The Spread of Klebsiella Pneumoniae Carbapenemases: A Tale of Strains, Plasmids, and Transposons
Diunggah oleh
Mohammad K AlshomraniDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
The Spread of Klebsiella Pneumoniae Carbapenemases: A Tale of Strains, Plasmids, and Transposons
Diunggah oleh
Mohammad K AlshomraniHak Cipta:
Format Tersedia
E D I T O R I A L C O M M E N TA R Y
The Spread of Klebsiella pneumoniae Carbapenemases: A Tale of Strains, Plasmids, and Transposons
L. Silvia Munoz-Price1,2 and John P. Quinn3
1
Division of Infectious Diseases, University of Miami, and 2Jackson Memorial Hospital, Miami, Florida; and 3Pzer Global Research and Development, Groton, Connecticut
(See the brief report by Sidjabat et al, on pages 17368.)
Downloaded from cid.oxfordjournals.org by guest on February 27, 2011
Carbapenemases are a large and diverse family of microbial enzymes that hydrolyze not only carbapenems but also other b-lactams, with the occasional exception of monobactams, such as aztreonam. For clinicians, the nomenclature of carbapenemases, like that of other b-lactamases, is confusing. In keeping with other b-lactamases, carbapenemases can be classied on the basis of function or structure. The most commonly used classicationAmbleris based on molecular structure. In this classication, carbapenemases may belong to classes A, B, or D [1]. Class A and D are serine carbapenemases, meaning that they have a serine at their active sites, like extended spectrum b-lactamases (ESBLs). In contrast, the class B enzymes are known as metallo-b-lactamases, because they require zinc as a cofactor [1]. Although the metalloenzymes were rst described in the early 1990s, mostly in Pseudomonas aeruginosa, they remain uncommon in the United States [1]. A more recent arrival seems to pose a greater
Received 23 August 2009; accepted 24 August 2009; electronically published 27 October 2009. Reprints or correspondence: Dr John P. Quinn, 50 Pequot Avenue, MS 6025-B3122, New London, CT 06320 (john.p.quinn@pzer.com). Clinical Infectious Diseases 2009; 49:173941 2009 by the Infectious Diseases Society of America. All rights reserved. 1058-4838/2009/4911-0019$15.00 DOI: 10.1086/648078
threat. Klebsiella pneumoniae carbapenemases (KPCs) of molecular class A have become the most frequently found carbapenemase in the United States [2]. First isolated in 1996 from a patient in North Carolina, over the past 5 years, KPCs have spread across the East coast of the United States and are now considered endemic in certain areas of New York and New Jersey [3]. Furthermore, clonal expansion has been recently described, with ST 258 being the predominant strain in 70% of all US KPC-producing K. pneumoniae isolates received by the Centers for Disease Control and Prevention [4]. Since 2005, outbreaks have occurred all over the world, including Israel, Colombia, Greece, France, India, Norway, Sweden, China, Puerto Rico, Argentina, and Brazil [2]. Intercontinental travel has been directly linked with the spread of KPCs. The rst KPC producer identied outside the United States was isolated from a patient at a French hospital who had received previous care in New York City [5]. Similarly, KPC-3producing K. pneumoniae in Israel was found to be genetically linked to a US strain, which suggested intercontinental transfer of strains as the most likely etiology [6]. KPC variants are subclassied on the basis of single amino-acid mutations that expand from KPC-1 up to the recently described KPC-10 [7]. The most com-
monly reported variants in the United States are KPC-2 and KPC-3, which are clinically and microbiologically quite similar [4]. KPCs acquired their name because they were rst detected in K. pneumoniae, and this is still the species most likely to harbor them. However, they are now widely disseminated in other enterics, such as Escherichia coli, Enterobacter species, Serratia species, Morganella morganii, Citrobacter freundii, Salmonella enterica, and Klebsiella oxytoca [2]. More disturbingly, KPCs have been identied in nonfermenters, such as P. aeruginosa and Pseudomonas putida [2], where they typically cause a much higher degree of resistance because of the additional contribution of diminished outer membrane permeability. KPC genes are typically located on mobile genetic elements, especially a particular transposon known as Tn4401, which facilitates transfer between plasmids and across bacterial species [8, 9]. Tn4401 and related transposons have been detected in many species from different continents. Genes encoding other b-lactamases (eg, TEM and SHV class ESBLs) have been detected within Tn4401 [8]. In fact, most KPC producers carry multiple additional b-lactamases; in one case, 7 unique enzymes were detected [10]. Furthermore, Tn4401 has been found to be associated with genes conferring resistance to non b-lactams, such as plasmid-mediated re-
