Part2 Phrgroupfinal
Diunggah oleh
api-106423440Deskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Part2 Phrgroupfinal
Diunggah oleh
api-106423440Hak Cipta:
Format Tersedia
PHR
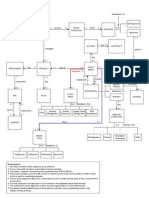
Project Provider ital Behavior Patient V Vital Behavior
Access PHR ttrack daily, and submit weekly to Access PHR, o review patients data and respond whe following: provider t ith any treatment plan adjustments within 24 hours of receipt Daily glucose readings Recovery behaviors: Meds taken oral, insulin) Designate time on s(chedule for PHR catch up work Food intake journal Weekly PHR Team check in meeting Exercise log Recovery behaviors: Family/provider phone or send PHR reminder to send in patient data Send feedback to patient weekly even if no action is needed to provide incentive and support Recovery behaviors: EHR alert for high glucose and when delay in response to paccess PHR Advice and Actions Once a week atient Provide read information and take quiz eport tools to monthly Diabetic panel status r Recovery behaviors: Family to provide weekly reminder Send patients a weekly tip to help keep focus Review lab schedule and make appointment. Go to clinic lab to have HGBA1c test drawn to provide an over time glucose assessment Recovery behaviors: Provider sends patient a weekly reminder to schedule lab appointment; phone call if appointment is missed.
Influence Strategies Influence Strategies
Personal Motivation: Have video of a patient Personal Motivation: Show provider shadow another provider a PHR to model. Personal successfully using using the enter glucose level, Ability: Provide a playground where provider food journal, and exercise log and send to the can practice. Social Motivation: S patient as provider. Personal Ability: Coach taff meeting agenda topic: Use of PHR data in treatment they practice e ntering health information into plans. Social end to provider. S experienced the PHR and sAbility: Pair more ocial user with less experienced user. Structural Motivation: Provider discusses with patient Motivation: Clinic rivacy and shows how the about concerns of pprovides PHR software and education. Structural Ability: Hold 30 ocial provider will manage the information. Sminutes on provider schedule each w create PHR work. Ability: Family helps patient eek for schedule Social Motivation: omfortable settings to where patient is in cProvide support group to learn from each other. Personal Ability: encourage daily tracking. Structural Provide at t Clinic provides software physician Motivation: he elbow support to the and and staff as they i tructural Ability: Provide training for free. Sncorporate PHR tasks into daily workflow. Structural M Help Desk Link for assistance. otivation: Send provider monthly report for all gives Personal Motivation: Provider diabetic patients that he can u or patient to a results of PHR and opportunity fse to compare ccess PHR Actions non-PHR patients. tool for practice. Personal Ability: At provider
Team
Members:
Nicole
Wayne,
Linda
Vind,
Kerry
Heinecke
Challenges
Challenges
Personal:
Personal:
Finding
ime
/
nd
reason
or
reviewing
the
Finding
ttime
areason
for
fentering
daily
glucose
patients
d completion
of
educational
values
and
ata;
may
have
concerns
about
the
accuracy
of
p assessments
atient
data
Possess
technical
knowledge
o
review
t Need
to
be
computer
savvy
to
tenter
data
he
data
and
integrate
nto
c orget
to
enter
electronically;
imay
flinical
care
the
data,
may
Social:
not
understand
Lack
of
shared
eason
for
r with
colleagues
Finding
time
/
rexperience
eviewing
PHR
advice
May
n review
information/take
quiz.
and
to
eed
to
learn
a
new,
shared
care
delivery
approach
instead
of
current
directed
care
model.
Social:
May
need
to
develop
a
new
way
of
communicating/relating
to
patients.
May
want
to
keep
health
condition
private.
Structural:
May
not
have
support
of
family
to
assist
/
Lack
of
technological
tools
ay
require
change
n
reinforce
vital
behaviors;
mavailable
in
order
tio
review
and
r about
t to
healthcare
d data;
n belief
system
espond
he
the
patients
elivery
eed
to
plan
model
potentially
uncompensated
time
into
schedule
for
PHR
review
and
communication
with
patients.
Need
resources
for
maintaining
Structural:
the
technology.
Need
to
have
technological
tools
available
to
enter
their
data
Need
resources
for
maintaining
the
technology
i.e.
battery
backups,
chargers
for
iPhone
or
laptop
Develop
new
way
of
communicating
with
health
provider,
families/friends
PHR
Model
Shift
how
patients
manage
Type
II
diabetes
by
using
integrated
PHR
to
cause
a
10X
increase
in
patient
compliance
as
evidenced
by
reduced
hospital
admission,
increased
success
in
managing
daily
blood
sugar,
improved
test
results
such
asHgbA1C,
decreased
dependence
on
or
eliminate
need
for
meds
Target
Stakeholders:
Patients
with
Type
II
Diabetes,
Primary
Care
Physicians
Key
Metrics:
%
of
diagnostic
tests
within
range,
Patient
and
Provider
Satisfaction
Vital
Behaviors
Metrics:
%
Diagnostic
tests
within
range,
Patient
satisfaction,
Provider
satisfaction
The
Disruptors:
Integration
of
PHR
into
clinical
workflow,
Meaningful
Use.
