Colaboration Medical
Diunggah oleh
dobutakuHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Colaboration Medical
Diunggah oleh
dobutakuHak Cipta:
Format Tersedia
Collaboration Between the Anesthesia and Surgical Teams
In the Perioperative Setting
Merck Consultants
Roy G. Soto, MD
r
ll
Professor
Oakland University William Beaumont School of Medicine
Residency Program Director
Department of Anesthesiology
Royal Oak, Michigan
Co
ts
Associate Professor and Chief
Division of Colorectal Surgery
Drexel University College of Medicine
Philadelphia, Pennsylvania
Medical Writer
Oren Traub, MD, PhD
This article was written with significant input,
direction, and editorial review by Merck.
Introduction
ANESTHESIOLOGY NEWS AUGUST 2013
Perspectives of the Anesthesia Provider
And the Surgeon
A recent survey conducted with surgeons, anesthesiologists, and certified registered nurse anesthetists (CRNAs)
from one institution suggests that the level and quality of
communication often is perceived differently by team members.2 Awad et al used a validated Likert-scale survey with
questions aimed at communication in the operating room
(OR) to establish the baseline of communication among surgeons, anesthesiologists, and CRNAs prior to participating in
Table 1. Definitions of Types of Communication Failure With Illustrative Examples and Notes
Occasion Failures
Definition
Illustrative Example and Analytical Note (In Italics)
Content failures
Problems in the situation The staff surgeon asks the anesthesiologist whether the antibiotics
or context of the comhave been administered. At the point of this question, the procedure
munication event
has been under way for >1 h.
As antibiotics are optimally given within 30 min of incision, the timing
of this inquiry is ineffective both as a prompt and as a safety redundancy
measure.
Audience failures
Insufficiency or inaccuracy apparent in the
information being
transferred
As the case is set up, the anesthesia fellow asks the staff surgeon
if the patient has an ICU bed. The staff surgeon replies that the bed
is probably not needed, and there isnt likely one available anyway,
so well just go ahead.
Relevant information is missing and questions are left unresolved:
Has an ICU bed been requested, and what will be the plan if the patient
does need critical care and an ICU bed is not available? [Note: classified
as a content and purpose failure.]
Purpose failures
Gaps in the composition The nurses and the anesthesiologist discuss how the patient should
of the group engaged in be positioned for surgery without the participation of a surgical
the communication
representative.
Surgeons have particular positioning needs so they should be participants in this discussion. Decisions made in their absence occasionally
lead to renewed discussions and repositioning upon their arrival.
Failure
Communication events
in which the purpose is
unclear, not achieved,
or inappropriate
.
ed
Active coordination by different members of the health
care team (eg, surgeons, anesthesiologists, and nurse anesthetists) is important during the perioperative period; investigational and anecdotal observations suggest that poor
communication among anesthesia professionals, surgeons,
and other surgical staff may exist during this period.
Lingard et al observed 48 selected surgical procedures
at a Canadian hospital center over 3 months in 2003 in
order to describe the content and effects of communication
events as well as identify common communication failures.1
The authors identified 421 communication eventsdefined
as a verbal or non-verbal exchange between 2 or more surgical team membersand categorized 129 of these events
as communication failures in that content of the communication was directed at the wrong team member, had the
incorrect goal or intent for the current situation, or was miscommunicated or not communicated due to the physical or
temporal situation at the time (eg, a request was inaudible
because of an alarm) (Table 1).1
In separate interviews conducted for this article, David E.
Stein, MD, associate professor and chief of the Division of
Colorectal Surgery at Drexel University College of Medicine
in Philadelphia, Pennsylvania, and Roy G. Soto, MD, professor of anesthesiology and director of the residency program
at Oakland University William Beaumont School of Medicine
in Royal Oak, Michigan, discussed their experience regarding
communication among the health care team. In my experience, one of the things that gets pushed aside during the
perioperative period is communication, said Dr. Stein, who
has practiced since 2003. Its important to take a step back
and communicate with your team members.
In the aforementioned study by Lingard et al, incidents
of communication failure (30.6% of the 421 total number
of events) were divided into several categories: poor timing
(45.7%), missing or inaccurate information communicated
10
medical team training. A study objective was to determine
if OR communication could be improved through training.2
The study found that anesthesiologists perceived overall
communication to be poor; nurses viewed communication
as adequate; and surgeons found communication among
OR staff was good. The study found that medical team training could improve communication in the OR.2
Similarly, Sexton et al sought to survey operating theatre and intensive care unit staff about attitudes concerning stress, error, and teamwork.3 Using 4 questionnaires that
contained a core set of questions whose responses could
match across disciplines and countries, researchers evaluated responses from 1,033 doctors, residents, fellows, and
nurses from 12 urban hospitals in Italy, Germany, Switzerland, Israel, and the United States.3 Results showed that
62% of surgical staff reported high levels of teamwork with
anesthesia staff. Among anesthesia staff, 41% (106 out of 250)
reported high levels of teamwork with surgical staff.3 Also,
less than 30% of anesthesia residents, anesthesia nurses,
and surgical nurses (10%, 26%, and 28%, respectively), and
it
d.