EDITORIAL COMMENTARY CID 2009:49 (1 December) 1739
sistance to quinolones (qnr) and aminoglycosides [2]. As expected, the accumulation of this formidable array of resistance genes produces a multidrug-resistant phenotype. In this edition of Clinical Infectious Diseases, Sidjabat et al [11] elegantly describe the sequential transfer of KPC-3 among 3 different gram-negative species; this occurred in a single patient with a prolonged and complicated hospital stay. Molecular data suggest that the gene transferred from K. pneumoniae to E. coli occurred because of a Tn4401 recombination event and then spread to Serratia marscescens on a plasmid. This illustrates the various routes by which KPC genes can spread between species. There are previous reports that describe 11 organism expressing identical KPCs in the same patient, presumably reecting the same phenomenon. In Texas, KPC-2producing Enterobacter species and P. putida were identied in a liver transplant recipient [12]. Similarly, KPC2producing E. coli and Enterobacter species were reported in a patient with a psoas abscess treated at a French hospital who had been recently discharged from an Israeli health care facility [13]. KPC enzymes may be difcult to detect, because they only cause weak hydrolysis of carbapenems. As a result, automated systems of clinical microbiology laboratories can erroneously report imipenem or meropenem as susceptible in up to 52% of isolates [2]. Phenotypically, ertapenem resistance is the most useful characteristic to screen for KPC production [1]; resistant enterics should then undergo either a modied Hodge test or a boronic acid screening test and, if results are positive, a conrmatory polymerase chain reaction [1, 2]. Molecular conrmation is necessary, because ertapenem resistance in enterics is commonly conferred by unrelated mechanisms, such as the combination of porin loss, production of other b-lactamases (such as AmpCs or CTX-M), and upregulation of efux pumps. KPC-producing organisms are clinically
important because of the limited treatment options available and a high crude mortality rate. Most strains are susceptible only to colistin or tigecycline. There are very limited data to support either of these. Tigecycline achieves low serum levels and probably should not be used in bloodstream infections [14], and colistin can cause nephrotoxicity in up to 20% of patients [15]. Despite the lack of controlled studies, some clinicians combine agents using either tigecycline, colistin, or rifampin, sometimes adding inhaled agents for lower respiratory tract infections. Further evolution of resistance of KPC-producers to include tigecycline or colistin has been described, although rarely. In a recent study, factors associated with KPC-producing K. pneumoniae were transplantation, receipt of mechanical ventilation, long duration of hospital stay, and exposure to cephalosporins and carbapenems. Patients had a 48% mortality rate, compared with 26% among patients infected with carbapenem-susceptible K. pneumoniae [16]. Given the dire state of the pipeline for new antibiotics to treat gram-negative pathogens, infection control will be our main weapon against these organisms for the short term. Heightened contact precautions and active surveillance have proven to be helpful in outbreak control [17]. Although community spread has not yet been recognized, patients from longterm acute care hospitals were recently identied as a reservoir in a city-wide outbreak [18]. KPC-producing gram-negative pathogens are evolving rapidly. Until new agents are developed, we agree with Srivinivasan and Patel, who stated recently: a pound of prevention really is worth a pound of cure [19, p. 1107].
Acknowledgments
Potential conicts of interest. J.P.Q. is an employee of Pzer Global Research and Development. L.S.M.P.: no conicts.
