Nursing Diagnosis For Tonsillitis
Diunggah oleh
Vaneca GoDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Nursing Diagnosis For Tonsillitis
Diunggah oleh
Vaneca GoHak Cipta:
Format Tersedia
Nursing Diagnosis for Tonsillitis : Preoperative 1. 2. 3. Swallowing disorders related to inflammatory processes.
Acute pain related to tonsil tissue swelling. Imbalance nutrition less than body requirements related to tonsil tissue swelling.
4. Hipertermi related to the disease process.
5. Anxiety related to discomfort.
Nursing Diagnosis for Tonsillitis : Postoperative 1. 2. 3. Acute pain related to surgical incision, tissue discontinuities. High risk of infection related to invasive procedures. Lack of knowledge about the diet related to less information.
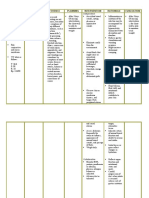
Nursing Diagnosis Impaired Skin integrity Altered epidermis and/or dermis: Invasion of body structures, destruction of skin layers (dermis), and disruption of skin surface (epidermis). Related Factors: External: Hyperthermia, hypothermia, chemical substance, mechanical factors (e.g. friction, shearing forces, pressure, restraint), physical immobilization, humidity, extremes in age, moisture, radiation, medications Internal: Altered metabolic state, altered nutritional state (e.g. obesity, emaciation), altered circulation, altered sensation, altered pigmentation, skeletal prominence, developmental factors, immunological deficit, alterations in skin turgor (change in elasticity), altered fluid status. Suggested Nursing Outcomes Tissue Integrity: Skin and Mucous Membranes Wound Healing: Primary Intention Wound Healing: Secondary Intention Regains integrity of skin surface Reports any altered sensation or pain at site of skin impairment Demonstrates understanding of plan to heal skin and prevent reinjury Describes measures to protect and heal the skin and to care for any skin lesion Incision Site Care Pressure Ulcer Care Skin Care: Topical Treatments Skin Surveillance Wound Care
Client Outcomes
Suggested Nursing Interventions
Nursing Interventions and Rationales Nursing Interventions Assess site of skin impairment and determine etiology (e.g., acute or chronic wound, burn, dermatological lesion, pressure ulcer, skin tear) Monitor site of skin impairment at least once a day for color changes, redness, swelling, warmth, pain, or other signs of infection. Individualize plan according to client's skin condition, needs, and preferences. Avoid harsh cleansing agents, hot water, extreme friction or force, or cleansing too frequently . For clients with limited mobility, use a risk-assessment tool to systematically assess immobility-related risk factors. A validated risk-assessment tool such as the Norton or Braden scale should be used to identify clients at risk for immobility-related skin breakdown. Transfer client with care to protect against the adverse effects of external mechanical forces such as pressure, friction, and shear. Rationales Prior assessment of wound etiology is critical for proper identification of nursing interventions.
Systematic inspection can identify impending problems early.
Do not position client on site of skin impairment. If consistent with overall client management goals, turn and position client at least every 2 hours Evaluate for use of specialty mattresses, beds Select a topical treatment that will maintain a moist wound-healing environment and that is balanced with the need to absorb exudates Avoid massaging around the site of skin impairment and
To reduce shear and friction, and use lift devices, pillows, foam wedges, and pressure-reducing devices in the bed.
