Nurs440leadershipstrategyanalysis Timeoutprocedure
Diunggah oleh
api-240028260Deskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Nurs440leadershipstrategyanalysis Timeoutprocedure
Diunggah oleh
api-240028260Hak Cipta:
Format Tersedia
Running head: 'TIME OUT' UNIVERSAL PROTOCOL
'Time Out' Universal Protocol: Essential in Prevention of Wrong-site Surgeries
Catherine Buckel, Cherie McKay-Horst, Lindsay Vasquez, Michelle Wronski
Ferris State University
'TIME OUT' UNIVERSAL PROTOCOL
'Time Out' Universal Protocol: Essential in Prevention of Wrong-site Surgeries
The goal of an organization committed to quality care is a comprehensive systematic
approach that prevents errors or identifies and corrects errors so that adverse events are
decreased and safety and quality outcomes are maximized (Yoder-Wise, 2015, p. 362). The
success of these quality improvement (QI) and safety initiatives depend greatly on the culture
and paradigm of the healthcare institution, one in which, values a continuous process of
improvement that affect positive patient outcomes (Yoder-Wise, 2015, p. 362). In practice, the
(QI) process is performed through a systematized progression of steps, designed to plan,
implement, and evaluate changes in healthcare activities (Yoder-Wise, 2015, p. 367).
Without a doubt, it is imperative that nurse leaders in healthcare, ... be excellent change
managers and this means, facilitating changes needed at a system, unit, or team level
(Yoder-Wise, 2015, p. 306). In the case of the quality improvement process, nurse leaders can
affect a change in clinical practice and via evidenced-based guidelines these (QI) endeavors can
be met. Subsequently, as a result, registered nurses (RNs), have a direct impact on patient
safety and healthcare outcomes (Yoder-Wise, 2015, p. 364). The process begins with the
designation of a clinical activity within the healthcare institution that is in need of review for
improvement. Of course, it is imperative that when a QI project is established, efforts should
be concentrated on changes to patient care that will have the greatest effect (Yoder-Wise, 2015,
p. 368). Finally, Yoder-Wise (2015) affirms that, QI involves continual analysis and evaluation
of product and services to prevent errors and to achieve customer satisfaction (Yoder-Wise,
2015, p. 367).
'TIME OUT' UNIVERSAL PROTOCOL
Identify Clinical Need
In an attempt to prevent devastating medical errors during the surgical process, in 2004,
The Joint Commission (TJC) established the Universal Protocol to reduce wrong site, wrong
procedure, and wrong person surgeries (Mainthia et al., 2011, p. 660). The three step QI
protocol requires healthcare institutions to perform a pre-procedure verification process, marking
of correct surgical site, and then, conduct a timeout discussion as a final check before the
procedure begins (OReilly, 2010). Although mandatory rules were put into place to prevent
wrong site surgical errors from ensuing, Officials estimate that wrong-site surgery alone occurs
40 times a week in U.S. hospitals and clinics (Mainthia et al., 2011, p. 660).
For this reason, the objective of this quality improvement QI and safety initiative analysis
is to evaluate the compliance and effectiveness of the Surgical Time Out STO through the
quality improvement process. Analyzing the STO involves several key concerns and common
problem areas. First, one of three areas of concern with the success of STO is communication.
Effective communication among healthcare workers is imperative and there is no other more
vital area for clear, concise and accurate communication than in the operating room,
especially at the start of a surgical procedure, to identify patient care concerns and to clear up
and questions team members may have (Morell Edel, 2010, p. 420). Obviously, the
consequence of poor communication results in the potentiality of valuable patient information
being lost or inadvertently not passed on, which is than conducive to medical errors.
The second area of concern regarding the efficacy of STO is the willingness of the
surgical team in complying with the existing time out procedure (Mainthia et al., 2011).
Communication and compliance, .are arguably 2 of the most important components in
decreasing preventable surgical errors (Mainthia et al., 2011, p. 661). Ultimately, after analyzing
'TIME OUT' UNIVERSAL PROTOCOL
the data with respect to wrong procedure cases, the research revealed that compliance with
protocols was the number one reason that they occur (OReilly, 2010).
