The
Diunggah oleh
Bhaktha SinghDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
The
Diunggah oleh
Bhaktha SinghHak Cipta:
Format Tersedia
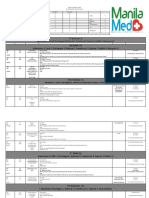
Group Mediclaim Insurance Program FAQs - Parent
Q1: What is the definition of Hospital/Nursing Home? A: Hospital/Nursing Home, means any institution in India established for indoor care and treatment of sickness and injuries and which has been registered either as a hospital or Nursing Home with the local authorities and is under the supervision of registered and qualified medical practitioner OR Should comply with minimum criteria as under: It should have atleast 15 inpatient beds. Fully equipped Operation Theatre of its own wherever surgical operations is carried out. Fully qualified nursing staff under its employment round the clock. Fully qualified doctor(s) should be in charge round the clock. The term, `Hospital/Nursing Home, shall not include an establishment, which is a place of rest, a place for the aged, a place for drug addiction or place of alcoholics, a hotel or a similar place. Q2: Is there any time limit for Hospitalisation? A: Yes, The admissible minimum period of hospitalization is 24 hours. However, this time limit is not applied to specific treatments i.e. Dialysis, Chemotherapy, Radiotherapy, Eye Surgery, Dental Surgery, Lithotripsy (Kidney Stone removal), D&C, Tosillectomy taken in the Hospital/Nursing Home and the Insured is discharged on the same day. Q3: Are Pre and Post Hospitalisation expenses covered? A: Yes, all relevant medical expenses incurred during a period upto 30 days prior to and 60 days after hospitalization on disease/illness/injury sustained will be considered as part of claim. Q4: What are the diseases/illness that are excluded from the Program? A: Broadly the following diseases/illness/situations are not covered: Injury or disease directly or indirectly caused by or arising from or attributable to War Invasion Act or Foreign Enemy Warlike operations (whether war be declared or not). Circumcision unless necessary for treatment or a disease not excluded hereunder or as may be necessitated due to an accident. Vaccination or inoculation or change of life or cosmetic or aesthetic treatment of any description, plastic surgery other than as my be necessitated due to as accident or as part of any illness. The Cost of Spectacles and contact lenses hearing aids are not reimbursable. Dental treatment or surgery of any kind unless arising due to an accident and requiring hospitalization. Convalescence general debility Run Down condition or rest cure, congenital external disease or defects or anomalies, sterility, venereal disease, intentional self-injury and use of intoxicating drugs/alcohol. AIDS.
Naturopathy treatment and all other diseases /illness/situations as explained in the Insurance policy. Refer policy document for more details.
Q5: What is the time frame within which the Claim has to be submitted? A: The claim must be filed within 75 days from date of discharge from the Hospital in case of post hospitalization and 15 days for normal hospitalization. Q6. What are the documents that are required to be submitted? A: Following are the documents that are required to be submitted: Claim form: All original Bills, receipts and Discharge Summary/Certificate/Card from the Hospital. Cash Memos from the Hospital/Chemist(s), supported by the proper prescription, investigation reports etc,. Q7: Is the claims applicable to those Hospitalisation expenses incurred abroad ? A: No, the Program covers only those Hospitalisation expenses that are incurred in India. Q8: What does Immediate Family floater cover mean? A: Immediate family Floater indicates the total sum insured for your family (as declared by you) within a given year. The same can be either claimed entirely by one member or shared within the family upto the maximum limit. Q9: What is the maximum amount allowable under the Maternity benefit? A: Not applicable under this program Q10: Is there an age limit to cover any dependents under this program? A: For any new entrants into this program the upper age limit is 80. There is no minimum age limit. Please note that the upper age limit does not apply for those who joined the program prior to attaining the age of 80. Q11: Can I include my parents/ parents in law under the Program during the course of the year? A: In case you have got married during the course of the year, you can include only your parents in law into the policy. Please note this has to be done within 45 days of the date of marriage and the same time as including your spouse. Parents cannot be added to the policy during the course of the year. Q12: Can I include other relatives/friends under this Scheme, by personally paying the premium amount? A: No, this program is only limited to 4 members - parents & parents in law. Q13: Will I be reimbursed all the expenses that I incurred during hospitalization? A: The following expenses can be reimbursed as per Insurance policy norm: Room, Boarding Expenses as provided by the Hospital/Nursing Home. Nursing Expenses, Surgeon, Anesthetist, Medical Practitioner, Consultants Specials fees
Anesthesia, Blood, Oxygen, OT Charges, Surgical appliances, Medicines, Drugs Diagnostic material and X-Ray, Dialysis, Chemotherapy, Radiotherapy, Cost of pacemaker, artificial limbs, cost of organs and similar expenses.
