JH 0215
Diunggah oleh
Muhammad RezaJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
JH 0215
Diunggah oleh
Muhammad RezaHak Cipta:
Format Tersedia
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
Ovarian Epithelial Cancer: Etiology and Pathogenesis
Jung-Hye Choi
Department of Pathology, Johns Hopkins University School of Medicine
To whom correspondence should be addressed. E-mail jchoi63@jhmi.edu
. Abstract
. Ovarian cancer
A. Clinical features
B. Classification and features
. Etiology
A. Epidemiological findings
B. Tumorigenesis hypothesis
C. Stem cell-like etiology
. Molecular pathogenesis
A. Molecular changes
B. Molecular carcinogenesis model
. Concluding remark
. References
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
. Abstract
Ovarian epithelial cancer is the fifth leading cuase of cancerrelated death among women in developed countires, and it is the most lethal
gynecological
malignancy.
Despite
its
clincal
significance,
the
pathophysiology of ovarian cancer is the least understood among all major
human malignancies due to a poor understanding of the etiological factors
and mechanisms of ovarian cancer progression. This review first summarize
the key findings and rencent advances in our understanding of etiology of
this disease, with particular emphasis on reproductive factors including
ovulation and hormones. The stem cell-like etiology of ovarian cancer is
briefly disccused as well. Ovarian carcinogenesis model based on recent
clinical, histopathological, and molecular genetic findings is next
summarized.
. Ovarian cancer
A. Clinical features
Ovarian cancer is the sixth most common cancer and the fifth leading
cause of cancer-related death among women in developed countries (1).
Worldwide, the total number of cases is approximately 190,000 per year (2).
In the United States, about 23,000 new cases were diagnosed while
approximately 14,000 women died from the disorder in the same year (3).
About 1 in 70 women in the United States will develop ovarian cancer (4).
In Korea, 11,404 cases were diagnosed and 855 women died of ovarian cancer
between 1993 and 2002 (5).
Only about 25% of women have localized disease at the time of
diagnosis because of the absence of specific symptoms and signs and the
lack of trustworthy screening system. Signs and symptoms of ovarian cancer
may include nausea, loss of appetite, abdominal discomfort and/or pain,
abnormal vaginal bleeding, and weight change. Despite the limitations of
sensitivity and specificity, the combination of pelvic exam, transvaginal
ultrasound, and CA125 assay are currently used as diagnostic tools. The
International Federation of Gynecology and Obstetrics (FIGO) stage has been
recognized as a significant prognostic factor in most studies (6, 7).
Patients in most cases present in stage III or IV with a 5-year survival of
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
around 28% and 16%, respectively, while the 5-year survival rate is up to
80% for patients in stage I. Standard management for advanced ovarian
cancer is cytoreductive surgery followed by paclitaxel/platinum-based
chemotherapy. Current regimens can achieve 25-30% complete pathological
response rate and 15.5-22 months median progression-free survival (2, 8).
Although ovarian cancer is considered a chemosensitive neoplasm with 80%
initially responding to conventional treatment, the common chemoresistance
resulting in eventual tumor recurrence gives rise to a poor long-term
survival rate among the women with advanced stage cancer at diagnosis. Thus,
improving the predictive value of screening and identifying the critical
drug targets are urgent for prevention, treatment, and survival of patients.
In this regard, current efforts are being directed toward increasing the
understanding of mechanism by which ovarian cancer develops and progresses.
B. Classification and features
According to the World Health Organization (WHO) histological
classification, an ovarian tumor can be classified into three categories
according to the most probable tissue of origin: surface epithelial tumors,
sex cord-stromal tumors, and germ cell tumors. Approximately 90% of
malignant tumors arise from the ovarian surface epithelium (OSE) with the
rest originating from granulosa cells (~ 5%) or, rarely, germs cells (~1%).
The OSE is a single layer of flat-to-cuboidal epithelial cells covering the
ovary. Ovarian epithelial cancers are heterogeneous and are primarily
divided into a number of subtypes, including serous (fallopian tube),
mucinous (endocervical-like), and endometrioid (endometrium-like) tumors (9,
10) based on the morphological, functional, and antigenic resemblance to
epithelium of Mullerian ducts. The rare clear cell and transitional cell
carcinomas are also classified as epithelial carcinoma, and they express
features like mesonephros and urothelium, respectively (9, 10). According
to the propensity of their proliferative and invasive behavior, ovarian
tumors are further subdivided into benign, borderline, or malignant tumor.
For example, benign tumors have little copious proliferation and invasive
behavior while malignant cancers have both proliferative and invasive
features. Borderline tumors, also known as low malignant potential, have
aggressive cellular proliferation but no invasive behavior.
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
. Etiology
A. Epidemiological findings
The etiology of ovarian cancer remains poorly understood. To date,
family history of ovarian cancer, age, early menarche, and nulliparity have
been consistently recognized as risk factors of ovarian epithelial cancer,
while pregnancy, oral contraceptive use, hysterectomy, and tubal ligation
are protective factors.
Familial ovarian epithelial cancer comprise approximately 5-10% of
ovarian cancer (11). BRCA1 or BRCA2 mutations are found in about 50% and
70% of ovarian cancer patients with at least one first-degree and two or
more affected relatives, respectively (12-14). The risk to develop ovarian
cancer is likely to increase, as women grow older. In the United States,
the mean age of incidence of ovarian cancer is 57-59 years, 50% of all
cases occur over age 65, and age-specific incidence peaks in the mid-70s
(15, 16). Recent studies have linked tobacco products/smoking to an
increased incidence of a specific type of ovarian cancer (17-19). In
addition, talc (20, 21), asbestos (22), and alcohol (23) have been
sometimes associated with an increased risk. However, these issues are
limited by inconsistent data and/or the lack of supportive animal models.
Thus, to date, epidemiological studies have failed to yield a consensus
regarding the contribution of chemical carcinogens to the development of
ovarian cancer. The data on obesity and ovarian cancer risk are
inconclusive, but generally suggest an increased risk for obese women.
Obesity is likely associated with some physiological or pathological
conditions in gynecology such as hormone levels, ovulatory function,
infertility, polycystic ovary syndrome, hyperandrogenism, and endometriosis
(24-26).
Countless epidemiological findings demonstrated the influence of
menstrual and/or reproductive factors in ovarian cancer development. Each
additional pregnancy decreases the risk 10-16% (27, 28). Interestingly,
several studies have reported a significant trend of decreasing ovarian
cancer risk with increasing age at first birth and/or greater age at last
birth (29-31). For example, Pike et al. in their population-based case
control study demonstrated that women whose only and last birth was after
age 35 years had about a 50% reduced risk of invasive ovarian cancer while
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
the protective effect was decreased with childbirth earlier than age 35
years (30). It is most likely that the use of oral contraceptives (OC)
decreases ovarian cancer risk. In several recent studies, the reduction of
ovarian cancer risk in women ever taking OC compared with non-users is
about 30% (32-34). The protection increases approximately 7% per year of
use, such that the long term users (over 10 years) had up to an 80%
reduction (33, 35). The beneficial effect of OC against ovarian cancer
risk persists for at least 10-15 years since last use, or even as long as
20-25 years (33, 36, 37). The favorable effect of OC has been observed in
most histological subtypes, but mucinous, and even in BRCA mutation
carriers (35). No significant difference in protective effect among the
diverse types of OC preparations is apparent. Hormone replacement therapy
(HRT), which is frequently prescribed for menopausal women due to its
possible benefits in reducing the risks of osteoporosis and heart disease,
provides another source for exogenous steroid. The epidemiologic findings
concerning HRT use and ovarian cancer risk are equivocal. However,
available data suggest that a moderately increased risk of ovarian cancer
may be related to estrogen therapy alone, but not with estrogen-progestin
combined regimes (37-39). Women suffering from infertility have about a
twofold higher ovarian cancer risk than does the general population (40).
Ovulation induction agents used in the treatment of infertility (clomiphene
or gonadotropins) may also be a risk factor for ovarian cancer (37-39, 41,
42). Tubal ligation and hysterectomy without oophorectomy reduced the risk
of ovarian cancer, presumably due to decreased exposure of the ovary to
potential carcinogen factors and/or inflammation (36, 43, 44).
B. Tumorigenesis hypothesis
To date, several hypotheses have been suggested to explain the
epidemiological findings. The incessant ovulation hypothesis, which was
initially proposed by Fathalla et al. in 1971 and later extended by other
researchers, postulates that repeated trauma during ovulation leads to an
increased exposure of the OSE to genetic abnormalities and/or other risk
factors (45, 46). Indeed, early menarche, late menopause, and nulliparity,
all of which have more ovulation episodes, increase the risk of developing
ovarian cancer. On the other hand, conditions in which ovulation is
suppressed, such as multiple pregnancies and prolonged breastfeeding, have
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
been reported to lower the risk to develop ovarian cancer (1, 47, 48).