The third common problem related to the Universal Protocol is that the information is
either missing or often recorded in multiple areas such as, intraoperative record, anesthesia
notes, patient chart instrument count sheets, and sometime even on handwritten notes made by
the circulating nurse on various pieces of paper (Morell Edel, 2010, p. 421). Further, The
patient may also be at risk for medical errors when time out information is gathered before
surgery by individual practitioners who do not formally confer with each other to communicate
the information or to confirm its reliability (Morell Edel, 2010, p. 421). Unquestionably, the
assumption by the medical team that all the patient information is not only valid as well as
documented and present in the chart may not be correct, leading to possible medical errors
(Morell Edel, 2010). Because adverse events in surgical patients have been assessed to be
exceedingly preventable, a QI initiative to review and improve upon the current surgical
Universal Protocol practice is advantageous for healthcare institutions and patient outcomes
(Haugen, Murugesh, Haaverstad, Eide, & Softeland, 2013).
Interdisciplinary Team
There are numerous moving parts in a surgical care team and each member shares the
responsibility of performing a necessary time out before a procedure occurs. The biggest
stakeholder in this quality initiative is the surgeon or physician performing the operation or
procedure; the ultimate liability and burden of wrong-site surgery falls on his or her shoulders. In
addition to a terribly detrimental, often life changing, mistake, a wrong-site surgery, might
result in a settlement or award on verdict in the six to seven figure range in 2005 US dollars
'TIME OUT' UNIVERSAL PROTOCOL
(Clarke, Johnston, & Finley, 2007, p. 395). In addition, physicians can irrevocably ruin their
reputation as a trusted and competent surgeon.
Wrong-site surgery is perceived as a medical error that should never happen, not a
medical risk that the patient must accept, and therefore a core patient safety problem. The
National Quality Forum (NQF) includes wrong-site surgery events on its list of Serious
Reportable Events, commonly referred to as never events.(Clarke et al., 2007, p. 395)
The physician has an ethical obligation to abide by the principles of beneficence and
Nonmaleficence for their patient and does so by following the universal protocol enacted by the
Joint Commission on time out procedures. As Yoder-Wise (2015) defines, never events are,
errors in medical care that are clearly identifiable, preventable, and serious in their consequences
for patients and that indicate a real problem in the safety and credibility of a healthcare facility
(p. 377). Surgeons are the very last line of defense before an incision is made, and if a mistake is
clearly preventable, the importance of adhering to the time out protocol must be realized.
Following closely behind a surgeon, the registered operating room nurse is vital in this
quality initiative. As a healthcare professional and license holder, he or she holds accountability
to adhering to this protocol as well. The nurse has a large amount of contact and communication
with the patient before and during the procedure and has numerous opportunities to verify the
correct operation is occurring. The nurses doing reconciliation and verification in the
preoperative holding area were consistently effective in catching errors before they reached the
patient (Clarke et al., 2007, p. 398)
However, as Dillon (2008) points out, the potential does not stop there:
As the patients advocate, the RN should take the initiative to call a time out to guarantee
'TIME OUT' UNIVERSAL PROTOCOL
6
the correct patient; procedure; site (e.g. organ, limb, vertebral level, laterality); surgeon;
and position, as well as proper instrumentation, implants, and equipment for the
scheduled procedure. (p. 438)
In many facilities, the nurse initiates the start of the protocol and keeps the surgical team on track
with compliance. They force a pause in the chaos and allow a moment for every member of the
interdisciplinary team to review pertinent history or radiographs, for example. Examining even
further, the nurse is paramount in the proper documentation and recording of compliance and, in
so doing, protects the practice of all members of the healthcare team. Patient safety is the
responsibility of the entire surgical care team, but as the patients advocate, the RN should take
the lead in the OR (Dillon, 2008, p. 442).
Radiologists carry the responsibility of accurately interpreting and dictating images to
provide the surgical team with appropriate direction; therefore, their involvement in this quality
initiative is essential. A mistake in dictation could mean surgery on the wrong extremity or
incorrect region of the body.
Finally, anesthesiologists provide direct care to the patient during surgical procedures and
have an equal responsibility in time out procedures. In fact, their documentation requires
acknowledgement of a time out and they control, by means of anesthesia, when the operation
will begin. The final opportunity in which the patients can still advocate for themselves and
correct a misunderstanding is right before anesthesia is administered. Hence, in reference to case
studies on anesthesias impact in the operating room, In all but one, the anesthetic interventions
at the wrong site were corrected and did not result in completed wrong-site surgery (Clarke et
al., 2007, p. 398).