Q14: Can I get the coverage amount enhanced by paying extra premium? A: Yes you can opt for additional sum insured by paying additional premium as per section 6.4 in the policy document. Q15: I am a heart patient. Can I claim hospitalization expenses under this program? A: Yes, this illness is covered within the permissible pre existing disease/illness. Q16: Is there a waiting period before I can make a claim? A: No. Q17: My mother has diabetes, blood pressure and heart problems. I got admitted for angioplasty. Investigations for related problems of diabetes were done. Can I claim the investigation costs as I was admitted for a heart problem? A: Yes, you can. You will need to produce a letter/prescription from the doctor prescribing the tests. Q18: My father has been advised to undergo an operation for defective nasal septum. I also wanted to have plastic surgery done on my nose. Are expenses for the same reimbursable? A: Hospitalization costs for the operation performed for defective nasal septum is claimable under the program. In this case though plastic surgery is not covered. Q19: My mother in law has been advised to undergo a kidney organ transplant. Can I claim the cost of the organ? A: Yes. Provided the organ is already available at the hospital. Q20: My father in law has been advised to undergo kidney dialysis every week. He will not be hospitalized. Can I claim the expenses incurred under this program? A: Yes. Q21: My father is currently on special medication for reducing my weight. Can I claim the expenses incurred under this program? A: No. Q22: I have paid for the hospitalization expenses in foreign currency. Will the insurance company reimburse the equivalent amount in rupees to me? A: Even if the amount paid is in foreign currency, the bill receipt should be in Indian rupees for the same to be claimed from the insurer. Q23: In case of separation, can I continue to avail the benefit by paying the premium directly to the insurance company?
A: Yes, you may continue this benefit even once you leave the organization by converting it to a retail plan and paying the premium for the same. For more details on this, raise a Contact HR query. Q24: My father in law was hospitalized for heart ailment and passed away. Are the costs involved for the treatment claimable under the program in case the member expires? A: Yes, the expense incurred is claimable under the insurance program by the employee/nominee. Q23: My mother needs to travel to Mumbai for a Kidney transplant. Is my airfare reimbursable? A: No. Q24: What is co-pay ? A:Co-pay means out of the entire payable amount 90% will be borne by the insurance company and 10% will be borne by the employee. This co-pay is only for the basic sum Insured and not applicable on the buffer amount sanctioned/utilized. Example If the Sum Insured is Rs. 1 lakh and the claim amount is Rs.80,000/- insurance company will pay Rs.72,000/- and employee will bear Rs.8,000/-. If the claim amount is Rs. 1,10,000/- and Rs.10,000/- is granted from buffer, then insurance company will pay Rs.1,00,000/- i.e., Rs.90,000/- out of sum insured and Rs.10,000/- (without applying co-pay on buffer), i.e., totally Rs.1,00,000/-. And If the claim amount is Rs.2,00,000/- and Rs 1,00,000/- is granted out of buffer, then the insurance company will pay Rs.1,90,000/- i.e., Rs.90,000/- out of sum insured and Rs.1,00,000/- out of buffer and employee will bear Rs.10,000/-. The balance sum insured after applying co-pay remains for subsequent claims, if any. For Eg. Sum Insured-Rs.1,00,000/-, Claim for 1,00,000/-. Balance Rs.10,000/- would be available for next claim, if any. However on this also if and when a claim is received, co-pay of 10% is applicable. For Eg if the claim is for Rs.10,000/- Rs 1000 has to be borne by the employee. FAQs on MediAssist Services Q1: What is MediAssist? A: We have partnered with MediAssist who are healthcare services provider. At their empanelled hospitals you need not pay for hospitalisation expenses as they provide you with a credit facility. Q2: How do I enroll for MediAssistservices? A: You would need to fill the form available @ HP HR portal under Employee Resources >> Compensation/ Benefits >> Benefits Summary >> Health/ Medical Q3: Is a MediAssist card a necessity? A: Yes. Q4: Which are the empanelled hospitals, where cashless facility is available? A: The updated list of empanelled hospitals is available with the MediAssist representative or Log on to www.mediassistindia.com