over bony prominences. Assess client's nutritional status Massage may lead to deep-tissue trauma Inadequate nutritional intake places individuals at risk for skin breakdown and compromises healing Home Care Interventions Client and Family Teaching
Teach skin and wound assessment and ways to monitor for signs and symptoms of infection, complications, and healing Teach client to use a topical treatment that is matched to the client, wound, and setting. If consistent with overall client management goals, teach how to turn and reposition at least every 2 hours Teach client to use pillows, foam wedges, and pressure-reducing devices to prevent pressure injury
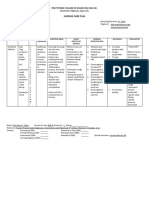
Subjective I do not feel like eating Objective Solu-Cortef 100 mg IV Q8hr RAC PICC Foley Catheter Wound L. Foot Recent hx of UTI Albumin 9/30/08 2.5 L Unwillingness to eat Wbc 9/30 8.4 and 10/02 10.7 normal Hgb 9/30 11.3 L 10/02 9.7 L Risk for Infection R/T inadequate secondary defenses, immunosuppression, invasive procedures, and malnutrition. GOAL: Client will remain free of infection, as evidenced by normal WBC count, temp < 100 F, and absence of purulent drainage from incisions. Or 1. Client will show no signs and symptoms of infection by discharge? Note ( cannot teach pt) does not recall information Assessment 1. Assess for presence, existence of, and history of risk factors of infection. 2. Monitor white blood count (WBC) 3. Observed/Monitor for signs and symptoms of infection. 4. Assess for nutritional status. 5. Assess immunization status. Decrease stressors: 6. Stress proper hand washing technique by all caregivers between therapies. 7. Encourage deep breathing, coughing, and turning q 2hr. 8. Provide regular catheter/perineal care and proper foley care daily. 9. Obtain appropriate tissue/fluid specimens for observation and culture/sensitivities testing. Teaching/counseling/referrals: 10. Teach family members and caregivers about protecting susceptible patient from themselves and others with infections or cold. 11. Teach patient and caregiver the signs and symptoms of infection, and when to report to physician 12. Review individual nutritional needs, appropriate exercise program, and need for rest. Assessment 1. Assess clt at 1530 am. and clt has a Foley catheter present, wound on the L. heel, PICC RAC and Hx of UTI as a risk factor. 2. Monitor WBC count, labs within normal parameters 9/30 (8.4) and 10/02 (10.7). 3. No signs and symptoms (redness, swelling, purulent drainage) at PICC, and Foley clear yellow urine w/o visible sediment and Temp of 98.1 F 4. Albumin level of 2.5 L and unwillingness to eat, pt states I do not feel like eating. and < 25% food eaten. Enjoys strawberry ice cream and hot chocolate, but drinks Ensure chocolate. 5. No records of a pneumonax vaccine given. MD placed an ordered and SN administered it. Decrease stressors: 6. Washed hands before and after pt. contact between therapies. Staff is aware of proper hand washing technique. 7. Taught patient to deep breath, cough and turn q hr, pt needs to be reminded. 8. Provided a total sponge bath on 10/02 at 1000, secured the foley catheter with tape and reminded pt not to pull on catheter, and cleaned the skin around the catheter and washed my hands before and after catheter care. 9. Obtain a Mersa swap at 1700 and results pending Teaching/counseling/referrals: 10. Taught son preventive hygiene practices/ methods by return demonstration and to gown up, wear a mask and glove if
they have infection or cold. 11. Unable to teach patient the signs and symptoms of infection, pt has short term memory loss, taught patients son the signs and symptoms of infection( fever >100 F, foul smelly urine, confusion, redness, purulent drainage at the wound) 12. Advice the nurse the best way to treat this patient is to be placed on routine care, provide enough rest and at sleep use BIPAP 35 %, and provided active and passive ROM. Unable to let patient get out of bed due to high risk of injury.
We do not have to do rationales.
A wound infection happens when germs enter a break in the skin. These germs, called bacteria, attach to tissues causing wounds to stop healing, and other signs and symptoms. Wounds can be punctures (holes), lacerations (tears), incisions (cuts), or burns. Deep ulcers (open sores), large burns, or bite wounds are more likely than other wounds to get infected. Wound infection can also happen in small wounds that were not treated.
