Procedure Vital Signs Taking
Diunggah oleh
Rency ReynonDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Procedure Vital Signs Taking
Diunggah oleh
Rency ReynonHak Cipta:
Format Tersedia
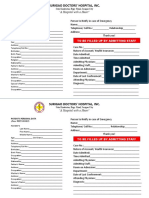
Name:
Date Performed: Shaking Down a Glass Thermometer
Rationale: The material inside the thermometer must be in the correct place for the temperature reading to be accurate and for the thermometer to be ready for the next use. Procedure 1. Assemble equipment. Thermometer in a container. 2. Wash hands. 3. Check the thermometer before using it to make sure that it is not cracked and the bulb is not chipped. 4. Hold the thermometer firmly between fingers and thumb at the stem end farthest from the bulb. 5. Stand clear of any hard surfaces such as counters and tables to avoid striking and breaking the thermometer while shaking it. 6. When youre sure that you have a good hold on the thermometer, shake your hand loosely from the wrist. Do it as youre shaking water from fingers. 7. Snap wrist again and again. This will shake down liquid to the lowest possible point- below the numbers and lines. 8. Always do this before and after using a thermometer. Total Point s 1 1 2 2 2 3 2 2 15 Don e Not Done
Reading a Fahrenheit Thermometer Rationale: Reading a thermometer correctly is an important part of client care. Procedure 1. Using thumb and first 2 fingers, hold the thermometer at the stem. 2. Hold the thermometer at eye level. Turn the thermometer back and forth between fingers until you can clearly see the column of liquid. 3. Notice the scale or calibrations. Each long line stands for 1 degree. 4. There are 4 short lines between each of the long lines. Each short line stands for two tenths (0.20) of a degree. 5. Between the long lines that represent 98 and 99, look for a longer line with an arrow directly beneath it. This special line points out-normal body temperature. 6. Look at the end of the liquid. Notice the line or number where the liquid ends. If it is one of the short lines, notice the previous longer line toward the silver tip that goes into the clients mouth. The temperature reading is the degree marked by that long line plus two-, four-, six-, or eight-tenths of a degree. If the liquid ends on the fourth short line after the 97 line, the temperature is 97.8. If the liquid ends between two lines, use the line closer to Poin ts 1 2 2 2 2 5 Don e Not Done
the silver tip. 7. Write down the clients temperature right away. Follow the method used by your agency. Always indicate if the reading is oral, rectal, or axillary. Total
3 17
Name:
Date Performed: Reading a Centigrade (Celsius) Thermometer
Rationale: Reading a thermometer correctly is an important part of client care. Procedure 1. Using thumb and first 2 fingers, hold the thermometer at the stem. 2. Hold the thermometer at eye level. Turn the thermometer back and forth between fingers until you can clearly see the column of liquid. 3. Notice the scale or calibrations. Each long line stands for 1 degree. 4. There are 9 short lines between each number. These short lines are one-, two-, three-, four-, five-, six-, seven-, eight-, and nine-tenths of a degree. If the liquid ended after the 36.3C. If the liquid ended after the long line 37 and on the eighth short line, the temperature would read 37.8C. If the liquid ends after line 37 on the fifth short line, the temperature would be 37.5C. 5. Write down the clients temperature right away. Follow the method used by your agency. Always indicate if the reading is oral, rectal, or axillary. Total Poin ts 1 2 2 5 Don e Not Done
3 13
Cleaning a Thermometer Rationale: Proper cleaning of a thermometer is an important part of infection control in the home. Procedure 1. Assemble equipment: Thermometer, Tissue and/or cotton balls, Alcohol, Disposable Gloves, waste bag 2. Wash hands and put on gloves. Wipe the thermometer off from the stem to the bulb. Throw away the tissue. 3. Get cotton balls with alcohol. 4. Holding the thermometer, rotate the cotton ball with alcohol around the thermometer from the stem to the bulb. Discard. 5. Get dry cotton ball and repeat the process. Point s 2 5 2 6 3 Don e Not Done
6. Discard the cotton ball.
7. In cleaning thermometer before using it, get a dry cotton ball and wipe the thermometer from bulb to stem. 8. Put the thermometer into a case, bulb first. 9. Dispose of gloves and wash your hands. Total
1 7 2 2 30
Name:
Date Performed: Measuring an Oral Temperature
Rationale: Taking a clients temperature correctly is an important part of client care.