ib
te oh
no pr
e
is n is
rw io
he iss
ot rm
e
ss
le
tp
un ou
up ith
ro t w
G
r
pa
ng
hi
in
is
or
bl
Pu ole
on wh
ah in
cM n
M
tio
13 duc
20
o
epr
ht . R
rig ed
py
rv
se
re
h
ig
David E. Stein, MD
(35.7%), unresolved issues (24%), and communication events
when key individuals were excluded (20.9%).1 Dr. Soto, who
has practiced for more than 10 years, noted that the size of
certain medical centers may contribute to communication
problems. At my center alone, there are 87 different locations where anesthesia might be administered, Dr. Soto said.
That means that youre working with people every day who
youve never met before and havent yet established a common language for good communication.
During a living donor liver resection, the nurses discuss whether ice
is needed in the basin they are preparing for the liver. Neither knows.
No further discussion ensues.
The purpose of this communicationto find out if ice is requiredis not
achieved. No plan to achieve it is articulated.
Reprinted with permission from Lingard L, Espin S, Whyte S, et al. Communication failures in the operating room: an observational classification of
recurrent types and effects. Qual Saf Health Care. 2004;13(5):330-334.
Article paid for
and sponsored by
39% of anesthesia consultants reported high levels of teamwork with consultant surgeons overall.3
In another study, 16 Canadian clinicians (11 anesthesiologists and 5 surgeons) were interviewed in order for researchers to identify beliefs about preoperative testing practices.4
The content of the physicians statements was analyzed and
separated into relevant conceptual domains. Results found
that surgeons and anesthesiologists differed as to who was
responsible for ordering tests and how many and which tests
should be ordered.4 Also, results showed that surgeons may
order tests based on what they perceive relevant for the anesthesiologist, as opposed to directly communicating with the
anesthesiologist about which tests would be most relevant.4
This problem can be compounded by the absence of a
formalized communications system or an integrated electronic medical records system across different groups.
If I see the patient in my clinic and ordered all the preoperative tests, the results may be sitting on my desk. I have
to remember to transmit those results to the anesthesiologist so that they are available when that practitioner evaluates the patient, Dr. Stein said. Having those results might
prompt the anesthesiologist to order other tests that I didnt
even consider. It doesnt do any good if were not sharing the
information we know.
r
ll
Co
Table 2. Preoperative Briefing Guide
Category
Components
Time out
Patient name
Procedure
Site verification
Laterality
ts
it
d.
ib
te oh
no pr
e
is n is
rw io
he iss
ot rm
e
ss
le
tp
un ou
up ith
ro t w
G
r
pa
ng
hi
in
is
or
bl
Pu ole
on wh
ah in
cM n
M
tio
13 duc
20
o
epr
ht . R
rig ed
py
rv
se
re
h
ig
Physicians also have indicated that documentation and/
or notes derived from a template sometimes can provide
further aid in assuring that all the vital information has
been obtained and documented.6,7 Finally, several groups
of investigators have studied the effect of formalized processes that incorporate these system improvements.
For example, Awad et al instituted a dedicated training
session (eg, didactic instruction, interactive participation,
role-play sessions, training films, and clinical vignettes) for
the entire surgical service using crew resource management principles and principles of change management.
Additionally, researchers established formal preoperative
briefings (Table 2) conducted among the surgeon, the
anesthesiologist, and the surgical nurse.2 Four months after
conducting the training session and initiation of the preoperative briefing protocol, investigators found briefings
occurred preoperatively for all patients, and there was a
significant increase in the perceived communication score
among anesthesiologists and surgeons (score increase
among OR nursing staff was not statistically significant).2
Lingard et al performed a 13-month prospective study
of a short team briefing structured by a checklist in order
to assess whether these briefings could improve OR communication. Participants included 11 general surgeons,
24 surgical trainees, 41 OR nurses, 28 anesthesiologists, and
24 anesthesia trainees from a Canadian academic tertiary care
hospital.8 The primary outcome measure was the total number of communication failures per surgical procedure. During
the structured briefings, led by the surgeon, team members
were to share their knowledge of the case and resolve knowledge gaps as to how the procedure would proceed.8 Study
researchers reported that the mean number of communication failures per procedure declined from 3.95 before the
briefing intervention was introduced to 1.31 failures per procedure following the intervention period (P<0.001).8
Improving Communication in the
Perioperative Setting
Conclusion
Overall, Dr. Stein noted that the success of these types
of interventions begins with the staff members themselves.
