Reupload Skin Graft Management
Diunggah oleh
hawaalia534Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Reupload Skin Graft Management
Diunggah oleh
hawaalia534Hak Cipta:
Format Tersedia
guideline
Skin Graft Management Guidelines
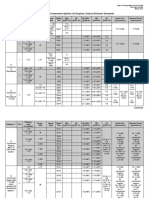
Document Number Publication Date Intranet location/s Summary Author Department Contact (Details) Wound Care, Aged Care & Rehabilitation, Acute/Post Acute Care, Critical Care, Community, Nursing, Surgical, Management of skin grafts post surgery. Rachel Kornhaber, Clinical Nurse Specialist (Burns & Plastic Surgery), Severe Burns Injury Unit/ Plastics, RNSH. Peter Campbell CNC Burns & Plastic Surgery 9926 5644 NSCCH Wound Care Committee NSCCH Clinicians September 2008 September 2010 Nil Donor Site Management Guidelines, Wound Standards, Infection Control Standards Precautions, Hand Hygiene / Hand washing, Environmental Services Waste Disposal Guidelines, Wound Swab Guidelines. Split skin, full thickness, wound bed, donor site, dermatome, harvesting, dermis, epidermis. Active
Endorsed By Scope (sector/service) Audience Date Created Review date Previous Reference Related Policy/s
Key Words Status
Warning: This document contains graphic wound photos that may be unpleasant to some viewers.
Disclaimer: This guideline is only authorised for use within NSCCH. Other organisations need to consider carefully before accepting.
NORTHERN SYDNEY CENTRAL COAST HEALTH The controlled version of this document appears on the intranet
Title: Skin Graft Management Guidelines
1. Summary Skin Graft .......................................................................................................... 3 2. Expected Outcome/s ............................................................................................................ 4 3. Scope of Practice ................................................................................................................. 4 3. Definitions............................................................................................................................. 5 4. Guideline .............................................................................................................................. 6 5. Actions.................................................................................................................................. 7 5.1 Introduction......................................................................................................................... 7 5.2 Aim of management ........................................................................................................... 9 5.3 Initial split skin graft management ...................................................................................... 9 5.4 Subsequent management of split skin grafts ................................................................... 12 5.5 Full thickness skin grafts .................................................................................................. 13 5.5 Complication with skin grafts ............................................................................................ 15 5.6 Healed skin graft care and scar management.................................................................. 18 6. References ......................................................................................................................... 20 7. Acknowledgements ............................................................................................................ 20
Guideline Name Document ID Date Printed
30/01/07
Version No. Page No.
2 of 20
NORTHERN SYDNEY CENTRAL COAST HEALTH The controlled version of this document appears on the intranet
1.
Summary Skin Graft
This summary should be read in conjunction with the guideline and is not a replacement for the full document available via NSCCAHS intranet.
a. Definition
A skin graft is the graft technique in which sheets of skin are harvested containing the epidermis and part of the dermis (Split Skin Graft) or both the epidermis and dermis (Full Thickness Graft) to cover skin loss (surgical or traumatic).
b. Patient Group/Key Associated Risk Factors
These guidelines apply to all clinicians managing patients with skin grafts within NSCCHS.
c. Key Principles of Clinical Care
i. Management of patients with skin grafts is a collaborative effort incorporating a multidisciplinary team, the patient/Carer. ii. In order to maintain the comfort and safety of the patient post operatively and through dressing changes, their pain must be assessed prior, during and after any procedure and analgesia MUST be offered. iii. Patients who are scheduled to have skin grafting are to be given the NSCCAHS Skin Graft Patient Information Brochure explaining the procedure and care of a patient with a skin graft. iv. Split skin grafts are usually taken down to view on day 5, unless otherwise requested by surgeon. v. Full thickness grafts are usually taken down to view on day 7, unless otherwise requested by surgeon. vi. The surgeon may request skin grafts to be taken down prior to this time, due to bleeding, infection and/or malodour. vii. It is advisable that a member of the Burns/Plastics or Surgical team be notified to review the graft at the time of the first dressing post skin grafting.
viii. Ongoing Responsibilities
All clinicians are responsible for following these guidelines and monitoring the wound healing outcomes of patients with skin grafts.
Guideline Name Document ID Date Printed
30/01/07
Version No. Page No.
3 of 20
NORTHERN SYDNEY CENTRAL COAST HEALTH The controlled version of this document appears on the intranet
2.
Expected Outcome/s
1. All care and management of the skin graft will be as per this guideline. 2. All care given is based on best current evidenced based practice. 3. All patients requiring skin grafts receive competent and safe care. 4. Skin graft will mature with minimal scaring and complications.
