Pleural Effusion Secondary To Community Acquired Pneumonia Pathophysiology
Diunggah oleh
Iris CaberteDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Pleural Effusion Secondary To Community Acquired Pneumonia Pathophysiology
Diunggah oleh
Iris CaberteHak Cipta:
Format Tersedia
VII.
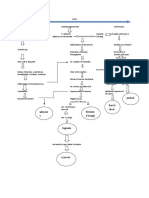
PATHOPHYSIOLOGY PLEURAL EFFUSION SECONDARY TO COMMUNITY ACQUIRED PNEUMONIA Theoretically Based
Non-Modifiable Factors: Extremes of Age: The Very Young The Elderly (60 and Above) Race or Ethnicity: Native Americans Native Alaskans Gender: Male Environmental: Inhalation of foreign materials into the lungs
Modifiable Factors: Lifestyle: Smoking and Alcohol abuse Improper diet causing malnutrition Environmental: Exposure to Pathogens: S. Pneumoniae, H. Influenza, Lagionella, P. Aureginosa, other gram (-) rods and viruses Exposure and inhalation of Secondhand smoke and other chemical pollutants Genetics: The immunocompromised or immunosuppressed patients with low neutrophil count Underlying Diseases: HIV/AIDS Diabetes Mellitus Cardiovascular Diseases Respiratory Diseases: Pulmonary tuberculosis and Chronic Obstructive Pulmonary Disease Medication: Drugs that may cause Respiratory Depression: General Anesthetics, Opioids, Sedatives Drugs that may cause Immunosuppresion: Corticosteroids, Chemotherapeutic Drugs Self-medicating with antibiotics that may cause bacterial/viral resistance: Penicillin, Cephalosporins Others:
Depressed Cough Reflex
Legend: Modifiable and Non-Modifiable Risk Factors Clinical Manifestations/Signs and Symptoms
RACE
AGE
GENDER
ENVIRONMENTAL
LIFESTYLE
GENETICS
UNDERLYING DISEASES
MEDICATION
OTHERS
Native Americans and Native Alaskans
Possible depressed cough and glotic reflex
Male
Highest morbidity and mortality rate
More men smoke than women
Exposure to 2nd hand smoke and other chemical pollutants
Exposure to pathogens:
S. Pneumoniae, H. Influenza, Lagionella, P. Aureginosa, other gram (-) rods and viruses
Excessive alcohol intake and smoking
Improper diet causing
malnutrition
The immunocompromised or immunosuppressed patients with low neutrophil count
HIV/ADIS, DM, CVD, COPD, PTB
Impairment of hosts immune defenses Susceptibility to bacterial invasion
Drugs that may cause Respiratory Depression and Immunosuppression:
General Anesthetics, Opioids, Sedatives, Corticosteroids, chemotherapeutic drugs
Selfmedicating with antibiotics that may cause pathogenic resistance
Decreased cough reflex
Inhalation of foreign materials
Alterations in normal flora
Decreased/Disruption of mucocilliary and macrophage activity
Decreased Immune response or immunesuppression
Aspiration of bacteria in lower respiratory tract Bacterial invasion into the lungs and lower respiratory tract (trachea > bronchus > bronchioles > alveoli) Immune response triggered
Inflammatory response
Lymphocytes produce cytokines WBC
Release of chemical mediators (Histamine, Bradykinin, etc.) Vasodilation and capillary permeability Fluid shifting and edema
Stimulate release of prostaglandin Fever Chills
Release of killer T-Cells, macrophages, phagocytes and anti-bodies
Migration to alveoli Killer T-Cells, macrophages, phagocytes and anti-bodies take effect to pathogens
Purulent exudate formation
Crackles Chest pain Cough with purulent yellowish secretions Dyspnea
Filling of WBC in alveoli and the normally air containing space Exudate/Fluid accumulation in alveoli Partial occlusion of bronchi and alveoli Altered ventilation and diffusion
Decrease oxygen level of blood that passes on the lungs Alveolar O2 tension
Venous blood entering pulmonary circulation passes unventilated area
Ventilation and Perfusion mismatch