Everybody has to check their egos at the door. The days of
having a central person saying I know best and you should
do what I say are well past, he said. Its best to have a team
that is communicating well with one another.
References
1. Lingard L, Espin S, Whyte S, et al. Communication failures in the operating room: an observational classification of recurrent types and effects.
Qual Saf Health Care. 2004;13(5):330-334.
2. Awad SS, Fagan SP, Bellows C, et al. Bridging the communication gap in
the operating room with medical team training. Am J Surg. 2005;190(5):
770-774.
3. Sexton JB, Thomas EJ, Helmreich RL. Error, stress, and teamwork in medicine and aviation: cross sectional surveys. BMJ. 2000;320(7237):745-749.
4. Patey AM, Islam R, Francis JJ, et al. Anesthesiologists and surgeons
perceptions about routine pre-operative testing in low-risk patients:
Staff surgeon
Anesthesiologist
Nurse
Anticipated problems
Documentation
Consent
History and physical within 30 d
Staff preoperative note
Case discussion
Anesthesia plans/concerns
Allergies
IV antibiotics
Position
Sequential compression device
Required instrumentation
Special equipment
Blood
Length of procedure
Postoperative disposition
Precautions
Consensus on plan and site
Reprinted with permission from Awad SS, Fagan SP, Bellows C,
et al. Bridging the communication gap in the operating room
with medical team training. Am J Surg. 2005;190(5):770-774.
application of the Theoretical Domains Framework (TDF) to identify
factors that influence physicians decisions to order pre-operative tests.
Implement Sci. 2012;7:52.
5. Rivers RM, Swain D, Nixon WR. Using aviation safety measures to
enhance patient outcomes. AORN J. 2003;77(1):158-162.
6. Lubarsky D, Candiotti K. Giving anesthesiologists what they want:
how to write a useful preoperative consult. Cleve Clin J Med. 2009;
76(suppl 4):S32-S36.
7. Bader AM, Sweitzer B, Kumar A. Nuts and bolts of preoperative
clinics: the view from three institutions. Cleve Clin J Med. 2009;
76(suppl 4):S104-S111.
8. Lingard L, Regehr G, Orser B, et al. Evaluation of a preoperative checklist and team briefing among surgeons, nurses, and anesthesiologists to
reduce failures in communication. Arch Surg. 2008;143(1):12-17;
discussion 18.
Disclosures
.
ed
In an effort to improve the level and quality of communication, one model often employed by experts is crew resource
management or the use of aviation techniques. Principles of
this strategy as applied to the perioperative setting include
using a preoperative briefing with all surgical staff. In the past
10 years, following the adoption of crew resource management techniques, the aviation industry has experienced a
marked decrease in communication-related mistakes.5
Dr. Soto explained that the recent integration of aviation
crew resource management techniques into surgical workflow at his institution is helping communication: In addition
to empowering each member of the surgical and anesthesia
staff to speak up when they see something during the case,
these aviation management techniques also involve immediate review of cases. This enables us to evaluate the case
and use that knowledge for our future cases, he said.
More and more centers are using a formalized preoperative huddle where they explicitly discuss the case, the
positioning, and the procedural details and time, Dr. Stein
said. Knowledge is power: Having this information can help
both surgeons and anesthesiologists navigate their intraoperative approach to the patient. Dr. Soto also described the
usefulness of preoperative meetings. The anesthesiologist
may want to obtain more information to prepare an appropriate anesthetic management plan, he said. Theres where
the preoperative huddle may help.
Roll call
Both Drs. Soto and Stein were paid by Merck for their contributions to this article. Dr. Soto reported receiving grant/
research support from Merck. Dr. Stein reported receiving
speaker fees from Cubist, Ethicon Endo-Surgery, and Merck.
BB1322
Disclaimer: This monograph is designed to be a summary of information. While it is detailed, it is not an exhaustive clinical review. McMahon Publishing, Merck, and the authors neither affirm nor deny the accuracy of the
information contained herein. No liability will be assumed for the use of this monograph, and the absence of typographical errors is not guaranteed. Readers are strongly urged to consult any relevant primary literature.
Copyright 2013, McMahon Publishing, 545 West 45th Street, New York, NY 10036. Printed in the USA. All rights reserved, including the right of reproduction, in whole or in part, in any form.