References
1. Queenan AM, Bush K. Carbapenemases: the versatile b-lactamases. Clin Microbiol Rev 2007; 20:44058. 2. Nordmann P, Cuzon G, Naas T. The real threat of Klebsiella pneumoniae carbapenemase-producing bacteria. Lancet Infect Dis 2009; 9: 22836. 3. Landman D, Bratu S, Kochar S, et al. Evolution of antimicrobial resistance among Pseudomonas aeruginosa, Acinetobacter baumannii and Klebsiella pneumoniae in Brooklyn, NY. J Antimicrob Chemother 2007; 60:7882. 4. Kitchel B, Rasheed JK, Patel JB, et al. Molecular epidemiology of KPC-producing Klebsiella pneumoniae isolates in the United States: clonal expansion of multilocus sequence type 258. Antimicrob Agents Chemother 2009; 53: 336570. 5. Naas T, Nordmann P, Vedel G, Poyart C. Plasmid-mediated carbapenem-hydrolyzing betalactamase KPC in a Klebsiella pneumoniae isolate from France. Antimicrob Agents Chemother 2005; 49:44234. 6. Navon-Venezia S, Leavitt A, Schwaber MJ, et al. First report on a hyperepidemic clone of KPC-3-producing Klebsiella pneumoniae in Israel genetically related to a strain causing outbreaks in the United States. Antimicrob Agents Chemother 2009; 53:81820. 7. Lahey Clinic Web site. Amino acid sequences for TEM, SHV and OXA extended-spectrum and inhibitor resistant b-lactamases. Available at: http://www.lahey.org/studies. Accessed 15 Oct 2009. 8. Gootz TD, Lescoe MK, Dib-Hajj F, et al. Genetic organization of transposase regions surrounding blaKPC carbapenemase genes on plasmids from Klebsiella strains isolated in a New York City hospital. Antimicrob Agents Chemother 2009; 53:19982004. 9. Naas T, Cuzon G, Villegas MV, Lartigue MF, Quinn JP, Nordmann P. Genetic structures at the origin of acquisition of the beta-lactamase bla KPC gene. Antimicrob Agents Chemother 2008; 52:125763. 10. Moland ES, Hong SG, Thomson KS, Larone DH, Hanson ND. Klebsiella pneumoniae isolate producing at least eight different betalactamases, including AmpC and KPC betalactamases. Antimicrob Agents Chemother 2007; 51:8001. 11. Sidjabat HE, Silveira FP, Potoski BA, et al. Interspecies spread of Klebsiella pneumoniae carbapenemase gene in a single patient. Clin Infect Dis 2009; 49:17368 (in this issue). 12. Bennett JW, Herrera ML, Lewis JS, Wickes BW, Jorgensen JH. KPC-2-producing Enterobacter cloacae and Pseudomonas putida coinfection in a liver transplant recipient. Antimicrob Agents Chemother 2009; 53:2924. 13. Petrella S, Ziental-Gelus N, Mayer C, Renard M, Jarlier V, Sougakoff W. Genetic and structural insights into the dissemination potential of the extremely broad-spectrum class A
Downloaded from cid.oxfordjournals.org by guest on February 27, 2011
1740 CID 2009:49 (1 December) EDITORIAL COMMENTARY
beta-lactamase KPC-2 identied in an Escherichia coli strain and an Enterobacter cloacae strain isolated from the same patient in France. Antimicrob Agents Chemother 2008; 52:372536. 14. Anthony KB, Fishman NO, Linkin DR, Gasink LB, Edelstein PH, Lautenbach E. Clinical and microbiological outcomes of serious infections with multidrug-resistant gram-negative organisms treated with tigecycline. Clin Infect Dis 2008; 46:56770. 15. Falagas ME, Kasiakou SK. Toxicity of polymyxins: a systematic review of the evidence
from old and recent studies. Crit Care 2006; 10:R27. 16. Patel G, Huprikar S, Factor SH, Jenkins SG, Calfee DP. Outcomes of carbapenem-resistant Klebsiella pneumoniae infection and the impact of antimicrobial and adjunctive therapies. Infect Control Hosp Epidemiol 2008; 29: 1099106. 17. Kochar S, Sheard T, Sharma R, et al. Success of an infection control program to reduce the spread of carbapenem-resistant Klebsiella pneumoniae. Infect Control Hosp Epidemiol 2009; 30:44752. 18. Won S, Munoz-Price LS, Lolans K, et al.
Multi-facility emergence and rapid spread of KPC+ Enterobacteriaceae in Northwest Indiana (NWI) and Illinois (IL) 224 [abstract: 67]. In: Programs and abstracts of the 19th Annual Scientic Meeting of the Society for Healthcare Epidemiology of America (San Diego). Arlington, VA: Society for Healthcare Epidemiology of America, 2009. 19. Srinivasan A, Patel JB. Klebsiella pneumoniae carbapenemase-producing organisms: an ounce of prevention really is worth a pound of cure. Infect Control Hosp Epidemiol 2008; 29:11079.
