenge
for the client the intervention can be graded up or down. The activity can be graded down by
setting up the kitchenware: pots and utensils. This will decrease the amount of time the client has
to stand, but still allow him to engage in functional ambulation to retrieve the ingredients from
the refrigerator. To grade up the activity the therapist could place the kitchenware in different
location throughout the kitchen to increase the amount of standing and functional ambulation the
client will have to engage in.
Evidence Based Article. Eschenfelder (2005) conducted a qualitative research study
aimed to determine if occupational therapists were creating goals for treatment plans that were
corresponding with meaningful life experiences of their clients. The research took place in a
skilled nursing facility with a sample of eight older adult residents. Theses eight individuals all
volunteered to be in the study. The participants were asked to share what domains of
occupational therapy are most meaningful to them. Personal accounts from all eight participants
involved stories about their past roles and occupations that were most meaningful to them.
OCCUPATIONAL PROFILE AND INTERVENTION
11
Indicating interest in regaining the ability to participate in those roles and engage in those
occupations again just as Mr. Garcia was interested in preparing meals for himself again.
Eschenfelder (2005), notes the goals for all eight participants were congruent with
meaningful past occupations. The results emphasize the importance of utilizing the information
provided during an evaluation regarding the clients interests, past roles, and routines. For
example, one participant expressed her desire to be able to prepare and cook meals for her
daughter because she enjoyed feeding her family. With this information the therapist created an
intervention goal having the client teach her daughter how to cook because it was more
physically appropriate for the client. Eschenfelder (2005), continues to note the significance of
identifying how performance in these occupations has changed over time due to illness or injury.
Therapists can use this information to create meaningful goals that reflect the clients interests
and values even if restoration of the task is not feasible the therapist can create a meaningful
intervention related to their interests in order to motivate client participation.
Outcome. The desired outcome for this meal preparation intervention is participation. By
participating in this intervention the client will improve his standing tolerance, endurance levels,
and practice maintenance of spinal precautions during functional activities, which are all
required for safely retrieving clothing from the hospital closet. Altogether this will allow Mr.
Garcia to engage in meal preparation, which is an occupation he desires to be more involved in.
The adaptive equipment provided to Mr. Garcia will allow him to continue to participate in meal
preparation after his discharge from acute rehab to his home.
Short Term Goal 1b. Client will don pants using reacher requiring 3 or fewer verbal
cues to maintain 3/3 spinal precautions.
OCCUPATIONAL PROFILE AND INTERVENTION
12
Intervention. The client will participate in skilled training of proper use of adaptive
equipment for lower body dressing. Mr. Garcia has difficulty following spinal precautions during
lower body dressing because he is used to his normal dressing routine prior to surgery.
Instruction will be given to the client of safe techniques to don pants with the use of a front
wheel walker, dressing stick, and reacher. The therapist will demonstrate how to use the adaptive
equipment to get both lower extremities through each pant legs, and use the walker for stability
when pulling pants around the waist. The client will then practice this technique taking rest
breaks as needed.
Approach. The most appropriate intervention approach for this intervention is modify.
The intervention will provide instruction on a modified way of completing lower body dressing.
The adaptive equipment provided to Mr. Garcia will modify the task of pulling pants over his
legs, and the walker will modify the task of pulling his pants around his waist.
Evidence Based Article. OToole, Connolly, and Smith (2013), investigated the potential
impact occupational based interventions could have on clients living with multiple chronic
diseases. The study aimed to identify the effects interventions created specifically for individuals
with chronic diseases would have on the participants quality of life, occupational performance,
and self-efficacy. The study was based in a community group setting involving sixteen
participants. The intervention incorporated education on self-management and individual goal
setting (O'Toole et al., 2013). Goals were set for participants with a focus on supporting
occupational performance while managing their chronic diseases.
To be able to measure if interventions on goal setting and self-management would
positively affect clients occupational performance a pre and posttest was given to the
participants. To determine levels of self-efficacy, the Stanford Self-Efficacy for Managing
OCCUPATIONAL PROFILE AND INTERVENTION
13
Chronic Disease six item scale was administered to each participant. Results indicate significant
changes with participants self-efficacy after completing the eight week occupational based
intervention.