3.
Scope of Practice
This guideline applies to all clinicians providing competent wound care for post operative nursing management of patients who have undergone skin grafts within NSCCH: Registered Nurses Podiatrists Physiotherapists Occupational Therapists Medical Officers Enrolled and Endorsed Enrolled Nurses.
Guideline Name Document ID Date Printed
30/01/07
Version No. Page No.
4 of 20
NORTHERN SYDNEY CENTRAL COAST HEALTH The controlled version of this document appears on the intranet
3. Definitions
Contraction Dermis Process where the skin graft contracts and shrinks the graft. The inner layer of tissue that forms the skin, containing blood and lymph vessels, hair follicles and glands that produce sweat and sebum. Dermatome Devitalised Donor site Epidermis Power driven knife used to harvest split skin grafts. Devoid of life; dead. The site from where the graft is taken. The upper layer of tissue that forms the skin containing keratinocytes. It is where melanin is produced for skin colour. Epithelisation Full thickness skin grafts (FTSG) Graft bed Granulation Formation of epithelium over the wound bed. A graft technique in which the skin contains both the epidermis and dermis. The wound bed on which the skin graft is laid. The process where a framework of new pink tissue and capillaries begin to form around the edges of the wound. Haematoma Harvesting Hypergranulation Collection of blood under the skin graft. The act of removing skin from the donor site. Hypergranulation is a result of an extended inflammatory response and bacterial burden Meshed graft Sheet graft Split skin graft (SSG) A split skin graft that is fenestrated. A split skin graft that is intact with no fenestrations. A graft technique in which sheets of skin are harvested containing the epidermis and part of the dermis for grafting. Strike-through Wound exudate that leaks through the outermost layer of bandage or dressing. Take Refers to the adherence of the graft to the wound bed. Usually discussed in terms of a percentage of overall wound surface area. (Hawkins Bradley 2002; Bailie & Wilson 2002; McGregor & McGregor, 2000).
Guideline Name Document ID Date Printed
30/01/07
Version No. Page No.
5 of 20
NORTHERN SYDNEY CENTRAL COAST HEALTH The controlled version of this document appears on the intranet
4.
Guideline 4.1 Policy Statement/Rationale
These guidelines apply to all clinicians managing skin grafts within the NSCCH. Best practice wound care aims to promote positive outcomes for patients ensuring optimal wound healing and maturation of the skin graft, minimising the risk of infection and to reduce pain and discomfort.
4.2 Requirements
1. Management of patients with skin grafts is a collaborative effort incorporating a multidisciplinary team, the patient/Carer. 2. In order to maintain the comfort and safety of the patient post operatively and through dressing changes, their pain must be assessed prior, during and after any procedure and analgesia MUST be offered. 3. Patients who are scheduled to have skin grafting are to be given the NSCCAHS Skin Graft Patient Information Brochure explaining the procedure and care of a patient with a skin graft. 4. Split skin grafts are usually taken down to view on day 5, unless otherwise requested by surgeon. 5. Full thickness grafts are usually taken down to view on day 7, unless otherwise requested by surgeon. 6. The surgeon may request skin grafts to be taken down prior to this time, due to bleeding, infection and/or malodour. 7. It is advisable that a member of the Burns/Plastics or Surgical team be notified to review the graft at the time of the first dressing post skin grafting.
Guideline Name Document ID Date Printed
30/01/07
Version No. Page No.
6 of 20
NORTHERN SYDNEY CENTRAL COAST HEALTH The controlled version of this document appears on the intranet
5.
Actions 5.1 Introduction
The surgical technique of skin grafting is utilised to cover wounds as a result of varying aetiologies such as burns, injury sustained or removal of lesions. Skin grafting involves moving the patients own skin from one position on the body to another. There are two types of skin grafts: Split skin grafts: consists of the epidermis and a portion of the dermis depending on the thickness of the graft. Full thickness skin graft: consists of the epidermis and the entire dermis.
Figure 1 - Demonstrates the varying thickness of a split skin grafts and full thickness skin grafts. Figure 1: Thickness of skin grafts.
(McGregor & McGregor, 2000)
Guideline Name Document ID Date Printed
30/01/07
Version No. Page No.