Procedure 1. Assemble equipment: Clean oral thermometer in a case, tissue or paper towel, gloves, pad, pencil, watch 2. Wash hands. 3. Tell the client that you are going to take his/her temperature orally. 4. Ask the client if he/she has recently had hot or cold liquids or if he has smoked. If the answer is yes, wait 10 minutes before taking his temperature. 5. The client should be in bed or sitting in a chair. Do not take a temperature while the client is walking. 6. Take the thermometer out of the container and inspect it for cracks or chips. Do not use it if you see any. 7. Shake the liquid down until it is below the calibrations. 8. Run the thermometer under cool water. This will make the thermometer more pleasant in the clients mouth. 9. Ask the client to lift up his tongue. Place the bulb end of the thermometer without biting it. (If the client cannot close his mouth, take the temperature by another method.) 10. Leave the thermometer in place for 8 minutes. 11. Stay with your client if you think that he cannot keep his mouth closed. (Wear gloves.) 12. Wash hands and put on gloves. Take the thermometer out of the clients mouth. Hold the stem end and wipe the thermometer with a tissue from the stem toward the bulb. 13. Read the thermometer. 14. Record the temperature and your observations concerning the client during this procedure. 15. Shake down the liquid. 16. Clean the thermometer. 17. Make the client comfortable. 18. Remove gloves and wash hands. Total Points 2 2 3 3 3 3 2 2 5 3 3 3 1 1 1 1 1 1 40 Done Not Done
Measuring an Axillary Temperature Rationale: Taking clients temperature correctly is an important part of client care. Procedure
1. 2. 3. Assemble equipment: Oral thermometer in a container, tissue or paper towel, pad, pencil, watch Wash hands. Ask visitors to leave the room, if appropriate.
Point s
2 2 2
Don e
Not Done
4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. Total
Tell the client that you are going to take his temperature by placing a thermometer under his arm. Remove the thermometer from its case and shake down the liquid so that it is below the calibration. Inspect the thermometer for cracks or chips. Do not use it if you see any. Remove the clients arm from sleeve. If the axillary region is moist with the perspiration, pat it dry with a towel. Place the bulb of the oral thermometer in the center of the armpit in an upright position. Put the clients arm across his chest or abdomen. If the client is unconscious or too weak to help, you will have to hold the arm in place. Leave the thermometer in place 10 minutes. Stay with the client. Remove the thermometer. Wipe it off with a tissue from the stem of the bulb. Read the thermometer. Record the temperature and your observations concerning the client during this procedure. Shake the liquid down until its below the calibrations. Clean the thermometer. Replace the thermometer in its case. Make the client comfortable. Wash your hand.
3 2 3 5 4 3 3 5 4 2 2 1 1 1 1 1 47
Name:
Date Performed: Measuring the Radial Pulse
Rationale: Correctly measuring a clients pulse is an important part of care.
