Gastrointestinal System
Diunggah oleh
theglobalnursingHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Gastrointestinal System
Diunggah oleh
theglobalnursingHak Cipta:
Format Tersedia
Medical-Surgical Nursing Gastrointestinal System
Anatomy and Structure of Gastrointestinal System
I. Upper alimentary canal - function for digestion a. Mouth b. Pharynx (throat) c. Esophagus d. Stomach e. 1st half of duodenum II. Middle Alimentary canal Function: for absorption - Complete absorption large intestine a. 2nd half of duodenum b. Jejunum c. Ileum d. 1st half of ascending colon III. Lower Alimentary Canal Function: elimination a. 2nd half of ascending colon b. Transverse c. Descending colon d. Sigmoid e. Rectum IV. Accessory Organ a. Salivary gland b. Verniform appendix c. Liver d. Pancreas auto digestion e. Gallbladder storage of bile Salivary Glands 1. Parotid below & front of ear 2. Sublingual 3. Submaxillary Produces saliva for mechanical digestion 1200 -1500 ml/day - saliva produced
GASTROINTESTINAL SYMPTOMS
1. 2. 3. 4. 5. Nausea and Vomiting Bloating Constipation Diarrhea Abdominal Pain
Disorders of the Gastrointestinal Tract PAROTITIS
mumps inflammation of parotid gland -Paramyxo virus Signs and Symptoms 1. Fever, chills anorexia, gen body malaise 2. Swelling of parotid gland 3. Dysphagia 4. Ear ache otalgia Mode of transmission: Direct transmission & droplet nuclei Incubation period: 14 21 days
Period of communicability 1 week before swelling & immediately when swelling begins. Nursing Management 1. CBR 2. Strict isolation 3. Meds: analgesic Antipyretic Antibiotics to prevent 2 complications 4. Alternate warm & cold compress at affected part 5. Gen liquid to soft diet 6. Complications a. Women cervicitis, vaginitis, oophoritis b. Both sexes meningitis & encephalitis/ reason why antibiotics is needed c. Men orchitis might lead to sterility if it occur during / after puberty
APENDICITIS
inflamation of verniform appendix Predisposing factor 1. Microbial infection 2. Feacalith undigested food particles tomato seeds, guava seeds 3. Intestinal obstruction Signs and Symptoms 1. Pathognomonic sign: (+) rebound tenderness 2. Low grade fever, anorexia, n/v 3. Diarrhea / & or constipation 4. Pain at Rt iliac region 5. Late sign due pain tachycardia Diagnosis 1. CBC mild leukocytosis increase WBC 2. PE (+) rebound tenderness (flex Rt leg, palpate Rt iliac area rebound) 3. Urinalysis Treatment - appendectomy 24 45 Nursing Management 1. Consent 2. Routinary nursing measures: a.) Skin prep b.) NPO c.) Avoid enema lead to rupture of appendix 3. Meds: Antipyretic Antibiotics *Dont give analgesic will mask pain - Presence of pain means appendix has not ruptured. 4. Avoid heat application will rupture appendix. 5. Monitor VS, I&O bowel sound Nursing Management:Post op 1. If (+) to Pendrose drain indicates rupture of appendix Position- affected side to drain 2. Meds: analgesic due post op pain Antibiotics, Antipyretics PRN 3. Monitor VS, I&O, bowel sound 4. Maintain patent IV line 5. Complications- peritonitis, septicemia
LIVER CIRRHOSIS
- lost of architectural design of liver leading to fat necrosis & scarring Early sign hepatic encephalopathy
Asterixis flapping hand tremors Late signs headache, restlessness, disorientation, decrease LOC hepatic coma. Nursing priority assist in mechanical ventilation Predisposing factor: Decrease Laennacs cirrhosis caused by alcoholism 1. Chronic alcoholism 2. Malnutrition decreaseVit B, thiamin - main cause 3. Virus 4. Toxicity- eg. Carbon tetrachloride 5. Use of hepatotoxic agents Signs and Symptoms Early signs: a.) Weakness, fatigue b.) Anorexia, n/v c.) Stomatitis d.) Urine tea color Stool clay color e.) Amenorrhea f.) Decrease sexual urge g.) Loss of pubic, axilla hair h.) Hepatomegaly i.) Jaundice j.) Pruritus or urticaria Late signs 1.Hematological changes all blood cells decrease 1. Leukopenia- decrease 2. Thrombocytopenia- decrease 3. Anemia- decrease 2.Endocrine changes 1. Spider angiomas, Gynecomastia 2. Caput medusate, Palmar errythema 3.GIT changes 1. Ascitis, bleeding esophageal varices due to portal HPN 4.Neurological changes: Hepatic encephalopathy - ammonia (cerebral toxin) Late signs: Headache Fetor hepaticus Confusion Restlessness Decrease LOC Hepatic coma Diagnosis 1,Liver enzymes- increase SGPT (ALT) SGOT (AST) 2.Serum cholesterol & ammonia increase 3.Indirect bilirubin increase 4.CBC - pancytopenia 5.PTT prolonged 6.Hepatic ultrasonogram fat necrosis of liver lobules Nursing Management 1. CBR 2. Restrict Na! 3. Monitor VS, I&O 4. With pt daily & assess pitting edema 5. Measure abdominal girth daily notify MD Early signs: asterexis(flapping hand tremors)
6. 7. 8.