7 of 20
NORTHERN SYDNEY CENTRAL COAST HEALTH The controlled version of this document appears on the intranet
Split skin grafts are usually harvested using a dermatone (a surgical instrument used to cut thin slices of skin for grafting). Figure 2 4 demonstrates how the skin is harvested for skin grafting and the meshing process. Figure 2: Dermatone used to harvest skin The SSG is either meshed or left intact as a sheet graft. (Koljonen, Gerdin, Vuola & Aili Low, 2007) Figure 3: Meshing a split skin graft. (Koljonen, Gerdin, Vuola & Aili Low, 2007)
Figure 4: Meshed skin ready to be laid onto the wound bed. (Koljonen, Gerdin, Vuola & Aili Low, 2007)
Figure 5: Meshed skin graft taken down Day 5 100% take
Guideline Name Document ID Date Printed
30/01/07
Version No. Page No.
8 of 20
NORTHERN SYDNEY CENTRAL COAST HEALTH The controlled version of this document appears on the intranet
5.2 Aim of management
The objectives of skin graft management are to: Cover the deficit with a skin graft Achieve healing as swiftly as possible without any complications Maintain patient comfort Maintain cost effectiveness.
5.3 Initial split skin graft management
Pre-operative education is essential. The NSCCAHS Split Skin Graft Patient/Carer Information Brochure gives a detailed description of the procedure and information with clear guidelines necessary for their post operative education and management. On arrival post operatively: 1. Assess the positioning needs of the patient. 2. Excessive pressure on the graft site is detrimental to the wound bed and skin graft due to a reduction in blood flow to the area and shearing forces. 3. Confirm with the surgical team the limitation and expectations of the post operative management. 4. Grafted areas and donor sites should be identified, differentiated and documented on the wound care chart and medical record. 5. It is essential that all wounds are dressed post operatively and that these dressings are maintained according to the NSCCAHS Wound Care Standards
(http://intranet02.nsccahs.health.nsw.gov.au/policyprocedure/clinicalpatientcare/PO2 007_006.pdf). E.g. outer dressings are renewed if soiled.
Figure 6: Common sites for split skin grafts: Donor Site Graft Site Thigh Upper arm Buttocks Anterior trunk Posterior trunk
Note: The thigh is the most common site for a donor site.
Guideline Name Document ID Date Printed
30/01/07
Version No. Page No.
9 of 20
NORTHERN SYDNEY CENTRAL COAST HEALTH The controlled version of this document appears on the intranet
Management of Newly Grafted Areas:
Figure 7: Graft site to extremities must remain
immobile for 5 days with a split skin graft. In most cases a plaster backslab is used to reduce movement in the limb and therefore friction between the graft and the surgical site. Figure 8: Elevate arm/s in gallows with the aid of an IV pole. A pillow is placed under the elbow for support and comfort.
Retrieved on the21/12/07 from http://www.salitas.co.uk/
Elevate grafted arm/s on pillows or in a gallows (see figure 8). Elevate grafted leg/s on pillows. Grafts to the lower extremities require bed rest for a period of 5 days. It must be noted that it is at the surgeons request that toilet privileges are allowed. If toilet privileges are granted, the leg must remain elevated and the patient transported to the toilet using a commode chair. Occasionally patients are allowed to mobilise day 1 post operatively with the use of support bandages. Refer to post operative orders/surgical team to confirm.
Guideline Name Document ID Date Printed
30/01/07
Version No. Page No.
10 of 20
NORTHERN SYDNEY CENTRAL COAST HEALTH The controlled version of this document appears on the intranet
If hands or feet are grafted or across joints, splints must be insitu to immobilise the graft site to avoid shearing forces. Splints are applied to the patient in theatre. Monitor the placement of the splint used to immobilise the grafted area for pressure areas. Notify the physiotherapist or occupational therapist if the patient complains of pain related to the positioning of the splint.
Circulation observations may be requested for 24 hours post operatively. Assess hourly the splinted extremity if the dressing permits. Document on the Peripheral Extremities Form U6A
Grafted sites to the torso: Prevent excessive pressure or shearing forces to the grafted area. Grafted areas to the neck: Patients require a soft collar to immobilise graft site and NO PILLOW is allowed to avoid contractures. Assess for signs of active bleeding, indications of active bleeding are dressings with excessive strike through or those that are soaked. Draw around the blood stained area on the outer dressing noting the date and time to visually monitor active bleeding.
Integrity of the dressing must be assessed. It is essential that the graft site remains dry and intact for 5 days with a split skin graft and approximately 7 - 10 days with a full thickness skin graft.
If the graft site is being managed using Negative Pressure Wound Therapy such as Vacuum Assisted Closure (VAC) (link to follow) then assess for an adequate seal and correct negative pressure as ordered.