Procedure 1. Assemble equipment: Watch with second hand, pad, and pencil 2. Wash hands. 3. Tell the client that you are going to take his pulse. 4. If the client is standing, ask him to sit down. Or have him lying in comfortable position in bed for 5 minutes before you measure the pulse. 5. The clients hand and arm should be well supported and resting comfortably. 6. Find the pulse by placing the tips of your middle three fingers on the palm side of the clients wrist, in line with his thumb directly next to the bone. Press lightly until you feel the beat. When you have found the pulse, notice the rhythm. Note if the beat is steady or irregular. Notice the force of the beat. 7. Look at the position of the second hand on the watch. Start counting the pulse beats until the second hand comes back to the same number on the clock. a. Method A: Count the pulse beats for 1 full minute and report the full-minute count. This is always done if the client has an irregular beat. b. Method B: Count for 30 seconds, until the second hand is opposite its position when started. Then multiply the number of beats by 2. This answer is the number recorded. 8. Record the pulse rate, rhythm, and force immediately. 9. Make the client comfortable. 10. Wash hands. Total Point s 2 2 3 5 3 6 Done Not Done
7 7
3 1 1 40
Measuring the Apical Pulse Rationale: Correctly measuring a clients pulse is important part of care
Procedure 1. Assemble equipment: Stethoscope, antiseptic swabs (cottonballs with alcohol), watch with a second hand, pad and pencil 2. Wash hands. 3. Ask visitors to leave the room, if appropriate. 4. Explain to the client that youre going to take his apical pulse. 5. Clean the earpieces of the stethoscope with antiseptic solution. Put the earpieces facing forward in your ears. 6. Uncover the left side of the clients chest. Avoid overexposing the client. 7. Locate the apex of the clients heart by placing the bell or diaphragm of the stethoscope under the clients left breast. Be sure this is the place you hear the heart beating the loudest. 8. Count the heart sounds for a full minute. 9. Write the full-minute count on the note paper. Also record the rhythm and the quality of the sounds and your observations concerning the client during this procedure. 10. Cover the client and make him comfortable. 11. Clean the earpieces of the stethoscope. Return the equipment to its proper place. 12. Wash hands. Total
Poin ts 2 2 2 3 3 3 10
Don e
Not Done
4 3 2 2 1 37
Name:
Date Performed: Measuring the Apical-Radial Deficit
Rationale: Correctly measuring a clients pulse is an important part of care. Procedure 1. Assemble equipment: Stethoscope, antiseptic swabs, watch with a second hand, pad, pencil 2. Wash hands. 3. Ask visitors to leave the room, if appropriate. 4. Explain to the client that you are going to take his pulse both apically and radially. 5. There are two methods of taking the apical pulse deficit. a. Method A: Two people do the procedure together at the same time. One counts the radial pulse and the other counts the apical pulse for 1 full minute. The difference between the two pulses is known as the apical-radial deficit. b. Method B: The homemaker/home health aide first takes the apical pulse, then the radial pulse. The difference between the two pulses is known as the apical-radial deficit. Because the readings are not taken at the same time, method B is not considered as accurate as method A. 6. Count the apical pulse and the radial pulse for a full minute, and record both figures. Poin ts 2 2 2 3 10 Don e Not Done
10
7. Record the figure for the pulse deficit and the observations concerning the client during the procedure. 8. Make the client comfortable. 9. Clean the equipment and return it to its proper place. 10. Wash hands. Total Measuring Respirations
3 1 1 1 38
Rationale: Correctly measuring a clients respirations is an important part of a clients care. Procedure
1. 2. 3. 4. 5. Assemble equipment: Watch with a second hand, pad, pencil Wash hands. Ask visitors to leave the room, if appropriate. Hold the clients wrist just as if you were taking his pulse. Count the clients respirations, without knowing it, immediately after counting his pulse rate. If the client is a child who has been crying or is restless, wait until he is quiet before counting respirations. If a child is asleep, count his respirations before he wakes up. Always count a childs pulse and respirations before you measure his temperature. One rise and one fall of the clients chest count as one respiration. If you cannot clearly see the chest rise and fall, fold the clients arms across his chest. Then you will feel his breathing as you hold his wrist. Check the position of the second hand on the watch. Count one when you see the clients chest rising as he breathes in. The next time his chest rises, count two. Keep doing this for a full minute. Report the number of respirations you count. You may be permitted to count for 30 seconds. Count the respirations for 30 seconds and then multiply the number you counted by 2. If the clients breathing rhythm is irregular, always count for a full minute. Observe the depth of the breathing while counting the respirations. Immediately write down the number you counted. Note whether the respirations were noisy or labored and your observations concerning the client during this procedure. Make the client comfortable. Wash hands.
Poin ts
2 2 2 10 5
Don e
Not Done
6. 7. 8.