ANES-1081276-0001 06/13
ANESTHESIOLOGY NEWS AUGUST 2013
11
Anda mungkin juga menyukai
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- NURS FPX 6030 Assessment 6 Final Project SubmissionDokumen11 halamanNURS FPX 6030 Assessment 6 Final Project Submissionzadem5266Belum ada peringkat
- Building Occupational Safety and Health k3 Analysis of The Work Environment and Work DisciplineDokumen10 halamanBuilding Occupational Safety and Health k3 Analysis of The Work Environment and Work Disciplineipraul167Belum ada peringkat
- Colorado Department of Public Health and Environment: November 14 Public-Health Order UpdateDokumen9 halamanColorado Department of Public Health and Environment: November 14 Public-Health Order UpdateMichael_Roberts2019Belum ada peringkat
- Gap AnalysisDokumen9 halamanGap Analysisapi-706947027Belum ada peringkat
- Becky Ortiz ResumeDokumen1 halamanBecky Ortiz ResumeBecky OrtizBelum ada peringkat
- Key To Reading 3Dokumen2 halamanKey To Reading 3Thùy TrangBelum ada peringkat
- Histologia, Conceitos Básicos Dos Tecidos - GitiranaDokumen13 halamanHistologia, Conceitos Básicos Dos Tecidos - GitiranaJhonnatam EliasBelum ada peringkat
- Englishmelon Oet Writing Test 2Dokumen2 halamanEnglishmelon Oet Writing Test 2Cam Achondo56% (27)
- Form2a 1Dokumen2 halamanForm2a 1ghi YoBelum ada peringkat
- Food Systems For ChildrenDokumen12 halamanFood Systems For ChildrenPaulin koffiBelum ada peringkat
- Core CompetencyDokumen9 halamanCore CompetencyCharm BarinosBelum ada peringkat
- PARCO Project HSE Closing ReportDokumen22 halamanPARCO Project HSE Closing ReportHabib UllahBelum ada peringkat
- Survey QuestionnaireDokumen2 halamanSurvey Questionnairecyrusbatayan100% (1)
- An Electromyographical Analysis of Sumo and Conventional Style DeadliftsDokumen8 halamanAn Electromyographical Analysis of Sumo and Conventional Style DeadliftsRafael EscamillaBelum ada peringkat
- Break The Cycle Activity GuidesDokumen19 halamanBreak The Cycle Activity GuidesJuanmiguel Ocampo Dion SchpBelum ada peringkat
- Vape Waste Report PAE C3Dokumen14 halamanVape Waste Report PAE C3LVNewsdotcomBelum ada peringkat
- Ponr 1Dokumen14 halamanPonr 1Jhade RelletaBelum ada peringkat
- Congestive Cardiac FailureDokumen22 halamanCongestive Cardiac FailureSampada GajbhiyeBelum ada peringkat
- Tetanus - AnatomyDokumen7 halamanTetanus - AnatomyJoro27Belum ada peringkat
- SHARON SCHULTZ, ET AL. v. JANOS GUOTH, M.D. AND KHALED F. RABIE, M.D. (Parish of Rapides)Dokumen18 halamanSHARON SCHULTZ, ET AL. v. JANOS GUOTH, M.D. AND KHALED F. RABIE, M.D. (Parish of Rapides)wstBelum ada peringkat
- Septic System Design ManualDokumen31 halamanSeptic System Design ManualtonyBelum ada peringkat
- Outbreak of S. Weltevreden Linked To Fermented Cashew Nut Cheese in Victoria, BCDokumen8 halamanOutbreak of S. Weltevreden Linked To Fermented Cashew Nut Cheese in Victoria, BCLeila RochaBelum ada peringkat
- 01 EnemaDokumen4 halaman01 Enemabunso padillaBelum ada peringkat
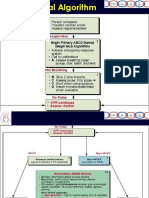
- VF-VT AlgorithmDokumen10 halamanVF-VT AlgorithmPuskesmas Pinang JayaBelum ada peringkat
- 2022 SWMS - Combined SWMSDokumen8 halaman2022 SWMS - Combined SWMSSteveBelum ada peringkat
- Management Control in Nonprofit Organizations, Fourth EditionDokumen74 halamanManagement Control in Nonprofit Organizations, Fourth EditionSUHAIRI19084488100% (1)
- Ellness F T I O: Rom He Nside UtDokumen5 halamanEllness F T I O: Rom He Nside UthbgossBelum ada peringkat
- Local Government Financial Statistics England #23-2013Dokumen222 halamanLocal Government Financial Statistics England #23-2013Xavier Endeudado Ariztía FischerBelum ada peringkat
- Enhancing Communication To Improve Patient Safety.5Dokumen6 halamanEnhancing Communication To Improve Patient Safety.5Ang Timotius Raymond AngkajayaBelum ada peringkat
- APDSA SRC Submitssion FormDokumen2 halamanAPDSA SRC Submitssion FormDevi 吴姗姗 GunawanBelum ada peringkat