Poorly oxygenated blood travels to the left side of the heart
Circulating O2 Arterial hypoxemia Hypoxia Altered Tissue Perfusion Oxygen demand
Hypoventilation Cerebral hypoxia CNS Alterations Headache, dizziness, fatigue, lethargy, restlessness, confusion, irritability, loss of appetite, mood swings
Continuous exudates/fluid accumulation
Pallor Cyanosis
Hemoptysis
Alveolar damage
Alveolar collapse
Pulmonary consolidation
Atelectasis
RBC
Hyperventilation
Heart Rate Pulmonary neutrophilia
Difficulty of breathing and shortness of breath
Use of accessory muscles
Respiratory Rate Apoptosis of other phagocytes
Secondary necrosis of other phagocytes Further damage to other lung parenchyma near the affected part
Inflammation
Permeability of pleural capillary membrane
Altered fluid absorption Pale, Yellow, Cloudy Exudate; Protein; WBC; pH
Accumulation of fluid in pleural space
Irritation of pleural surfaces
Non-productive cough
Protein in Pleural fluid or absent tactile fremitus
Oncotic pressure
Dullness in percussion
Further accumulation of exudates in pleural space
Empyema
Chest pain
> 150-200ml
Flattening or inversion of the diaphragm
Thoracic cavity size and lung size
Mediastinal compression
Compromised cardiac output
Dyspnea
Lung tissue compression
Lung expansion
Ventilation-perfusion mismatch
Arterial hypoxemia
Total lung capacity, functional residual capacity, force vital capacity
Gas-exchange capacity
Difficulty in taking deep breaths
Compromised breathing Shallow breaths Hypoxemia Tachypnea Hypoxia Breath sounds on affected area Unmanaged effusion
Lung compliance
Ventilatory restriction
Atelectasis Source: Focus on Pathophysiology by Bullock and Henze pp253-285 & 572-573 Medical-Surgical Nursing by Brunner and Suddarth pp328330 & 574
Anda mungkin juga menyukai
- Acute Respiratory Distress SyndromeDokumen20 halamanAcute Respiratory Distress SyndromeAngel Cauilan100% (1)
- Shock, Sirs & ModsDokumen37 halamanShock, Sirs & ModsambitioustamannaBelum ada peringkat
- COPD PathoDokumen1 halamanCOPD PathoLeah May AnchetaBelum ada peringkat
- Pathophysiology of PneumoniaDokumen2 halamanPathophysiology of PneumoniaMaria Cristina100% (1)
- IntrapartumDokumen17 halamanIntrapartumIris CaberteBelum ada peringkat
- COPD PathophysiologyDokumen1 halamanCOPD Pathophysiologyaj ajBelum ada peringkat
- Revised Case Report - HemorrhoidsDokumen47 halamanRevised Case Report - Hemorrhoidschristina_love08100% (2)
- CounterclaimDokumen53 halamanCounterclaimTorrentFreak_Belum ada peringkat
- COPD PathophysiologyDokumen1 halamanCOPD PathophysiologyJustin Ahorro-Dionisio33% (3)
- Pathophysiology of CVD InfarctDokumen2 halamanPathophysiology of CVD InfarctIris Caberte86% (7)
- CAP and Hypertension: Predisposing and Precipitating FactorsDokumen5 halamanCAP and Hypertension: Predisposing and Precipitating FactorsLeonaPunzalanBelum ada peringkat
- (Patho) PTB COPDDokumen1 halaman(Patho) PTB COPDKyle HannahBelum ada peringkat
- Pleural Effusion-Individual CPDokumen42 halamanPleural Effusion-Individual CPKristine Mae Sugarol100% (1)
- Chronic Obstructive Pulmonary Disease (COPD)Dokumen32 halamanChronic Obstructive Pulmonary Disease (COPD)matrixtrinityBelum ada peringkat
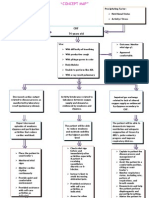
- Iv. Pathophysiology 1. Schematic Diagram Book Based Pathophysiology: Precipitating/Modifiable Factors Non Modifiable / Predisposing FactorsDokumen2 halamanIv. Pathophysiology 1. Schematic Diagram Book Based Pathophysiology: Precipitating/Modifiable Factors Non Modifiable / Predisposing Factorsikemas67% (6)
- Pleural EffusionDokumen1 halamanPleural Effusionarvinian01100% (2)
- Drugs Psych WardDokumen4 halamanDrugs Psych WardIris CaberteBelum ada peringkat