Outcome. The expected outcome of this intervention is prevention. Due to the clients
spinal precautions the goal is to have the client perform lower body dressing safely without
breaking spinal precautions. Spinal precautions are put in place in order to prevent injury at the
surgical site.
Long Term Goal 2
Client will complete showering with Modified Independence within 2 weeks.
Short Term Goal 2a. Client will shower maintaining 3/3 spinal precautions with 3 or
fewer verbal cues within 1 week.
Intervention. The client will participate in skilled instruction on use of adaptive
equipment for showering when following spinal precautions. The client will be provided
adaptive equipment including: long handled sponge, reacher and handheld shower head to
facilitate maintenance of spinal precautions during showering. The client will be use the adaptive
equipment to wash 10/10 body parts during this activity. The client will instructed with contact
assistant from therapist to ensure safe washing and efficient use of the adaptive equipment.
Approach. The intervention approach used by the therapist leading the activity is modify.
The washing tasks of showering are being modified with the use of adaptive equipment. Mr.
Garcia cannot bend down or lean forward like he usually would during his showering routine, so
it is important to provide him instruction on how to adapt to his new showering routine based off
of his spinal precautions.
OCCUPATIONAL PROFILE AND INTERVENTION
14
Evidence Based Article. Wielandt, McKenna, Tooth, and Strong (2001), conducted a
study aimed to assess the use and benefits of adaptive equipment for bathing. In this study
participants were given adaptive equipment and durable medical equipment to help support their
engagement in bathing tasks post discharge. An aim of this research study was to determine how
often clients were actually using the equipment provided to them and to gain a clients
perspective of the equipment. This information was gained by administering a questionnaire that
asked participants if there was any benefit to using the adaptive equipment and if participants
had a choice in what equipment they would be using.
A significant finding that is relevant to client education during an intervention plan took
note of the importance of training clients how to properly use the adaptive equipment. Another
26.9 % of the equipment had been discarded since discharged because patients stated that they
did not know how to use the equipment correctly (Wielandt et al., 2001, p.12). It is incredibly
important to provide training and instruction to clients during treatment sessions, so that they can
gain the benefits of using adaptive equipment for safe and functional bathing not only during
treatment, but after discharge when the therapist is no longer there to provide cuing.
Outcome. The anticipated outcome for this intervention is improvement in occupational
performance. Currently Mr. Garcia is having difficulty showering 10/10 body parts because of
his spinal precautions. The use of adaptive equipment will allow him to reach all areas of his
body while continuing to maintain all three spinal precautions. Therefore, the intervention will
improve the clients current occupational performance.
Short Term Goal 2b. Client will shower using shower chair with standby assistance
within 1 week.
OCCUPATIONAL PROFILE AND INTERVENTION
15
Intervention. Client will collaborate with therapist to determine the most appropriate
durable medical equipment to be used during showering activities. The therapist will educate the
client of the importance of using a shower chair when showering to prevent fatigue and promote
safe showering. The client will be instructed in the use of a shower chair and will practice
transferring on and off the shower chair during showering. Demonstration of safe transferring
techniques to standup from the shower chair will be provided to the client in order to ensure
safety awareness in a wet environment and to help him follow spinal precautions.
Approach. The intervention approach the therapist is using to guide their intervention is
prevent. This intervention utilizes a shower chair to prevent any injury or harm to the client while
moving in a wet environment. The shower chair will help to prevent the client from breaking
spinal precautions as well as inflicting pain in his back.
Evidence Based Research. Stark (2004), led a research study aimed to identify the
potential benefits of home modification intervention program for older adults with physical
disabilities. The study identified home modification as making architectural modifications in
participants home or providing them with adaptive equipment. In order to assess any changes in
participant satisfaction with occupational performance all thirty participants were asked to
complete the Canadian Occupational Performance Measure (COPM) before and after
intervention. The participants also participated in the Functional Independence Measure (FIM)
assessment to evaluate their level of performance before and after home modification was
provided to them.
Scores on the COPM pretest and posttest were compared after home modifications were
complete and participants were able to engage in occupations with modification. A significant
improvement was made from the initial mean score of 2.25 to 7.69 on the pretest (Stark, 2004).