Data Collection Method
'TIME OUT' UNIVERSAL PROTOCOL
7
In any quality improvement process it is necessary to establish a baseline upon which to
improve. For the time out protocol this will be accomplished by researching the current
percentage of incorrect surgeries occurring within the organization. These statistics will be
determined by an extensive investigation into any incident reports involving wrong-site
surgeries; these figures will be recorded for future comparison. Next, the team will collect data
on the current compliance to the time out protocol already in place. The main avenue to
accomplish this task would be through chart auditing and examination for proper documentation.
To ensure consistency, researchers will follow a formatted flowchart that displays the correct
universal protocol tasks. In this case, The flowchart is a data tool that uses boxes and directional
arrows to diagram all the steps of a process or procedure in the proper sequence (Yoder-Wise,
2015, p. 369). This will allow the interdisciplinary team a display of the correct sequence of
events and a quick way to determine where the breakdown in procedure is occurring. For
example, at Childrens Hospital Boston after a thorough review, It immediately became clear
that it was necessary to improve overall compliance and educate surgeons and nurses on correct
site marking protocol (Norton, 2007, p. 1187). They noticed that the surgical site marking
preoperatively was inadequate (illegible writing and questionable marking) or was altogether
omitted. One area of focus in data collection will be on high risk situations where, for example,
surgery is emergent of rushed. These cases will be systematically broken down in order to
determine where in the protocol they faltered and how best to approach these unique
circumstances. Once all this information is obtained, a list of failings will then be compiled and
brought back to the team for brainstorming on ways to remediate these issues. By determining
areas for improvement, it is then possible to establish the desired outcomes of the quality
improvement initiative.
'TIME OUT' UNIVERSAL PROTOCOL
Established Outcomes
The established goal or outcome is to have 100 percent compliance with the surgical
time-out procedure for every surgery to prevent the wrong surgery from taking place. Wrong
surgery can be classified into three groups: surgery at the wrong site, surgery on the wrong
patient and carrying out the wrong procedure (VanSchoten, Kop, & Block, 2014). The time-out
procedure should take place just before anesthesia and involves, a review of the names and
roles of all team members, characteristics of the patient, the operation plan, familiarity with the
procedure, the presence of the correct materials/equipment and potential issues for the patient
(VanSchoten et al., 2014). After implementation, a chart audit will reveal compliance with the
Universal Protocol and it will be properly documented.
Implementation Strategies
The strategy that will be used to implement change is Kotters eight-step model. The
eight steps are the following: Create urgency, form a powerful coalition, create a vision for
change, communicate the change vision, remove obstacles, create short-term wins, build on the
change, and anchor the changes in the culture (Yoder-Wise, 2015, p. 315). Urgency can be
created by providing documented cases of errors that have occurred when a surgical or
procedural time out have not been properly conducted. Staff will feel a pressing need to change
when the facts about medical errors are presented to them. A small committee of nurses that will
advocate for change will help gain support from other staff members. They will also keep the
vision of change focused on the main goal of preventing medical errors. The committee of nurses
will communicate with other staff on a regular basis, keeping the team focused and reinforcing
'TIME OUT' UNIVERSAL PROTOCOL
the need for the time out prior to any surgery or procedure. Staff should stay alert for any
barriers that may inhibit the process and ability to change. These obstacles should be removed
when noted. Short-term goals should be celebrated when accomplished to maintain a successful
environment. As staff observes success, this culture of improvement and change will become the
norm. The final step of Kotters eight-step model involves recognizing when changes are
effective and making a point of acknowledging those who have helped the process, this behavior
will help anchor the changes (Yoder-Wise, P., 2015).
A few examples of changes that when implemented will help staff meet the goal of 100%
compliance with surgical time-out procedures are: placing a steel plate inside every CPD tray
that the surgical team uses so it is immediately visible and will act as a reminder to the OR staff
to complete a surgical time-out, re-education and continued education for staff that reemphasizes
the importance of the time-out protocol. This can done by holding mandatory in-service
education meetings for all surgical staff, including surgeons, anesthesiologists, and radiologists.