3 5 5
9. 10. 11. 12. 13. 14. Total
3 3 2 2 1 1 46
Name: Measuring Blood Pressure
Date Performed:
Rationale: Correctly measuring a clients blood pressure is an important part of client care.
Procedure 1. Assemble equipment: Sphygmomanometer, stethoscope, antiseptic pad, pad and pencil. 2. Wash hands. 3. Tell the client that you are going to take his blood pressure. 4. Wipe the earpieces of the stethoscope with the antiseptic pad. 5. Have the client resting quietly. He should be either lying down or sitting on a chair. 6. If you are using the mercury apparatus, the measuring scale should be level with your eyes. 7. The clients arm should be bare up to the shoulder or the clients sleeve should be well above the elbow. 8. The clients arm from the elbow down should be resting fully extended on the bed, the arm of the chair, or your hip, well supported, with the palm upward. 9. Unroll the cuff and loosen the valve on the bulb. Then squeeze the compression bag to deflate it completely. Point s 2 2 3 3 3 3 3 4 3 Done Not Done
10.Wrap the cuff snugly and smoothly around the clients arm above the elbow. Do not wrap it so tightly that the client is uncomfortable from the pressure. 11.Leave the area clear where you will place the bell or diaphragm of the stethoscope. 12.Be sure the manometer is in position so you can read the numbers easily. 13.With your fingertips, find the clients brachial pulse at the inner side of the arm above the elbow. Hold the bell or diaphragm there and inflate the cuff until the pulse disappears. Note the reading on the indicator. Quickly deflate the cuff. This is the approximation of the clients systolic reading and is called the palpated systolic pressure. 14.Put the earpiece of the stethoscope into your ears and place the bell or diaphragm of the stethoscope on the brachial pulse. Hold it snugly but not too tightly. Do not let the stethoscope touch the blood pressure cuff. 15.Tighten the thumbscrew of the valve to close it. Turn it clockwise. Be careful not to turn it too tightly. If you do, you will have trouble opening it. 16.Hold the stethoscope in place. Inflate the cuff until the dial points to 30 mm above the palpated systolic pressure. 17.Open the valve counterclockwise. This allows the air to escape. Let it out slowly until the sound of the pulse comes back. A few seconds must go by without sounds. If you do hear pulses sounds immediately, you must stop the procedure. Then completely deflate the cuff. Wait a few seconds. Then inflate the cuff to a much higher calibration above 200. Again, loosen the thumbscrew to let the air out. Listen for a repeated pulse sound. At the same time, watch the indicator. 18.Note the calibration that the pointer passes as you hear the first sound. This point indicates the systolic pressure. 19.Continue releasing the air from the cuff. When the sounds change to a softer and faster thud or disappear, note the calibration. This is the diastolic pressure. 20.Deflate the cuff completely. Remove it from the clients arm. 21.Record your reading on the clients chart. 22.After using the blood pressure cuff, roll it up over the manometer and replace it in the case. 23.Wipe the earpieces of the stethoscope again with an antiseptic swab. Put the stethoscope back in its proper place. 24.Wash hands. 25.Record the blood pressure and your observations concerning the client during the procedure. Total