Social
networking,
PHR
Use
How
Do
We
Know
These
Are
Vital
Behaviors?
Project
HealthDesign
research
shows
that
information
gathered
by
patients
was
more
important
in
determining
treatment
decisions
than
their
official
clinical
medical
record.
It
is
thought
that
sharing
information
with
providers
helped
both
the
provider
and
patient
determine
how
medical
treatments
were
working
and
make
needed
adjustments
in
treatment
to
maintain
health.
To
uncover
Real
Vital
Behaviors,
we
propose
testing
our
assumptions
by
running
a
controlled
pilot
using
our
suggested
vital
behaviors,
suggested
recovery
behaviors
and
monitoring
outcomes.
The
goal
of
the
pilot
will
be
to
find
and
validate
best
practice
vital
behaviors
that
can
be
used
for
successful
patient
and
provider
engagement
to
bring
the
desired
outcomes.
We
believe
costs
would
be
minimal,
as
we
will
pilot
internally
with
2
providers
and
20
patients.
We
would
use
existing
staff
to
support
the
physician/practice
workflows.
We
would
ask
the
provider
to
invest
30
minutes
per
day
to
manage
PHR
work.
We
will
monitor
and
study
the
outcomes
and
then
will
expand
the
pilot
to
a
larger
group
while
we
continue
to
monitor
and
study
the
patient
outcomes.
Metrics
we
would
use
include:
%
of
diagnostic
tests
within
control
ranges,
patient
satisfaction,
and
provider
satisfaction,
number
of
hospital/ED
visits,
number
of
clinic
visits,
and
cost
to
payers
/
patients.
We
will
also
seek
feedback
from
patients
and
provider.
appointment, have patient access the Advice tool and ask a question. Personal Motivation: Send patient a monthly diabetes summary that tracks completion status of patient tasks, glucose trend graph, and most recent HgbA1C. Personal Ability: Show patient how to schedule appointment and create appointment reminder in PHR.
Main
Challenges
Patient
Engagement:
Personal
motivation
-
patient
will
need
to
commit
and
engage
at
level
that
will
make
a
difference
in
health
outcome
Provider
Engagement:
Personal
motivation
-
provider
will
need
to
add
work
that
is
potentially
uncompensated
time
and
will
need
to
connect
the
improved
patient
outcome
to
added
effort
that
will
be
required
Project
References:
1. 2. 3. 1. 2. 3. 4. 5. 6. Influencer
The
Power
to
Change
Anything
Kerry
Patterson,
Joseph
Grenny,
David
Maxfield,
Ron
McMillan,
Al
Switzler,
McGraw- Hill
American
Diabetes
Association.
(2010).
American
Diabetes
Home
Page.
Retrieved
from
http://www.diabetes.org/
Robert
Wood
Johnson
Foundation
(RWJF).
(2010).
Project
HealthDesign.
Retrieved
from
http://www.projecthealthdesign.org/
Robert
Wood
Johnson
Foundation
(RWJF).
(2008).
Design
teams
unveil
innovative
PHR
applications
that
help
people
take
charge
of
their
health.
Retrieved
from
http://www.rwjf.org/pr/product.jsp?id=34528
Robert
Wood
Johnson
Foundation
(RWJF).
(2010).
Retrieved
from
http://rwjfblogs.typepad.com/pioneer/personal-health- records/
Robert
Wood
Johnson
Foundation
(RWJF).
(2010).
Tracking
and
sharing
observations
from
daily
life
could
transform
chronic
care
management.
Retrieved
from
http://www.rwjf.org/pioneer/product.jsp?id=56368
Geisz,
M.
(2010).
Project
HealthDesign:
Rethinking
the
power
and
potential
of
personal
health
records.
Retrieved
from
http://www.rwjf.org/pr/product.jsp?id=69288
\
Early
Experiences
with
Personal
Health
Records,
John
Halamka,
Kenneth
Mandl,
Paul
Tang,
Journal
of
Medical
Informatics
Association,
Volume
15
No
1
Jan/Feb
2008
Integrated
Personal
Health
Records:
Transformative
Tools
for
Consumer
-Centric
Care.