Perform weekly live-audits in which time-out protocols are directly witnessed, develop and
follow a no-tolerance policy for improper/neglected surgical site marking. Also, bi-weekly chart
reviews to audit findings with pertinent staff members.
Evaluation
The interdisciplinary team will be doing a Learned Evaluation approach for compliance
of TJC protocol for reduction in errors in the operating room. A Learned Evaluation approach is
an assessment that is flexible grounded, interactive, contextualized, and participatory
(Balasubramaina et al., 2015, p. 2). This way all disciplines are engaged in the quality
improvement process. A root cause analysis of the Operating room will be conducted to identify
specific area for the facility to focus on. Once that is completed the facility will then, perform a
'TIME OUT' UNIVERSAL PROTOCOL
Plan-Do-Study Act (Balasubramaina et al., 2015, p. 2). A Plan-Do-Study Act (PDSA) is a
10
systemic approach to collecting data, study the root cause and create a specific plan on how to
make the changes. This will give focus to the facility to allow for measurable outcomes to the
(PDSA). On a quarterly basis the facility will review the data collected that is qualitative and
quantitative on which to measure their success. Finally, using qualitative data assists with the
specific needs of each facility while quantitative data help to set future goals for each quarterly
review.
Conclusion
The success of the QI will be determined by how committed the facility as well as each
member of the interdisciplinary team. The Time Out process is crucial to patient safety,
especially at the beginning of a surgical procedure. Communication in the operating room will
ensure the correct site, correct procedure and correct patient. The protocols established by the
TJC are a guideline for operating room safety and should be followed at all times. There need to
be a quality assurance program (QA) in place. The QA program will ensure conformity to a
standard (Yoder-Wise, 2015, p. 375). Conformity to the standard the TJC set out for all
practitioners to follow is not a choice but a responsibility. All practitioners take an oath, to do
no harm; by not following the established standards it puts the patient in harms way. Despite
the estimated 40 annual STO errors currently made, it can be avoidable with the watchful eye of
each person in the operating room (Mainthia et al., 2011, p. 660).
'TIME OUT' UNIVERSAL PROTOCOL
11
References
Balasubramaina, B. A., Cohen, D. J., Davis, M. M., Gunn, R., Dickinson, L. M., Miller, W. L.,
Stange, K. C. (2015). Learning Evaluation: blending quality improvement and
implementation research methods to study healthcare innovations. Implementation
Science, 10(31). http://dx.doi.org/10.1186/s13012-015-0219-z
Clarke, J.R., Johnston, J., & Finley, E.D. (2007). Getting Surgery Right. Annals of Surgery,
246(3), 395-405.
Dillon, K.A. (2008). Time Out: An Analysis. Association of periOperative Registered Nurses
Journal, 88(3), 437-442.
Haugen, A. S., Murugesh, S., Haaverstad, R., Eide, G. E., & Softeland, E. (2013). A Survey of
surgical team members. A survey of surgical team members perceptions on near misses
and attitudes towards Time Out protocols, 13(46), 1-7. http://dx.doi.org/10.1186/14712482-13-46
Norton, E. (2007). Implementing the Universal Protocol Hospital-Wide. Association of
periOperative Registered Nurses Journal, 85(6), 1187-1197.
Mainthia, R., Lockney, T., Zotov, A., France, D. J., Bennett, M., St. Jacques, P. J., Anders, S.
(2011, December, 8). Novel use of electronic whiteboard in the operating room increases
surgical team compliance with pre-incision safety practices. SURGERY, 151(5), 660-666.
http://dx.doi.org/1
'TIME OUT' UNIVERSAL PROTOCOL
12
Morell Edel, E. (2010, October). Increasing Patient Safety and Surgical Team Communication by
Using a Count/Time Out Board. AORN Journal, 92, 420-424.
http://dx.doi.10.1016/j.aorn.210.03.013
OReilly, K. B. (2010, November, 1). Wrong patient, wrong-site procedures persist despite safety
protocol. American Medical News. Retrieved from
http://www.amednews.com/article/20101101/profession/311019963/2/
Yoder-Wise, P. S. (2015). Leading and Managing in Nursing (6th Ed.). St. Louis, MO: Elsevier,
Mosby.