Downloaded from cid.oxfordjournals.org by guest on February 27, 2011
EDITORIAL COMMENTARY CID 2009:49 (1 December) 1741
Anda mungkin juga menyukai
- Klebsiella Pneumoniae ThesisDokumen6 halamanKlebsiella Pneumoniae Thesisaprillaceyjackson100% (1)
- Idr 5 133Dokumen9 halamanIdr 5 133Jose Daniel Muñoz FuentesBelum ada peringkat
- Ijms 22 04042 v2Dokumen20 halamanIjms 22 04042 v2Alexandru NeatuBelum ada peringkat
- Reviews: Population Genomics ofDokumen16 halamanReviews: Population Genomics ofRaul MolloBelum ada peringkat
- Klebsiella Infections Treatment & ManagementDokumen5 halamanKlebsiella Infections Treatment & ManagementCecilia GrunauerBelum ada peringkat
- Carbapenem Resistant EnterobacteriaceaeDokumen15 halamanCarbapenem Resistant Enterobacteriaceaeja_sam_radivoje3093Belum ada peringkat
- Plasmid-Mediated Transmission of KPC-2 Carbapenema PDFDokumen8 halamanPlasmid-Mediated Transmission of KPC-2 Carbapenema PDFJose Daniel Muñoz FuentesBelum ada peringkat
- Enterobacter Cloacae: Carbapenem-Resistant in Patients From The US Veterans Health Administration, 2006-2015Dokumen3 halamanEnterobacter Cloacae: Carbapenem-Resistant in Patients From The US Veterans Health Administration, 2006-2015Mayang WulanBelum ada peringkat
- Antibiotic ResistanceDokumen3 halamanAntibiotic ResistanceJanine AndersonBelum ada peringkat
- Final Project VinceDokumen21 halamanFinal Project Vincekiss4444f4Belum ada peringkat
- Jiao PDFDokumen7 halamanJiao PDFRodrigo GarciaBelum ada peringkat
- JCM 10 02067 With CoverDokumen14 halamanJCM 10 02067 With CoverAnhBelum ada peringkat
- Clinical Implications of Genomic Adaptation andDokumen10 halamanClinical Implications of Genomic Adaptation andPhuong NguyenBelum ada peringkat
- Carbapenem Resistant Enterobacteriaceae - StatPearls - NCBI BookshelfDokumen9 halamanCarbapenem Resistant Enterobacteriaceae - StatPearls - NCBI BookshelfOG3 PolizuBelum ada peringkat
- Quantifying The Clinical Virulence of Klebsiella Pneumoniae Producing Carbapenemase Klebsiella Pneumoniae With A Galleria Mellonella Model and A Pilot Study To Translate To Patient OutcomesDokumen10 halamanQuantifying The Clinical Virulence of Klebsiella Pneumoniae Producing Carbapenemase Klebsiella Pneumoniae With A Galleria Mellonella Model and A Pilot Study To Translate To Patient OutcomesJuwita PratiwiBelum ada peringkat
- Annals of The New York Academy of Sciences - 2014 - Temkin - Carbapenem Resistant Enterobacteriaceae Biology EpidemiologyDokumen21 halamanAnnals of The New York Academy of Sciences - 2014 - Temkin - Carbapenem Resistant Enterobacteriaceae Biology EpidemiologyKavyarani RathodBelum ada peringkat
- Research Papers On KlebsiellaDokumen8 halamanResearch Papers On Klebsiellagzrvpcvnd100% (1)
- Peter Hawkey: The Enemy Within - Hospital-Acquired, Antibiotic-Resistant BacteriaDokumen3 halamanPeter Hawkey: The Enemy Within - Hospital-Acquired, Antibiotic-Resistant BacteriaCoffee CojjeeBelum ada peringkat
- Infections in Cancer Chemotherapy: A Symposium Held at the Institute Jules Bordet, Brussels, BelgiumDari EverandInfections in Cancer Chemotherapy: A Symposium Held at the Institute Jules Bordet, Brussels, BelgiumBelum ada peringkat
- Blee NuevoDokumen11 halamanBlee Nuevomarivero23Belum ada peringkat
- Genoma TBDokumen14 halamanGenoma TBMARIO CASTROBelum ada peringkat