- Pathophysiology of Community Acquired PneumoniaDokumen3 halamanPathophysiology of Community Acquired Pneumoniajordan aguilar67% (3)
- Adopted Child & Foster Parents Case StudyDokumen10 halamanAdopted Child & Foster Parents Case StudyIris Caberte100% (1)
- Pathophysiology of StrokeDokumen3 halamanPathophysiology of StrokeAqeel Al-Mahdaly0% (1)
- Disaster Management Training Program Ethics UNDPDokumen65 halamanDisaster Management Training Program Ethics UNDPTAKI - TAKIBelum ada peringkat
- AntepartumDokumen128 halamanAntepartumIris Caberte100% (1)
- Acute Respiratory FailureDokumen2 halamanAcute Respiratory FailurePaolo Luis MontenegroBelum ada peringkat
- Congestive Heart FailureDokumen19 halamanCongestive Heart FailureIlavenil PanduranganBelum ada peringkat
- FNCP - UtiDokumen1 halamanFNCP - UtiIris Caberte100% (2)
- Pathophysiology of Colon Cancer and Associated ComplicationsDokumen5 halamanPathophysiology of Colon Cancer and Associated ComplicationsKristaMaeC.Lazo0% (3)
- Patho Physiology of Kawasaki DiseaseDokumen2 halamanPatho Physiology of Kawasaki DiseaseIris CaberteBelum ada peringkat
- NP of Acute Calculous CholecystitisDokumen19 halamanNP of Acute Calculous CholecystitisIris Caberte100% (1)
- Dyspnea PresentationDokumen37 halamanDyspnea PresentationamgoperaBelum ada peringkat
- Patho (Lung Cancer)Dokumen1 halamanPatho (Lung Cancer)k.n.e.d.Belum ada peringkat
- Pathophysiology (Chronic Renal Failure)Dokumen3 halamanPathophysiology (Chronic Renal Failure)marshmalou86% (7)
- NCP: DysrhythmiasDokumen12 halamanNCP: DysrhythmiasJavie100% (3)
- Acute Respiratory FailureDokumen29 halamanAcute Respiratory FailurePIYALI BISWASBelum ada peringkat
- Acute Respiratory Failure Pa Tho PhysiologyDokumen4 halamanAcute Respiratory Failure Pa Tho Physiologyroseanne18100% (4)
- ThangkaDokumen8 halamanThangkasifuadrian100% (1)
- Pathophysiology of Tuberculosis Airborne InfectionDokumen2 halamanPathophysiology of Tuberculosis Airborne InfectionRj MagpayoBelum ada peringkat
- Causes and Nursing Care of Pleural EffusionDokumen4 halamanCauses and Nursing Care of Pleural EffusionHania Polangi100% (1)
- Initial Database FNCPDokumen8 halamanInitial Database FNCPIris CaberteBelum ada peringkat
- Family Nursing Care Plan & Community DXDokumen65 halamanFamily Nursing Care Plan & Community DXIris Caberte80% (10)
- Asthma PathophysiologyDokumen4 halamanAsthma PathophysiologyCee SanchezBelum ada peringkat
- Bronchial Asthma PathophysiologyDokumen1 halamanBronchial Asthma PathophysiologyElisa Kerr100% (2)
- Microsoft End-Point ManagerDokumen25 halamanMicrosoft End-Point ManagermaazBelum ada peringkat
- NCP Impaired Gas Exhange CHEST INJURYDokumen4 halamanNCP Impaired Gas Exhange CHEST INJURYMa. Elaine Carla Tating100% (2)
- Nurse Patient InteractionDokumen14 halamanNurse Patient InteractionIris Caberte96% (55)
- Pathophysiology Acute Respiratory FailureDokumen2 halamanPathophysiology Acute Respiratory FailureKimberly Regacho88% (8)
- Pleural Effusion Case StudyDokumen5 halamanPleural Effusion Case Studyjanice ianBelum ada peringkat
- Case Study Pleural EffusionDokumen4 halamanCase Study Pleural EffusionKhristine Anne FabayBelum ada peringkat
- PUD PathophysiologyDokumen1 halamanPUD PathophysiologyHerbert A Serquina100% (1)
- Patho Pleural EffusionDokumen2 halamanPatho Pleural EffusionJess Prodigo50% (2)
- NCP MiDokumen4 halamanNCP MiPitaca Madiam Annabehl PaulBelum ada peringkat
- Shared Psychotic Disorder A Case Study Submitted byDokumen27 halamanShared Psychotic Disorder A Case Study Submitted byChin Lee100% (1)
- Pleural Effusion FdarDokumen1 halamanPleural Effusion FdarvanessabdeveraBelum ada peringkat