Although
this
incessant
ovulation
theory
reconciles
appreciable
epidemiological and experimental data, the underlying mechanism remains
poorly understood. Moreover, some observations do not fit this theory (37,
49-51). Several hypotheses explore the etiology of ovarian cancer, which
are not exclusive with the incessant ovulation theory, and not with each
other. Based on the risk factor of pelvic inflammatory disease and the
favorable effects of hysterectomy and tubal ligation, the inflammation
hypothesis was advocated (22). The stromal hypothesis suggests that
some follicular cells escape from programmed cell death, continuously
produce steroid hormones, and stimulate neoplastic conversion of the OSE
cells in stroma (52). Considering hormonal carcinogenesis shown in
endocrine-related cancers such as breast and prostate cancers, two major
hormonal hypotheses are currently under examination. One is an
androgenic/progesterone hypothesis stating that androgens, which are
increased in menopausal or obese women, stimulate tumorigenesis in the
ovary while progesterone protects it (53). The other is the
gonadotropin
hypothesis
proposing
that
excessive
levels
of
gonadotropins, follicle stimulating hormone (FSH) and luteinizing
hormone(LH), related to the surge occurring during ovulation and the loss
of gonadal negative feedback for menopause and premature ovarian failure,
may play a role in the development and progression of ovarian epithelial
cancer (54). Indeed, author has demonstrated a regulatory role of
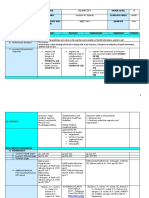
gonadotropins in both normal and neoplastic OSE cells (Figure 1). Treatment
with FSH or LH reduced the levels of gonadotropin-releasing hormone type II
(GnRH II) and gonadotropin-releasing hormone receptor (GnRHR) mRNA in IOSE
and ovarian cancer cells (55). The growth inhibitory effect of GnRH I or II
was blocked by pretreatment with FSH or LH. Treatment of pre-neoplastic
IOSE-80PC cells with gonadotropins resulted in a significant increase of
EGFR mRNA and EGFR protein levels(56). Both FSH and LH induced a
significant synergistic stimulation of mitogenesis in the presence of EGF.
The effect of gonadotropins on the expression of EGFR involved enhanced
cell growth via ERK-1/-2 and PI3K activation in pre-neoplastic ovarian
surface epithelial cells. In parallel experiments on metastasis, treatment
with FSH or LH significantly increased the invasion of ovarian cancer
cells(57). Treatment of SKOV-3 cells with FSH or LH enhanced net MMP/TIMP
balance and proteolysis potential. In addition, we demonstrated that
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
gonadotropins induced an increase in SKOV-3 invasiveness via the activation
of protein kinase A (PKA) and phosphatidyl-inositol-3-kinase (PI3K)
signaling pathways. There is increasing evidence suggesting that the key
reproductive hormones, not only androgen, progesterone and gonadotropin but
also GnRH (gonadotropin releasing hormone), activin/inhibin, leptin (58),
and estrogen, regulate the growth of normal OSE and ovarian cancer cells
(59).
A.
OSE
EGF/TNFa
Tunica albuginea
EGFR
IC
GnRH
GII and GR
FSH/LH
BV
Follicle
Proliferation/
Neoplastic conversion
B.
Other Tissues
FSH/LH
Invasion
MMP2/9
Metastasis
MMP2/9
and uPA
Peritoneal Fluid
OEC
OSE
Tunica albuginea
and uPA
Metastasis
FSH/LH
Figure
1.
Diagrammatic
representation
of
the
potential
role
of
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
gonadotropins in neoplastic transition of OSE cells (A) and metastasis of
ovarian epithelial cancer (B). Gonadotropins have been shown to regulate
the expression of EGFR and GnRH and its receptor, resulting in the
stimulation of growth potential in OSE trapped into the ovarian stroma (A).
Gonadotropins play a role in the invasiveness of ovarian cancer cells by
regulating the expression and secretion of tumor proteinases. FSH, follicle
stimulating hormone; LH, luteinizing hormone; EGF, Epidermal growth factor;
TNFa, tumor necrosis factor alpha; GnRH, gonadotropin releasing hormone;
GII, gonadotropin releasing hormone type two; GR, gonadotropins releasing
hormone receptor; BV, blood vessel; IC, inclusion cyst; OSE, ovarian
surface epithelium; MMP, matrix metalloproteinase.
C. Stem cell-like etiology
More recently, there is the stem cell niche concept for cancer
development (60). Somatic stem cells seem to reside within specialized area,
so called niche, where they may remain quiescent until activation by
injury or other stimulation. Adult OSE cells have the stem cell property of
self-renewal. It is also noteworthy that the OSE is closer in its
differentiation state to the pluripotent or multipotent mesodermal
embryonic precursor cells than other epithelial derivates (61, 62) As
discussed above, OSE is a simple, rather primitive epithelium with some
stromal features, but as it progresses to malignancy it loses stromal
characteristics and acquires the characteristics of the complex glandular
epithelial phenotypes of Mullerian duct-derived tissues such as serous
(fallopian
tube),
mucinous
(endocervical-like),
and
endometrioid
(endometrium-like) types. This retention of pluripotentiality may be
accompanied by greater proliferative capacity with reduced induction of
apoptotic cell death pathways and therefore perhaps enhanced the
susceptibility to neoplastic transformation. However, the cellular and
molecular mechanism by which pluripotent stem-like OSE cells escape from
quiescent status and undergo tumor formation is still not understood. It
may be mediated through incessant ovulation and following stimulation by
various factors such as inflammation, hormone, and growth factors. The OSE
is separated from the hormone/growth factor-producing stroma by the
collagenous tunica albuginea and a basement membrane. Ovulation and agingrelated trapping of OSE fragments result in surface invaginations (clefts)
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
and inclusion cysts in the ovarian cortex (63). Numerous studies have
provided direct evidence bearing on the frequent metaplasia and neoplastic
conversion of the clefts and inclusion cysts, presumably, via the aberrant
exposure to the hormone/growth factor-rich stromal microenvironment (64-67).
Thus, the OSE trapped into the ovarian cortex has been generally considered
as a neoplastic progression-prone site for OEC.
However, whether the
surface and/or cyst epithelial cells directly progress to a malignant
neoplasm is still not clear. Ness and Cottreau have suggested that an
inflammatory microenvironment such as cell damage, oxidative stress, and
elevations of cytokines and prostaglandins, rather than the trapping of the
OSE into the stroma, may mediate the mutagenesis induced by ovarian
ovulation (22). Repetitive loss of the basement membrane, which the OSE
cells generally are attached to as well as organized by, during ovulation,
has been implicated as an early event in the preneoplastic transformation
of OSE. This may be mediated through enhanced survival of the OSE cells,
which are multipotent mesodermal embryonic precursor cells, and/or
preferential selection of tumorigenically transformed cells (68-70).
Side population of tumor cells showing stem cells-like features
including unlimited self-renewal and proliferation has been recently
identified in leukemia, breast, and gastrointestinal cancer. If a small
number of these specialized cells escaped from chemotherapy or radiationinduced cytotoxicity, the tumor would be able to recur and subsequently
resistant to chemotherapy. Although 50-80% of patients with high stage
ovarian carcinoma initially response to conventional chemotherapy using
paclitaxel/platinum, the vast majority of patients will relapse and develop
chemoresistant. Thus, the high incidence of recurrence of ovarian cancer as
well as the multiple histological phenotypes indicative of multipotency
strongly suggests a stem cell-like etiology of ovarian cancer. Two recent
studies have identified stem/progenitor-like cells in ovarian cancer. Bapat
et al. found that two transformed clones from the ascites from a patient
possess stem-like characteristics and grow in an anchorage-independent
manner as spheroids (71). Significantly, both clones expressed self-renewal
mechanisms in vivo (sequential tumorigenicity) as well as multipotency and
tissue-specific differentiation markers. Szotek et al. also identified
side population (SP) with characteristics of the cancer stem cells
found with other tumors (72). In addition, the SP cells led to the
formation of new tumors much faster than did injections of non-SP (NSP)
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
10
cells when equal numbers were injected into the dorsal fat pad of nude mice.
As for chemoresistance, the SP cells were less responsive than NSP cells to
in vitro treatment with doxorubicin. Interestingly, Mullerian Inhibiting
substance, a glycoprotein hormone that causes Mullerian duct regression in
male embryos, maintained the sensitivity of SP cells to the drug. These
findings suggest that stem cell transformation can be the underlying cause
of development and progression of ovarian cancer.
