Angina Pectoris
Diunggah oleh
Hendrix Antonni AmanteDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Angina Pectoris
Diunggah oleh
Hendrix Antonni AmanteHak Cipta:
Format Tersedia
Angina pectoriscommonly known as anginais chest pain due to ischemia of the heart muscle, generally due to obstruction or [1]
spasm of the coronary arteries. The main cause of angina pectoris is Coronary Artery Disease, due to atherosclerosis of the arteries feeding the heart. The term derives from the Latin angina ("infection of the throat") from theGreek ankhon ("strangling"), and the Latin pectus ("chest"), and can therefore be translated as "a strangling feeling in the chest". There is a weak relationship between severity of pain and degree of oxygen deprivation in the heart muscle (i.e., there can be severe pain with little or no risk of a heart attack, and a heart attack can occur without pain). Worsening ("crescendo") angina attacks, sudden-onset angina at rest, and angina lasting more than 15 minutes are symptoms ofunstable angina (usually grouped with similar conditions as the acute coronary syndrome). As these may herald myocardial infarction(a heart attack), they require urgent medical attention and are generally treated as a presumed heart attack.
Classification
Stable angina Also known as effort angina, this refers to the more common understanding of angina related to myocardial ischemia. Typical presentations of stable angina is that of chest discomfort and associated symptoms precipitated by some activity (running, walking, etc.) with minimal or non-existent symptoms at rest. Symptoms typically abate several minutes following cessation of precipitating activities and reoccur when activity resumes. In this way, stable angina may be thought of as being similar to claudication symptoms. Unstable angina Unstable angina (UA) (also "crescendo angina;" this is a form of acute coronary syndrome) is defined as angina pectoris that changes [1] or worsens. It has at least one of these three features: 1. it occurs at rest (or with minimal exertion), usually lasting >10 min; 2. it is severe and of new onset (i.e., within the prior 46 weeks); and/or 3. it occurs with a crescendo pattern (i.e., distinctly more severe, prolonged, or frequent than before). UA may occur unpredictably at rest which may be a serious indicator of an impending heart attack. What differentiates stable angina from unstable angina (other than symptoms) is the pathophysiology of the atherosclerosis. The pathophysiology of unstable angina is the reduction of coronary flow due to transient platelet aggregation on apparently normal endothelium, coronary artery spasms or coronary thrombosis. The process starts with atherosclerosis, and when inflamed leads to an active plaque, which undergoes [4] thrombosis and results in acute ischemia, which finally results in cell necrosis after calcium entry. Studies show that 64% of all unstable anginas occur between 10 PM and 8 AM when patients are at rest. In stable angina, the developing atheroma is protected with a fibrous cap. This cap (atherosclerotic plaque) may rupture in unstable angina, allowing blood clots to precipitate and further decrease the lumen of the coronary vessel. This explains why an unstable angina appears to be independent of activity. Microvascular angina Microvascular Angina or Angina Syndrome X is characterized by angina-like chest pain, but has different causes.The cause of Microvascular Angina is unknown, but it appears to be the result of poor function in the tiny blood vessels of the heart, arms and legs.Since microvascular angina isn't characterized by arterial blockages, it's harder to recognize and diagnose, but its prognosis is excellent.
Signs and symptoms
Most patients with angina complain of chest discomfort rather than actual pain: the discomfort is usually described as a pressure, heaviness, tightness, squeezing, burning, or choking sensation. Apart from chest discomfort, anginal pains may also be experienced in the epigastrium (upper central abdomen), back, neck area, jaw, or shoulders. This is explained by the concept of referred pain, and is due to the spinal level that receives visceral sensation from the heart simultaneously receiving cutaneous sensation from parts of the skin specified by that spinal nerve's dermatome, without an ability to discriminate the two. Typical locations for referred pain are arms (often inner left arm), shoulders, and neck into the jaw. Angina is typically precipitated by exertion or emotional stress. It is exacerbated by having a full stomach and by cold temperatures. Pain may be accompanied by breathlessness, sweating and nausea in some cases. In this case, the pulse rate and the blood pressure increases. Chest pain lasting only a few seconds is normally not angina (such as Precordial catch syndrome). Myocardial ischemia comes about when the myocardia (the heart muscles) receive insufficient blood and oxygen to function normally either because of increased oxygen demand by the myocardia or by decreased supply to the myocardia. This inadequate perfusion of blood and the resulting reduced delivery of oxygen and nutrients is directly correlated to blocked or narrowed blood vessels.