OCCUPATIONAL PROFILE AND INTERVENTION
16
This COPM was a great measuring tool to help researchers identify how satisfied participants
were with their occupational performance, and because their satisfaction scores improved greatly
after home modifications it can be said that both architectural modification and adaptive
equipment support an individual's occupational performance.
Outcome. The expected outcome for this intervention is improvement in occupational
performance. The use of the shower chair will reduce several limitations he is currently
experiencing when participating in showering. Due to Mr. Garcias spinal precautions, COPD,
and lymphocytic leukemia he has difficulty washing 10/10 body parts in the shower because he
fatigues easily and needs to remember his spinal precautions. The shower chair will support his
occupational performance by allowing him to safely and efficiently wash his entire body.
Precautions and Contraindications
Due to Mr. Garcias kyphoplasty he has to maintain three spinal precautions: no bending,
no lifting, and no twisting. The client should not lift anything heavier than five pounds. When
move his body he needs to move his head, shoulders, and knees together in a synchronized
movement. These precautions are in place to prevent injury to the back due to the surgical sites
limited range of motion. Contraindications include blood oxygen levels below 90 percent, this
should be monitored throughout treated due to the clients COPD and lymphocytic leukemia.
Frequency and Duration
The client will continue to participate in skilled OT services for 30 minutes twice daily
for 5 days a week over the next two weeks. All short term goals will be met within the first week
of treatment, and the long term goals will be met between one to two weeks.
Framework
OCCUPATIONAL PROFILE AND INTERVENTION
17
The Canadian Model of Occupational Performance (CMOP) is the primary framework
guiding this intervention plan because it keeps the clients interests as its focus. According to
Ikiugu (2012), the CMOP has spirituality at the core of the model, which is defined as anything
that motivates the person. Due to the state of Mr. Garcias pulmonary diseases in addition to his
rehab diagnosis, it important to keep in mind the clients spiritual and physical factors. The
intervention plan is guided not only by the clients rehab diagnosis, but also takes into account
the interrelationship among the client, their environment, and the affected occupations.
Client Training
Adaptive equipment and durable medical equipment is utilized in all four interventions
for Mr. Garcia. In order for the client to become successful in these intervention activities, which
promote achievement of short term goals the client must be provided with skilled instruction on
how to properly use the equipment involving demonstration and verbal cuing. In addition to
client training in use of adaptive equipment and durable medical equipment the client will be
trained in spinal precautions. The client will be provided training in how to maintain spinal
precautions throughout each intervention activity, which will encourage maintenance of spinal
precautions after being discharged home.
Response to Intervention
The clients response to the intervention will be assessed and monitored throughout each
therapy session by using the FIM. The FIM will help the therapist identify the clients level of
independence and provide a score for the clients occupational performance. The goal is to have
the client achieve a higher score as he progresses through treatment. Therapists can record each
OCCUPATIONAL PROFILE AND INTERVENTION
18
score and determine whether or not the client is increasing his level of independence and thus
responding well to the intervention plan.
References
American Occupational Therapy Association. (2014). Occupational therapy practice framework:
Domain and process (3rd ed.). American Journal of Occupational Therapy, 68(Suppl. 1),
S1-S48. http://dx.doi.org/10.5014/ajot.2014.682006
OCCUPATIONAL PROFILE AND INTERVENTION
19
Eschenfelder, V. (2005). Shaping the goal setting process in OT: The role of meaningful
occupation. Physical & Occupational Therapy In Geriatrics, 23(4), 67-81.
Ikiugu, M. (2012). Models of practice and frames of reference. In J. OBrien, S. Hussesy, & B.
Sabonis-Chafee (Eds.), Introduction to Occupational Therapy (p.137). St. Louis, MO:
Mosby Elsevier.
Stark, S. (2004). Removing environmental barriers in the homes of older adults with disabilities
improves occupational performance. OTJR: Occupation, Participation & Health, 24(1),
32-39
Toole, L. O., Connolly, D., & Smith, S. (2013). Impact of an occupation-based self-management
programme on chronic disease management. Australian Occupational Therapy Journal,
60(1), 30-38. doi:10.1111/1440-1630.12008
Wielandt, T., McKenna, K., Tooth, L., & Strong, J. (2001). Post discharge use of bathing
equipment prescribed by occupational therapists: What lessons to be learned?. Physical
& Occupational Therapy In Geriatrics, 19(3), 47-63.