Calories, Proteins, Vitamin C and Zinc are all an important adjuncts to the wound healing. Ensure patients are able to optimise their nutritional and hydration status. Patients/clients considered to be in a poor nutritional state must be referred to a dietician (wherever possible) and a nutritional plan devised and implemented.
Discuss limitations with the patient and provide rationales. Educate the patient on the importance of compliance with their post-operative instructions and nutrition in order to achieve optimal healing.
If the patient is a smoker explain the importance of the cessation of smoking related to wound healing. A drug and alcohol consult may be required if the patient is withdrawing from nicotine.
Guideline Name Document ID Date Printed
30/01/07
Version No. Page No.
11 of 20
NORTHERN SYDNEY CENTRAL COAST HEALTH The controlled version of this document appears on the intranet
5.4 Subsequent management of split skin grafts
The graft site for a SSG is taken down for the surgical team to review at day 5. The graft site is assessed for take and the splints are removed if applicable. Make sure: Adequate pain relief is given prior to the removal of the dressing. The staples are removed from the graft edges. Devitalised graft tissue is trimmed around the graft site. If the graft site is clean it is not necessary to cleanse the wound with normal saline per the NSCCAHS Wound Cleansing Guidelines
http://intranet02.nsccahs.health.nsw.gov.au/policyprocedure/clinicalpatientcare/GE20 07_001_.pdf . The graft site is redressed ensuring the deficit of the wound is filled to the level of the skin. Dressing choice for the graft site needs to ensure: Figure 9: Example of bandaging toe to knee with final layer of a non stick dressing not exposed to shearing forces and tearing provides a moist clean environment for optimal wound healing. Bandaging complies with the principle of distal to proximal i.e.
compression visible.
Figure 10: Example of bandaging finger to palm, palm to wrist with final layer of compression visible.
Guideline Name Document ID Date Printed
30/01/07
Version No. Page No.
12 of 20
NORTHERN SYDNEY CENTRAL COAST HEALTH The controlled version of this document appears on the intranet
The graft site is redressed 2nd to 4th daily depending on the dressing product used. A retentive dressing is placed over the primary dressing. However care must be taken to ensure the retentive dressing is not too tight and does not restrict blood flow. Those using retentive/pressure dressing should be assessed and competent practitioners in this area of practice prior to commencing this task (See NSCCAHS Compression Policy link to follow). Follow up care for the patient following discharge is arranged with an appropriate entity i.e. outpatient ambulatory care clinic, doctors rooms or community nursing. If the graft site is on the lower extremities, the patient must be educated on the importance of elevation lower limb or arms when not mobilising.
5.5 Full thickness skin grafts
Full thickness skin grafts are often used on the patients face, hands, over joints or where avascular tissue is exposed such as where there is tendon or bone is on show. However the size of the grafts are limited due to the donor sites requiring primary closure or require a split skin graft to cover the defect. Table 1 states common full thickness donor sites.
Table 1: Common donor sites for full thickness grafts 1. Postauricular 2. Preauricular 3. Supraclavicular 4. Upper eyelid 5. Scalp 6. Antecubital 7. Inguinal skin
Benefits of Full Thickness Skin Grafts: 1. They contain the complete dermis therefore there is less contraction of the graft compared to a split skin graft due to a greater collagen component, vascularity and the skin appendages (e.g. hair follicles, sweat gland etc) . 2. For full thickness skin graft on the face, hands and over joints as it maintains a more normal appearance of skin and undergoes less contraction and scarring.
Guideline Name Document ID Date Printed
30/01/07
Version No. Page No.
13 of 20
NORTHERN SYDNEY CENTRAL COAST HEALTH The controlled version of this document appears on the intranet
Figure 13: Full thickness skin grafts are sutured in place and a sponge bolster known as a tie over dressing is applied sutured or stapled on top of the full thickness skin graft. The tie over dressing is a pressure dressing that must stay intact for a period of 1 week and must not be wet or be removed. The take of a full thickness skin graft is slower than a split skin graft. In order for the full thickness skin graft to take it requires: a good blood supply between the graft and the wound bed, that is not interrupted by a physical barrier such as a haematoma or seroma immobility of the graft site graft site to be free of infection Pressure and contact with the wound bed and surrounding tissue.
Tie over pack
Guideline Name Document ID Date Printed
30/01/07
Version No. Page No.