4 3 2 7
3 3 15
2 5 2 1 2 2 1 1 84
Anda mungkin juga menyukai
- Copar - Ust-ConDokumen5 halamanCopar - Ust-ConEdgarBelum ada peringkat
- NCP FeuDokumen2 halamanNCP FeuFejlean Angelica AntineoBelum ada peringkat
- Case Study FormatDokumen5 halamanCase Study FormatEden OlasabBelum ada peringkat
- NCP PainDokumen4 halamanNCP PainMark Allison BuenaventuraBelum ada peringkat
- Abdomen AssessmentDokumen7 halamanAbdomen Assessmentbi santiagoBelum ada peringkat
- Examination of The Child With CerebralpalsyDokumen52 halamanExamination of The Child With CerebralpalsyRiaz KhanBelum ada peringkat
- Valdez Reflective-Questions PDFDokumen3 halamanValdez Reflective-Questions PDFDexel Lorren ValdezBelum ada peringkat
- Checklist For Physical AssessmentDokumen13 halamanChecklist For Physical AssessmentSharene Kate EribalBelum ada peringkat
- Nursing Progress Notes FINALDokumen2 halamanNursing Progress Notes FINALROXANNE V. LOPEZBelum ada peringkat
- Art Criticism: Discussion, Evaluation, Interpretation, and Analysis of A Work of ArtDokumen8 halamanArt Criticism: Discussion, Evaluation, Interpretation, and Analysis of A Work of ArtMylin Robles LobatonBelum ada peringkat
- ImD-Med L4 (Immunization)Dokumen33 halamanImD-Med L4 (Immunization)VancopBelum ada peringkat
- Health History Format BlankDokumen32 halamanHealth History Format BlankRich-Anne LagarasBelum ada peringkat
- Philippine Health AgendaDokumen9 halamanPhilippine Health AgendaCzeazarBelum ada peringkat
- Thoracentesis Reflective EssayDokumen2 halamanThoracentesis Reflective EssayAnjae GariandoBelum ada peringkat
- Postmortem Care: Rigor MortisDokumen2 halamanPostmortem Care: Rigor Mortisqwerty24Belum ada peringkat
- Gynecologist Career EssayDokumen4 halamanGynecologist Career Essayapi-531232390Belum ada peringkat
- Industrial AnalysisDokumen12 halamanIndustrial AnalysisFazal KhadimBelum ada peringkat
- UNIT 6 The Nursing Role in Supporting The Health of Ill Children and Their FamiliesDokumen5 halamanUNIT 6 The Nursing Role in Supporting The Health of Ill Children and Their FamiliesStephanie LeeBelum ada peringkat
- Nursing InterventionsDokumen18 halamanNursing InterventionsMark BellBelum ada peringkat
- NCP DiarrheaDokumen2 halamanNCP DiarrheaPrincess Xzmae RamirezBelum ada peringkat
- NCPDokumen3 halamanNCPErica Denice CastilloBelum ada peringkat
- Steps Rationale: Respiratory RateDokumen2 halamanSteps Rationale: Respiratory RateChubs RiegoBelum ada peringkat
- Acute Pain (AGE) NCPDokumen1 halamanAcute Pain (AGE) NCPMike SoySauce LibrojoBelum ada peringkat
- Assignment For Oxy. Online BasedDokumen5 halamanAssignment For Oxy. Online BasedNurhassem Nor AkangBelum ada peringkat
- CHN - Written ReportDokumen3 halamanCHN - Written ReportJastine DiazBelum ada peringkat
- PRC Form (Minor Operation)Dokumen1 halamanPRC Form (Minor Operation)mawelBelum ada peringkat
- Republic ActDokumen36 halamanRepublic ActjanBelum ada peringkat
- FNCPDokumen48 halamanFNCPYvette SadacBelum ada peringkat
- NCP RiskDokumen2 halamanNCP RiskNorries Jonell CaballarBelum ada peringkat
- Dbe and Cough TCPDokumen3 halamanDbe and Cough TCPBeverlyBelum ada peringkat
- Cues Diagnosis Background Knowledge Planning Intervention Rationale EvaluationDokumen2 halamanCues Diagnosis Background Knowledge Planning Intervention Rationale EvaluationhaniehaehaeBelum ada peringkat