Anda mungkin juga menyukai
- Kristen Kincaid Occupational Analysis & Intervention PlanDokumen23 halamanKristen Kincaid Occupational Analysis & Intervention Planapi-282525755100% (1)
- 630 Occupational Profile AssignmentDokumen13 halaman630 Occupational Profile Assignmentapi-201999002Belum ada peringkat
- 630 Submitted Occupational Profile and AnalysisDokumen21 halaman630 Submitted Occupational Profile and Analysisapi-310815315Belum ada peringkat
- Occt 651 - Occupational Profile and Intervention PlanDokumen22 halamanOcct 651 - Occupational Profile and Intervention Planapi-279916752Belum ada peringkat
- Occt630 Occupational Profile InterventionDokumen19 halamanOcct630 Occupational Profile Interventionapi-290880850Belum ada peringkat
- Dickson Occupational ProfileDokumen18 halamanDickson Occupational Profileapi-255001706Belum ada peringkat
- Occt 651 - Occupational Profile PaperDokumen20 halamanOcct 651 - Occupational Profile Paperapi-293243330Belum ada peringkat
- Occupational Profile and Intervention PlanDokumen13 halamanOccupational Profile and Intervention Planapi-251993533Belum ada peringkat
- Ashley M Occt 651 Occupational ProfileDokumen11 halamanAshley M Occt 651 Occupational Profileapi-25080062950% (2)
- Occupational Profile and Analysis Final EditedDokumen14 halamanOccupational Profile and Analysis Final Editedapi-233645719Belum ada peringkat
- Occupational Profile Intervention PlanDokumen17 halamanOccupational Profile Intervention Planapi-264481356Belum ada peringkat
- Running Head: Occupational Profile and Intervention Plan 1Dokumen19 halamanRunning Head: Occupational Profile and Intervention Plan 1api-292735638Belum ada peringkat
- Occupational Profile AnalysisDokumen20 halamanOccupational Profile Analysisapi-292815157Belum ada peringkat
- Occupational Profile and Intervention PlanDokumen18 halamanOccupational Profile and Intervention Planapi-282525755Belum ada peringkat
- Occupational Profile and Intervention Plan FinalDokumen21 halamanOccupational Profile and Intervention Plan Finalapi-293223028Belum ada peringkat
- 4th Sem 651 Occupational ProfileDokumen19 halaman4th Sem 651 Occupational Profileapi-291545292100% (1)
- Eval Soap Note 2Dokumen9 halamanEval Soap Note 2api-435763096Belum ada peringkat
- Occupational Profile FinalDokumen20 halamanOccupational Profile Finalapi-238703581100% (1)
- Occupational Analysis Intervention Plan PDFDokumen20 halamanOccupational Analysis Intervention Plan PDFapi-293182319Belum ada peringkat
- Soap NoteDokumen2 halamanSoap Noteapi-285542134Belum ada peringkat
- Dick, Elisa - Occupational ProfileDokumen10 halamanDick, Elisa - Occupational Profileapi-234536968Belum ada peringkat
- 11 17 Soap NoteDokumen4 halaman11 17 Soap Noteapi-435469413Belum ada peringkat
- Initial TemplateDokumen8 halamanInitial TemplateZuj PayBelum ada peringkat
- Soap Note 2 Community ClientDokumen12 halamanSoap Note 2 Community Clientapi-271984934Belum ada peringkat
- Occupational ProfileDokumen21 halamanOccupational Profileapi-293223028100% (1)
- New Intervention PlanDokumen17 halamanNew Intervention Planapi-282753416Belum ada peringkat
- Occupational Profile & Intervention PlanDokumen20 halamanOccupational Profile & Intervention Planapi-262531856Belum ada peringkat
- Clients Goals To Address in SessionDokumen8 halamanClients Goals To Address in Sessionapi-436429414Belum ada peringkat
- Occupational Profile Intervention PlanDokumen19 halamanOccupational Profile Intervention Planapi-263353704Belum ada peringkat
- Soap 11Dokumen4 halamanSoap 11api-436429414Belum ada peringkat