14 of 20
NORTHERN SYDNEY CENTRAL COAST HEALTH The controlled version of this document appears on the intranet
5.5 Complication with skin grafts
The following are suggestions on how to manage complications that may arise when managing skin grafts: Active bleeding - Sometimes the grafted area may begin to bleed excessively: 1. Apply pressure and notify the burns/plastics registrar, medical officer or CNC/NP Wound Care or Burns/Plastics. 2. If blood loss is large monitor observations closely. 3. Monitor the graft site for the formation of a haematoma. Non compliance with post operative orders: 1. Educate the patient on the importance of compliance with treatment, in order for best results for their skin graft. 2. Document clearly in the integrated notes the patients non compliance and actions taken. Pain: 1. Discuss donor site pain and pain management with the patient. 2. Educate the patient on the importance of regular analgesia. 3. Assess the patients pain and provide regular and break through pain as required. 4. If pain management is not adequate contact the Pain Team or medical team for review. 5. Document clearly actions in the integrated notes and on the NSCCAHS General Observations Chart.
Guideline Name Document ID Date Printed
30/01/07
Version No. Page No.
15 of 20
NORTHERN SYDNEY CENTRAL COAST HEALTH The controlled version of this document appears on the intranet
Infection of skin graft: Signs of infection: Onset of sudden or increased pain at the site Swelling Redness / cellulitis of the surrounding tissue Malodorous Sudden increase or change to purulent exudate
1. Change in general patient condition including: General Malaise Loss of appetite, in diabetic patients deterioration in glycaemic control Increased Temperature (WUWHS, 2008).
2. If infection is suspected inform the treating medical team. 3. Consider taking down the dressing and perform a wound swab of the infected graft site (see NSCCH Wound Swab Guideline http://intranet02.nsccahs.health.nsw.gov.au/policyprocedure/clinicalpatientcare/G E2007_005.pdf). 4. Redress the graft site with an appropriate dressing. 5. For advice on the relevant dressing and ongoing management contact the CNC/NP Wound Care or Burns/Plastics. 6. The general patient condition should be monitored. 7. Document clearly in the integrated notes after the procedure. Graft loss: 1. If the graft has not taken, is no longer present or viable contact the treating medical team, CNC/NP Wound Care or Burns/Plastics to inform them of the condition of the graft site. 2. A wound swab may be requested to see if there is an underlying infection. See NSCCAHS Wound Swab Guidelines
http://intranet02.nsccahs.health.nsw.gov.au/policyprocedure/clinicalpatientcare/G E2007_005.pdf 3. Redress the wound bed appropriately. 4. The CNC/NP Wound Care or Burns/Plastics may be contacted for advice on the relevant dressing and ongoing management. Document clearly in the integrated notes a wound swab has been taken and the signs and symptoms of infection.
Guideline Name Document ID Date Printed
30/01/07
Version No. Page No.
16 of 20
NORTHERN SYDNEY CENTRAL COAST HEALTH The controlled version of this document appears on the intranet
Graft site not healing: 1. If the graft site has a prolonged healing time (greater than 10 14 days) contact the CNC/NP Wound Care or Burns/Plastics or treating medical team for review. 2. A wound swab may be requested to check for infection, assess for other signs of infection including the patients temperature 3. The CNC/NP Wound Care or Burns/Plastics may be contacted for advice on the relevant dressing and ongoing management. If nutritional intake is poor assess the patients nutrition and obtain a dietician review. Document clearly in the integrated notes.
1.
Hypergranulation Tissue: Hypergranulation tissue is treated using a chemical cautery known as silver nitrate or other methods to treat hypergranulation as outlined in the NSCCAHS Wound Debridement Guidelines http://intranet02.nsccahs.health.nsw.gov.au/policyprocedure/clinicalpatientcare/PO20 08_034.pdf 2. 3. The wound is cleansed thoroughly prior to the procedure. The aim of the treatment is to reduce the hypergranulation tissue to the level of the skin. The CNC/NP Wound Care or Burns/Plastics may be contacted for advice and recommendations in regard to the treatment of hypergranulation tissue.
Guideline Name Document ID Date Printed
30/01/07
Version No. Page No.
17 of 20
NORTHERN SYDNEY CENTRAL COAST HEALTH The controlled version of this document appears on the intranet
Haematoma: 1. Bleeding from the wound bed may result in the formation of a haematoma. 2. This creates a separation of the graft from the wound bed therefore failure of the graft to vascularise resulting in loss of the graft. 3. Rolling the fluid out from under the edges of the graft is not advisable as it disrupts the adherence of the graft to the wound bed. 4. To treat a hematoma of a sheet graft, make a small incision over the collection and gently express the underlying contents. 5. This should only be attempted in consultation with the CNC/NP Wound Care or Burns/Plastics or treating medical team. 6. Hematomas that occur in split skin grafts are usually treated with BD or TDS saline soaked gauze to gently debride the hematoma. Consult with the CNC/NP Wound Care or Burns/Plastics or treating medical team for review or advice.