. Molecular pathogenesis
A. Molecular changes
Several recent studies have contributed to the understanding of the
molecular biology of the OSE and ovarian carcinogenesis. During neoplastic
progression, the tendency of the OSE to undergo epithelio-mesenchymal
conversion diminishes and the cells become increasingly committed to
complex epithelial phenotypes, which include the appearance of E-cadherin
(73, 74), and secretory products, such as mucins and CA 125 (75, 76),
increased expression of the receptor for hepatocyte growth factor (c-Met)
(77) and keratin (78). Tumorigenesis is thought to result, at least in part,
from genetic abnormalities that lead to the disruption or enhancement of
intracellular signaling pathways that control cell proliferation, apoptosis,
or metastasis. In recent years, several key signaling pathways have been
extensively studied in ovarian cancer cells, including the loss of tumor
suppressor genes, failure of cell cycle regulation, telomerase upregulation and activation of oncogenic pathways. Specifically, tumor
suppressor genes such as BRCA1/BRCA2 (1), p53 (79), PTEN (80), Lot-1 (81),
OVCA-1 (82), DOC-2 (83), and NOEY2 (ARHI) (84) are highly mutated in
ovarian cancer. While the interaction of cyclins, cyclin-dependent kinases
(CDKs) and CDK inhibitors (CDKIs) are tightly regulated in normal cells,
some ovarian cancer cells lose their growth regulation as a result of the
overexpression of cyclins/CDKs and/or the loss of CDKIs such as p21 and p27
(85-90). Ovarian cancer cells have high levels of telomerase, a
ribonucleoprotein enzyme complex that adds new oligonucleotide repeats to
the ends of chromosomes, which maintains telomere length and eventually
results in rescue from senescence and resistance to apoptosis (91-93). In
contrast, normal OSE and pre-malignant lesions have little or no telomerase
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
11
activity (93, 94). Oncogenic signaling molecules, such as PI3K/Akt (95, 96),
K-Ras (97), Src (98), MAPK (99-103), and STATs (104), as well as tyrosine
kinase receptors, including ERBB2 (105), EGFR (106), and cFMS (the receptor
for colony-stimulating factor I) (107), are frequently amplified in ovarian
carcinomas. In addition, growth factors, hormones, and even fluctuations in
intracellular calcium levels can modulate cell proliferation and/or
metastasis through the MAPK and PI3K/Akt pathways. The intracellular
signals arising from MAPK cascades invariably lead to the activation of a
set of molecules that regulate cell growth, division and/or differentiation.
In ovarian cancer cells, MAPKs are regulated by cisplatin (108), paclitaxel
(103), endothelin-1 (109), gonadotropin-releasing hormone (GnRH) (110), and
gonadotropins (56, 111). It is becoming increasingly clear that the PI3K
signaling pathway plays a major role in the regulation of cell
proliferation, apoptosis, differentiation, tumorigenesis, cell migration,
invasion, and angiogenesis in ovarian cancer (99, 112-117). PI3K can be
activated by estrogen, gonadotropins, 4-hydroxy estradiol, hypoxia,
lysophosphatidic acid, as well as by various growth factors and receptor
tyrosine kinases in ovarian cancer cells (56, 99, 113, 115, 118-120).
Most deaths from ovarian cancer are due to its metastasis that easily
becomes resistant to conventional therapies. Recent findings have suggested
that proteolysis directed at the interface between ovarian cancer cells and
peritoneal tissues may play a role in the localized invasion and
dissemination of ovarian cancer cells in the peritoneal cavity (121, 122).
The metalloproteinases (MMPs) and the urokinase plasminogen activator (uPA)
have been the most intensely investigated proteolyic systems in ovarian
cancer. The MMP family contains 24 human members, of which MMP-2 and MMP-9
(gelatinase A, 72-kD type IV collagenase and gelatinase B, 92-kD type IV
collagenase) have been observed in several ovarian cancer cell lines and
detected in ascitic fluid from patients with advanced ovarian cancers, and
experimental metastasis is suppressed by a synthetic MMP inhibitor (123).
In ovarian cancer, uPA is also present in significant levels in ascites and
increased levels are related to poor prognosis (124-126). The invasiveness
of ovarian cancer cells has been reported to correlate with the expression
of MMP-2/-9 and uPA (124, 127, 128).
Drug resistance is described as a multifactorial phenomenon,
involving the expression of defense factors and/or detoxification
mechanisms, alterations in drug-target interactions (e.g., target
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
12
accessibility, target sensitivity, persistence of DNA cleavage, genomic
localization of DNA damage) and cellular response to specific cytotoxic
lesions (129). The resistance to cytotoxic agents might be stimulated by
increased expression of P-glycoprotein, the drug efflux pumps, and
multidrug resistance protein. However, recent data on the chemoresistance
of ovarian cancer suggested that a decreased susceptibility of the cancer
to apoptosis is strongly associated with drug resistance (130-134).
Chemotherapy led to a significant increase in p53 expression, which plays a
role in both apoptosis and DNA repair, along with enhanced chemoresistance
(135, 136). Although prognostic value of the expression of Bcl-2 family is
still inconclusive, up-regulation of Bcl-2 and/or down-regulation of Bax
have been correlated with increased chemoresistance (137-140). In addition,
inhibitors of caspases such as FLICE inhibitory protein (FLIP) and
inhibitor of apoptosis (IAP) were implicated as determinants of the
chemosensitivity of ovarian cancer (141-145).
B. Molecular carcinogenesis model
The OEC encompasses a diverse, biologically complex, group of
malignant neoplasms. As discussed above, this heterogenous neoplasmas are
classified by cell type into serous, mucinous, endometrioid, clear cell,
and transitional type, and then subdivided by clinical behavior into benign,
intermediate (borderline or low malignant-potential) and malignant. Despite
considerable efforts to elucidate the molecular mechanisms of ovarian
carcinoma, unlike colorectal carcinoma, its pathogenesis model has not been
described. Scully suggested that a predominant proportion of serous and
undifferentiated carcinomas, which accounts for about 65% of epithelial
ovarian carcinoma, arise directly from the trapped OSE cells and spread
rapidly (146). However, other studies suggested the possibility of a
stepwise progression from serous benign and borderline tumors to serous
carcinoma as well as de novo (147-149). In contrast with a de novo origin,
mucinous carcinoma (about 13% of epithelial cancers) most likely appear to
arise within or contiguous to pre-existing benign and borderline mucinous
tumors (150, 151). It has been suggested that the clear cell and
endometrioid carcinoma (about 20% of epithelial cancers) may arise from
endometriotic deposits or adenofibromas (146).
Based on the review of recent clinicopathological and molecular
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
13
genetic findings, we recently proposed a new ovarian carcinogenesis model
which suggests two main pathways of tumorigenesis (type I and type II).
Type I tumors (low-grade serous carcinoma, mucinous carcinoma, endometrioid
carcinoma, malignant transition tumor, and clear cell carcinoma) tend to be
low-grade neoplasms that arise in a stepwise manner from borderline tumors
that in turn develop from cystadenomas/adenofibromas. In contrast, type II
tumors (high grade serous carcinoma, malignant mixed mesodermal tumors, and
undifferentiated carcinoma) have been proposed to develop directly from the
OSE or inclusion cysts. It is so-called de novo development because
morphologically recognizable precursor lesions, like borderline tumor for
type I, have not been identified. Clinicopathological feature of the two
types are significantly distinct. Low-grade serous carcinomas typically
pursue an indolent course that may last more than 20 years. They are large
and often confined to the ovary at the time of diagnosis. Approximately 50
to 60% of patients ultimately succumb because of widespread intra-abdominal
carcinomatosis but the tumor maintains its low-grade appearance and low
proliferative index throughout its course. This contrasts with conventional
high-grade serous carcinoma that presents as a clinically aggressive
neoplasm that progress rapidly, metastasizes early in their course, and is
associated with a poor outcome. In addition to clinicopathological
observations, significant molecular evidences support the dualistic
carcinogenesis model. Type I low-grade serous carcinomas are frequently
associated with BRAF and KRAS mutations (~65%), while type II high-grade
serous carcinoma is likely involved in p53 mutation (~50-80%) and human
leukocyte antigen-G (HLA-G) overexpression (61%). It is noteworthy that the
molecular alterations for each type are mutually exclusive as shown in
Figure 2.
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
14
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
ISSN 1598-8767
Ovarian surface epithelium/Inclusion cysts
Serous borderline tumor (SBT)
Atypical proliferative serous tumor (APST)
Micropapillary serous carcinoma (MPSC)
Invasive MPSC
Low-grade serous carcinoma
Type
Type
Low grade (25% of serous carcinoma)
Slow progression,
~55% 5 year survival
Poor response to chemotherapy
High-grade serous carcinoma
High grade (75%)
Clinical
behavior
Rapid progression,
~30% 5 year survival
Initial response ~80%
Kras mutation
Braf mutation
Kras or Braf mutation
p53 mutations
HLA-G expression
35%
30%
65%
0%
0%
0%
0%
0%
50-80%
61%
Figure 2. Schematic representation of the dualistic model depicting the
development of ovarian serous carcinoma, the most common type of ovarian
cancer (147).