Meticulous skin care Diet increase CHO, vit & minerals. Moderate fats. Decrease CHON Well balanced diet Complications: a.) Ascites fluid in peritoneal cavity Nursing Management 1. Meds: Loop diuretics 10 15 min effect 2. Assist in abdominal paracentesis - aspiration of fluid - Void before paracentesis to prevent accidental puncture of bladder as trochar is inserted b.) Bleeding esophageal varices - Dilation of esophageal veins 1. Meds: Vit K Pitrisin or Vasopresin (IM) 2. NGT decompression- lavage - Give before lavage ice or cold saline solution - Monitor NGT output 3. Assist in mechanical decompression - Insertion of sengstaken-blackemore tube - 3 lumen typed catheter - Scissors at bedside to deflate balloon. Hepatic encephalopathy 1. Assist in mechanical ventilation due coma 2. Monitor VS, neuro check 3. Siderails due restless 4. Meds Laxatives to excrete ammonia
c.)
HEPATITIS
-Inflammation & infection of the liver Hepatitis A Hepa A virus 25 days 2 weeks before onset of jaundice Hepatitis B Hepa B virus 120 days Later part of the incubation period, acute stage Contaminated blood, plasma or semen, placental transmission, contaminated syringe
Causative agent Incubation period Period of communicability
Mode of transmission
ingestion of contaminated water, sexual transmission from oral intercourse
Signs and Symptoms 1. Headache, vomiting 2. Generalized aching 3. Right upper quadrant pain 4. Icteric sclera 5. Generalized jaundice 6. White or gray-colored stool 7. Low-grade fever, sore throat, nasal discharge 8. Dark-colored urine after 3-7 days Nursing Management 1. Maintain a high-caloric diet 2. Strict hand washing & isolation technique 3. Cool bath to reduce discomfort from pruritus 4. Complication: Hepatic coma
PANCREATITIS
acute or chronic inflammation of pancreas leading to pancreatic edema, hemorrhage & necrosis due to auto digestion. Bleeding of pancreas - Cullens sign at umbilicus
Predisposing factors 1. Chronic alcoholism 2. Hepatobilary disease 3. Obesity 4. Hyperlipidemia 5. Hyperparathyroidism 6. Drugs Thiazide diuretics, pills Pentamidine HCL (Pentam) 7. Diet increase saturated fats Signs and Symptoms 1. Severe Left epigastric pain radiates from back & flank area Aggravated by eating, with DOB 2. Nausea/Vomiting 3. Tachycardia 4. Palpitation due to pain 5. Dyspepsia indigestion 6. Decrease bowel sounds 7. (+) Cullens sign - ecchymosis of umbilicus hemorrhage 8. (+) Grey Turners spots ecchymosis of flank area 9. Hypocalcemia Diagnosis 1. 2. 3. Serum amylase & lipase increase Urine lipase increase Serum Ca decrease
Nursing Management 1. Administer Medications as ordered a.) Narcotic analgesic - Meperidine Hcl (Demerol) Dont give Morphine SO4 will cause spasm of sphincter. b.) Smooth muscle relaxant/ anti cholinergic - Ex. Papavarine Hcl Prophantheline Bromide (Profanthene) c.) Vasodilator NTG d.) Antacid Maalox e.) H2 receptor antagonist - Ranitidin (Zantac) f.) Ca gluconate 2. Withold food & fluid because it aggravates pain 3. Assist in Total Parenteral Nutrition (TPN) or hyperalimentation Complications of TPN 1. Infection 2. Embolism 3. Hyperglycemia 4. Institute stress Management technique a.) Deep Breathing Exercise b.) Biofeedback 5. Assist in comfortable position - Knee chest or fetal like position 6. If pt. can tolerate food, give increase CHO, decrease fats, and increase CHON Complications -Chronic hemorrhagic Pancreatitis
CHOLECYSTITIS/ CHOLELITHIASIS