- Occupations Profile & Intervention PlanDokumen20 halamanOccupations Profile & Intervention Planapi-282223043Belum ada peringkat
- Occupational Profile & Intervention PlanDokumen19 halamanOccupational Profile & Intervention Planapi-262531856100% (1)
- Discontinuation NoteDokumen2 halamanDiscontinuation Noteapi-435763096Belum ada peringkat
- Instrumental Activities Daily Living: Try ThisDokumen11 halamanInstrumental Activities Daily Living: Try ThisbalryoBelum ada peringkat
- Occupational Profile Intervention PlanDokumen17 halamanOccupational Profile Intervention Planapi-264481356Belum ada peringkat
- Occupational Profile WeeblyDokumen34 halamanOccupational Profile Weeblyapi-293253519100% (1)
- Occupational Analysis Intervention PlanDokumen19 halamanOccupational Analysis Intervention Planapi-293223028Belum ada peringkat
- Occupational TherapyDokumen5 halamanOccupational TherapyZahra IffahBelum ada peringkat
- Fieldwork Case Study Treatment Plan AssignmentDokumen11 halamanFieldwork Case Study Treatment Plan Assignmentapi-398892840Belum ada peringkat
- CC StrokeDokumen13 halamanCC Strokeapi-436090845100% (1)
- AOTA Occupational Profile TemplateDokumen2 halamanAOTA Occupational Profile TemplateVIJAYA DHARSHINI M Bachelor in Occupational Therapy (BOT)Belum ada peringkat
- Artifact 5 Soap NoteDokumen3 halamanArtifact 5 Soap Noteapi-517998988Belum ada peringkat
- Davis Occupational Profile Intervention PlanDokumen19 halamanDavis Occupational Profile Intervention Planapi-292843843Belum ada peringkat
- Occupational Profile and Intervention Plan FinalDokumen21 halamanOccupational Profile and Intervention Plan Finalapi-263352281Belum ada peringkat
- World's Largest Science, Technology & Medicine Open Access Book PublisherDokumen17 halamanWorld's Largest Science, Technology & Medicine Open Access Book PublisherValeria Sousa de AndradeBelum ada peringkat
- 630 Occupational Profile and Intervention PlanDokumen22 halaman630 Occupational Profile and Intervention Planapi-282538590100% (1)
- Eval Soap NoteDokumen10 halamanEval Soap Noteapi-436577744Belum ada peringkat
- 2001 Candidate Handbook: National Board For Certification in Occupational Therapy, Inc. (Nbcot)Dokumen54 halaman2001 Candidate Handbook: National Board For Certification in Occupational Therapy, Inc. (Nbcot)engshi18Belum ada peringkat
- Social Worker or Caesmanager or Mental Health CounselorDokumen3 halamanSocial Worker or Caesmanager or Mental Health Counselorapi-77565760Belum ada peringkat
- Occupational Profile Intervention Plan-Danielle PalmerDokumen20 halamanOccupational Profile Intervention Plan-Danielle Palmerapi-292894327Belum ada peringkat
- Occt 630 - Occupational Profile and Intervention Plan - PortfolioDokumen21 halamanOcct 630 - Occupational Profile and Intervention Plan - Portfolioapi-279916752Belum ada peringkat
- Immuno Part CsDokumen15 halamanImmuno Part CsCecilia TesoreroBelum ada peringkat
- LOTCA Assessment ReviewDokumen10 halamanLOTCA Assessment ReviewManik MishraBelum ada peringkat
- Occupational Identity Disruption After Traumatic Brain Injury - An Approach To Occupational Therapy Evaluation and TreatmentDokumen13 halamanOccupational Identity Disruption After Traumatic Brain Injury - An Approach To Occupational Therapy Evaluation and Treatmentapi-234120429Belum ada peringkat
- Occt651 - Occupational Profile Paper - FinalDokumen20 halamanOcct651 - Occupational Profile Paper - Finalapi-293182319Belum ada peringkat