. Concluding remarks
To
conquer
ovarian
cancer,
identification
of
specific
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
15
diagnostic/prognostic factors and development of new preventive and/or
therapeutic approaches are urgently needed. It will be facilitated by
fundamental understanding of the etiology and pathogenesis of ovarian
cancer. For example, the characterization of ovarian cancer stem cells will
allow for the identification of molecules specifically expressed in these
cells that could serve as targets to eliminate this side population of
cancer cells that can rapidly develop the critical tumor cell mass and/or
resistance to conventional therapy. As reviewed above, there is increasing
evidence implicating a role of several reproductive factors in ovarian
cancer development. It is important that we gain a thorough understanding
of how the hormones/growth factors related to these reproductive events
exert their effect on the OSE, especially in view of the rapid increase in
ovarian cancer incidence after menopause and the potential prevention
associated with oral contraceptive use. The continued characterization of
the molecular and signaling mechanisms underlying the stimulatory or
inhibitory actions of these hormones in the growth, differentiation and
progression of OSE to ovarian cancer should bring about a better
understanding of ovarian pathogenesis. It will provide an opportunity for
the development of diagnostic and/or preventive approaches targeting signal
transduction pathways or key molecules.
. References
1. Greenlee RT, Murray T, Bolden S, Wingo PA 2000 Cancer statistics, 2000.
CA Cancer J Clin 50:7-33
2. Gadducci A, Cosio S, Gargini A, Genazzani AR 2004 Sex-steroid hormones,
gonadotropin and ovarian carcinogenesis: a review of epidemiological and
experimental data. Gynecol Endocrinol 19:216-228
3. Jemal A, Thomas A, Murray T, Thun M 2002 Cancer statistics, 2002. CA
Cancer J Clin 52:23-47
4. Quirk JT, Natarajan N 2005 Ovarian cancer incidence in the United States,
1992-1999. Gynecol Oncol 97:519-523
5. Chung HH, Hwang SY, Jung KW, Won YJ, Shin HR, Kim JW, Lee HP 2007
Ovarian cancer incidence and survival in Korea: 1993-2002. Int J Gynecol
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
16
Cancer 17:595-600
6. Heintz AP, Odicino F, Maisonneuve P, Beller U, Benedet JL, Creasman WT,
Ngan HY, Sideri M, Pecorelli S 2001 Carcinoma of the ovary. J Epidemiol
Biostat 6:107-138
7. Tingulstad S, Skjeldestad FE, Halvorsen TB, Hagen B 2003 Survival and
prognostic factors in patients with ovarian cancer. Obstet Gynecol 101:885891
8. Conte PF, Cianci C, Gadducci A 1999 Up date in the management of
advanced ovarian carcinoma. Crit Rev Oncol Hematol 32:49-58
9. Auersperg N, Wong AS, Choi KC, Kang SK, Leung PC 2001 Ovarian surface
epithelium: biology, endocrinology, and pathology. Endocr Rev 22:255-288
10. Chen VW, Ruiz B, Killeen JL, Cote TR, Wu XC, Correa CN 2003 Pathology
and classification of ovarian tumors. Cancer 97:2631-2642
11. Swisher E 2003 Ovarian cancer associated with inherited mutations in
BRCA1 or BRCA2. Curr Womens Health Rep 3:27-32
12. Xu CF, Solomon E 1996 Mutations of the BRCA1 gene in human cancer.
Semin Cancer Biol 7:33-40
13. Gayther SA, Harrington P, Russell P, Kharkevich G, Garkavtseva RF,
Ponder BA 1996 Rapid detection of regionally clustered germ-line BRCA1
mutations by multiplex heteroduplex analysis. UKCCCR Familial Ovarian
Cancer Study Group. Am J Hum Genet 58:451-456
14. Reedy M, Gallion H, Fowler JM, Kryscio R, Smith SA 2002 Contribution of
BRCA1 and BRCA2 to familial ovarian cancer: a gynecologic oncology group
study. Gynecol Oncol 85:255-259
15. Ries LA, Miller, B.A., Hankey, B.F., Kosary, C.L., Harras, A., Edwards,
B.K. ed. 1994 SEER cancer statistics review, 1973-1991:tables and graphs.
Bethesda (MD): NIH Plublication
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
17
16. Weiss NS, Cook, L.S., Farrow, D.C., Rosenblatt, K.A. 1996 Ovarian
cancer. In: Schottenfeld D, Faumeni, F.S.J. ed. Cancer epidemiology and
prevention. New York: Oxford University Press; 1040-1057
17. Modugno F, Ness RB, Cottreau CM 2002 Cigarette smoking and the risk of
mucinous and nonmucinous epithelial ovarian cancer. Epidemiology 13:467-471
18. Green A, Purdie D, Bain C, Siskind V, Webb PM 2001 Cigarette smoking
and risk of epithelial ovarian cancer (Australia). Cancer Causes Control
12:713-719
19. Marchbanks PA, Wilson H, Bastos E, Cramer DW, Schildkraut JM, Peterson
HB 2000 Cigarette smoking and epithelial ovarian cancer by histologic type.
Obstet Gynecol 95:255-260
20. Chang S, Risch HA 1997 Perineal talc exposure and risk of ovarian
carcinoma. Cancer 79:2396-2401
21. Harlow BL, Cramer DW, Bell DA, Welch WR 1992 Perineal exposure to talc
and ovarian cancer risk. Obstet Gynecol 80:19-26
22. Ness RB, Cottreau C 1999 Possible role of ovarian
inflammation in ovarian cancer. J Natl Cancer Inst 91:1459-1467
epithelial
23. Modugno F, Ness RB, Allen GO 2003 Alcohol consumption and the risk of
mucinous and nonmucinous epithelial ovarian cancer. Obstet Gynecol
102:1336-1343
24. Brannian JD, Hansen KA 2002 Leptin and ovarian folliculogenesis:
implications for ovulation induction and ART outcomes. Semin Reprod Med
20:103-112
25. Frost C, Coleman MP 1997 Obesity and ovarian cancer. Eur J Cancer
33:1529-1531
26. Purdie DM, Bain CJ, Webb PM, Whiteman DC, Pirozzo S, Green AC 2001 Body
size and ovarian cancer: case-control study and systematic review
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
18
(Australia). Cancer Causes Control 12:855-863
27. Risch HA, Marrett LD, Jain M, Howe GR 1996 Differences in risk factors
for epithelial ovarian cancer by histologic type. Results of a case-control
study. Am J Epidemiol 144:363-372
28. Hankinson SE, Colditz GA, Hunter DJ, Willett WC, Stampfer MJ, Rosner B,
Hennekens CH, Speizer FE 1995 A prospective study of reproductive factors
and risk of epithelial ovarian cancer. Cancer 76:284-290
29. Riman T, Dickman PW, Nilsson S, Correia N, Nordlinder H, Magnusson CM,
Persson IR 2002 Risk factors for invasive epithelial ovarian cancer:
results from a Swedish case-control study. Am J Epidemiol 156:363-373
30. Pike MC, Pearce CL, Peters R, Cozen W, Wan P, Wu AH 2004 Hormonal
factors and the risk of invasive ovarian cancer: a population-based casecontrol study,. Fertility and Sterility 82:186-195
31. Whiteman DC, Siskind V, Purdie DM, Green AC 2003 Timing of pregnancy
and the risk of epithelial ovarian cancer. Cancer Epidemiol Biomarkers Prev
12:42-46
32. Modugno F, Ness RB, Allen GO, Schildkraut JM, Davis FG, Goodman MT 2004
Oral contraceptive use, reproductive history, and risk of epithelial
ovarian cancer in women with and without endometriosis. Am J Obstet Gynecol
191:733-740
33. Bosetti C, Negri E, Trichopoulos D, Franceschi S, Beral V, Tzonou A,
Parazzini F, Greggi S, La Vecchia C 2002 Long-term effects of oral
contraceptives on ovarian cancer risk. Int J Cancer 102:262-265
34. Tung KH, Wilkens LR, Wu AH, McDuffie K, Nomura AM, Kolonel LN, Terada
KY, Goodman MT 2005 Effect of anovulation factors on pre- and
postmenopausal ovarian cancer risk: revisiting the incessant ovulation
hypothesis. Am J Epidemiol 161:321-329
35. McGuire V, Felberg A, Mills M, Ostrow KL, DiCioccio R, John EM, West DW,
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
19
Whittemore AS 2004 Relation of contraceptive and reproductive history to
ovarian cancer risk in carriers and noncarriers of BRCA1 gene mutations. Am
J Epidemiol 160:613-618
36. Ness RB, Grisso JA, Vergona R, Klapper J, Morgan M, Wheeler JE 2001
Oral contraceptives, other methods of contraception, and risk reduction for
ovarian cancer. Epidemiology 12:307-312
37. Whittemore AS, Harris R, Itnyre J 1992 Characteristics relating to
ovarian cancer risk: collaborative analysis of 12 US case-control studies.