Anda mungkin juga menyukai
- Nursing Care Plan: Risk For Ineffective Airway Clearance Related To Bleeding From Tonsillectomy Short TermDokumen4 halamanNursing Care Plan: Risk For Ineffective Airway Clearance Related To Bleeding From Tonsillectomy Short TermErika Danalle ArceoBelum ada peringkat
- Nursing Care Plan For TonsillitisDokumen3 halamanNursing Care Plan For TonsillitisEden Cruz50% (6)
- Nursing Care of Client With Cataract SurgeryDokumen11 halamanNursing Care of Client With Cataract SurgeryFatin Fatihah AzizanBelum ada peringkat
- NCP LaminectomyDokumen4 halamanNCP LaminectomyMark Zedrix MediarioBelum ada peringkat
- NCP TonsilitisDokumen11 halamanNCP TonsilitisGra Cie50% (6)
- Nursing Care Plan For Pneumonia NCP PDFDokumen3 halamanNursing Care Plan For Pneumonia NCP PDFFARAH MAE MEDINA100% (2)
- CP Intestinal Obstruction Nursing Care PlanDokumen7 halamanCP Intestinal Obstruction Nursing Care PlanShiella Heart MalanaBelum ada peringkat
- Assessment Diagnosis Planning Implementation Evaluation No Subjective Cues ObjectiveDokumen3 halamanAssessment Diagnosis Planning Implementation Evaluation No Subjective Cues ObjectiveMaverick LimBelum ada peringkat
- Bronchopneumonia Care PlanDokumen6 halamanBronchopneumonia Care PlanAbhijit Soundade0% (1)
- FractureDokumen1 halamanFractureReechie TeasoonBelum ada peringkat
- NCP PancreatitisDokumen2 halamanNCP PancreatitisJeanelle Generoso100% (1)
- NCP Acute Pain RT CancerDokumen3 halamanNCP Acute Pain RT CancerCharissa Magistrado De LeonBelum ada peringkat
- NCP HyperthermiaDokumen1 halamanNCP HyperthermiaPastor James PacadaljenBelum ada peringkat
- Altered Bowel EliminationDokumen1 halamanAltered Bowel EliminationneoclintBelum ada peringkat
- Ineffective Airway Clearance: Nursing Care PlanDokumen2 halamanIneffective Airway Clearance: Nursing Care PlanJose Mari F. Esguerra0% (1)
- Nursing Care Plan Pedia TB MeningitisDokumen2 halamanNursing Care Plan Pedia TB Meningitisderic100% (10)
- Nursing Care Plan: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDokumen3 halamanNursing Care Plan: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationAbdallah AlasalBelum ada peringkat
- Nursing Care Plan: IndependentDokumen2 halamanNursing Care Plan: IndependentAdhaBelum ada peringkat
- NCP FeverDokumen2 halamanNCP FeverMary Joyce LimoicoBelum ada peringkat
- Nursing Care Plan JaudiceDokumen3 halamanNursing Care Plan Jaudicepapadaad100% (1)
- NCP Measles Case PresDokumen1 halamanNCP Measles Case PresFranz RolfBelum ada peringkat
- NCP Pre EclampsiaDokumen2 halamanNCP Pre EclampsiaFarrah Grace Birowa0% (1)
- NCPDokumen7 halamanNCPChris Denver BancaleBelum ada peringkat
- Nursing Care Plan For Pedia TB Meningitis NCPDokumen2 halamanNursing Care Plan For Pedia TB Meningitis NCPderic100% (1)
- Nursing Care Plan Peptic UlcerDokumen3 halamanNursing Care Plan Peptic UlcerJefferson Baluyot PalmaBelum ada peringkat
- Nursing Care Plan: Chronic PancreatitisDokumen8 halamanNursing Care Plan: Chronic PancreatitisAnne B. Buenvenida100% (2)
- Nursing Care Plan of MeningitisDokumen2 halamanNursing Care Plan of MeningitisŦỏṯặ Łaẕỗzą100% (7)
- Word Ncp.......... TetanusDokumen6 halamanWord Ncp.......... TetanusaianrBelum ada peringkat
- Nursing Care PlanDokumen13 halamanNursing Care PlanCris Solis33% (3)
- Thyroidectomy NCPDokumen1 halamanThyroidectomy NCPkzbreakerrBelum ada peringkat
- Nursing Care Plan: General: Goals Met GenreralDokumen3 halamanNursing Care Plan: General: Goals Met GenreralRomzy BasañesBelum ada peringkat
- NCP LocDokumen2 halamanNCP LocMel RodolfoBelum ada peringkat