Don
Detmer,
Meryl
Bloomrosen,
Brian
Raymond,
Paul
Tang,
BMC
Medical
Informatics
and
Decision
Making
October
2008
7. 8. 9. 10. 11. 12. 13. 14.
Roundtable Summary Report- Personal Health Records and Electronic Health Reports, Navigating the Intersections, Sponsored by: The Agency for Healthcare Research and Quality, American Medical Informatics Association, Kaiser Permanente Institute for Health Policy, The Robert Wood Johnson Foundation. www.kpihp.org, IHP Institute for Health Policy Ferguson, J. (2009). Can your doctor trust your electronic health data? Retrieved from http://xnet.kp.org/ihp/observations/archive/trustehr.html Potential of electronic personal health records, Claudia Pagliari, Don Detmer, Peter Singleton, BMJ 2007 August BMJ Publishing Group Using Personal Health Records to Improve the Quality of Health Care for Children, Council on Clinical Information Technology, Pediatrics Vol 124 No 1 July 2009 pp 403-409\ Personal Health Records: Definitions, Benefits and Strategies for Overcoming Barriers to Adoption , Paul Tang, Joan S Ash, David Bates, J Marc Overhage, Daniel Sands, Journal of the American Medical Informatics Association Volume 13 Issue 2 JAMIA 2006 The Missing Link: Bridging the Patient-Provider Health Information Gap Paul Tan and David Lansky, Healthaffairs.org A Framework and Approach for Assessing the Value of Personal Health Records (PHRs)Douglas Johnston, David Kaelber, Eric C Pan, Davis Bu, Sapna Shah, Julie Hook, Blackford Middleton, Center for Information Technology Leadership, Partners HealthCare System, Clinical Informatics Research and Development, Partners Healthcare System and Harvard Medical School, Boston MA Implementing EHRs Requires a Shift in Thinking, James Pope, June 2006, Health Management Technology
Anda mungkin juga menyukai
- PHR 3 Draft110610Dokumen2 halamanPHR 3 Draft110610api-106423440Belum ada peringkat
- Part1finaldraft PhrgroupdocDokumen1 halamanPart1finaldraft Phrgroupdocapi-106423440Belum ada peringkat
- Assignmentsession 4Dokumen17 halamanAssignmentsession 4api-106423440Belum ada peringkat
- PHR Story Final - My Journal 11212010 Group SubmissonDokumen2 halamanPHR Story Final - My Journal 11212010 Group Submissonapi-106423440Belum ada peringkat
- Web Experience Request For Proposal-FinalDokumen14 halamanWeb Experience Request For Proposal-Finalapi-106423440Belum ada peringkat
- Final Web Experience Statement of WorkDokumen13 halamanFinal Web Experience Statement of Workapi-106423440Belum ada peringkat
- Group 3 PPT Take2 FinalDokumen24 halamanGroup 3 PPT Take2 Finalapi-106423440Belum ada peringkat
- Medinf406 Su11 Assign2 KerryheineckeDokumen9 halamanMedinf406 Su11 Assign2 Kerryheineckeapi-106423440Belum ada peringkat
- Medication Management For The Elderly Decision Support System (Mmedss)Dokumen25 halamanMedication Management For The Elderly Decision Support System (Mmedss)api-106423440Belum ada peringkat
- Legal and Ethical Issues Arising From Use of Human Implantable RFID ChipsDokumen21 halamanLegal and Ethical Issues Arising From Use of Human Implantable RFID Chipsapi-106423440Belum ada peringkat
- ChicagopressprojectDokumen7 halamanChicagopressprojectapi-106423440Belum ada peringkat
- Kerry Heinecke Med Inf 407 - Group Case Study Project Case Study #1Dokumen6 halamanKerry Heinecke Med Inf 407 - Group Case Study Project Case Study #1api-106423440Belum ada peringkat
- Never Events Board Presentation: Lisa Beckman, Connie Egerer, Kerry HeineckeDokumen30 halamanNever Events Board Presentation: Lisa Beckman, Connie Egerer, Kerry Heineckeapi-106423440Belum ada peringkat
- Heinecke Wan DiagramDokumen1 halamanHeinecke Wan Diagramapi-106423440Belum ada peringkat
- Personal Health Record: Northwestern University MMI 403Dokumen27 halamanPersonal Health Record: Northwestern University MMI 403api-106423440Belum ada peringkat
- Heinecke ProjectphaseiiiDokumen1 halamanHeinecke Projectphaseiiiapi-106423440Belum ada peringkat