- Introduction of Klebsiella PneumoniaeDokumen189 halamanIntroduction of Klebsiella PneumoniaeAnia sahaBelum ada peringkat
- Medical Conference: Crohn DiseaseDokumen9 halamanMedical Conference: Crohn DiseasetiaraBelum ada peringkat
- Wajib - Tuberculosis - Pathophysiology, Clinical Features, and DiagnosisDokumen12 halamanWajib - Tuberculosis - Pathophysiology, Clinical Features, and DiagnosisnurulahdiahBelum ada peringkat
- Review of Known and Unknown Facts of Klebsiella Pneumoniae and Its Relationship With AntibioticsDokumen8 halamanReview of Known and Unknown Facts of Klebsiella Pneumoniae and Its Relationship With AntibioticsPhuong NguyenBelum ada peringkat
- Crabapenem With EDTADokumen9 halamanCrabapenem With EDTApharmbharathiBelum ada peringkat
- E00261-16 FullDokumen12 halamanE00261-16 FullSandu AlexandraBelum ada peringkat
- Klebsiella Sp. Epidemiology Taxonomy and PatogenicityDokumen15 halamanKlebsiella Sp. Epidemiology Taxonomy and PatogenicityDulce MariaBelum ada peringkat
- Acinetobacter Infection in The Intensive Care Unit: Review ArticleDokumen16 halamanAcinetobacter Infection in The Intensive Care Unit: Review ArticleDrashua AshuaBelum ada peringkat
- Auto-Inflammatory Syndromes: Pathophysiology, Diagnosis, and ManagementDari EverandAuto-Inflammatory Syndromes: Pathophysiology, Diagnosis, and ManagementPetros EfthimiouBelum ada peringkat
- Fast Facts: Blastic Plasmacytoid Dendritic Cell Neoplasm: Shedding light on a rare diseaseDari EverandFast Facts: Blastic Plasmacytoid Dendritic Cell Neoplasm: Shedding light on a rare diseaseBelum ada peringkat
- Ben Ami ESBL in Community Risk FactorsDokumen9 halamanBen Ami ESBL in Community Risk FactorsSIUSANTO HadiBelum ada peringkat
- Colonization, Infection, and The Accessory Genome of KlebsiellaDokumen15 halamanColonization, Infection, and The Accessory Genome of KlebsiellaStephanie ZengBelum ada peringkat
- Life 12 00746Dokumen20 halamanLife 12 00746roberto gallegosBelum ada peringkat
- Samman MSDokumen5 halamanSamman MSSamman zakaBelum ada peringkat
- Next Generation Sequencing of Microbial Cell Free DNA To Rapidly Detect Fluoribacter Bozemanae Pneumonia in An Immunocompromised HostDokumen4 halamanNext Generation Sequencing of Microbial Cell Free DNA To Rapidly Detect Fluoribacter Bozemanae Pneumonia in An Immunocompromised HostAthenaeum Scientific PublishersBelum ada peringkat
- Literature Review of Mycobacterium TuberculosisDokumen8 halamanLiterature Review of Mycobacterium Tuberculosisafmacfadbdwpmc100% (1)
- Kaposi's Sarcoma in Renal Transplantation: Report of Three CasesDokumen3 halamanKaposi's Sarcoma in Renal Transplantation: Report of Three CasesSayab MursiBelum ada peringkat
- American Journal of Infection Control: Major ArticleDokumen6 halamanAmerican Journal of Infection Control: Major ArticleHugoMarcelo77Belum ada peringkat
- TreatmentDokumen3 halamanTreatmentNarasimharao HarnoorBelum ada peringkat
- Klebsiella Pneumonia - StatPearls - NCBI BookshelfDokumen7 halamanKlebsiella Pneumonia - StatPearls - NCBI BookshelfMariel Siason-OrbisoBelum ada peringkat
- Namita JaggiDokumen4 halamanNamita JaggiIJAMBelum ada peringkat
- Streptococcus Gallolyticus Subsp. PasteuranusDokumen7 halamanStreptococcus Gallolyticus Subsp. PasteuranusBárbara RochaBelum ada peringkat
- Research Paper On PneumoniaDokumen6 halamanResearch Paper On Pneumoniagz8bjzmj100% (1)