inflammation of gallbladder with gallstone formation. Predisposing factor 1. High risk women 40 years old 2. Post menopausal women undergoing estrogen therapy 3. Obesity 4. Sedentary lifestyle 5. Hyperlipidemia 6. Neoplasm
Signs and Symptoms 1. Severe Right abdominal pain (after eating fatty food). Occurring especially at night 2. Fatty intolerance 3. Anorexia 4. Nausea/vomiting 5. Jaundice 6. Pruritus 7. Easy bruising 8. Tea colored urine 9. Steatorrhea Diagnosis 1. Oral cholecystogram (or gallbladder series)- confirms presence of stones Nursing Management 1. Administer Medications as ordered a.) Narcotic analgesic - Meperdipine Hcl Demerol b.) Anti cholinergic - Atropine SO4 c.) Anti emetic -Phenergan Phenothiazide with anti emetic properties 2. Diet increase CHO, moderate CHON, decrease fats 3. Meticulous skin care 4. Surgery: Cholecystectomy Nursing Management Post Cholecystectomy -Maintain patency of T-tube intact & prevent infection
PEPTIC ULCER DISEASE
excoriation / erosion of submucosa & mucosal lining due to: a.) Hypercecretion of acid pepsin b.) Decrease resistance to mucosal barrier Incidence Rate: 1. Men 40 55 yrs old 2. Aggressive persons Predisposing factors 1. Hereditary 2. Emotional 3. Smoking vasoconstriction GIT ischemia 4. Alcoholism stimulates release of histamine = Parietal cell release Hcl acid = ulceration 5. Caffeine tea, soda, chocolate 6. Irregular diet 7. Rapid eating 8. Ulcerogenic drugs NSAIDS, aspirin, steroids, indomethacin, ibuprofen Indomethacin - S/E corneal cloudiness. Needs annual eye check up. 9. Gastrin producing tumor or gastrinoma Zollinger Ellisons sign 10. Microbial invasion helicobacter pylori. Metromidazole (Flagyl)
Types of ulcers Ascending to severity 1. Acute affects submucosal lining 2. Chronic affects underlying tissue heals & forms a scar According to location 1. Stress ulcer 2. Gastric ulcer 3. Duodenal ulcer most common Stress ulcers common among eritically ill clients
2 Types GASTRIC ULCER Intrum or lesser curvature -30 min 1 hr after eating - epigastrium - gaseous & burning - not usually relieved by food & antacid Normal gastric acid secretion common hematemeis Wt loss a. stomach cause b. hemorrhage 60 years old DUODENAL ULCER Duodenal bulb -2-3 hrs after eating - mid epigastrium - cramping & burning - usually relieved by food & antacid - 12 MN 3am pain Increased gastric acid secretion Not common Melena Wt gain a. perforation 20 years old
SITE PAIN
HYPERSECRETION VOMITING HEMORRHAGE WT COMPLICATIONS HIGH RISK Diagnosis 1. 2. 3. 4.
Endoscopic exam Stool from occult blood Gastric analysis GI series confirms presence of ulceration
Nursing Management 1. Diet bland, non irritating, non spicy 2. Avoid caffeine & milk/ milk products 3. Administer meds as ordered a.) Antacids b.) H2 receptor antagonist 1. Ranitidine (Zantac) 2. Cimetidine (Tagamet) 3. Tamotidine (Pepcid) Avoid smoking decrease effectiveness of drug c.) Cytoprotective agents 1. Sucralfate (Carafate) - Provides a paste like subs that coats mucosal lining of stomach 2. Cytotec d.) Sedatives/ Tranquilizers - Valium, lithium e.)Anticholinergics 1. Atropine SO4 2. Prophantheline Bromide (Profanthene) 4.Surgery: subtotal gastrectomy - Partial removal of stomach Billroth I (Gastroduodenostomy) -Removal of of stomach & anastomoses of gastric stump to the duodenum. Billroth II (Gastrojejunostomy) - removal of -3/4 of stomach & duodenal bulb & anastomostoses of gastric stump to jejunum.