II. Invasive epithelial ovarian cancers in white women. Collaborative
Ovarian Cancer Group. Am J Epidemiol 136:1184-1203
38. Riman T, Dickman PW, Nilsson S, Correia N, Nordlinder H, Magnusson CM,
Weiderpass E, Persson IR 2002 Hormone replacement therapy and the risk of
invasive epithelial ovarian cancer in Swedish women. J Natl Cancer Inst
94:497-504
39. Lacey JV, Jr., Mink PJ, Lubin JH, Sherman ME, Troisi R, Hartge P,
Schatzkin A, Schairer C 2002 Menopausal hormone replacement therapy and
risk of ovarian cancer. Jama 288:334-341
40. Ness RB, Cramer DW, Goodman MT, Kjaer SK, Mallin K, Mosgaard BJ, Purdie
DM, Risch HA, Vergona R, Wu AH 2002 Infertility, fertility drugs, and
ovarian cancer: a pooled analysis of case-control studies. Am J Epidemiol
155:217-224
41. Rossing MA, Daling JR, Weiss NS, Moore DE, Self SG 1994 Ovarian tumors
in a cohort of infertile women. N Engl J Med 331:771-776
42. Anderson SM, Dimitrievich E 1996 Ovulation induction for infertility is
it safe or not? S D J Med 49:419-421
43. Kurian AW, Balise RR, McGuire V, Whittemore AS 2005 Histologic types of
epithelial ovarian cancer: have they different risk factors? Gynecol Oncol
96:520-530
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
20
44. Parazzini F, Negri E, La Vecchia C, Luchini L, Mezzopane R 1993
Hysterectomy, oophorectomy, and subsequent ovarian cancer risk. Obstet
Gynecol 81:363-366
45. Fathalla MF 1971 Incessant ovulation--a factor in ovarian neoplasia?
Lancet 2:163
46. Casagrande JT, Louie EW, Pike MC, Roy S, Ross RK, Henderson BE 1979
"Incessant ovulation" and ovarian cancer. Lancet 2:170-173
47. Ford D, Easton DF, Bishop DT, Narod SA, Goldgar DE 1994 Risks of cancer
in BRCA1-mutation carriers. Breast Cancer Linkage Consortium. Lancet
343:692-695
48. Ford D, Easton DF, Stratton M, Narod S, Goldgar D, Devilee P, Bishop DT,
Weber B, Lenoir G, Chang-Claude J, Sobol H, Teare MD, Struewing J, Arason A,
Scherneck S, Peto J, Rebbeck TR, Tonin P, Neuhausen S, Barkardottir R,
Eyfjord J, Lynch H, Ponder BA, Gayther SA, Zelada-Hedman M, et al. 1998
Genetic heterogeneity and penetrance analysis of the BRCA1 and BRCA2 genes
in breast cancer families. The Breast Cancer Linkage Consortium. Am J Hum
Genet 62:676-689
49. Westhoff C, Murphy P, Heller D, Halim A 1993 Is ovarian cancer
associated with an increased frequency of germinal inclusion cysts? Am J
Epidemiol 138:90-93
50. Whiteman DC, Murphy MF, Cook LS, Cramer DW, Hartge P, Marchbanks PA,
Nasca PC, Ness RB, Purdie DM, Risch HA 2000 Multiple births and risk of
epithelial ovarian cancer. J Natl Cancer Inst 92:1172-1177
51. Lambe M, Wuu J, Rossing MA, Hsieh CC 1999 Twinning and maternal risk of
ovarian cancer. Lancet 353:1941
52. Cramer DW, Barbieri RL, Fraer AR, Harlow BL 2002 Determinants of early
follicular phase gonadotrophin and estradiol concentrations in women of
late reproductive age. Hum Reprod 17:221-227
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
21
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
53. Risch H 1998 Hormonal etiology of epithelial ovarian cancer, with a
hypothesis concerning the role of androgens and progesterone. JNCI Cancer
Spectrum 90:1774-1786
54. Choi JH, Wong AS, Huang HF, Leung PC 2007 Gonadotropins and ovarian
cancer. Endocr Rev 28:440-461
55. Choi JH, Choi KC, Auersperg N, Leung PC 2006 Differential regulation of
two forms of gonadotropin-releasing hormone messenger ribonucleic acid by
gonadotropins in human immortalized ovarian surface epithelium and ovarian
cancer cells. Endocr Relat Cancer 13:641-651
56. Choi JH, Choi KC, Auersperg N, Leung PC 2005 Gonadotropins upregulate
the epidermal growth factor receptor through activation of mitogenactivated protein kinases and phosphatidyl-inositol-3-kinase in human
ovarian surface epithelial cells. Endocr Relat Cancer 12:407-421
57. Choi JH, Choi KC, Auersperg N, Leung PC 2006 Gonadotropins activate
proteolysis and increase invasion through protein kinase A and
phosphatidylinositol 3-kinase pathways in human epithelial ovarian cancer
cells. Cancer Res 66:3912-3920
58. Choi JH, Park SH, Leung PC, Choi KC 2005 Expression of leptin receptors
and potential effects of leptin on the cell growth and activation of
mitogen-activated protein kinases in ovarian cancer cells. J Clin
Endocrinol Metab 90:207-210
59. Leung PC, Choi JH 2007 Endocrine signaling
epithelium and cancer. Hum Reprod Update 13:143-162
in
ovarian
surface
60. Li L, Xie T 2005 Stem cell niche: structure and function. Annu Rev Cell
Dev Biol 21:605-631
61. Bukovsky A, Svetlikova M, Caudle MR 2005 Oogenesis in cultures derived
from adult human ovaries. Reprod Biol Endocrinol 3:17
62. Bukovsky A, Caudle MR, Svetlikova M, Upadhyaya NB 2004 Origin of germ
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
22
cells and formation of new primary follicles in adult human ovaries. Reprod
Biol Endocrinol 2:20
63. Murdoch WJ 1994 Ovarian surface epithelium during ovulatory and
anovulatory ovine estrous cycles. Anat Rec 240:322-326
64. Scully RE 1995 Pathology of ovarian cancer precursors. J Cell Biochem
Suppl 23:208-218
65. Maines-Bandiera SL, Auersperg N 1997 Increased E-cadherin expression in
ovarian surface epithelium: an early step in metaplasia and dysplasia? Int
J Gynecol Pathol 16:250-255
66. Blaustein A, Kaganowicz A, Wells J 1982 Tumor markers in inclusion
cysts of the ovary. Cancer 49:722-726
67. Mittal KR, Goswami S, Demopoulos RI 1995 Immunohistochemical profile of
ovarian inclusion cysts in patients with and without ovarian carcinoma.
Histochem J 27:119-122
68. Roland IH, Yang W-L, Yang D-H, Daly MB, Ozols RF, Hamilton TC, Lynch HT,
Godwin AK, Xu X-X 2003 Loss of surface and cyst epithelial basement
membranes
and
preneoplastic
morphologic
changes
in
prophylactic
oophorectomies. Cancer 98:2607-2623
69. Capo-Chichi CD, Smith ER, Yang DH, Roland IH, Vanderveer L, Cohen C,
Hamilton TC, Godwin AK, Xu XX 2002 Dynamic alterations of the extracellular
environment of ovarian surface epithelial cells in premalignant
transformation, tumorigenicity, and metastasis. Cancer 95:1802-1815
70. Ozols RF, Bookman MA, Connolly DC, Daly MB, Godwin AK, Schilder RJ, Xu
X, Hamilton TC 2004 Focus on epithelial ovarian cancer. Cancer Cell 5:19-24
71. Bapat SA, Mali AM, Koppikar CB, Kurrey NK 2005 Stem and progenitor-like
cells contribute to the aggressive behavior of human epithelial ovarian
cancer. Cancer Res 65:3025-3029
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
23
72. Szotek PP, Pieretti-Vanmarcke R, Masiakos PT, Dinulescu DM, Connolly D,
Foster R, Dombkowski D, Preffer F, Maclaughlin DT, Donahoe PK 2006 Ovarian
cancer side population defines cells with stem cell-like characteristics
and Mullerian Inhibiting Substance responsiveness. Proc Natl Acad Sci U S A
103:11154-11159
73. Kantak SS, Kramer RH 1998 E-cadherin regulates anchorage-independent
growth and survival in oral squamous cell carcinoma cells. J Biol Chem
273:16953-16961
74. Sundfeldt K, Piontkewitz Y, Ivarsson K, Nilsson O, Hellberg P,
Brannstrom M, Janson PO, Enerback S, Hedin L 1997 E-cadherin expression in
human epithelial ovarian cancer and normal ovary. Int J Cancer 74:275-280
75. Young RH, Clement, P.B., Scully, R.E. 1988 The ovary In. New York:
Raven Press
76. Van Niekerk CC, Ramaekers FC, Hanselaar AG, Aldeweireldt J, Poels LG
1993 Changes in expression of differentiation markers between normal
ovarian cells and derived tumors. Am J Pathol 142:157-177
77. Huntsman D, Resau JH, Klineberg E, Auersperg N 1999 Comparison of c-met
expression in ovarian epithelial tumors and normal epithelia of the female
reproductive tract by quantitative laser scan microscopy. Am J Pathol
155:343-348
78. Dyck HG, Hamilton TC, Godwin AK, Lynch HT, Maines-Bandiera S, Auersperg
N 1996 Autonomy of the epithelial phenotype in human ovarian surface
epithelium: changes with neoplastic progression and with a family history
of ovarian cancer. Int J Cancer 69:429-436
79. Kacinski BM, Carter D, Kohorn EI, Mittal K, Bloodgood RS, Donahue J,
Kramer CA, Fischer D, Edwards R, Chambers SK, et al. 1989 Oncogene
expression in vivo by ovarian adenocarcinomas and mixed-mullerian tumors.