5.6 Healed skin graft care and scar management
Maturation of the graft and scaring is a progressive process taking up to 2 years to be remodelled. Patients should be educated on the following: 1. That wound contraction and remodelling occurs, which can continue up to 18 months post grafting. 2. The graft will become dry and scaly therefore the importance of applying a moisturiser to the grafted areas with a non-perfumed moisturiser (such as Dermaven or Sorbelene) should be reinforced. 3. To expect that the sensation of the grafted sites will be altered. 4. The importance of wearing sunscreen and to not expose their graft sites to excessive sun exposure as this will result in damage to the graft site.
Guideline Name Document ID Date Printed
30/01/07
Version No. Page No.
18 of 20
NORTHERN SYDNEY CENTRAL COAST HEALTH The controlled version of this document appears on the intranet
5. Compression garments may be used for large areas of skin grafts (see fig. 11). These are only used after consultation with the Burns and Plastics occupational therapist or
physiotherapist. 6. They are usually worn for a period of up to 2 years post grafting. The pressure garments are used to control hypertrophic scarring (see fig. 12) and contractures. The patient must be educated on the importance of compliance of the pressure garment. 7. Care must be taken when applying the garment to avoid any damage to fragile graft areas. If the patient experience problems with the pressure garment it must be reported back to the burn physiotherapist or occupational therapist trained in garment maintenance. Figure 12: Hypertrophic scaring. (Bailie & Wilson, 2002) 8. The Severe Burn Injury Unit (SBIU), RNSH Physiotherapist and Occupational Therapist can be contacted for information on 9926 8934. Figure 11: Pressure garment suit. (Second Skin, 2006)
Guideline Name Document ID Date Printed
30/01/07
Version No. Page No.
19 of 20
NORTHERN SYDNEY CENTRAL COAST HEALTH The controlled version of this document appears on the intranet
6.
References
Bailie, F. & Wilson, D., (2002). Early wound excision and grafting in Bosworth Bousfield, C (ed), Burn Trauma: Management and nursing care, 2nd edn, Whurr Publishers, London, pp. 142-157. Koljonen, V., Gerdin, B., Vuola, J. & Aili Low, J., (2007). Non expandable mesh grafts combine the advantages of mesh grafts and sheet grafts, Dermatologic Surgery, vol. 33, no. 7, pp. 831-834. McGregor, A.D & McGregor, I.A., (2000). Fundamental techniques of plastic surgery and their surgical applications, 10th edn, Churchill Livingstone, London. Salitas: Innovative Healthcare Solutions, (2007). Retrieved from 21/12/2007 from http://www.salitas.co.uk/ Second Skin. (2006), Second skin medical garments and splints, [brochure], Second Skin, Perth. World Union Wound Healing Societies (WUWHS), (2008). Wound Infection in Clinical Practice An International Consensus. International Wound Journal. 5(3):1-4.
7.
Acknowledgements
This document was developed in consultation Diane Elfleet and with the members of the NSCCHS Wound Care Committee. Their participation, feedback and comments in developing this document are appreciated and acknowledged. Photos used throughout this document were provided by Jan Darke and Melissa OBrien from their professional records. Consent was obtained from the patients prior to their publication.
Guideline Name Document ID Date Printed
30/01/07
Version No. Page No.