- Nursing Management: OF ArteriosclerosisDokumen6 halamanNursing Management: OF ArteriosclerosisANCHAL SHARMABelum ada peringkat
- LARYNGITISDokumen13 halamanLARYNGITIStherese BBelum ada peringkat
- Fever NCPDokumen3 halamanFever NCPBruno MercuryBelum ada peringkat
- Hypospadia CompletedDokumen92 halamanHypospadia Completedgideon A. owusu100% (1)
- NCP FVDDokumen2 halamanNCP FVDMarlon AnryBelum ada peringkat
- Nursing DX: Acute Pain Related To Surgical Manipulation (Laminectomy) As Manifested by Reports of Pain On The Lumbar Area Rated As 7/10Dokumen1 halamanNursing DX: Acute Pain Related To Surgical Manipulation (Laminectomy) As Manifested by Reports of Pain On The Lumbar Area Rated As 7/10YESSAMIN GUADIZ100% (2)
- NCPDokumen3 halamanNCPChrisTine M. MoralesBelum ada peringkat
- NCP InfectionDokumen3 halamanNCP InfectionPrince AhmirBelum ada peringkat
- Nursing Care Plan 1Dokumen4 halamanNursing Care Plan 1Johndelle Banlasan Hernan100% (1)
- Postnatal ExaminationDokumen19 halamanPostnatal ExaminationAlpha100% (1)
- NCP TonsillitisDokumen4 halamanNCP TonsillitisYuyu Tulawie75% (4)
- HerniaDokumen6 halamanHerniahani alzo3bi100% (7)
- NCP PryllDokumen6 halamanNCP PryllpjcolitaBelum ada peringkat
- Nursing Care Plan2Dokumen13 halamanNursing Care Plan2Nna ANn CastleBelum ada peringkat
- Novilyn C. Pataray BSN - Ii Conjunctivitis: St. Paul College of Ilocos SurDokumen1 halamanNovilyn C. Pataray BSN - Ii Conjunctivitis: St. Paul College of Ilocos SurCharina Aubrey100% (2)
- Nursing Care PlanDokumen4 halamanNursing Care PlanKath RubioBelum ada peringkat
- Subdural HematomaDokumen4 halamanSubdural Hematomarodamel gundanBelum ada peringkat
- Nursing Care Plan SeizureDokumen2 halamanNursing Care Plan Seizuretimie_reyes100% (1)
- Nursing Care PlanDokumen23 halamanNursing Care PlanLorielle HernandezBelum ada peringkat
- NCP For ConcussionDokumen3 halamanNCP For Concussiontamtam_antonio100% (1)
- Nursing Care Plan (Bronchiectasis)Dokumen4 halamanNursing Care Plan (Bronchiectasis)Leah QuiñanolaBelum ada peringkat
- HyperthermiaDokumen2 halamanHyperthermiapamgee100% (11)
- Nursing Care PlanDokumen4 halamanNursing Care PlanDewi PurnamasariBelum ada peringkat
- NCP NutritionDokumen2 halamanNCP NutritionBuhkz HermosoBelum ada peringkat
- "May Mga Sugat Ako.": As Verbalized by The PatientDokumen6 halaman"May Mga Sugat Ako.": As Verbalized by The Patientedifier_moonBelum ada peringkat
- Trinidad, Alyssa Angela ADokumen4 halamanTrinidad, Alyssa Angela AAngelaTrinidadBelum ada peringkat
- Case Study: Patient With Appendicitis: Submitted By: Farzaneh Yeganeh Submitted To: Ms. Amara SabriDokumen19 halamanCase Study: Patient With Appendicitis: Submitted By: Farzaneh Yeganeh Submitted To: Ms. Amara Sabrifarzaneh yeganehBelum ada peringkat
- DIABETES Nursing ManagementDokumen11 halamanDIABETES Nursing ManagementKaloy KamaoBelum ada peringkat
- Ambaji Nursing College, Ganeshpura: 2 Year B.Sc. (N) Medical Surgical Nursing-IDokumen2 halamanAmbaji Nursing College, Ganeshpura: 2 Year B.Sc. (N) Medical Surgical Nursing-INEHA PANDEYBelum ada peringkat
- Annex 4 - CXR Voucher Summary ReportDokumen1 halamanAnnex 4 - CXR Voucher Summary ReportAllen ChesterBelum ada peringkat
- Cerebral InfractionDokumen2 halamanCerebral InfractionEdsel MagnoBelum ada peringkat
- Hello Grade 10 Students!: Welcome To The New NormalDokumen26 halamanHello Grade 10 Students!: Welcome To The New NormalLaurice SaquinBelum ada peringkat
- Duodenal UlcerDokumen1 halamanDuodenal UlcerNeferterieManguinaoVillanueva100% (1)