- Diarrhea Care PlanDokumen2 halamanDiarrhea Care Planzepoli_zepoly6232100% (1)
- PP - Community-Acquired PneumoniaDokumen1 halamanPP - Community-Acquired Pneumonialpetallo100% (2)
- Concept Map - Abby !Dokumen2 halamanConcept Map - Abby !Abegail Abaygar100% (3)
- NCP and Fdar Wk2 Sarscov-19Dokumen4 halamanNCP and Fdar Wk2 Sarscov-19Jamaica Malicdem0% (1)
- 3 NCP AsthmaDokumen6 halaman3 NCP AsthmajaninenicoleBelum ada peringkat
- Hemorrhagic StrokeDokumen12 halamanHemorrhagic StrokeManggara Surya DharmaBelum ada peringkat
- NCP H MoleDokumen6 halamanNCP H MoleMina RacadioBelum ada peringkat
- Pulmonary HypertensionDokumen26 halamanPulmonary Hypertensionakoeljames8543Belum ada peringkat
- Clinical Physiology of Respiration: Dr. M Qathar RF TDokumen76 halamanClinical Physiology of Respiration: Dr. M Qathar RF TTiwi Lestari TiwiBelum ada peringkat
- Pulmonary Hypertension: An Overview of Causes, Symptoms and DiagnosisDokumen40 halamanPulmonary Hypertension: An Overview of Causes, Symptoms and DiagnosisAlexander Santiago ParelBelum ada peringkat
- Nursing Care for Patients with PneumoniaDokumen44 halamanNursing Care for Patients with PneumoniaFahmi SyarifBelum ada peringkat
- Diagnosing the Cause of BreathlessnessDokumen10 halamanDiagnosing the Cause of BreathlessnessbellinasarsaBelum ada peringkat
- Path o PhysiologyDokumen2 halamanPath o PhysiologyJaessa FelicianoBelum ada peringkat
- Acute Pulmonary Edema: Purwoko Sugeng HDokumen25 halamanAcute Pulmonary Edema: Purwoko Sugeng HBee DanielBelum ada peringkat
- Pulmonary Hypertension GuideDokumen8 halamanPulmonary Hypertension Guidemerin sunilBelum ada peringkat
- DyspneaDokumen6 halamanDyspneaIlyes FerenczBelum ada peringkat
- Ageing and DiseaseDokumen13 halamanAgeing and DiseaseAtharva MehtaBelum ada peringkat
- Hypoxia: Name: Abdalaziz Mostafa No: 1176Dokumen14 halamanHypoxia: Name: Abdalaziz Mostafa No: 11763omar18Belum ada peringkat
- Respiratory Failure Nursing Care and ManagementDokumen19 halamanRespiratory Failure Nursing Care and ManagementYudionoBelum ada peringkat
- Respiratory Failure (Aan) PDFDokumen19 halamanRespiratory Failure (Aan) PDFYudionoBelum ada peringkat
- COPD - Bahan Kuliah Blok 16Dokumen24 halamanCOPD - Bahan Kuliah Blok 16Dermaida SimamoraBelum ada peringkat
- Transfusion Reactions AlphaDokumen27 halamanTransfusion Reactions AlphabeautifulbeastBelum ada peringkat
- 12 RLDDokumen43 halaman12 RLDNur akilaBelum ada peringkat
- Patho Physiology Spinal Cord InjuryDokumen2 halamanPatho Physiology Spinal Cord InjuryIris Caberte100% (1)
- Nursing Process DRUG ABUSEDokumen24 halamanNursing Process DRUG ABUSEIris Caberte0% (1)
- DRUGS Pleural Effusion 2ndary To CAPDokumen6 halamanDRUGS Pleural Effusion 2ndary To CAPIris CaberteBelum ada peringkat
- Right VaricocoelectomyDokumen10 halamanRight VaricocoelectomyIris CaberteBelum ada peringkat
- Theoretical Psycho Pathology FINALDokumen6 halamanTheoretical Psycho Pathology FINALIris CaberteBelum ada peringkat
- NCP Post VaricocoelectomyDokumen4 halamanNCP Post VaricocoelectomyIris CaberteBelum ada peringkat
- Pathology of VaricocoelectomyDokumen2 halamanPathology of VaricocoelectomyIris CaberteBelum ada peringkat
- Drugs Study Post VaricocoelectomyDokumen2 halamanDrugs Study Post VaricocoelectomyIris CaberteBelum ada peringkat
- CVD Infart, Urti, HPNDokumen16 halamanCVD Infart, Urti, HPNIris CaberteBelum ada peringkat
- Drugs Indication Action Side Effect/ Adverse Reaction Nursing Consideration Patient TeachingsDokumen4 halamanDrugs Indication Action Side Effect/ Adverse Reaction Nursing Consideration Patient TeachingsIris CaberteBelum ada peringkat