Before surgery for BI or BII - Do vagotomy (severing of vagus nerve) & pyloroplasty (drainage) first. Nursing Management 1. Monitor NGT output a.) Immediately post op should be bright red b.) Within 36- 42h output is yellow green c.) After 42h output is dark red 2. Administer meds: a.) Analgesic b.) Antibiotic c.) Antiemetics 3. Maintain patent IV line 4. VS, I&O & bowel sounds 5. Complications: a.) Hemorrhage hypovolemic shock Late signs anuria b.) Peritonitis c.) Paralytic ileus most feared
d.) e.) f.)
Hypokalemia Thromobphlebitis Pernicious anemia hypovolemia.
Dumping syndrome common complication rapid gastric emptying of hypertonic food solutions CHYME leading to
Signs of Dumping syndrome: 1. Dizziness 2. Diaphoresis 3. Diarrhea 4. Palpitations Nursing Management 1. Avoid fluids in chilled solutions 2. Small frequent feeding s-6 equally divided feedings 3. Diet decrease CHO, moderate fats & CHON 4. Flat on bed 15 -30 minutes after q feeding
Hiatal Hernia
-protrusion (or herniation) of the upper part of the stomach into the thorax through a tear or weakness in the diaphragm Two major kinds a. sliding hiatul hernia b. rolling (or paraesophageal) hiatul hernia Signs and Symptoms 1. dull pains in the chest 2. shortness of breath 3. heart palpitations 4. swallowed food "balling up" and causing discomfort in lower esophagus until it passes on to stomach Risk Factors 1. Heavy lifting or bending over 2. Frequent or hard coughing 3. Hard sneezing 4. Pregnancy and delivery 5. Violent vomiting 6. Straining with constipation 7. Obesity (extra weight pushes down on the abdomen increasing the pressure) 8. Use of the sitting position for defecation 9. Heredity 10. Smoking 11. Drug use, such as cocaine 12. Stress 13. Diaphragm weakness Nursing Intervention 1. 2. 3. Prepare the patient for diagnostic tests, as needed. Administer prescribed antacids and other medications To reduce intra-abdominal pressure and prevent aspiration, have the patient sleep in a reverse Trendelenburg position with the head of the bed elevated. 4. Assess the patients response to treatment. 5. Observe for complications, especially significant bleeding, pulmonary aspiration, or incarceration or streangulation of the herniated stomach portion. 6. After endoscopy, watch for signs of perforation such as falling blood pressure, rapid pulse, shock, and sudden pain caused by endoscope. 7. To enhance compliance, teach the patient about the disorder. Explain significant symptoms, diagnostic tests, and prescribed treatments. 8. Review prescribed medications, explaining their desired actions and possible adverse effects. 9. Teach the patient dietary changes to reduce reflux. 10. Encourage the patient to delay lying down for 2 hours after eating.
Anda mungkin juga menyukai
- Gastrointestinal NursingDokumen8 halamanGastrointestinal Nursingohsnapitslei90% (10)
- GI Study GuideDokumen11 halamanGI Study GuideNursingSchoolNotes75% (4)
- Gastrointestinal System and Nutrition Drug ChartsDokumen3 halamanGastrointestinal System and Nutrition Drug ChartsNursingSchoolNotesBelum ada peringkat
- Gastrointestinal System: Anatomy Physiology &disordersDokumen52 halamanGastrointestinal System: Anatomy Physiology &disordersprabha5050100% (1)
- Fecal Elimination and Urinary EliminationDokumen6 halamanFecal Elimination and Urinary Eliminationincent100% (1)
- Hematological NursingDokumen4 halamanHematological Nursingkhaeydianco100% (5)
- EndocrineDokumen12 halamanEndocrineAna FelBelum ada peringkat
- Alteration in OxygenationDokumen8 halamanAlteration in Oxygenationraquel maniegoBelum ada peringkat