Q5: Do I need to visit only MediAssist-empanelled hospitals? A: No, though it is preferred to use the MediAssist empanelled hospitals as you can avail the credit facility and discounts. Employees can still go to any other hospital, pay for the hospitalization expenses and have the same reimbursed with the help of MediAssist. Q6: Is Outpatient treatment like common cold, asthma etc covered at the hospital? A: No. Outpatient treatment at the hospital is not covered under the program. The expenses incurred have to be claimed under the company medical program as mentioned under the FBP. Q7: What do I do in case of a planned hospitalisation at an empanelled hospital? A: You would need to fill a pre-authorisation form(available with MediAssist). The preauthorisation form includes details of the patient, hospital and estimated expenses. On receiving the pre-authorisation form, MediAssist would issue an authorisation letter to the hospital. Thereafter, the patient shows the MediAssist card and gets admitted at the hospital. No upfront security deposit is required. At the time of discharge, the patient needs to ensure to sign the bill. You would not need to pay for any of the expenses covered under the program. Any auxiliary expenses (not covered under the program) like telephone calls would be charged to you. You would need to sign on an insurance claim form at the time of discharge. All relevant documents should be handed over to MediAssist. Q8: What do I do in case of an emergency hospitalisation? A: In the case of an emergency, the employee or his/her dependents can undergo hospitalization without the pre-authorization letter from MediAssist. Empanelled hospitals have been instructed to admit the patient under emergency with only the photo-ID card. MediAssist should be contacted in order to avoid paying at the time of discharge. In case it is a non-empanelled hospital, MediAssist will help the employee settle the bill at the time of discharge in case the employee is in trauma or is no position to make arrangements for the money.
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Monitoring & Remediation: © 2018, Amazon Web Services, Inc. or Its Affiliates. All Rights ReservedDokumen21 halamanMonitoring & Remediation: © 2018, Amazon Web Services, Inc. or Its Affiliates. All Rights ReservedBhaktha SinghBelum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- One World Flutes - SDokumen3 halamanOne World Flutes - SBhaktha SinghBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- Session 08 - Intro To M ProgrammingDokumen57 halamanSession 08 - Intro To M ProgrammingBhaktha SinghBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- 2 Lab1 Build Secure Web AppDokumen49 halaman2 Lab1 Build Secure Web AppBhaktha SinghBelum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- DR Daniel Soper Database l2Dokumen41 halamanDR Daniel Soper Database l2Bhaktha SinghBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- MB200.1 M1L5T1 Practice Lab - Creating An AppDokumen5 halamanMB200.1 M1L5T1 Practice Lab - Creating An AppBhaktha SinghBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Keyboard Shortcuts Windows Vs CodeDokumen1 halamanKeyboard Shortcuts Windows Vs Codeenescu.alin1429Belum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- AWS Best PracticesDokumen27 halamanAWS Best PracticesBhaktha SinghBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- HTML CSS Content1Dokumen4 halamanHTML CSS Content1Bhaktha SinghBelum ada peringkat
- MB200.1 M1L3T1 Practice Lab - Set Up EnvironmentDokumen3 halamanMB200.1 M1L3T1 Practice Lab - Set Up EnvironmentBhaktha SinghBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- MB200.1 M3L4T1 Practice Lab - Modifying FormsDokumen4 halamanMB200.1 M3L4T1 Practice Lab - Modifying FormsBhaktha SinghBelum ada peringkat