'TIME OUT' UNIVERSAL PROTOCOL
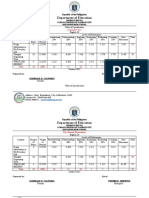
Introduction: Background and purpose for
quality and safety initiatives. Discusses the
leadership strategy to be performed.
Identify Clinical Need: Identifies a clinical
activity for review. Provides an analysis of the
problem using current nursing literature.
Designs an Interdisciplinary Team:
Identifies and analyzes the inclusion of team
members involved with the problem.
Data Collection Method: Chooses and
designs a method of data collection. Provides
support for collection method as a leadership
strategy.
Establishes Outcomes: Identifies a standard
of care (goal for improvement) that reflects
evidence-based practice.
Implementation Strategies: Selects and
describes a process for implementing change.
Integrates theory and EBP to support the
identified process.
Evaluation: Identifies and designs a method
for measuring improvement. Integrates theory
and EBP in analyzing improvement.
Scholarship: Integrates evidence of theory,
current evidence-based research and
information management resources to support
decisions.
Score
Sentence structure, spelling, grammar &
punctuation; APA Format
TOTAL POINTS
Nice job ladies! Rhonda Bishop
13
POINTS
POSSIBLE
5
POINTS
AWARDED
Comments
5
10
10
10
10
10
No tool
8
5
5
10
10
10
10
10
10
100
30
98
100
95
-3
Excessive use of quotes.
Paragraphing,
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Activity Design ScoutingDokumen10 halamanActivity Design ScoutingHoneyjo Nette100% (9)
- Geo Lab Report Point LoadDokumen9 halamanGeo Lab Report Point Loaddrbrainsol50% (2)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- 8 DaysDokumen337 halaman8 Daysprakab100% (1)
- Lindsay: VasquezDokumen1 halamanLindsay: Vasquezapi-240028260Belum ada peringkat
- Bullying IncivilitynovoiceDokumen14 halamanBullying Incivilitynovoiceapi-240028260Belum ada peringkat
- Project Final ReportDokumen13 halamanProject Final Reportapi-240028260Belum ada peringkat
- Service Learningnurs450Dokumen7 halamanService Learningnurs450api-240028260Belum ada peringkat
- Nurs 300 PortfolioDokumen2 halamanNurs 300 Portfolioapi-240028260Belum ada peringkat
- L Vasqueznurs340vulnerablepopulationDokumen6 halamanL Vasqueznurs340vulnerablepopulationapi-240028260Belum ada peringkat
- Ctu Medication ManagementnovoiceDokumen12 halamanCtu Medication Managementnovoiceapi-240028260Belum ada peringkat
- Vasquez L Nurs310-RealageDokumen11 halamanVasquez L Nurs310-Realageapi-240028260Belum ada peringkat
- Service Learningno VoiceDokumen8 halamanService Learningno Voiceapi-240028260Belum ada peringkat
- Osp Step 2Dokumen3 halamanOsp Step 2api-240028260Belum ada peringkat
- Running Head: Scope and Standards of Practice 1Dokumen11 halamanRunning Head: Scope and Standards of Practice 1api-240028260Belum ada peringkat
- Nurs 324 Discussion Post Dated 1Dokumen2 halamanNurs 324 Discussion Post Dated 1api-240028260Belum ada peringkat
- Patricia Benner: Brianna Rich Denise Preston Lindsay Vasquez Nursing 324 Ferris State UniversityDokumen9 halamanPatricia Benner: Brianna Rich Denise Preston Lindsay Vasquez Nursing 324 Ferris State Universityapi-240028260Belum ada peringkat
- L Vasquez AnalyzingaleaderDokumen11 halamanL Vasquez Analyzingaleaderapi-240028260Belum ada peringkat
- CaseDokumen2 halamanCaseapi-240028260Belum ada peringkat
- My Ethical ProfileDokumen7 halamanMy Ethical Profileapi-240028260Belum ada peringkat
- Oral HealthDokumen2 halamanOral Healthapi-240028260Belum ada peringkat