- Physiologic Changes of Aging: System AlterationDokumen1 halamanPhysiologic Changes of Aging: System Alterationshenric16100% (1)
- Cranial Nerves AssessmentDokumen8 halamanCranial Nerves AssessmentTrisha Najial AlmendraBelum ada peringkat
- Hematologic System and DisordersDokumen68 halamanHematologic System and DisordersRellie Castro100% (1)
- Paroxysmal Nocturnal Hemoglobinuria Case StudyDokumen87 halamanParoxysmal Nocturnal Hemoglobinuria Case Studyrachael100% (4)
- Hepatobiliary Disorders: Katrina Saludar Jimenez, R. NDokumen42 halamanHepatobiliary Disorders: Katrina Saludar Jimenez, R. NKatrinaJimenezBelum ada peringkat
- Care of Patient With Musculoskeletal DisordersDokumen3 halamanCare of Patient With Musculoskeletal DisordersBryan Mae H. DegorioBelum ada peringkat
- Renal SystemDokumen65 halamanRenal Systemxarae23Belum ada peringkat
- Fluid & ElectrolytesDokumen6 halamanFluid & ElectrolyteskauragiousBelum ada peringkat
- NERVOUS SYSTEM Communicable Diseases LEPROSYDokumen3 halamanNERVOUS SYSTEM Communicable Diseases LEPROSYFreeNursingNotesBelum ada peringkat
- Gastro Intestinal DisordersDokumen14 halamanGastro Intestinal DisordersJustine Jake L. Ella100% (1)
- Disorders of The Genitourinary SystemDokumen49 halamanDisorders of The Genitourinary SystemYemaya84Belum ada peringkat
- Endocrine Study QuestionsDokumen16 halamanEndocrine Study QuestionsAcjdd143Belum ada peringkat
- Musculoskeletal Note1Dokumen34 halamanMusculoskeletal Note1FreeNursingNotes100% (4)
- Pathology Lecture SeriesDokumen168 halamanPathology Lecture SeriesButch DumdumBelum ada peringkat
- Respiratory System ReviewerDokumen7 halamanRespiratory System ReviewerVictoria Ellex TiomicoBelum ada peringkat
- Endocrine Disorders (Study Notes)Dokumen11 halamanEndocrine Disorders (Study Notes)Danelle Harrison, RN90% (10)
- Cranial NervesDokumen3 halamanCranial Nervesjulialeo100% (1)
- Digestive SystemDokumen117 halamanDigestive SystemKBDBelum ada peringkat
- Gastro Intestinal SystemDokumen9 halamanGastro Intestinal SystemJe Lyn100% (1)
- Respiratory System Upper Respiratory DiseasesDokumen32 halamanRespiratory System Upper Respiratory DiseasesPrince Rener Velasco Pera100% (1)
- Eye DisordersDokumen7 halamanEye DisordersClara De GuzmanBelum ada peringkat
- Gastrointestinal DisordersDokumen27 halamanGastrointestinal DisordersRI NA100% (5)
- Nursing Cardiology: Rebound HypertensionDokumen8 halamanNursing Cardiology: Rebound HypertensionVon R SemillaBelum ada peringkat
- Liver Nursing NotesDokumen7 halamanLiver Nursing NotesHeather ShantaeBelum ada peringkat
- Gastrointestinal Nclex Questions Part 2Dokumen11 halamanGastrointestinal Nclex Questions Part 2Manilyn Delos Reyes Patlunag100% (1)
- Medical Surgical: Nervous SystemDokumen90 halamanMedical Surgical: Nervous SystemCatherine G. Borras100% (1)
- Urinary EliminationDokumen7 halamanUrinary EliminationJeityynnee Tubeo100% (1)
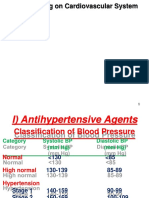
- Drugs Acting On Cardiovascular SystemDokumen18 halamanDrugs Acting On Cardiovascular SystemIbrahem AlBelum ada peringkat
- Human Nervous-SystemDokumen32 halamanHuman Nervous-SystemhwzeeeBelum ada peringkat
- Cardiac SystemDokumen7 halamanCardiac Systemsccctutor100% (3)
- Endocrine DisordersDokumen3 halamanEndocrine DisordersIrish OrleansBelum ada peringkat
- Drug StudyDokumen7 halamanDrug StudyCee-jay SalesBelum ada peringkat
- GI Ch.44-47Dokumen40 halamanGI Ch.44-47W11795800% (1)
- Assessment of Cardiovascular SystemDokumen41 halamanAssessment of Cardiovascular Systembicariato100% (7)