Yale J Biol Med 62:379-392
80. Kurose K, Zhou XP, Araki T, Cannistra SA, Maher ER, Eng C 2001 Frequent
loss of PTEN expression is linked to elevated phosphorylated Akt levels,
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
24
but not associated with p27 and cyclin D1 expression, in primary epithelial
ovarian carcinomas. Am J Pathol 158:2097-2106
81. Abdollahi A, Godwin AK, Miller PD, Getts LA, Schultz DC, Taguchi T,
Testa JR, Hamilton TC 1997 Identification of a gene containing zinc-finger
motifs based on lost expression in malignantly transformed rat ovarian
surface epithelial cells. Cancer Res 57:2029-2034
82. Schultz DC, Vanderveer L, Berman DB, Hamilton TC, Wong AJ, Godwin AK
1996 Identification of two candidate tumor suppressor genes on chromosome
17p13.3. Cancer Res 56:1997-2002
83. Mok SC, Chan WY, Wong KK, Muto MG, Berkowitz RS 1996 SPARC, an
extracellular matrix protein with tumor-suppressing activity in human
ovarian epithelial cells. Oncogene 12:1895-1901
84. Yu Y, Xu F, Peng H, Fang X, Zhao S, Li Y, Cuevas B, Kuo WL, Gray JW,
Siciliano M, Mills GB, Bast RC, Jr. 1999 NOEY2 (ARHI), an imprinted
putative tumor suppressor gene in ovarian and breast carcinomas. Proc Natl
Acad Sci U S A 96:214-219
85. Garzetti GG, Ciavattini A, Goteri G, De Nictolis M, Stramazzotti D,
Lucarini G, Biagini G 1995 Ki67 antigen immunostaining (MIB 1 monoclonal
antibody) in serous ovarian tumors: index of proliferative activity with
prognostic significance. Gynecol Oncol 56:169-174
86. Worsley SD, Ponder BA, Davies BR 1997 Overexpression of cyclin D1 in
epithelial ovarian cancers. Gynecol Oncol 64:189-195
87. Farley J, Smith LM, Darcy KM, Sobel E, O'Connor D, Henderson B,
Morrison LE, Birrer MJ 2003 Cyclin E expression is a significant predictor
of survival in advanced, suboptimally debulked ovarian epithelial cancers:
a Gynecologic Oncology Group study. Cancer Res 63:1235-1241
88. Ichikawa Y, Yoshida S, Koyama Y, Hirai M, Ishikawa T, Nishida M,
Tsunoda H, Kubo T, Miwa M, Uchida K 1996 Inactivation of p16/CDKN2 and
p15/MTS2 genes in different histological types and clinical stages of
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
25
primary ovarian tumors. Int J Cancer 69:466-470
89. Schmider A, Gee C, Friedmann W, Lukas JJ, Press MF, Lichtenegger W,
Reles A 2000 p21 (WAF1/CIP1) protein expression is associated with
prolonged survival but not with p53 expression in epithelial ovarian
carcinoma. Gynecol Oncol 77:237-242
90. Anttila MA, Kosma VM, Hongxiu J, Puolakka J, Juhola M, Saarikoski S,
Syrjanen K 1999 p21/WAF1 expression as related to p53, cell proliferation
and prognosis in epithelial ovarian cancer. Br J Cancer 79:1870-1878
91. Kyo S, Kanaya T, Ishikawa H, Ueno H, Inoue M 1996 Telomerase activity
in gynecological tumors. Clin Cancer Res 2:2023-2028
92. Kim NW, Piatyszek MA, Prowse KR, Harley CB, West MD, Ho PL, Coviello GM,
Wright WE, Weinrich SL, Shay JW 1994 Specific association of human
telomerase activity with immortal cells and cancer. Science 266:2011-2015
93. Counter CM, Hirte HW, Bacchetti S, Harley CB 1994 Telomerase activity
in human ovarian carcinoma. Proc Natl Acad Sci U S A 91:2900-2904
94. Kruk PA, Godwin AK, Hamilton TC, Auersperg N 1999 Telomeric instability
and reduced proliferative potential in ovarian surface epithelial cells
from women with a family history of ovarian cancer. Gynecol Oncol 73:229236
95. Mills GB, Lu Y, Fang X, Wang H, Eder A, Mao M, Swaby R, Cheng KW,
Stokoe D, Siminovitch K, Jaffe R, Gray J 2001 The role of genetic
abnormalities of PTEN and the phosphatidylinositol 3-kinase pathway in
breast and ovarian tumorigenesis, prognosis, and therapy. Semin Oncol
28:125-141
96. Cheng JQ, Godwin AK, Bellacosa A, Taguchi T, Franke TF, Hamilton TC,
Tsichlis PN, Testa JR 1992 AKT2, a putative oncogene encoding a member of a
subfamily of protein-serine/threonine kinases, is amplified in human
ovarian carcinomas. Proc Natl Acad Sci U S A 89:9267-9271
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
26
97. Enomoto T, Weghorst CM, Inoue M, Tanizawa O, Rice JM 1991 K-ras
activation occurs frequently in mucinous adenocarcinomas and rarely in
other common epithelial tumors of the human ovary. Am J Pathol 139:777-785
98. Wiener JR, Windham TC, Estrella VC, Parikh NU, Thall PF, Deavers MT,
Bast RC, Mills GB, Gallick GE 2003 Activated SRC protein tyrosine kinase is
overexpressed in late-stage human ovarian cancers. Gynecol Oncol 88:73-79
99. Wong AS, Kim SO, Leung PC, Auersperg N, Pelech SL 2001 Profiling of
protein kinases in the neoplastic transformation of human ovarian surface
epithelium. Gynecol Oncol 82:305-311
100. Pan ZZ, Bruening W, Giasson BI, Lee VM, Godwin AK 2002 Gamma-synuclein
promotes cancer cell survival and inhibits stress- and chemotherapy druginduced apoptosis by modulating MAPK pathways. J Biol Chem 277:35050-35060
101. Yazlovitskaya EM, Pelling JC, Persons DL 1999 Association of apoptosis
with the inhibition of extracellular signal-regulated protein kinase
activity in the tumor necrosis factor alpha-resistant ovarian carcinoma
cell line UCI 101. Mol Carcinog 25:14-20
102. Yamada SD, Hickson JA, Hrobowski Y, Vander Griend DJ, Benson D, Montag
A, Karrison T, Huo D, Rutgers J, Adams S, Rinker-Schaeffer CW 2002 Mitogenactivated protein kinase kinase 4 (MKK4) acts as a metastasis suppressor
gene in human ovarian carcinoma. Cancer Res 62:6717-6723
103. Wang TH, Popp DM, Wang HS, Saitoh M, Mural JG, Henley DC, Ichijo H,
Wimalasena J 1999 Microtubule dysfunction induced by paclitaxel initiates
apoptosis through both c-Jun N-terminal kinase (JNK)-dependent and independent pathways in ovarian cancer cells. J Biol Chem 274:8208-8216
104. Burke WM, Jin X, Lin HJ, Huang M, Liu R, Reynolds RK, Lin J 2001
Inhibition of constitutively active Stat3 suppresses growth of human
ovarian and breast cancer cells. Oncogene 20:7925-7934
105. Berchuck A, Kamel A, Whitaker R, Kerns B, Olt G, Kinney R, Soper JT,
Dodge R, Clarke-Pearson DL, Marks P, et al. 1990 Overexpression of HEROvarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
27
2/neu is associated with poor survival in advanced epithelial ovarian
cancer. Cancer Res 50:4087-4091
106. Kohler M, Janz I, Wintzer HO, Wagner E, Bauknecht T 1989 The
expression of EGF receptors, EGF-like factors and c-myc in ovarian and
cervical carcinomas and their potential clinical significance. Anticancer
Res 9:1537-1547
107. Kacinski BM, Carter D, Mittal K, Yee LD, Scata KA, Donofrio L,
Chambers SK, Wang KI, Yang-Feng T, Rohrschneider LR, et al. 1990 Ovarian
adenocarcinomas express fms-complementary transcripts and fms antigen,
often with coexpression of CSF-1. Am J Pathol 137:135-147
108. Persons DL, Yazlovitskaya EM, Cui W, Pelling JC 1999 Cisplatin-induced
activation of mitogen-activated protein kinases in ovarian carcinoma cells:
inhibition of extracellular signal-regulated kinase activity increases
sensitivity to cisplatin. Clin Cancer Res 5:1007-1014
109. Vacca F, Bagnato A, Catt KJ, Tecce R 2000 Transactivation of the
Epidermal Growth Factor Receptor in Endothelin-1-induced Mitogenic
Signaling in Human Ovarian Carcinoma Cells. Cancer Res 60:5310-5317
110. Kimura A, Ohmichi M, Kurachi H, Ikegami H, Hayakawa
Y, Nishio Y, Jikihara H, Matsuura N, Murata Y 1999
activated protein kinase/extracellular signal-regulated
gonadotropin-releasing hormone-induced growth inhibition
cancer cell line. Cancer Res 59:5133-5142
J, Tasaka K, Kanda
Role of mitogenkinase cascade in
of a human ovarian
111. Choi KC, Kang SK, Tai CJ, Auersperg N, Leung PC 2002 Folliclestimulating hormone activates mitogen-activated protein kinase in
preneoplastic and neoplastic ovarian surface epithelial cells. J Clin
Endocrinol Metab 87:2245-2253
112. Chang F, Lee JT, Navolanic PM, Steelman LS, Shelton JG, Blalock WL,
Franklin RA, McCubrey JA 2003 Involvement of PI3K/Akt pathway in cell cycle
progression, apoptosis, and neoplastic transformation: a target for cancer
chemotherapy. Leukemia 17:590-603
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
28
113. Vara JAF, Casado E, de Castro J, Cejas P, Belda-Iniesta C, GonzalezBaron M 2004 PI3K/Akt signalling pathway and cancer. Cancer Treatment
Reviews 30:193-204
114. Brader S, Eccles SA 2004 Phosphoinositide 3-kinase signalling pathways