- NewbornDokumen43 halamanNewbornIris Caberte67% (3)
- Preschooler & Pre AdolescentDokumen35 halamanPreschooler & Pre AdolescentIris CaberteBelum ada peringkat
- SAS HB 06 Weapons ID ch1 PDFDokumen20 halamanSAS HB 06 Weapons ID ch1 PDFChris EfstathiouBelum ada peringkat
- LDN Mun BrgysDokumen8 halamanLDN Mun BrgysNaimah LindaoBelum ada peringkat
- Career Decision-Making Difficulties QuestionnaireDokumen2 halamanCareer Decision-Making Difficulties Questionnaireapi-251146669Belum ada peringkat
- Taxation of XYZ Ltd for 2020Dokumen2 halamanTaxation of XYZ Ltd for 2020zhart1921Belum ada peringkat
- Qustion 2020-Man QB MCQ - MAN-22509 - VI SEME 2019-20Dokumen15 halamanQustion 2020-Man QB MCQ - MAN-22509 - VI SEME 2019-20Raees JamadarBelum ada peringkat
- FinTech BoguraDokumen22 halamanFinTech BoguraMeraj TalukderBelum ada peringkat
- AN ORDINANCE ESTABLISHING THE BARANGAY SPECIAL BENEFIT AND SERVICE IMPROVEMENT SYSTEMDokumen7 halamanAN ORDINANCE ESTABLISHING THE BARANGAY SPECIAL BENEFIT AND SERVICE IMPROVEMENT SYSTEMRomel VillanuevaBelum ada peringkat
- SECTION 26. Registration of Threatened and Exotic Wildlife in The Possession of Private Persons. - NoDokumen5 halamanSECTION 26. Registration of Threatened and Exotic Wildlife in The Possession of Private Persons. - NoAron PanturillaBelum ada peringkat
- Pure TheoryDokumen3 halamanPure TheoryAshima MishraBelum ada peringkat
- Guidelines: For Submitting A Candidature To OrganiseDokumen19 halamanGuidelines: For Submitting A Candidature To OrganiseDan ZoltnerBelum ada peringkat
- Lancaster University: January 2014 ExaminationsDokumen6 halamanLancaster University: January 2014 Examinationswhaza7890% (1)
- Planning Assortments Chapter 12Dokumen34 halamanPlanning Assortments Chapter 12denise_pimentel100% (1)
- How To Become A Hacker - Haibo WuDokumen281 halamanHow To Become A Hacker - Haibo WuAlex de OliveiraBelum ada peringkat
- Senate Hearing, 110TH Congress - The Employee Free Choice Act: Restoring Economic Opportunity For Working FamiliesDokumen83 halamanSenate Hearing, 110TH Congress - The Employee Free Choice Act: Restoring Economic Opportunity For Working FamiliesScribd Government DocsBelum ada peringkat
- Vedic MythologyDokumen4 halamanVedic MythologyDaniel MonteiroBelum ada peringkat
- Chapter 3-Hedging Strategies Using Futures-29.01.2014Dokumen26 halamanChapter 3-Hedging Strategies Using Futures-29.01.2014abaig2011Belum ada peringkat
- Legal Notice: Submitted By: Amit Grover Bba L.LB (H) Section B A3221515130Dokumen9 halamanLegal Notice: Submitted By: Amit Grover Bba L.LB (H) Section B A3221515130Amit GroverBelum ada peringkat
- Introduction to Social Media AnalyticsDokumen26 halamanIntroduction to Social Media AnalyticsDiksha TanejaBelum ada peringkat
- Introduction To The Appian PlatformDokumen13 halamanIntroduction To The Appian PlatformbolillapalidaBelum ada peringkat
- Group 1 - MM - Vanca Digital StrategyDokumen10 halamanGroup 1 - MM - Vanca Digital StrategyAashna Duggal100% (1)
- The Emergence of Provincial PoliticsDokumen367 halamanThe Emergence of Provincial PoliticsHari Madhavan Krishna KumarBelum ada peringkat
- ICPC Members 24 July 2023Dokumen6 halamanICPC Members 24 July 2023Crystal TsangBelum ada peringkat
- List LaguDokumen13 halamanList LaguLuthfi AlbanjariBelum ada peringkat
- MG6863 - ENGINEERING ECONOMICS - Question BankDokumen19 halamanMG6863 - ENGINEERING ECONOMICS - Question BankSRMBALAABelum ada peringkat
- Pension Field Verification FormDokumen1 halamanPension Field Verification FormRaj TejBelum ada peringkat
- AACCSA Journal of Trade and Business V.1 No. 1Dokumen90 halamanAACCSA Journal of Trade and Business V.1 No. 1Peter MuigaiBelum ada peringkat