- Occupational Therapy Practice FrameworkDokumen31 halamanOccupational Therapy Practice FrameworkLian Michael0% (1)
- Occupational Therapy Discharge SummaryDokumen4 halamanOccupational Therapy Discharge Summaryapi-518285126Belum ada peringkat
- Community Client Discharge SummaryDokumen3 halamanCommunity Client Discharge Summaryapi-271980676Belum ada peringkat
- Running Head: Occupational Profile & Intervention Plan 1Dokumen18 halamanRunning Head: Occupational Profile & Intervention Plan 1api-238107777Belum ada peringkat
- Occupation Analysis in PracticeDari EverandOccupation Analysis in PracticeLynette MackenzieBelum ada peringkat
- Social JusticeDokumen2 halamanSocial Justiceapi-293258738Belum ada peringkat
- Leadership ReflectionDokumen1 halamanLeadership Reflectionapi-293258738Belum ada peringkat
- Your Brand Viveros MDokumen2 halamanYour Brand Viveros Mapi-293258738Belum ada peringkat
- Physiotherapy & Occupational Therapy Traumatic Brain Injury in The Intensive Care UnitDokumen6 halamanPhysiotherapy & Occupational Therapy Traumatic Brain Injury in The Intensive Care UnitHardeep Singh BaliBelum ada peringkat
- Evaluation 2Dokumen4 halamanEvaluation 2api-292843843Belum ada peringkat
- Occupation-Based ReflectionDokumen2 halamanOccupation-Based Reflectionapi-293258738Belum ada peringkat
- Occt645 - Home Evaluation Report Blacked OutDokumen7 halamanOcct645 - Home Evaluation Report Blacked Outapi-293182319Belum ada peringkat
- Early Mobility in Trauma IcuDokumen12 halamanEarly Mobility in Trauma Icuapi-293258738Belum ada peringkat
- Specific Diagnosis Reference SheetsDokumen12 halamanSpecific Diagnosis Reference Sheetsapi-293258738Belum ada peringkat
- Cotx Early Mobility AcuteDokumen7 halamanCotx Early Mobility Acuteapi-293258738Belum ada peringkat
- Mals Resume FinalDokumen1 halamanMals Resume Finalapi-293258738Belum ada peringkat
- Semester 5 Evidence Based FWDokumen3 halamanSemester 5 Evidence Based FWapi-293258738Belum ada peringkat
- Professional Development Plan MCVDokumen3 halamanProfessional Development Plan MCVapi-293258738Belum ada peringkat
- Occt 643 Cat PaperDokumen10 halamanOcct 643 Cat Paperapi-264481356Belum ada peringkat
- E ValueDokumen3 halamanE Valueapi-293258738Belum ada peringkat
- Occt 523 - Work Life Balance Final Paper - PortfolioDokumen14 halamanOcct 523 - Work Life Balance Final Paper - Portfolioapi-279916752Belum ada peringkat
- The Last Dropout PresentationDokumen36 halamanThe Last Dropout Presentationapi-293219537Belum ada peringkat
- Cat Evidence Table - FinalDokumen31 halamanCat Evidence Table - Finalapi-293258738Belum ada peringkat
- At Paper M ViverosDokumen10 halamanAt Paper M Viverosapi-293258738Belum ada peringkat
- Occupationalprofile M ViverosDokumen17 halamanOccupationalprofile M Viverosapi-293258738Belum ada peringkat
- PediatricsDokumen3 halamanPediatricsapi-291545292Belum ada peringkat
- Evidencesynthesis EmploymenttransitionDokumen14 halamanEvidencesynthesis Employmenttransitionapi-293258738Belum ada peringkat
- PediatricsDokumen3 halamanPediatricsapi-291545292Belum ada peringkat
- Running Head: Arthrogryposis A Case Study 1Dokumen21 halamanRunning Head: Arthrogryposis A Case Study 1api-291545292Belum ada peringkat
- PediatricsDokumen3 halamanPediatricsapi-291545292Belum ada peringkat
- Occupational Analysis Intervention Plan M ViverosDokumen17 halamanOccupational Analysis Intervention Plan M Viverosapi-293258738Belum ada peringkat
- Occt 504 - Group Research Paper - HomeaholicsDokumen8 halamanOcct 504 - Group Research Paper - Homeaholicsapi-293258738Belum ada peringkat