in tumor progression, invasion and angiogenesis. Tumori 90:2-8
115. Ellerbroek SM, Halbleib JM, Benavidez M, Warmka JK, Wattenberg EV,
Stack MS, Hudson LG 2001 Phosphatidylinositol 3-kinase activity in
epidermal growth factor-stimulated matrix metalloproteinase-9 production
and cell surface association. Cancer Res 61:1855-1861
116. Wong AS, Roskelley CD, Pelech S, Miller D, Leung PC, Auersperg N 2004
Progressive changes in Met-dependent signaling in a human ovarian surface
epithelial model of malignant transformation. Exp Cell Res 299:248-256
117. Zhou HY, Wong AS 2006 Activation of p70S6K induces expression of
matrix metalloproteinase 9 associated with hepatocyte growth factormediated invasion in human ovarian cancer cells. Endocrinology 147:25572566
118. Xu L, Pathak PS, Fukumura D 2004 Hypoxia-induced activation of p38
mitogen-activated protein kinase and phosphatidylinositol 3'-kinase
signaling pathways contributes to expression of interleukin 8 in human
ovarian carcinoma cells. Clin Cancer Res 10:701-707
119. Gao N, Nester RA, Sarkar MA 2004 4-Hydroxy estradiol but not 2-hydroxy
estradiol induces expression of hypoxia-inducible factor 1alpha and
vascular endothelial growth factor A through phosphatidylinositol 3kinase/Akt/FRAP pathway in OVCAR-3 and A2780-CP70 human ovarian carcinoma
cells. Toxicol Appl Pharmacol 196:124-135
120. Lu J, Xiao Yj YJ, Baudhuin LM, Hong G, Xu Y 2002 Role of ether-linked
lysophosphatidic acids in ovarian cancer cells. J Lipid Res 43:463-476
121. Rodriguez C, Patel AV, Calle EE, Jacob EJ, Thun MJ 2001 Estrogen
replacement therapy and ovarian cancer mortality in a large prospective
study of US women. Jama 285:1460-1465
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
29
122. Song J, Fadiel A, Edusa V, Chen Z, So J, Sakamoto H, Fishman DA,
Naftolin F 2005 Estradiol-induced ezrin overexpression in ovarian cancer: a
new signaling domain for estrogen. Cancer Lett 220:57-65
123. Davies B, Waxman J, Wasan H, Abel P, Williams G, Krausz T, Neal D,
Thomas D, Hanby A, Balkwill F 1993 Levels of matrix metalloproteases in
bladder cancer correlate with tumor grade and invasion. Cancer Res 53:53655369
124. Schmalfeldt B, Kuhn W, Reuning U, Pache L, Dettmar P, Schmitt M,
Janicke F, Hofler H, Graeff H 1995 Primary tumor and metastasis in ovarian
cancer differ in their content of urokinase-type plasminogen activator, its
receptor, and inhibitors types 1 and 2. Cancer Res 55:3958-3963
125. Chambers SK, Gertz RE, Jr., Ivins CM, Kacinski BM 1995 The
significance of urokinase- type plasminogen activator, its inhibitors, and
its receptor in ascites of patients with epithelial ovarian cancer. Cancer
75:1627-1633
126. Moser TL, Young TN, Rodriguez GC, Pizzo SV, Bast RC, Jr., Stack MS
1994 Secretion of extracellular matrix-degrading proteinases is increased
in epithelial ovarian carcinoma. Int J Cancer 56:552-559
127. Ellerbroek SM, Fishman DA, Kearns AS, Bafetti LM, Stack MS 1999
Ovarian carcinoma regulation of matrix metalloproteinase-2 and membrane
type 1 matrix metalloproteinase through beta1 integrin. Cancer Res 59:16351641
128. Pustilnik TB, Estrella V, Wiener JR, Mao M, Eder A, Watt MA, Bast RC,
Jr., Mills GB 1999 Lysophosphatidic acid induces urokinase secretion by
ovarian cancer cells. Clin Cancer Res 5:3704-3710
129. Zunino F, Perego P, Pilotti S, Pratesi G, Supino R, Arcamone F 1997
Role of apoptotic response in cellular resistance to cytotoxic agents.
Pharmacol Ther 76:177-185
130. Hanahan D, Weinberg RA 2000 The hallmarks of cancer. Cell 100:57-70
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
30
131. Mor G, Straszewski S, Kamsteeg M 2002 Role of the Fas/Fas ligand
system in female reproductive organs: survival and apoptosis. Biochem
Pharmacol 64:1305-1315
132. Mueller PW, Price RG, Finn WF 1998 New approaches for detecting
thresholds of human nephrotoxicity using cadmium as an example. Environ
Health Perspect 106:227-230
133. Xerri L, Devilard E, Hassoun J, Mawas C, Birg F 1997 Fas ligand is not
only expressed in immune privileged human organs but is also coexpressed
with Fas in various epithelial tissues. Mol Pathol 50:87-91
134. Arts HJ, Van Der Zee AG, De Jong S, De Vries EG 2000 Options for
modulation of drug resistance in ovarian cancer. Int J Gynecol Cancer
10:47-52
135. Levesque MA, Katsaros D, Yu H, Zola P, Sismondi P, Giardina G,
Diamandis EP 1995 Mutant p53 protein overexpression is associated with poor
outcome in patients with well or moderately differentiated ovarian
carcinoma. Cancer 75:1327-1338
136. Petty R, Evans A, Duncan I, Kurbacher C, Cree I 1998 Drug resistance
in ovarian cancer - the role of p53. Pathol Oncol Res 4:97-102
137. Diebold J, Baretton G, Felchner M, Meier W, Dopfer K, Schmidt M, Lohrs
U 1996 bcl-2 expression, p53 accumulation, and apoptosis in ovarian
carcinomas. Am J Clin Pathol 105:341-349
138. Eliopoulos AG, Kerr DJ, Herod J, Hodgkins L, Krajewski S, Reed JC,
Young LS 1995 The control of apoptosis and drug resistance in ovarian
cancer: influence of p53 and Bcl-2. Oncogene 11:1217-1228
139. Herod JJ, Eliopoulos AG, Warwick J, Niedobitek G, Young LS, Kerr DJ
1996 The prognostic significance of Bcl-2 and p53 expression in ovarian
carcinoma. Cancer Res 56:2178-2184
140. Tai YT, Lee S, Niloff E, Weisman C, Strobel T, Cannistra SA 1998 BAX
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
31
protein expression and clinical outcome in epithelial ovarian cancer. J
Clin Oncol 16:2583-2590
141. Zygmunt M, Herr F, Keller-Schoenwetter S, Kunzi-Rapp K, Munstedt K,
Rao CV, Lang U, Preissner KT 2002 Characterization of human chorionic
gonadotropin as a novel angiogenic factor. J Clin Endocrinol Metab 87:52905296
142. Sasaki H, Sheng Y, Kotsuji F, Tsang BK 2000 Down-regulation of Xlinked inhibitor of apoptosis protein induces apoptosis in chemoresistant
human ovarian cancer cells. Cancer Res 60:5659-5666
143. Sasaki H, Kotsuji F, Tsang BK 2002 Caspase 3-mediated focal adhesion
kinase processing in human ovarian cancer cells: possible regulation by Xlinked inhibitor of apoptosis protein. Gynecol Oncol 85:339-350
144. Kirchhoff S, Muller WW, Krueger A, Schmitz I, Krammer PH 2000 TCRmediated up-regulation of c-FLIPshort correlates with resistance toward
CD95-mediated apoptosis by blocking death-inducing signaling complex
activity. J Immunol 165:6293-6300
145. Krueger A, Schmitz I, Baumann S, Krammer PH, Kirchhoff S 2001 Cellular
FLICE-inhibitory protein splice variants inhibit different steps of
caspase-8 activation at the CD95 death-inducing signaling complex. J Biol
Chem 276:20633-20640
146. Scully RE 2000 Influence of origin of ovarian cancer on efficacy of
screening. Lancet 355:1028-1029
147. Shih Ie M, Kurman RJ 2004 Ovarian tumorigenesis: a proposed model
based on morphological and molecular genetic analysis. Am J Pathol
164:1511-1518
148. Tibiletti MG, Bernasconi B, Taborelli M, Facco C, Riva C, Capella C,
Franchi M, Binelli G, Acquati F, Taramelli R 2003 Genetic and cytogenetic
observations among different types of ovarian tumors are compatible with a
progression model underlying ovarian tumorigenesis. Cancer Genet Cytogenet
146:145-153
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
ISSN 1598-8767
BioWave Vol. 10 No.4 2008
http://bric.postech.ac.kr/webzine/
32
149. Horiuchi A, Itoh K, Shimizu M, Nakai I, Yamazaki T, Kimura K, Suzuki A,
Shiozawa I, Ueda N, Konishi I 2003 Toward understanding the natural history
of ovarian carcinoma development: a clinicopathological approach. Gynecol
Oncol 88:309-317
150. Puls LE, Powell DE, DePriest PD, Gallion HH, Hunter JE, Kryscio RJ,
Van Nagell J, J. R. 1992 Transition from benign to malignant epithelium in
mucinous and serous ovarian cystadenocarcinoma. Gynecologic Oncology 47:5357
151. Bell DA, Scully RE 1994 Early de novo ovarian carcinoma. A study of
fourteen cases. Cancer 73:1859-1864
Key Words: Ovarian epithelial cancer, Ovarian surface epithelium, Etiology,
Pathogenesis, Cancer stem cells, p53, BRAF, KRAS, Serous borderline tumor,
Gonadotropin
Disclaimer: "BioWave" is not political. The views and opinions expressed by its
writers do not necessarily reflect those of the Biological Research Information
Center(BRIC). Copyright 2008, the Biological Research Information Center(BRIC),
Pohang 790-784, Korea.