Some experience "autonomic symptoms" (related to increased activity of the autonomic nervous system) such as nausea, vomiting andpallor. Major risk factors for angina include cigarette smoking, diabetes, high cholesterol, high blood pressure, sedentary lifestyle and family history of premature heart disease. A variant form of angina (Prinzmetal's angina) occurs in patients with normal coronary arteries or insignificant atherosclerosis. It is thought to be caused by spasms of the artery. It occurs more in younger women.
Cause
Major risk factors Age ( 55 years for men, 65 for women) Cigarette smoking Diabetes mellitus (DM) Dyslipidemia Family History of premature Cardiovascular Disease (men <55 years, female <65 years old) Hypertension (HTN) Kidney disease (microalbuminuria or GFR<60 mL/min) Obesity (BMI 30 kg/m2) Physical inactivity
Conditions that exacerbate or provoke angina Medications vasodilators excessive thyroid replacement vasoconstrictors polycythemia which thickens the blood causing it to slow its flow through the heart muscle
One study found that smokers with coronary artery disease had a significantly increased level of sympathetic nerve activity when compared to those without. This is in addition to increases in blood pressure, heart rate and peripheral vascular resistance associated with nicotine which may lead to recurrent angina attacks. Additionally, CDC reports that the risk of CHD (Coronary heart disease), stroke, and PVD (Peripheral vascular disease) is reduced within 12 years of smoking cessation. In another study, it was found that after one year, the prevalence of angina in smoking men under 60 after an initial attack was 40% less in those who had quit smoking compared to those who continued. Studies have found that there are short term and long term benefits to smoking cessation.
Diagnosis
Suspect angina in people presenting with tight, dull, or heavy chest discomfort which is: 1. Retrosternal or left-sided, radiating to the left arm, neck, jaw, or back. 2. Associated with exertion or emotional stress and relieved within several minutes by rest. 3. Precipitated by cold weather or a meal. Some people present with atypical symptoms, including breathlessness, nausea, or epigastric discomfort or burping. These atypical [23] symptoms are particularly likely in older people, women, and those with diabetes. Angina pain is not usually sharp or stabbing or influenced by respiration. Anti-acids and simple analgesia do not usually relieve the pain. If chest discomfort (of whatever site) is precipitated by exertion, relieved by rest, and relieved by glyceryl trinitrate, the [23] likelihood of angina is increased. In angina patients who are momentarily not feeling any one chest pain, an electrocardiogram (ECG) is typically normal, unless there have been other cardiac problems in the past. During periods of pain, depression or elevation of the ST segment may be observed. To elicit these changes, an exercise ECG test ("treadmill test") may be performed, during which the patient exercises to their maximum ability before fatigue, breathlessness or, importantly, pain intervenes; if characteristic ECG changes are documented (typically more than 1 mm of flat or downsloping ST depression), the test is considered diagnostic for angina. Even constant monitoring of the blood pressure and the pulse rate can lead us to some conclusion regarding the angina. The exercise test is also useful in looking for other markers of myocardial ischaemia: blood pressure response (or lack thereof, particularly a drop in systolic pressure), dysrhythmia and chronotropic response. Other alternatives to a standard exercise test include a thallium scintigram or sestamibi scintigram (in patients who cannot exercise enough for the purposes of the treadmill tests, e.g., due to asthma or arthritis or in whom the ECG is too abnormal at rest) or Stress Echocardiography.