- 2008-Project Management of Unexpected EventsDokumen7 halaman2008-Project Management of Unexpected EventsJoey RossBelum ada peringkat
- (New Lacanian School) Psychoanalytical Notebooks (28) - The ChildDokumen146 halaman(New Lacanian School) Psychoanalytical Notebooks (28) - The ChildAndré Luiz Pacheco da Silva100% (1)
- Session 12 13Dokumen26 halamanSession 12 13KANIKA GORAYABelum ada peringkat
- SENG James T. Webb Scholarship Application: Family Information FormDokumen4 halamanSENG James T. Webb Scholarship Application: Family Information FormAnonymous gjKuCDOBelum ada peringkat
- British Airways Recruitment StrategyDokumen2 halamanBritish Airways Recruitment StrategyAbhishek Srivastava100% (1)
- Project Report: A Brief Study On Perception of Women Towards Himalaya Beauty Care ProductsDokumen40 halamanProject Report: A Brief Study On Perception of Women Towards Himalaya Beauty Care ProductsankitBelum ada peringkat
- EthicsDokumen6 halamanEthicsCess UrrizaBelum ada peringkat
- Educ 101 Module 1Dokumen12 halamanEduc 101 Module 1Kyle GomezBelum ada peringkat
- Psychosocial Care in Disasters ToT NIDMDokumen162 halamanPsychosocial Care in Disasters ToT NIDMVaishnavi JayakumarBelum ada peringkat
- ACKNOWLEDGEMENT NOTSUREajDokumen4 halamanACKNOWLEDGEMENT NOTSUREajMira Jin SardidoBelum ada peringkat
- Research Methods in Tourism: By. Kimberly Bunquin Mialyn CustodioDokumen20 halamanResearch Methods in Tourism: By. Kimberly Bunquin Mialyn CustodiorhyzeneBelum ada peringkat
- Contribution of East India Company Towards EducationDokumen20 halamanContribution of East India Company Towards EducationSunil Shekhar Nayak50% (2)
- Persuasive Speech OutlineDokumen3 halamanPersuasive Speech OutlineChristian Fernandez25% (4)
- Australian Digital ThesisDokumen194 halamanAustralian Digital ThesisGinger KalaivaniBelum ada peringkat
- RK 000613 Worksheet PDFDokumen2 halamanRK 000613 Worksheet PDFNhung KimBelum ada peringkat
- Teacher Transfer Schedule ProceedingsDokumen10 halamanTeacher Transfer Schedule Proceedingsnavn76100% (7)
- Krajewski Om12 02Dokumen69 halamanKrajewski Om12 02Keana Flowers100% (1)
- Stella SoftwareDokumen15 halamanStella SoftwareGee AgomBelum ada peringkat
- Brand Resonance ModelDokumen3 halamanBrand Resonance ModelNaimul KaderBelum ada peringkat
- TRAINING AND DEVELOPMENT SURVEYDokumen32 halamanTRAINING AND DEVELOPMENT SURVEYKhushboo KhannaBelum ada peringkat
- Cot 1 DLLDokumen3 halamanCot 1 DLLY Sa So RiBelum ada peringkat
- Potrayal of Women in CinemaDokumen97 halamanPotrayal of Women in CinemaMitali Srivastava BhatnagarBelum ada peringkat
- Ispo Self-Study DocumentDokumen24 halamanIspo Self-Study DocumentFatima SanchezBelum ada peringkat
- Zumba Dance RubricsDokumen1 halamanZumba Dance RubricsJuliane Rebecca PitlongayBelum ada peringkat
- MIDTERM EXAM (Professional Development and Apllied Ethics Answer Key)Dokumen2 halamanMIDTERM EXAM (Professional Development and Apllied Ethics Answer Key)Daniel BeloncioBelum ada peringkat
- GL Bajaj FormateDokumen5 halamanGL Bajaj FormateFARMANBelum ada peringkat
- English DLL Week 1 Qrtr.4 AvonDokumen7 halamanEnglish DLL Week 1 Qrtr.4 Avonlowel borjaBelum ada peringkat
- Full Download Consumer Behavior 12th Edition Schiffman Solutions ManualDokumen35 halamanFull Download Consumer Behavior 12th Edition Schiffman Solutions Manualbaytermilucak97% (37)
- Resume FinalDokumen3 halamanResume Finalapi-399694454Belum ada peringkat
- Organizational DevelopmentDokumen29 halamanOrganizational DevelopmentvaijayanthiBelum ada peringkat