- Heinecke ProjectphaseiiDokumen2 halamanHeinecke Projectphaseiiapi-106423440Belum ada peringkat
- Heinecke NetworklegendDokumen1 halamanHeinecke Networklegendapi-106423440Belum ada peringkat
- Heinecke Lan DiagramDokumen3 halamanHeinecke Lan Diagramapi-106423440Belum ada peringkat
- Heinecke SQLDokumen3 halamanHeinecke SQLapi-106423440Belum ada peringkat
- PhaseiDokumen1 halamanPhaseiapi-106423440Belum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- 2 Annexure-IIDokumen297 halaman2 Annexure-IIStanley RoyBelum ada peringkat
- Jam Jim Jam PlanDokumen7 halamanJam Jim Jam PlangrgBelum ada peringkat
- IMNCIDokumen19 halamanIMNCIdocsaurabh777Belum ada peringkat
- Katie Evans - School Counselor Identity StatementDokumen4 halamanKatie Evans - School Counselor Identity Statementapi-469144202Belum ada peringkat
- PLINEJDokumen21 halamanPLINEJMaja KvrgićBelum ada peringkat
- SLP ThesisDokumen9 halamanSLP ThesisbeverlyBelum ada peringkat
- About VALSDokumen3 halamanAbout VALSMara Ioana100% (2)
- School Form 5 (SF 5) Report On Promotion and Progress & AchievementDokumen1 halamanSchool Form 5 (SF 5) Report On Promotion and Progress & AchievementMK TengcoBelum ada peringkat
- Supporting Statements: Do You Find Interesting?Dokumen5 halamanSupporting Statements: Do You Find Interesting?abdul0% (1)
- ENGLISH 102 - PARAPHRASINGDIRECT QUOTATIONDOCUMENTAION (Lucio Hernandez) (Lucio Hernandez)Dokumen33 halamanENGLISH 102 - PARAPHRASINGDIRECT QUOTATIONDOCUMENTAION (Lucio Hernandez) (Lucio Hernandez)ddwererBelum ada peringkat
- Obstetric Team Debriefing Form: Safe Motherhood InitiativeDokumen2 halamanObstetric Team Debriefing Form: Safe Motherhood InitiativeSheinna BarcelonaBelum ada peringkat
- Decimal Operations Study GuideDokumen3 halamanDecimal Operations Study Guideapi-276363929Belum ada peringkat
- Position PaperDokumen12 halamanPosition PaperNona Grace Olmedo IsturisBelum ada peringkat
- Treiman Et Al Knowledge of Letter SoundsDokumen24 halamanTreiman Et Al Knowledge of Letter SoundsEaint Hmu TharBelum ada peringkat
- Tibigar. Performance Task Week 4Dokumen1 halamanTibigar. Performance Task Week 4Grace TibigarBelum ada peringkat
- P. E. Bull - Posture & GestureDokumen190 halamanP. E. Bull - Posture & GestureTomislav FuzulBelum ada peringkat
- Asdfghnm, LDokumen5 halamanAsdfghnm, Lziade roalesBelum ada peringkat
- Stem Activity Lesson PlanDokumen3 halamanStem Activity Lesson Planapi-668801294Belum ada peringkat
- Multielectron Electrode Reaction Kinetics With RDE and RRDE: An Advanced Electrochemical Laboratory ExperimentDokumen6 halamanMultielectron Electrode Reaction Kinetics With RDE and RRDE: An Advanced Electrochemical Laboratory ExperimentLoga NathanBelum ada peringkat
- Evaluation FormDokumen1 halamanEvaluation FormAnnaLiza Rapsing SisonBelum ada peringkat
- LoadRunner Stormrunner-Cloud-DsDokumen4 halamanLoadRunner Stormrunner-Cloud-DsbetapetBelum ada peringkat
- Principles and Applications of Mobile Learning and TechnologiesDokumen20 halamanPrinciples and Applications of Mobile Learning and Technologies117. godlief erwin semuel migeBelum ada peringkat
- Indian Research Papers On ManagementDokumen5 halamanIndian Research Papers On Managementafeaqzhna100% (1)
- JS PROM PscriptDokumen5 halamanJS PROM PscriptSerafinesBelum ada peringkat
- Berkeley'S Active Self: Jonathan DancyDokumen16 halamanBerkeley'S Active Self: Jonathan DancyHayeonBelum ada peringkat
- Usability MetricsDokumen4 halamanUsability MetricsAna Jiménez NúñezBelum ada peringkat
- NCM 57: Health AssessmentDokumen2 halamanNCM 57: Health AssessmentEmvie Loyd Pagunsan-ItableBelum ada peringkat
- Art Therapy DV.280101208Dokumen40 halamanArt Therapy DV.280101208Mas AditBelum ada peringkat
- CV SyaharussajaliDokumen2 halamanCV SyaharussajaliirulBelum ada peringkat
- 002LLI Castillo LTDokumen6 halaman002LLI Castillo LTJohnny AbadBelum ada peringkat