[23]
In patients in whom such noninvasive testing is diagnostic, a coronary angiogram is typically performed to identify the nature of the coronary lesion, and whether this would be a candidate for angioplasty, coronary artery bypass graft (CABG), treatment only with medication, or other treatments. There has been research which concludes that a frequency is attained when there is increase in the blood pressure and the pulse rate. This frequency varies normally but the range is 4550 kHz for the cardiac arrest or for the heart [clarification needed] failure. In patients who are in hospital with unstable angina (or the newer term of "high risk acute coronary syndromes"), those with resting ischaemic ECG changes or those with raised cardiac enzymes such as troponin may undergo coronary angiography directly.
Treatment
The most specific medicine to treat angina is nitroglycerin. It is a potent vasodilator that makes more oxygen available to the heart muscle. Beta-blockers and calcium channel blockers act to decrease the heart's workload, and thus its requirement for oxygen. Nitroglycerin should not be given if certain inhibitors such as Sildenafil (Viagra), Tadalafil (Cialis), or Vardenafil (Levitra) have been taken within the previous 12 hours as the combination of the two could cause a serious drop in blood pressure. Treatments are balloon angioplasty, in which the balloon is inserted at the end of a catheter and inflated to widen the arterial lumen. Stents to maintain the arterial widening are often used at the same time. Coronary bypass surgery involves bypassing constricted arteries with venous grafts. This is much more invasive than angioplasty. The main goals of treatment in angina pectoris are relief of symptoms, slowing progression of the disease, and reduction of future events, especially heart attacks and death. Beta blockers (e.g., carvedilol, propranolol, atenolol) have a large body of evidence in morbidity and mortality benefits (fewer symptoms, less disability and longer life) and short-acting nitroglycerin medications have been used since 1879 for symptomatic relief of angina. Calcium channel blockers (such as nifedipine (Adalat) and amlodipine), isosorbide mononitrate and nicorandil are vasodilators commonly used in chronic stable angina. A new therapeutic [25] class, called If inhibitor, has recently been made available: ivabradine provides pure heart rate reduction leading to major antiischemic and antianginal efficacy. ACE inhibitors are also vasodilators with both symptomatic and prognostic benefit and, lastly, statins are the most frequently used lipid/cholesterol modifiers which probably also stabilize existing atheromatous plaque. Low-dose aspirindecreases the risk of heart attack in patients with chronic stable angina, and was previously part of standard treatment; however, it has since been discovered that the increase in haemorrhagic stroke and gastrointestinal bleeding offsets this gain so they are no longer advised unless the risk of myocardial infarction is very high. Exercise is also a very good long term treatment for the angina (but only particular regimens - gentle and sustained exercise rather than intense short bursts), probably working by complex mechanisms such as improving blood pressure and promoting coronary artery collateralisation. Identifying and treating risk factors for further coronary heart disease is a priority in patients with angina. This means testing for elevated cholesterol and other fats in the blood, diabetes and hypertension (high blood pressure), and encouraging smoking cessation andweight optimisation. The calcium channel blocker nifedipine prolongs cardiovascular event- and procedure-free survival in patients with coronary artery disease. New overt heart failures were reduced by 29% compared to placebo; however, the mortality rate difference between the [28] two groups was statistically insignificant. The fatty acid oxidation inhibitor mildronate is a clinically-used anti-ischemic drug for the treatment of angina and myocardial infarction Mildronate shifts the myocardial energy metabolism from fatty acid oxidation to the more oxygen sparing glucoseoxidation under ischemic conditions, by inhibiting enzymes in the carnitine biosynthesis pathway including gammabutyrobetaine dioxygenase. Mildronate also inhibits carnitine acetyltransferase and therefore acts as a myocardial energy metabolism regulator.