- Activity IntoleranceDokumen1 halamanActivity IntoleranceAndrea Francesca SantosBelum ada peringkat
- SeizuresDokumen2 halamanSeizureskaythe08Belum ada peringkat
- NCP Cavernous Sinus ThrombosisDokumen3 halamanNCP Cavernous Sinus ThrombosisVencel Mae Famas Villahermosa50% (2)
- History of Present IllnessDokumen1 halamanHistory of Present IllnessMenly SusadaBelum ada peringkat
- NCP Acute PainDokumen2 halamanNCP Acute PainLyka Mae DominguezBelum ada peringkat
- Ppe4 Reflection AssignmentDokumen11 halamanPpe4 Reflection Assignmentapi-318846856100% (1)
- Pb-Research-1 1 EditedDokumen20 halamanPb-Research-1 1 EditedDianne Mae DagaBelum ada peringkat
- Buddy WorksDokumen3 halamanBuddy WorksJamaica Leslie NovenoBelum ada peringkat
- Assessment Diagnosis Intervention Rationale EvaluationDokumen11 halamanAssessment Diagnosis Intervention Rationale EvaluationBenjie DimayacyacBelum ada peringkat
- Scribd 020922 Case Study-Oncology A&kDokumen2 halamanScribd 020922 Case Study-Oncology A&kKellie DBelum ada peringkat
- Think Critically and AnswerDokumen3 halamanThink Critically and AnswerSareno PJhēaBelum ada peringkat
- NCM 112 Computation 2021Dokumen3 halamanNCM 112 Computation 2021Marie Kelsey Acena Macaraig100% (1)
- Student Nurses' Community Nursing Care PlanDokumen3 halamanStudent Nurses' Community Nursing Care PlanMussaib MushtaqBelum ada peringkat
- AnxietyDokumen3 halamanAnxietyJenny Pearl Pasal100% (1)
- Assisting IV BTDokumen89 halamanAssisting IV BTmhelshy villanuevaBelum ada peringkat
- Assessmen T Diagnosis Planning Intervention Rationale EvaluationDokumen3 halamanAssessmen T Diagnosis Planning Intervention Rationale EvaluationJoric MagusaraBelum ada peringkat
- Fever: What Is A Fever?Dokumen2 halamanFever: What Is A Fever?Sheikh ZakirBelum ada peringkat
- Gordon S 11 Functional Health PatternsDokumen6 halamanGordon S 11 Functional Health PatternsMrs RehanBelum ada peringkat
- Community Health Nursing ReflectionDokumen4 halamanCommunity Health Nursing ReflectionLuis WashingtonBelum ada peringkat
- Manguiat, Reyes Head and Neck AssessmentDokumen4 halamanManguiat, Reyes Head and Neck AssessmentCiara Manguiat100% (1)
- Patient Personal Data FormDokumen1 halamanPatient Personal Data FormGerald TalledoBelum ada peringkat
- Colchicine DosageDokumen6 halamanColchicine DosageHam SotheaBelum ada peringkat
- NURSING CARE PLAN - Risk For Fluid Volume DeficitDokumen2 halamanNURSING CARE PLAN - Risk For Fluid Volume DeficitDaniel Andre S. SomorayBelum ada peringkat
- III. Nursing Care Plan Nursing Priority No. 1: Ineffective Airway Clearance Related To Excessive Accumulation of Secretions Secondary To PneumoniaDokumen6 halamanIII. Nursing Care Plan Nursing Priority No. 1: Ineffective Airway Clearance Related To Excessive Accumulation of Secretions Secondary To PneumoniaRae Marie Aquino100% (1)
- Assessment Diagnosis Planning Intervention Rationale EvaluationDokumen2 halamanAssessment Diagnosis Planning Intervention Rationale EvaluationJustine Mae A. LoriaBelum ada peringkat
- Community Teaching Plan and Evaluation Submission, Assignment Week 6Dokumen10 halamanCommunity Teaching Plan and Evaluation Submission, Assignment Week 6taniaBelum ada peringkat
- Nursing Care For Patients With LungDokumen14 halamanNursing Care For Patients With LungAyu RahayuniBelum ada peringkat