- Urinary System Disorders Practice Quiz #1 (50 Questions)Dokumen26 halamanUrinary System Disorders Practice Quiz #1 (50 Questions)Emy TandinganBelum ada peringkat
- Nursing Management in Abdominal SurgeryDokumen19 halamanNursing Management in Abdominal Surgeryejguy7777100% (2)
- 1538 Exam 4 Cell Reg & GriefDokumen35 halaman1538 Exam 4 Cell Reg & GriefJade EdanoBelum ada peringkat
- Overview of The Digestive SystemDokumen9 halamanOverview of The Digestive SystemMehmet SaylıkBelum ada peringkat
- Transes EndoDokumen20 halamanTranses EndoISABEL REGASPIBelum ada peringkat
- MS4 Midterm NCLEX BurnsDokumen5 halamanMS4 Midterm NCLEX BurnsDebbie Dela Cruz100% (5)
- Anatomy and PhysiologyDokumen4 halamanAnatomy and PhysiologyAaron Jacob Omaña100% (1)
- Endocrine Review NotesDokumen9 halamanEndocrine Review Noteslisette_sakura100% (5)
- HemiplegiaDokumen17 halamanHemiplegiaStefany CelineBelum ada peringkat
- NURS02-Assessment of The Musculoskeletal SystemDokumen129 halamanNURS02-Assessment of The Musculoskeletal SystemAlec AnonBelum ada peringkat
- Fluids and Electrolytes ConceptDokumen31 halamanFluids and Electrolytes ConceptDarwin AndalBelum ada peringkat
- ECG PlacementDokumen2 halamanECG Placementvin_XVIIIBelum ada peringkat
- NCLEX StrokeSeizureDokumen9 halamanNCLEX StrokeSeizureArthur Christopher CorpuzBelum ada peringkat
- BurnsDokumen3 halamanBurnsROBERT C. REÑA, BSN, RN, MAN (ue)67% (3)
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- E. A. D. A.: Gastrointestinal SystemDokumen9 halamanE. A. D. A.: Gastrointestinal SystemDominic ReambonanzaBelum ada peringkat
- Git SystemDokumen16 halamanGit SystemedithlucnasBelum ada peringkat
- Disorders of Cranial NervesDokumen3 halamanDisorders of Cranial Nervestheglobalnursing100% (2)
- Summary Differences Between Dementia and DeliriumDokumen4 halamanSummary Differences Between Dementia and Deliriumtheglobalnursing100% (1)
- Perioperative NursingDokumen12 halamanPerioperative Nursingtheglobalnursing100% (12)
- Major Fluid and Electrolyte ImbalancesDokumen5 halamanMajor Fluid and Electrolyte ImbalancestheglobalnursingBelum ada peringkat
- Common Eye Problems in ChildrenDokumen6 halamanCommon Eye Problems in ChildrentheglobalnursingBelum ada peringkat
- NLE 12-2012 ResultsDokumen359 halamanNLE 12-2012 ResultsPRC Baguio0% (2)
- Congenital Heart DiseasesDokumen6 halamanCongenital Heart Diseasestheglobalnursing100% (2)
- Common Signs and Symptoms of Diseases (Pathognomonic Sign)Dokumen3 halamanCommon Signs and Symptoms of Diseases (Pathognomonic Sign)theglobalnursing91% (11)
- Emergency Management of Patients With Drug OverdoseDokumen6 halamanEmergency Management of Patients With Drug Overdosetheglobalnursing0% (1)
- Respiratory SystemDokumen9 halamanRespiratory Systemtheglobalnursing89% (9)
- Expanded Program On ImmunizationDokumen1 halamanExpanded Program On ImmunizationtheglobalnursingBelum ada peringkat
- Disorders of The Lips, Mouth and GumsDokumen5 halamanDisorders of The Lips, Mouth and GumstheglobalnursingBelum ada peringkat
- Cardiovascular SystemDokumen10 halamanCardiovascular Systemtheglobalnursing75% (4)
- Fundamentals of NursingDokumen44 halamanFundamentals of Nursingtheglobalnursing100% (2)
- Endocrine SystemDokumen8 halamanEndocrine Systemtheglobalnursing80% (5)
- Pyschiatric NursingDokumen40 halamanPyschiatric Nursingtheglobalnursing100% (1)
- Neurologic NursingDokumen14 halamanNeurologic Nursingtheglobalnursing100% (6)
- Musculoskeletal System Nursing ReviewerDokumen11 halamanMusculoskeletal System Nursing Reviewerposh003850% (2)