NCP for ANGINA PECTORIS
Assessment Subjective: My chest hurts and also I feel pain in my jaw, neck, shoulders, and upper extremities. But when I rest, it kinda disappears. I also experience some difficulty in my breathing., as verbalized by the patient. Objective: Facial grimacing, placing fist over midsternum, rubbing left arm, muscle tension, restlessness Autonomic response,( tachycardia, blood pressure changes) Exertional dyspnea Pain level: 8 out of 10
Vital Signs: o o o Diagnosis Acute pain related todecreased myocardial blood flow possibly evidenced by blood pressure, pulse rate changes and increased respiratory rate Pulse rate: 120 bpm BP taken at 4 PM : 130/90, BP taken at 4:15 PM: 140/90 RR: 25 cpm
Planning LTO (Long Term Objective): After 3 days of effective nursing interventions, the patient will demonstrate absence of pain as manifested by :Absence of facial grimace STO (short Term Objective): After 8 hours of of nursing intervention the patient will demonstrate relief of pain from 8 to 3 , decrease pulse rate from 120 bpm to 100 bpm, decreased BP from 140/90 to 120/80 and decrease respratory rate from 25 to 18 cpm.
Intervention Independent Instruct patient to notify nurse immediately when chest pain occurs.
Rationale
Pain and decreased cardiac output may stimulate the sympathetic nervous system to release excessive amounts of norepinephrine, which increases platelet aggregation and release of thromboxane A2. This potent vasoconstrictor causes coronary artery spasm, which can precipitate, complicate, and/or prolong an anginal attack. Unbearable pain may cause vasovagal response, decreasing BP and heart rate.
Assess and document patient response/effects of medication. Provides information about disease progression. Aids in evaluating effectiveness of interventions, and may indicate need for change in therapeutic regimen.
Identify precipitating event, if any; frequency, duration, intensity, and location of pain.
Helps differentiate this chest pain, and aids in evaluating possible progression to unstable angina. (Stable angina usually lasts 315 min and is often relieved by rest and sublingual nitroglycerin (NTG); unstable angina is more intense, occurs unpredictably, may last longer, and is not usually relieved by NTG/rest.)
Observe for associated symptoms, e.g., dyspnea, nausea/vomiting, dizziness, palpitations, desire to micturate.
Decreased cardiac output (which may occur during ischemic myocardial episode) stimulates sympathetic/parasympathetic nervous system, causing a variety of vague sensations that patient may not identify as related to anginal episode.
Evaluate reports of pain in jaw, neck, shoulder, arm, or hand (typically on left side).
Cardiac pain may radiate, e.g., pain is often referred to more superficial sites served by the same spinal cord nerve level.
Place patient at complete rest during anginal episodes.
Reduces myocardial oxygen demand to minimize risk of tissue injury/necrosis. Facilitates gas exchange to decrease hypoxia and resultant shortness of breath. Patients with unstable angina have an increased risk of acute lifethreatening dysrhythmias, which occur in response to ischemic changes and/or stress.
Elevate head of bed if patient is short of breath.
Monitor heart rate/rhythm.
Monitor vital signs every 5 min during initial anginal attack.
Blood pressure may initially rise because of sympathetic stimulation, then fall if cardiac output is compromised. Tachycardia also develops in response to sympathetic stimulation and may be sustained as a compensatory response if cardiac output falls.
Anxiety releases catecholamines, which increase myocardial Stay with patient who is experiencing pain or appears anxious. workload and can escalate/prolong ischemic pain. Presence of nurse can reduce feelings of fear and helplessness. Maintain quiet, comfortable environment; restrict visitors as necessary. Mental/emotional stress increases myocardial workload.
Provide light meals. Have patient rest for 1 hr after meals.
Decreases myocardial workload associated with work of digestion, reducing risk of anginal attack.