- Chapter 4 Viral Diseases of RuminantsDokumen15 halamanChapter 4 Viral Diseases of RuminantsJAD IMADBelum ada peringkat
- How I Have Experienced The 2020 LockdownDokumen2 halamanHow I Have Experienced The 2020 Lockdown4BFBelum ada peringkat
- Nail Diseases and DisordersDokumen45 halamanNail Diseases and DisordersMariel Balmes HernandezBelum ada peringkat
- Varicose Veins: A Clinical Study: Original Research ArticleDokumen5 halamanVaricose Veins: A Clinical Study: Original Research ArticleAndhika DBelum ada peringkat
- PyuriaDokumen19 halamanPyuriaRia Puji PangestutiBelum ada peringkat
- Epidemiology TriangleDokumen1 halamanEpidemiology TriangleMelDred Cajes BolandoBelum ada peringkat
- CHN NotesDokumen33 halamanCHN NotesErika MarieBelum ada peringkat
- ElephantiasisDokumen7 halamanElephantiasisLucas TobingBelum ada peringkat
- Diaz 2009Dokumen1 halamanDiaz 2009Nasrudin EfendiBelum ada peringkat
- March 2019 Issue of Clinics in Dermatology PDFDokumen71 halamanMarch 2019 Issue of Clinics in Dermatology PDFcuteBelum ada peringkat
- DysarthriachartDokumen6 halamanDysarthriachartapi-494142720Belum ada peringkat
- Drugs For AmebiasisDokumen13 halamanDrugs For AmebiasisDiartha Budi LegawaBelum ada peringkat
- 1.1.1 How To Stop COVID-19 From Coming On BoardDokumen4 halaman1.1.1 How To Stop COVID-19 From Coming On BoardMikee MoganBelum ada peringkat
- Revised RECIST Guideline Version 1.1: What Oncologists Want To Know and What Radiologists Need To KnowDokumen22 halamanRevised RECIST Guideline Version 1.1: What Oncologists Want To Know and What Radiologists Need To KnowSitha MahendrataBelum ada peringkat
- Case-Control Study1Dokumen72 halamanCase-Control Study1Fidya WherrWherrBelum ada peringkat
- COVID-19 Vaccine Breakthrough Case Investigation: Information For Public Health, Clinical, and Reference LaboratoriesDokumen2 halamanCOVID-19 Vaccine Breakthrough Case Investigation: Information For Public Health, Clinical, and Reference LaboratoriesMarcusBelum ada peringkat
- Health Is Wealth. To What Extent Would You AgreeDokumen9 halamanHealth Is Wealth. To What Extent Would You AgreeCharlene ChongBelum ada peringkat
- Bacterial Infections of SkinDokumen72 halamanBacterial Infections of SkinSiddharth DashBelum ada peringkat
- A Rare Case Presentation: Superior Mesenteric Artery SyndromeDokumen1 halamanA Rare Case Presentation: Superior Mesenteric Artery SyndromeKriti KumariBelum ada peringkat
- Background Information - Ebola Virus DiseaseDokumen5 halamanBackground Information - Ebola Virus DiseaseFlabberBelum ada peringkat
- Nhs Covid Pass - Vaccinated: Pfizer/Biontech Covid-19 Vaccine Pfizer/Biontech Covid-19 VaccineDokumen1 halamanNhs Covid Pass - Vaccinated: Pfizer/Biontech Covid-19 Vaccine Pfizer/Biontech Covid-19 VaccineVadim TuscariBelum ada peringkat
- S.N O Nursing Assessmen T Nursing Diagnosis Goal Nursing Intervention Nursing Implementati ON Rationale Evaluati ONDokumen7 halamanS.N O Nursing Assessmen T Nursing Diagnosis Goal Nursing Intervention Nursing Implementati ON Rationale Evaluati ONSimran JosanBelum ada peringkat
- Gendec - 2022-02-05T074422.847Dokumen1 halamanGendec - 2022-02-05T074422.847Robinson llanos ceraBelum ada peringkat
- Necrotizing EnterocolitisDokumen7 halamanNecrotizing EnterocolitisWardah AlAkrahBelum ada peringkat
- Soil Transmitted Helminths: Dr. Madhusudan Swarnkar Professor, Community Medicine, JMC, JhalawarDokumen34 halamanSoil Transmitted Helminths: Dr. Madhusudan Swarnkar Professor, Community Medicine, JMC, Jhalawarmadhusudan swarnkarBelum ada peringkat