" BioWave" .
" BioWave (http://bric.postech.ac.kr/webzine)
Vol. 10 No. 4" .
(mail: biowave@bric.postech.ac.kr Tel: 054-279-8197~8) .
(. .)
Ovarian Epithelial Cancer: Etiology and Pathogenesis-Jung-Hye Choi
Anda mungkin juga menyukai
- Final File Hypo GuidelinesDokumen41 halamanFinal File Hypo Guidelinesroatfatchuri100% (1)
- WiliamDokumen5 halamanWiliamMuhammad RezaBelum ada peringkat
- WiliamDokumen5 halamanWiliamMuhammad RezaBelum ada peringkat
- Community Pharmacy Dispensing Costs in The State ofDokumen3 halamanCommunity Pharmacy Dispensing Costs in The State ofMuhammad RezaBelum ada peringkat
- Vane JRDokumen8 halamanVane JRMuhammad RezaBelum ada peringkat
- InTech-Ethics in Pharmaceutical IssuesDokumen21 halamanInTech-Ethics in Pharmaceutical IssuesMuhammad RezaBelum ada peringkat
- 44 Drug Information CenterDokumen5 halaman44 Drug Information CenterMuhammad RezaBelum ada peringkat
- We The Children: End-Decade Review of The Follow-Up To The World Summit For Children Report of The Secretary-General (2001)Dokumen2 halamanWe The Children: End-Decade Review of The Follow-Up To The World Summit For Children Report of The Secretary-General (2001)Muhammad RezaBelum ada peringkat
- Kurva PCTDokumen2 halamanKurva PCTMuhammad RezaBelum ada peringkat
- Extraction and Physicochemical Determination of Garlic: (Allium Sativum L) OilDokumen4 halamanExtraction and Physicochemical Determination of Garlic: (Allium Sativum L) OilMuhammad RezaBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Pil 2425Dokumen6 halamanPil 2425Gabriela ChiritoiuBelum ada peringkat
- Melatonina e EndometrioseDokumen8 halamanMelatonina e EndometrioseFatima VieiraBelum ada peringkat
- Nada Lincomycyn and Espectynomycin Solubleucm061812Dokumen4 halamanNada Lincomycyn and Espectynomycin Solubleucm061812laurz95Belum ada peringkat
- Applications of Humic and Fulvic Acids in AquacultureDokumen2 halamanApplications of Humic and Fulvic Acids in AquacultureAlexandra Nathaly Beltran Contreras100% (1)
- Nucleus DropDokumen1 halamanNucleus DropYovinus DenyBelum ada peringkat
- Chron's Disease 2Dokumen3 halamanChron's Disease 2TarantadoBelum ada peringkat
- Lymphatic Drainage 101Dokumen6 halamanLymphatic Drainage 101Vy HoangBelum ada peringkat
- MedicalDokumen3 halamanMedicalmumtazkauser74Belum ada peringkat
- AWWA Alt Disnfec Fro THM RemovalDokumen264 halamanAWWA Alt Disnfec Fro THM RemovalsaishankarlBelum ada peringkat
- Chronic Limb IschemiaDokumen29 halamanChronic Limb IschemiaSadia NaveedBelum ada peringkat
- JulieKJohnsonHe 2016 9ACascadeOfSmallEvent CaseStudiesInPatientSDokumen5 halamanJulieKJohnsonHe 2016 9ACascadeOfSmallEvent CaseStudiesInPatientSMarylanBelum ada peringkat
- Asia Pacific October 2022Dokumen24 halamanAsia Pacific October 2022Dhananjay VasuDevaBelum ada peringkat
- Código Descripción Costo Unita. Existencia Unidades Costo Existencia Precio 1 %utilDokumen24 halamanCódigo Descripción Costo Unita. Existencia Unidades Costo Existencia Precio 1 %utilNiky Dos SantosBelum ada peringkat
- Management of HydrocephalusDokumen4 halamanManagement of HydrocephalusShine CharityBelum ada peringkat
- Nerve PainDokumen1 halamanNerve PainRahafBelum ada peringkat
- Tel No.: 0141-2721966, Fax No.: 0141-2721919, Email: Mail@ruidp - Gov.in, Web Site: WWW - Ruidp.gov - inDokumen4 halamanTel No.: 0141-2721966, Fax No.: 0141-2721919, Email: Mail@ruidp - Gov.in, Web Site: WWW - Ruidp.gov - inPrasenjit DeyBelum ada peringkat
- Surgical Approaches To The Skull BaseDokumen2 halamanSurgical Approaches To The Skull Baseİbrahim ErkutluBelum ada peringkat
- DR Arzoo Nephrology ThesesDokumen35 halamanDR Arzoo Nephrology ThesesAzam ArzooBelum ada peringkat
- Thoughts Thoughts: 'Universe, Please Help Me Maintain An Effective Meditative-State. Thank You.'Dokumen4 halamanThoughts Thoughts: 'Universe, Please Help Me Maintain An Effective Meditative-State. Thank You.'Mincheol KangBelum ada peringkat
- Third Molar Impaction-A Review: Divya.T, Themozhi M.SDokumen5 halamanThird Molar Impaction-A Review: Divya.T, Themozhi M.SCiutac ŞtefanBelum ada peringkat
- Game Addiction PDFDokumen9 halamanGame Addiction PDFRonaldas GadzimugometovasBelum ada peringkat
- COE WorksheetDokumen16 halamanCOE WorksheetiloveraynaBelum ada peringkat
- Anorectal MalformationDokumen40 halamanAnorectal Malformationblessy83% (18)
- Q1 Grade 10 HEALTH DLL Week 2Dokumen14 halamanQ1 Grade 10 HEALTH DLL Week 2Leonor MayoyaBelum ada peringkat
- Lifepak 20e: Operating InstructionsDokumen218 halamanLifepak 20e: Operating InstructionsJorge ArturoBelum ada peringkat
- DrugStudyFormatDokumen2 halamanDrugStudyFormatSheryl Ann Barit PedinesBelum ada peringkat
- TramadolDokumen19 halamanTramadolanandhra2010Belum ada peringkat
- AHA ACLS Provider Manual $45Dokumen2 halamanAHA ACLS Provider Manual $45Jigar GandhiBelum ada peringkat
- MCQ ThyroidDokumen6 halamanMCQ ThyroidFaridOrahaBelum ada peringkat
- Jack Poylangada - Copy of Stamper Self-Care JournalDokumen8 halamanJack Poylangada - Copy of Stamper Self-Care Journalapi-503633296100% (3)