Collaborative Provide supplemental oxygen as indicated. Increases oxygen available for myocardial uptake/reversal of ischemia. Nitroglycerin has been the standard for treating and preventing anginal pain for more than 100 yr. Today it is available in many forms and is still the cornerstone of antianginal therapy. Rapid vasodilator effect lasts 1030 min and can be used prophylactically to prevent, as well as abort, anginal attacks. Long-acting preparations are used to prevent recurrences by reducing coronary vasospasms and reducing cardiac workload. May cause headache, dizziness, lightheadednesssymptoms that usually pass quickly. If headache is intolerable, alteration of dose or discontinuation of drug may be necessary. Note: Isordil may be more effective for patients with variant form of angina.
Administer antianginal medication(s) promptly as indicated: Nitroglycerin: sublingual (Nitrostat), buccal, or oral tablets, metered-dose spray; or sublingual isosorbide dinitrate (Isordil) Sustained-release tablets, caplets (Nitrong, Nitrocap T.D.), chewable tablets (Isordil, Sorbitrate), patches, transmucosal ointment (Nitro-Dur, Transderm-Nitro)
Beta-blockers, e.g., acebutolol (Sectral), atenolol (Tenormin), nadolol (Corgard), metroprolol (Lopressor), propranolol (Inderal)
Reduces frequency and severity of attack by producing prolonged/continuous vasodilation.
Calcium channel blockers, e.g., bepridil (Vascor), amlodipine (Norvasc), nifedipine (Procardia), felodipine (Plendil), isradipine (DynaCirc), diltiazem (Cardizem)
Reduces angina by reducing the hearts workload. (Refer to ND: Cardiac Output, risk for decreased, following, p. 000.) Note: Often these drugs alone are sufficient to relieve angina in less severe conditions. Produces relaxation of coronary vascular smooth muscle; dilates coronary arteries; decreases peripheral vascular resistance.
Analgesics, e.g., acetaminophen (Tylenol)
Usually sufficient analgesia for relief of headache caused by dilation of cerebral vessels in response to nitrates. Morphine sulphate (MS) Potent narcotic analgesic may be used in acute onset because of its several beneficial effects, e.g., causes peripheral vasodilation and reduces myocardial workload; has a sedative effect to produce relaxation; interrupts the flow of vasoconstricting catecholamines and thereby effectively relieves severe chest pain. MS is given IV for rapid action and because decreased cardiac output compromises peripheral tissue absorption. Ischemia during anginal attack may cause transient ST segment depression or elevation and T wave inversion. Serial tracings verify ischemic changes, which may disappear when patient is pain-free. They also provide a baseline against which to compare later pattern changes.
Monitor serial ECG changes
Anda mungkin juga menyukai
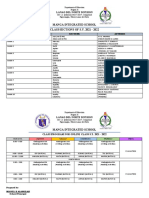
- Manga Integrated Schoo1Dokumen1 halamanManga Integrated Schoo1Hendrix Antonni AmanteBelum ada peringkat
- G10 Science 3rd QTR Exam 2Dokumen2 halamanG10 Science 3rd QTR Exam 2Hendrix Antonni AmanteBelum ada peringkat
- Second Grading MPSDokumen1 halamanSecond Grading MPSHendrix Antonni AmanteBelum ada peringkat
- School StatsDokumen3 halamanSchool StatsHendrix Antonni AmanteBelum ada peringkat
- Manga Is Classes Organized by LDM 2021-2022Dokumen3 halamanManga Is Classes Organized by LDM 2021-2022Hendrix Antonni AmanteBelum ada peringkat