20 of 20
Anda mungkin juga menyukai
- DOH Ambulatory Surgical Clinic LTO at 1262015rev1Dokumen12 halamanDOH Ambulatory Surgical Clinic LTO at 1262015rev1al gul50% (2)
- Pressure Garments: A Manual on Their Design and FabricationDari EverandPressure Garments: A Manual on Their Design and FabricationBelum ada peringkat
- CHCCCS007 Learner Guide V1.1Dokumen71 halamanCHCCCS007 Learner Guide V1.1rasna kc100% (1)
- Course 1 Prefixation and SuffixationDokumen6 halamanCourse 1 Prefixation and SuffixationSárközi TiborBelum ada peringkat
- Skin Graft: Technique, Indications and OutcomesDokumen9 halamanSkin Graft: Technique, Indications and OutcomesIJAR JOURNALBelum ada peringkat
- Skin Grafting ManuscriptDokumen6 halamanSkin Grafting ManuscriptMa. Ydela MeradoresBelum ada peringkat
- Clinical Protocol For Wound Management 2013Dokumen17 halamanClinical Protocol For Wound Management 2013Moloce BeatriceBelum ada peringkat
- Skin - Grafts by Madhuri GoreDokumen112 halamanSkin - Grafts by Madhuri GoreAnonymous 8hVpaQdCtr100% (1)
- Keratin-Based Products For Effective Wound Care Management in Superficial and Partial Thickness Burns InjuriesDokumen7 halamanKeratin-Based Products For Effective Wound Care Management in Superficial and Partial Thickness Burns InjuriesAllium AdiBelum ada peringkat
- A Thoroughgoing Detail of Surgical Dressings PDFDokumen17 halamanA Thoroughgoing Detail of Surgical Dressings PDFFortune JournalsBelum ada peringkat
- Clinical Study: Vacuum Assisted Closure Therapy Versus Standard Wound Therapy For Open Musculoskeletal InjuriesDokumen9 halamanClinical Study: Vacuum Assisted Closure Therapy Versus Standard Wound Therapy For Open Musculoskeletal InjuriesAndika FahruroziBelum ada peringkat
- Suturing Procedures Guidance: School of Medicine, Dentistry & NursingDokumen36 halamanSuturing Procedures Guidance: School of Medicine, Dentistry & NursingPutri RamadaniBelum ada peringkat
- Qureshi 2019Dokumen8 halamanQureshi 2019Jefferson RuizBelum ada peringkat
- Incision and DrainageDokumen8 halamanIncision and DrainageAbraham ChiuBelum ada peringkat
- Skin Grafts PDFDokumen112 halamanSkin Grafts PDFalinutza_childBelum ada peringkat
- Skin Graft Techniques Khan2020Dokumen15 halamanSkin Graft Techniques Khan2020danielBelum ada peringkat
- Debridement YazdanpanahDokumen34 halamanDebridement YazdanpanahMohammadBelum ada peringkat
- Intra-Operative Nursing 2Dokumen10 halamanIntra-Operative Nursing 2gbongatBelum ada peringkat
- Burns - Skin Integrity, ImpairedDokumen2 halamanBurns - Skin Integrity, Impairedmakyofrancis20Belum ada peringkat
- Fixation of Split Skin Graft Using Cyanoacrylate Tissue Adhesive Versus Skin Stapling: A Comparative StudyDokumen4 halamanFixation of Split Skin Graft Using Cyanoacrylate Tissue Adhesive Versus Skin Stapling: A Comparative StudysindujasaravananBelum ada peringkat
- SESLHDGL 094 - Skin Traction Application and ManagementDokumen13 halamanSESLHDGL 094 - Skin Traction Application and Managementjamila jayBelum ada peringkat
- SkinGrafting-Rivera RobinDokumen15 halamanSkinGrafting-Rivera RobinMonette Abalos MendovaBelum ada peringkat
- Cryotherapy Treatment ProcedureDokumen6 halamanCryotherapy Treatment ProcedureBoobesh Venkata RamananBelum ada peringkat
- NPWT RENASYS and PICO Clinical GuidelinesDokumen78 halamanNPWT RENASYS and PICO Clinical GuidelinesAgung GinanjarBelum ada peringkat
- Piis1748681514001739 PDFDokumen9 halamanPiis1748681514001739 PDFsonuguptapeeyushBelum ada peringkat
- Updated Scar Management Practical Guidelines Non-IDokumen10 halamanUpdated Scar Management Practical Guidelines Non-IChilo PrimaBelum ada peringkat
- NICE - Percutaneous Ultrasound-Guided Microwave AblationDokumen5 halamanNICE - Percutaneous Ultrasound-Guided Microwave AblationMalekseuofi مالك السيوفيBelum ada peringkat
- SESLHDPR 400 - Wound Management of Hypergranulation Tissue - 0Dokumen7 halamanSESLHDPR 400 - Wound Management of Hypergranulation Tissue - 0MohammadBelum ada peringkat
- Incision and DrainageDokumen35 halamanIncision and DrainageVilma Delos Reyes100% (1)