- Community Health NursingDokumen9 halamanCommunity Health NursingtheglobalnursingBelum ada peringkat
- Maternal and Child NursingDokumen63 halamanMaternal and Child Nursingtheglobalnursing100% (1)
- Normal Microflora of Human BodyDokumen24 halamanNormal Microflora of Human BodyBebu JoshiBelum ada peringkat
- Lic Health Plus FormDokumen27 halamanLic Health Plus FormKuldeep Chakerwarti100% (1)
- Acute Renal FailureDokumen10 halamanAcute Renal FailureSypheruBelum ada peringkat
- Normal Lower Limb Variants in ChildrenDokumen11 halamanNormal Lower Limb Variants in ChildrenIulia MoldovanBelum ada peringkat
- Human Biology 12th Edition Mader Test BankDokumen34 halamanHuman Biology 12th Edition Mader Test Banklaeliacaixpoyf100% (33)
- Renew Life Probiotics Information GuideDokumen69 halamanRenew Life Probiotics Information GuideCameronBelum ada peringkat
- Shared Psychotic Disorder A Case Study Submitted byDokumen27 halamanShared Psychotic Disorder A Case Study Submitted byChin Lee100% (1)
- Dr. Stanley S. BassDokumen6 halamanDr. Stanley S. BassLucian100% (1)
- 112-2 - Heather Bruce - Chapter 3 of Cold DamagesDokumen14 halaman112-2 - Heather Bruce - Chapter 3 of Cold Damagesmudrahora100% (1)
- Study of Histopathological Spectrum of GallbladderDokumen7 halamanStudy of Histopathological Spectrum of GallbladderleartaBelum ada peringkat
- Bio 336 Physio Exam 2 EssaysDokumen3 halamanBio 336 Physio Exam 2 Essayssheila100% (1)
- Drug Study Clindamycin, Ipatropium BromideDokumen8 halamanDrug Study Clindamycin, Ipatropium Bromidepaupaulala100% (2)
- Abg Analysis NotesDokumen32 halamanAbg Analysis Notesakheel ahammedBelum ada peringkat
- Herbal MedicineDokumen6 halamanHerbal MedicineZerlin Duran100% (8)
- Case Study AdimeDokumen1 halamanCase Study Adimeapi-252046756Belum ada peringkat
- Theme 11. Portal HypertentionDokumen33 halamanTheme 11. Portal HypertentionHashmithaBelum ada peringkat
- 1.9 Drug Abuse Prevention and EducationDokumen8 halaman1.9 Drug Abuse Prevention and EducationRiamie Cortes100% (1)
- California Gold Rush TextDokumen105 halamanCalifornia Gold Rush TexttombrodbeckBelum ada peringkat
- Alcohol and Alcohol-Related Problems in Caraka SamhitaDokumen14 halamanAlcohol and Alcohol-Related Problems in Caraka SamhitaAshu SinghBelum ada peringkat
- COMPARISONDokumen30 halamanCOMPARISONandri putraBelum ada peringkat
- Bacterial Sinusitis in Children: AcuteDokumen11 halamanBacterial Sinusitis in Children: AcutefriscahalimBelum ada peringkat
- Academic Texts For Lesson 3Dokumen3 halamanAcademic Texts For Lesson 3Assej Mean Dugat BahanBelum ada peringkat
- First Case of Cutaneous Mycobacteriosis in A Domestic Feline in Southern Brazil ActaVB+v17n3 - 16-19Dokumen4 halamanFirst Case of Cutaneous Mycobacteriosis in A Domestic Feline in Southern Brazil ActaVB+v17n3 - 16-19Ezequiel Davi Dos SantosBelum ada peringkat
- Geriatric Physical TherapyDokumen6 halamanGeriatric Physical Therapyirdasriwahyuni0% (1)
- Topic 5 Nursing Care of The High-Risk Post-Partal ClientsDokumen51 halamanTopic 5 Nursing Care of The High-Risk Post-Partal ClientsMarissa A AquinoBelum ada peringkat
- PfutznerDokumen41 halamanPfutznermina100% (1)
- Acute Kidney Injury and Chronic Kidney DiseaseDokumen44 halamanAcute Kidney Injury and Chronic Kidney DiseaseshihochanBelum ada peringkat
- AnticholinergicDokumen6 halamanAnticholinergicYudi ArBelum ada peringkat
- Broiler Breeder ProductionDokumen7 halamanBroiler Breeder ProductionCamille CarengBelum ada peringkat
- AnatomyDokumen9 halamanAnatomyAnchal LohanaBelum ada peringkat