- Marungko Reading Progress ToolDokumen2 halamanMarungko Reading Progress ToolHendrix Antonni AmanteBelum ada peringkat
- 501377-NLCA-2024-List of ExamineesDokumen4 halaman501377-NLCA-2024-List of ExamineesHendrix Antonni AmanteBelum ada peringkat
- 501377-NLCA-2024-List-of-Examinees-7-10-MANGA ISDokumen9 halaman501377-NLCA-2024-List-of-Examinees-7-10-MANGA ISHendrix Antonni AmanteBelum ada peringkat
- TV Broadcast ScriptDokumen2 halamanTV Broadcast ScriptHendrix Antonni AmanteBelum ada peringkat
- School Report Card 2020-2021Dokumen12 halamanSchool Report Card 2020-2021Hendrix Antonni AmanteBelum ada peringkat
- Math 4 DATDokumen4 halamanMath 4 DATHendrix Antonni AmanteBelum ada peringkat
- Medical HistoryDokumen1 halamanMedical HistoryHendrix Antonni AmanteBelum ada peringkat
- Template - Resume (Repaired)Dokumen1 halamanTemplate - Resume (Repaired)hendrixBelum ada peringkat
- Service Credits For BRIGADADokumen6 halamanService Credits For BRIGADAHendrix Antonni AmanteBelum ada peringkat
- Republic of The PhilippinesDokumen2 halamanRepublic of The PhilippinesHendrix Antonni AmanteBelum ada peringkat
- MANGA IS CLASS PROGRAM For S.Y. 2021 - 2022Dokumen6 halamanMANGA IS CLASS PROGRAM For S.Y. 2021 - 2022Hendrix Antonni EnriquezBelum ada peringkat
- IPPDDokumen2 halamanIPPDHendrix Antonni AmanteBelum ada peringkat
- Teachers Profile For EOSY & NLCDokumen2 halamanTeachers Profile For EOSY & NLCHendrix Antonni AmanteBelum ada peringkat
- NLC Action PlanDokumen6 halamanNLC Action PlanHendrix Antonni AmanteBelum ada peringkat
- Annex2-Enriquez, Hendrix Antonni ADokumen9 halamanAnnex2-Enriquez, Hendrix Antonni AHendrix Antonni AmanteBelum ada peringkat
- Report Attendance: Manga Integrated SchoolDokumen2 halamanReport Attendance: Manga Integrated SchoolHendrix Antonni AmanteBelum ada peringkat
- MAIS Identification of Learners For The Learning Delivery ModalityDokumen1 halamanMAIS Identification of Learners For The Learning Delivery ModalityHendrix Antonni AmanteBelum ada peringkat
- SBM Presentation WordDokumen8 halamanSBM Presentation WordHendrix Antonni AmanteBelum ada peringkat
- Budget Consultation DocsDokumen3 halamanBudget Consultation DocsHendrix Antonni AmanteBelum ada peringkat
- Application For Permission To Study: Lanao - Norte@deped - Gov.phDokumen2 halamanApplication For Permission To Study: Lanao - Norte@deped - Gov.phHendrix Antonni AmanteBelum ada peringkat
- Report AttendanceDokumen2 halamanReport AttendanceHendrix Antonni AmanteBelum ada peringkat
- Mais Lac Plan Sy 2021-2022Dokumen3 halamanMais Lac Plan Sy 2021-2022Hendrix Antonni AmanteBelum ada peringkat
- Manga Integrated School: Matrix For Lac Session (November) S.Y. 2021 - 2022Dokumen10 halamanManga Integrated School: Matrix For Lac Session (November) S.Y. 2021 - 2022Hendrix Antonni AmanteBelum ada peringkat
- Cover Design 1Dokumen2 halamanCover Design 1Hendrix Antonni AmanteBelum ada peringkat
- Sec - Wfp-Ppmp-App-Sob-Mdp Fy 2021Dokumen121 halamanSec - Wfp-Ppmp-App-Sob-Mdp Fy 2021Hendrix Antonni AmanteBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- KPJ Healthcare Berhad (NUS ANalyst)Dokumen11 halamanKPJ Healthcare Berhad (NUS ANalyst)noniemoklasBelum ada peringkat
- Higher Vapor Pressure Lower Vapor PressureDokumen10 halamanHigher Vapor Pressure Lower Vapor PressureCatalina PerryBelum ada peringkat