- Immunobiology of the Complement System: An Introduction for Research and Clinical MedicineDari EverandImmunobiology of the Complement System: An Introduction for Research and Clinical MedicineGordon D. RossPenilaian: 3 dari 5 bintang3/5 (2)
- The Potential Contributions of Chronic IDokumen17 halamanThe Potential Contributions of Chronic IJohn QuilumbaBelum ada peringkat
- Identifying 5Dokumen6 halamanIdentifying 5Nidia MaradiagaBelum ada peringkat
- Isolates Producing A KPC-Type First Identification Of: Aeruginosa PseudomonasDokumen4 halamanIsolates Producing A KPC-Type First Identification Of: Aeruginosa PseudomonasملاكBelum ada peringkat
- Stenotrophomona Maltophilia y Bulkorelia Cepacia. Mnadell 2009Dokumen8 halamanStenotrophomona Maltophilia y Bulkorelia Cepacia. Mnadell 2009Laura López Del Castillo LalydelcaBelum ada peringkat
- Resist Ncia Enterobact Rias PatersonDokumen9 halamanResist Ncia Enterobact Rias PatersonDrashua AshuaBelum ada peringkat
- Cancer Immunology: Bench to Bedside Immunotherapy of CancersDari EverandCancer Immunology: Bench to Bedside Immunotherapy of CancersBelum ada peringkat
- Sporulation in MycobacteriaDokumen6 halamanSporulation in MycobacteriaGUIDO ERNESTO VILLOTA CALVACHIBelum ada peringkat
- Mycoplasma Pneumoniae PHD ThesisDokumen8 halamanMycoplasma Pneumoniae PHD Thesisgjcezfg9100% (2)
- KCP 1Dokumen7 halamanKCP 1FurqanRidhaBelum ada peringkat
- PneumoniaDokumen10 halamanPneumoniaAubrey PerezBelum ada peringkat
- Atypical Presentation of Pseudomembranous Colitis Localized in Adenomatous PolypsDokumen3 halamanAtypical Presentation of Pseudomembranous Colitis Localized in Adenomatous PolypsKiana TehraniBelum ada peringkat
- Sanz Et Al 2024 KPC 2 Allelic Variants in Klebsiella Pneumoniae Isolates Resistant To Ceftazidime Avibactam FromDokumen13 halamanSanz Et Al 2024 KPC 2 Allelic Variants in Klebsiella Pneumoniae Isolates Resistant To Ceftazidime Avibactam FromABMOHEBelum ada peringkat
- What Is The Role of Antimicrobial Resistance in The New Epidemic ofDokumen4 halamanWhat Is The Role of Antimicrobial Resistance in The New Epidemic ofcarrrrr567Belum ada peringkat
- Macrolides in Children With Community-Acquired Pneumonia: Panacea or Placebo?Dokumen7 halamanMacrolides in Children With Community-Acquired Pneumonia: Panacea or Placebo?Agniya Ali FahmiBelum ada peringkat
- High Prevalence of KPC-2 Type Carbapenemase Coupled With CTX-M Type Extended-SpectrumDokumen6 halamanHigh Prevalence of KPC-2 Type Carbapenemase Coupled With CTX-M Type Extended-SpectrumMohammad K AlshomraniBelum ada peringkat
- Prevalence of Extended-Spectrum Beta-Lactamases Among Isolated Isolated From Blood Culture in A Tertiary Care HospitalDokumen4 halamanPrevalence of Extended-Spectrum Beta-Lactamases Among Isolated Isolated From Blood Culture in A Tertiary Care HospitalMohammad K AlshomraniBelum ada peringkat
- 2Dokumen4 halaman2Mohammad K AlshomraniBelum ada peringkat
- BALKHYDokumen9 halamanBALKHYMohammad K AlshomraniBelum ada peringkat
- AttachmentDokumen7 halamanAttachmentMohammad K AlshomraniBelum ada peringkat
- Multiple Pulp Polyps Associated With Deciduous TeethDokumen4 halamanMultiple Pulp Polyps Associated With Deciduous TeethJea Ayu YogatamaBelum ada peringkat
- Contact Lens Complications and ManagementDokumen10 halamanContact Lens Complications and Managementstrawberry8832850% (2)