- Group 7 EncouragingexerciseDokumen13 halamanGroup 7 Encouragingexerciseapi-240028260Belum ada peringkat
- Vasquez HP ToolDokumen6 halamanVasquez HP Toolapi-240028260Belum ada peringkat
- BSN ChecklistDokumen1 halamanBSN Checklistapi-306305343Belum ada peringkat
- 5.mpob - LeadershipDokumen21 halaman5.mpob - LeadershipChaitanya PillalaBelum ada peringkat
- Navid DDLDokumen7 halamanNavid DDLVaibhav KarambeBelum ada peringkat
- Capitalism Communism Socialism DebateDokumen28 halamanCapitalism Communism Socialism DebateMr. Graham Long100% (1)
- Table of Specification ENGLISHDokumen2 halamanTable of Specification ENGLISHDonn Abel Aguilar IsturisBelum ada peringkat
- Proportions PosterDokumen1 halamanProportions Posterapi-214764900Belum ada peringkat
- Embedded Systems - RTOSDokumen23 halamanEmbedded Systems - RTOSCheril MehtaBelum ada peringkat
- How To Prepare Squash Specimen Samples For Microscopic ObservationDokumen3 halamanHow To Prepare Squash Specimen Samples For Microscopic ObservationSAMMYBelum ada peringkat
- A Personality Trait-Based Interactionist Model of Job PerformanceDokumen18 halamanA Personality Trait-Based Interactionist Model of Job PerformanceAlvina AhmedBelum ada peringkat
- Backup 2Dokumen59 halamanBackup 2Fabiola Tineo GamarraBelum ada peringkat
- DEMO 2 Critical Reading As ReasoningDokumen3 halamanDEMO 2 Critical Reading As ReasoningConnieRoseRamosBelum ada peringkat
- Mitchell 1986Dokumen34 halamanMitchell 1986Sara Veronica Florentin CuencaBelum ada peringkat
- NMIMS MBA Midterm Decision Analysis and Modeling ExamDokumen2 halamanNMIMS MBA Midterm Decision Analysis and Modeling ExamSachi SurbhiBelum ada peringkat
- COS1512 202 - 2015 - 1 - BDokumen33 halamanCOS1512 202 - 2015 - 1 - BLina Slabbert-van Der Walt100% (1)
- Charny - Mathematical Models of Bioheat TransferDokumen137 halamanCharny - Mathematical Models of Bioheat TransferMadalena PanBelum ada peringkat
- Rolfsen Knot Table Guide Crossings 1-10Dokumen4 halamanRolfsen Knot Table Guide Crossings 1-10Pangloss LeibnizBelum ada peringkat
- Outgoing Call Block BroadcastReceiver ExampleDokumen3 halamanOutgoing Call Block BroadcastReceiver ExampleZainUlAbidinBelum ada peringkat
- Viola Jones AlgorithmDokumen4 halamanViola Jones AlgorithmBhumika GowdaBelum ada peringkat
- Math Curriculum Overview Grades 1 8Dokumen1 halamanMath Curriculum Overview Grades 1 8GuiselleBelum ada peringkat
- Significance of Vaiseshika's PragabhavaDokumen5 halamanSignificance of Vaiseshika's Pragabhavavskanchi0% (1)
- Dompet Digital Di Kota SemarangDokumen10 halamanDompet Digital Di Kota SemarangRikson TandelilinBelum ada peringkat
- NAVMC 3500.35A (Food Services)Dokumen88 halamanNAVMC 3500.35A (Food Services)Alexander HawkBelum ada peringkat
- Rhythm Music and Education - Dalcroze PDFDokumen409 halamanRhythm Music and Education - Dalcroze PDFJhonatas Carmo100% (3)
- Cost of Litigation Report (2015)Dokumen17 halamanCost of Litigation Report (2015)GlennKesslerWPBelum ada peringkat
- McCann MIA CredentialsDokumen20 halamanMcCann MIA CredentialsgbertainaBelum ada peringkat
- Relay Testing Management SoftwareDokumen10 halamanRelay Testing Management Softwarechichid2008Belum ada peringkat
- Saline Water Intrusion in Coastal Aquifers: A Case Study From BangladeshDokumen6 halamanSaline Water Intrusion in Coastal Aquifers: A Case Study From BangladeshIOSRJEN : hard copy, certificates, Call for Papers 2013, publishing of journalBelum ada peringkat
- Google Fusion Tables: A Case StudyDokumen4 halamanGoogle Fusion Tables: A Case StudySeanBelum ada peringkat