- Its A Shared Leadership World: Contributed by Don FrederiksenDokumen5 halamanIts A Shared Leadership World: Contributed by Don FrederiksenBhaktha SinghBelum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- MB200.1 M3L8T1 Practice Lab - Building Charts PDFDokumen3 halamanMB200.1 M3L8T1 Practice Lab - Building Charts PDFBhaktha SinghBelum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- MB200.1 M2L6T1 Practice Lab - Additional Entity OptionsDokumen3 halamanMB200.1 M2L6T1 Practice Lab - Additional Entity OptionsBhaktha SinghBelum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Keyboard Shortcuts Windows Vs CodeDokumen1 halamanKeyboard Shortcuts Windows Vs Codeenescu.alin1429Belum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- CAPM (PMBOK 5) Exam Prep Notes Project Management Risk Management PDFDokumen1 halamanCAPM (PMBOK 5) Exam Prep Notes Project Management Risk Management PDFBhaktha Singh0% (1)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- One World Flutes - SDokumen3 halamanOne World Flutes - SBhaktha SinghBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- Gonzato 2015 Lowtechwhistle PDFDokumen33 halamanGonzato 2015 Lowtechwhistle PDFLucian SirbuBelum ada peringkat
- Scert +2 EnglishDokumen35 halamanScert +2 EnglishsujasundarBelum ada peringkat
- Passive VoiceDokumen43 halamanPassive VoiceFernandaBecerra0% (1)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Systematic Problem Solving: Mind Maps and Problem Solving ToolsDokumen24 halamanSystematic Problem Solving: Mind Maps and Problem Solving Toolsthomasteepe50% (2)
- Oil GasDokumen12 halamanOil GasBhaktha SinghBelum ada peringkat
- PDFDokumen43 halamanPDFKeerthi KrishnanBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Determine RsDokumen22 halamanDetermine RsFatimah Humaira KhalidBelum ada peringkat
- Business Advanced Grammar TestDokumen4 halamanBusiness Advanced Grammar TestTijana Doberšek Ex Živković100% (1)
- Grammar Test1Dokumen11 halamanGrammar Test1Bhaktha SinghBelum ada peringkat
- 8 Types of NounsDokumen7 halaman8 Types of NounsNoneth Padillo BeldoroBelum ada peringkat
- Databases Course Book PDFDokumen44 halamanDatabases Course Book PDFBhaktha Singh100% (1)
- APMF Submission to Inquiry into Definition of CharitiesDokumen18 halamanAPMF Submission to Inquiry into Definition of CharitiesBhaktha SinghBelum ada peringkat
- North WindDokumen14 halamanNorth WindurcoadsBelum ada peringkat
- 10.6 Health Issues Related To The Human Circulatory SystemDokumen7 halaman10.6 Health Issues Related To The Human Circulatory SystemrynBelum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- The Function of Vitamins and Mineral in Hair LossDokumen2 halamanThe Function of Vitamins and Mineral in Hair LossDian AcilBelum ada peringkat
- Census August 8 - August 9, 2020Dokumen6 halamanCensus August 8 - August 9, 2020Patrick JohnBelum ada peringkat
- Influenza: CausesDokumen2 halamanInfluenza: CausesMaui ShihtzuBelum ada peringkat
- Slides 6 - ObturationDokumen22 halamanSlides 6 - Obturationبراءة أحمد السلاماتBelum ada peringkat
- Laboratory Tests for Hemostasis EvaluationDokumen5 halamanLaboratory Tests for Hemostasis EvaluationCMLBelum ada peringkat
- Pathophysiology of Respiratory Diseases: Obstructed AlveoliDokumen3 halamanPathophysiology of Respiratory Diseases: Obstructed AlveoliApril Dianne ParungaoBelum ada peringkat
- Mustang Track Loader Mtl25 Service Manual 908313 RevcDokumen23 halamanMustang Track Loader Mtl25 Service Manual 908313 Revcnicoleorr110382okaBelum ada peringkat
- Could A Disease Have Caused The Accusations - Is It Possible That The Girls Had Contracted An IllnessDokumen3 halamanCould A Disease Have Caused The Accusations - Is It Possible That The Girls Had Contracted An IllnessESTHER OGODOBelum ada peringkat
- Answers To Questions:: Analysis of SalivaDokumen2 halamanAnswers To Questions:: Analysis of Salivaerisseval14Belum ada peringkat
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Organ Transplantatio1Dokumen26 halamanOrgan Transplantatio1Bindashboy0Belum ada peringkat
- Causes, Signs, and Treatment of HyponatremiaDokumen65 halamanCauses, Signs, and Treatment of HyponatremiaFaryalBalochBelum ada peringkat
- Introduction and Basic Principles: Dr. K. S. Abbasi Department of Food Tech/Human NutritionDokumen8 halamanIntroduction and Basic Principles: Dr. K. S. Abbasi Department of Food Tech/Human Nutritionnouman ashrafBelum ada peringkat