- Kode Penjelasan Keterangan: ObgynDokumen14 halamanKode Penjelasan Keterangan: Obgynanon_507132438Belum ada peringkat
- PHD Research ProposalDokumen8 halamanPHD Research ProposalMalik Ijaz Khan100% (1)
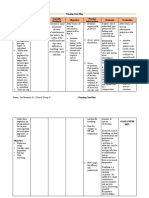
- Plan Training Session: Trainers Methodology Level I Templates Document No. Issued By: Ntta Page I of VIIDokumen31 halamanPlan Training Session: Trainers Methodology Level I Templates Document No. Issued By: Ntta Page I of VIIBenevict L. IbañezBelum ada peringkat
- Euthanasia ThesisDokumen11 halamanEuthanasia ThesisAyush MathurBelum ada peringkat
- Soca Review Genitourinary System Case 1-Urinary StoneDokumen6 halamanSoca Review Genitourinary System Case 1-Urinary StoneImania Salim Ahmad BawazierBelum ada peringkat
- Jci WP Med Suction and Fluid Waste MGT FinalDokumen16 halamanJci WP Med Suction and Fluid Waste MGT FinalAbhi RajBelum ada peringkat
- Nature and Characteristics of Services in HospitalsDokumen7 halamanNature and Characteristics of Services in HospitalsOun MuhammadBelum ada peringkat
- Second Hand Smoke Fact SheetDokumen9 halamanSecond Hand Smoke Fact Sheetwesa77Belum ada peringkat
- Kakawate Dog Soap ThesisDokumen55 halamanKakawate Dog Soap ThesisArturo Roman100% (4)
- Autism Spectre DisorderDokumen13 halamanAutism Spectre DisorderJesus Hurtado100% (2)
- OME Video DurationsDokumen7 halamanOME Video DurationsLucas RiosBelum ada peringkat
- Nursing Care PlanDokumen13 halamanNursing Care PlanJan DamesBelum ada peringkat
- FWD Medical Rider enDokumen12 halamanFWD Medical Rider enKhairul HMSBBelum ada peringkat
- Non - Food Meher Final Report (2023)Dokumen87 halamanNon - Food Meher Final Report (2023)atakltigebertsadikBelum ada peringkat
- A Potential Siddha Mineral Drug Pavala ParpamDokumen8 halamanA Potential Siddha Mineral Drug Pavala Parpamjmanuel108yahoo.co.ukBelum ada peringkat
- Endocrine Glands PDFDokumen99 halamanEndocrine Glands PDFXochitl ZambranoBelum ada peringkat
- Agc332 Lecture 10-Wheat DiseasesDokumen33 halamanAgc332 Lecture 10-Wheat DiseasesSolomon MbeweBelum ada peringkat
- Carvalho-2016-About AssesmentDokumen19 halamanCarvalho-2016-About AssesmentChiriac Andrei TudorBelum ada peringkat
- Cystic Hygroma - Symptoms - Diagnosis - Treatment of Cystic Hygroma - NY Times Health InformationDokumen3 halamanCystic Hygroma - Symptoms - Diagnosis - Treatment of Cystic Hygroma - NY Times Health InformationRenno AdiBelum ada peringkat
- DLP in Health 10 Global Health InitiativesDokumen10 halamanDLP in Health 10 Global Health InitiativesJoshua MaravillasBelum ada peringkat
- Chapter 123Dokumen56 halamanChapter 123Jane Guiron AballaBelum ada peringkat
- CHON Lecture PDFDokumen25 halamanCHON Lecture PDF2d HoehoeBelum ada peringkat
- Normal Periodontium 1Dokumen49 halamanNormal Periodontium 1mdio midoBelum ada peringkat
- 1 PPT Bioethics Lecture N1Dokumen44 halaman1 PPT Bioethics Lecture N1h.a.r.ade.v.ierBelum ada peringkat
- Exercises For DiabetesDokumen25 halamanExercises For DiabetesrichaBelum ada peringkat
- Home Quarantine Compliance 2022 1Dokumen1 halamanHome Quarantine Compliance 2022 1Puting KahoyBelum ada peringkat
- Pereneal CareDokumen2 halamanPereneal CareindumathiBelum ada peringkat
- Clinical Microbiology and Infection: Original ArticleDokumen6 halamanClinical Microbiology and Infection: Original ArticleAkira Masumi100% (1)