- EQUIP9-Operations-Use Case ChallengeDokumen6 halamanEQUIP9-Operations-Use Case ChallengeTushar ChaudhariBelum ada peringkat
- Know Your TcsDokumen8 halamanKnow Your TcsRocky SinghBelum ada peringkat
- F. Moyra Allen: A Life in Nursing, 1921-1996: Meryn Stuart, R.N., PH.DDokumen9 halamanF. Moyra Allen: A Life in Nursing, 1921-1996: Meryn Stuart, R.N., PH.DRose Nirwana HandayaniBelum ada peringkat
- ASHRAE Final Operating Room 508 PDFDokumen13 halamanASHRAE Final Operating Room 508 PDFSilisteanu AndreiBelum ada peringkat
- Quality Assurance Plan - CivilDokumen11 halamanQuality Assurance Plan - CivilDeviPrasadNathBelum ada peringkat
- LhiannanDokumen6 halamanLhiannanGreybornBelum ada peringkat
- Preboard Practice PDFDokumen25 halamanPreboard Practice PDFGracielle NebresBelum ada peringkat
- Data Mining For Business Analyst AssignmentDokumen9 halamanData Mining For Business Analyst AssignmentNageshwar SinghBelum ada peringkat
- Clock of Destiny Book-1Dokumen46 halamanClock of Destiny Book-1Bass Mcm87% (15)
- Feature Glance - How To Differentiate HoVPN and H-VPNDokumen1 halamanFeature Glance - How To Differentiate HoVPN and H-VPNKroco gameBelum ada peringkat
- Define Variable and ConstantDokumen17 halamanDefine Variable and ConstantSenthil MuruganBelum ada peringkat
- Python Programming Laboratory Manual & Record: Assistant Professor Maya Group of Colleges DehradunDokumen32 halamanPython Programming Laboratory Manual & Record: Assistant Professor Maya Group of Colleges DehradunKingsterz gamingBelum ada peringkat
- PTE Writing FormatDokumen8 halamanPTE Writing FormatpelizBelum ada peringkat
- Matrix CPP CombineDokumen14 halamanMatrix CPP CombineAbhinav PipalBelum ada peringkat
- Sel027 PDFDokumen9 halamanSel027 PDFSmart BiomedicalBelum ada peringkat
- Policy Implementation NotesDokumen17 halamanPolicy Implementation NoteswubeBelum ada peringkat
- Finance 2021 23Dokumen16 halamanFinance 2021 23GAURAV UPADHYAYBelum ada peringkat
- Evaluating Websites A Checklist - JOHN CARLO G. GAERLANDokumen3 halamanEvaluating Websites A Checklist - JOHN CARLO G. GAERLANMarvin CincoBelum ada peringkat
- Project Success - Stakeholders 1 PDFDokumen7 halamanProject Success - Stakeholders 1 PDFMoataz SadaqahBelum ada peringkat
- 1Dokumen14 halaman1Cecille GuillermoBelum ada peringkat
- Submitted By: S.M. Tajuddin Group:245Dokumen18 halamanSubmitted By: S.M. Tajuddin Group:245KhurshidbuyamayumBelum ada peringkat
- Purchasing and Supply Chain Management (The Mcgraw-Hill/Irwin Series in Operations and Decision)Dokumen14 halamanPurchasing and Supply Chain Management (The Mcgraw-Hill/Irwin Series in Operations and Decision)Abd ZouhierBelum ada peringkat
- Ryff's Six-Factor Model of Psychological Well-BeingDokumen7 halamanRyff's Six-Factor Model of Psychological Well-BeingYogi Sastrawan100% (1)
- Sun God NikaDokumen2 halamanSun God NikaElibom DnegelBelum ada peringkat
- Quadratic SDokumen20 halamanQuadratic SAnubastBelum ada peringkat
- Sample Paper Book StandardDokumen24 halamanSample Paper Book StandardArpana GuptaBelum ada peringkat
- Review On Antibiotic Reidues in Animl ProductsDokumen6 halamanReview On Antibiotic Reidues in Animl ProductsMa. Princess LumainBelum ada peringkat
- Vmware It Academy Program May2016Dokumen26 halamanVmware It Academy Program May2016someoneBelum ada peringkat