- Health and Social Care Inequalities: The Impact of COVID-19 On People Experiencing Homelessness in BrazilDokumen13 halamanHealth and Social Care Inequalities: The Impact of COVID-19 On People Experiencing Homelessness in BrazilcinacchiBelum ada peringkat
- COVID-19 Dummy ReportDokumen2 halamanCOVID-19 Dummy ReportVirat DaineBelum ada peringkat
- Elderly Hip FractureDokumen9 halamanElderly Hip FractureIlyes FerenczBelum ada peringkat
- Understanding Contraceptive Knowledge and Practices Among Breastfeeding WomenDokumen286 halamanUnderstanding Contraceptive Knowledge and Practices Among Breastfeeding WomenAastha JainBelum ada peringkat
- A Pain Education ProgrammeDokumen13 halamanA Pain Education Programmeapi-244230664Belum ada peringkat
- ABO Incompatible Platelets: Risks Versus Benefit: ReviewDokumen5 halamanABO Incompatible Platelets: Risks Versus Benefit: Reviewmy accountBelum ada peringkat
- TRIUMPHANT COLLEGE COVID-19 TRAINING NewDokumen26 halamanTRIUMPHANT COLLEGE COVID-19 TRAINING NewDaniellaBelum ada peringkat
- Nat Ag Winter Wheat in N Europe by Marc BonfilsDokumen5 halamanNat Ag Winter Wheat in N Europe by Marc BonfilsOrto di CartaBelum ada peringkat
- Cervical Cancer Screening and Occurrence TrendsDokumen109 halamanCervical Cancer Screening and Occurrence TrendsVincent eneBelum ada peringkat
- Nutritional Care in Respiratory Disease: DR Haerani Rasyid, Mkes, SPPD, K-GHDokumen94 halamanNutritional Care in Respiratory Disease: DR Haerani Rasyid, Mkes, SPPD, K-GHDesywinBelum ada peringkat
- Fundamentals of Nursing10-19Dokumen19 halamanFundamentals of Nursing10-19escolarBelum ada peringkat
- Heart Disease Course PDALongDokumen84 halamanHeart Disease Course PDALongArpanpatelBelum ada peringkat
- Vocational Rehabilitation Programs for People with DisabilitiesDokumen44 halamanVocational Rehabilitation Programs for People with DisabilitiesKannappa Shetty MudiyanuruBelum ada peringkat
- Tumor Detection Through Mri Brain Images: Rohit Arya 20MCS1009Dokumen25 halamanTumor Detection Through Mri Brain Images: Rohit Arya 20MCS1009Rohit AryaBelum ada peringkat
- Covid-19 Info DriveDokumen61 halamanCovid-19 Info DriveMac MacapilBelum ada peringkat
- Protozoa Tugas 1Dokumen5 halamanProtozoa Tugas 1De shila syailinda maulidaBelum ada peringkat
- Patient Rights and the Doctor-Patient RelationshipDokumen39 halamanPatient Rights and the Doctor-Patient RelationshipAhmad Yani NoorBelum ada peringkat
- An Architect's Guide to Construction: Tales from the Trenches Book 1Dari EverandAn Architect's Guide to Construction: Tales from the Trenches Book 1Belum ada peringkat
- Markup & Profit: A Contractor's Guide, RevisitedDari EverandMarkup & Profit: A Contractor's Guide, RevisitedPenilaian: 5 dari 5 bintang5/5 (11)
- A Place of My Own: The Architecture of DaydreamsDari EverandA Place of My Own: The Architecture of DaydreamsPenilaian: 4 dari 5 bintang4/5 (241)
- The Complete Guide to Alternative Home Building Materials & Methods: Including Sod, Compressed Earth, Plaster, Straw, Beer Cans, Bottles, Cordwood, and Many Other Low Cost MaterialsDari EverandThe Complete Guide to Alternative Home Building Materials & Methods: Including Sod, Compressed Earth, Plaster, Straw, Beer Cans, Bottles, Cordwood, and Many Other Low Cost MaterialsPenilaian: 4.5 dari 5 bintang4.5/5 (6)
- The E-Myth Contractor: Why Most Contractors' Businesses Don't Work and What to Do About ItDari EverandThe E-Myth Contractor: Why Most Contractors' Businesses Don't Work and What to Do About ItPenilaian: 4 dari 5 bintang4/5 (16)
- Practical Guides to Testing and Commissioning of Mechanical, Electrical and Plumbing (Mep) InstallationsDari EverandPractical Guides to Testing and Commissioning of Mechanical, Electrical and Plumbing (Mep) InstallationsPenilaian: 3.5 dari 5 bintang3.5/5 (3)
- Pressure Vessels: Design, Formulas, Codes, and Interview Questions & Answers ExplainedDari EverandPressure Vessels: Design, Formulas, Codes, and Interview Questions & Answers ExplainedPenilaian: 5 dari 5 bintang5/5 (1)
- Piping and Pipeline Calculations Manual: Construction, Design Fabrication and ExaminationDari EverandPiping and Pipeline Calculations Manual: Construction, Design Fabrication and ExaminationPenilaian: 4 dari 5 bintang4/5 (18)
- Building Construction Technology: A Useful Guide - Part 1Dari EverandBuilding Construction Technology: A Useful Guide - Part 1Penilaian: 4 dari 5 bintang4/5 (3)