- Handwashing QuestionsDokumen2 halamanHandwashing Questionsknicky FranciscoBelum ada peringkat
- Vital Signs 2024Dokumen50 halamanVital Signs 2024gntawfeqBelum ada peringkat
- EffectiveTeaching Full ManualDokumen340 halamanEffectiveTeaching Full ManualHabtamu AdimasuBelum ada peringkat
- Revised Week 3Dokumen61 halamanRevised Week 3John Teo DalisaymoBelum ada peringkat
- Botswana Ref Ranges PaperDokumen7 halamanBotswana Ref Ranges PaperMunyaradzi MangwendezaBelum ada peringkat
- Dentistry Indonesia, 20 (1), 5-8.: Daftar PustakaDokumen6 halamanDentistry Indonesia, 20 (1), 5-8.: Daftar PustakaSari RahayuniBelum ada peringkat
- The Girl With Green Eyes by John EscottDokumen10 halamanThe Girl With Green Eyes by John EscottAyman Charoui essamadiBelum ada peringkat
- CNS Stimulants PDFDokumen7 halamanCNS Stimulants PDFZehra AmirBelum ada peringkat
- The Real Music IndustryDokumen201 halamanThe Real Music IndustryStephenGladstone100% (11)
- Preschooler Development by Age and DomainDokumen8 halamanPreschooler Development by Age and DomainThoa KimBelum ada peringkat
- ResumeDokumen2 halamanResumeapi-281248740Belum ada peringkat
- Toolbox Talk 9: Critical Risks - ExcavationsDokumen2 halamanToolbox Talk 9: Critical Risks - ExcavationsPravin GowardunBelum ada peringkat
- CLC - Good Copy Capstone ProposalDokumen6 halamanCLC - Good Copy Capstone Proposalapi-549337583Belum ada peringkat
- HBN 00-09 Infection ControlDokumen47 halamanHBN 00-09 Infection ControlAntenehBelum ada peringkat
- h2s Hand BookDokumen34 halamanh2s Hand BookJorge Eliecer Ferro Cotes100% (4)
- High Times - November 2023Dokumen84 halamanHigh Times - November 2023miwoga7814Belum ada peringkat
- Altius Annual Leave Policy Wef 1st January 2012 Ver 1.1Dokumen11 halamanAltius Annual Leave Policy Wef 1st January 2012 Ver 1.1Mudassar HakimBelum ada peringkat
- Princess Mae S. ArellanoDokumen2 halamanPrincess Mae S. ArellanoPrincess Mae ArellanoBelum ada peringkat
- 978 3 642 25446 8Dokumen166 halaman978 3 642 25446 8Gv IIITBelum ada peringkat
- Burdock Root AeroponicDokumen8 halamanBurdock Root AeroponicNelson RiddleBelum ada peringkat
- Group Activity 1 - BAFF MatrixDokumen1 halamanGroup Activity 1 - BAFF MatrixGreechiane LongoriaBelum ada peringkat
- (Norma) Guia Fda CovidDokumen14 halaman(Norma) Guia Fda CovidJhovanaBelum ada peringkat
- VKC CertificateDokumen1 halamanVKC CertificateDigital Seva KendraBelum ada peringkat
- Anaemia in Pregnancy: Dr. Lama MehaisenDokumen11 halamanAnaemia in Pregnancy: Dr. Lama MehaisenWendy EvansBelum ada peringkat
- Satvik DietDokumen3 halamanSatvik DietDisha TBelum ada peringkat
- Cleaning Reusable Medical DevicesDokumen12 halamanCleaning Reusable Medical DevicesDavid Olamendi ColinBelum ada peringkat
- Top 10 Regulatory Challenges in The Healthcare EnvironmentDokumen3 halamanTop 10 Regulatory Challenges in The Healthcare EnvironmentNicki BombezaBelum ada peringkat
- Human Factors and Safety Culture in Maritime Safety (Revised)Dokumen10 halamanHuman Factors and Safety Culture in Maritime Safety (Revised)Al-aayan D. IsmaelBelum ada peringkat
- Industrial SafetyDokumen5 halamanIndustrial Safetykamujula reddyBelum ada peringkat
- Body GuideDokumen46 halamanBody GuideBárbara Leite95% (22)
- Citations Issued Due To COVID-19Dokumen726 halamanCitations Issued Due To COVID-19Maritza NunezBelum ada peringkat
- Psych 7A FinalDokumen16 halamanPsych 7A FinalMatthew Kim100% (1)