- Wound Dressings Update: Carolina Weller, Geoff SussmanDokumen7 halamanWound Dressings Update: Carolina Weller, Geoff SussmanKevin AdrianBelum ada peringkat
- Free Flap Management 2020Dokumen7 halamanFree Flap Management 2020shreya dasBelum ada peringkat
- JBI - Wound ManagementDokumen4 halamanJBI - Wound ManagementBethanyBelum ada peringkat
- Management Open FractureDokumen2 halamanManagement Open FracturecatharinamBelum ada peringkat
- Metatarsophalangeal Joint Replacement of The Hallux PDF 1899863212945093Dokumen6 halamanMetatarsophalangeal Joint Replacement of The Hallux PDF 1899863212945093JanetBelum ada peringkat
- Sutures, Clips and StaplesDokumen19 halamanSutures, Clips and StaplesCárin AlvesBelum ada peringkat
- 3541 14379 2 PBDokumen8 halaman3541 14379 2 PBCraj RajBelum ada peringkat
- Nursing Interventions and Rationales For Impaired Tissue IntegrityDokumen3 halamanNursing Interventions and Rationales For Impaired Tissue Integrityshadow gonzalezBelum ada peringkat
- Skin GraftingDokumen3 halamanSkin GraftingTrish PangilinanBelum ada peringkat
- Dermal SubstitutesDokumen9 halamanDermal SubstitutesEsq. Nelson OduorBelum ada peringkat
- Makalah Makalah LalalalaDokumen4 halamanMakalah Makalah LalalalaDevia SuciyantiBelum ada peringkat
- BEDAH (Skin Graft)Dokumen7 halamanBEDAH (Skin Graft)Jose FoxBelum ada peringkat
- Wound CareDokumen17 halamanWound CareLestia AgustinaBelum ada peringkat
- Negative Pressure Wound TherapyDokumen9 halamanNegative Pressure Wound TherapySuharyonoBelum ada peringkat
- Incision and Drainage Procedure - UpToDate PDFDokumen1 halamanIncision and Drainage Procedure - UpToDate PDFLeslieBelum ada peringkat
- Efficacy of Leukocyte - and Platelet-Rich Fibrin in Wound Healing - A Randomized Controlled Clinical TrialDokumen11 halamanEfficacy of Leukocyte - and Platelet-Rich Fibrin in Wound Healing - A Randomized Controlled Clinical TrialLerdsin PlasticBelum ada peringkat
- Dermabrasion Again and AgainDokumen8 halamanDermabrasion Again and AgainBenazier Marcella BesmayaBelum ada peringkat
- Skin Graft Vs DC 8DRDokumen2 halamanSkin Graft Vs DC 8DRibraheemBelum ada peringkat
- Skin Grafting: Different Types of Skin GraftDokumen4 halamanSkin Grafting: Different Types of Skin GraftMohd HafidzieBelum ada peringkat
- 137394-Article Text-367387-1-10-20160609Dokumen2 halaman137394-Article Text-367387-1-10-20160609Luis GarciaBelum ada peringkat
- Jurnal PlastiksDokumen5 halamanJurnal PlastiksbdhBelum ada peringkat
- Utilizing Free Skin Grafts in The Repair of Surgical Wounds: Madalene C. Y. HengDokumen11 halamanUtilizing Free Skin Grafts in The Repair of Surgical Wounds: Madalene C. Y. HengDefri ChanBelum ada peringkat
- Standard Guidelines of Care - Keloids and Hypertrophic Scars (Somesh Gupta VK Sharma)Dokumen8 halamanStandard Guidelines of Care - Keloids and Hypertrophic Scars (Somesh Gupta VK Sharma)AuroraBelum ada peringkat
- Surgery Trans CheckedDokumen5 halamanSurgery Trans CheckedHaloula MIBelum ada peringkat
- JCM 11 03305Dokumen8 halamanJCM 11 03305Vainatheya AnanthBelum ada peringkat
- Wound Debridement (Adult, Neonatal, Peds) PDFDokumen4 halamanWound Debridement (Adult, Neonatal, Peds) PDFPangestu KelvinBelum ada peringkat
- NAME: - SKILLS NO: - BSN: - DateDokumen5 halamanNAME: - SKILLS NO: - BSN: - DateJenny AjocBelum ada peringkat
- Refractive Surgery Standards Dec 2004Dokumen7 halamanRefractive Surgery Standards Dec 2004dr_jrcBelum ada peringkat
- Surgical Site MarkingDokumen12 halamanSurgical Site Markingh1m4w4nBelum ada peringkat
- Treatment of Nipple Hypertrophy by A Simplified Reduction TechniqueDokumen7 halamanTreatment of Nipple Hypertrophy by A Simplified Reduction TechniqueАндрей ПетровBelum ada peringkat
- Skin GraftingDokumen22 halamanSkin GraftingKumar SuryavanshiBelum ada peringkat
- Flaps in Maxillofacial ReconstructionDokumen29 halamanFlaps in Maxillofacial ReconstructionJaspreet Kaur33% (3)
- Rental Receipt TemplateDokumen6 halamanRental Receipt Templatehawaalia534Belum ada peringkat
- Reupload Skin GraftDokumen33 halamanReupload Skin Grafthawaalia534Belum ada peringkat
- Practical 12. ReuploadDokumen13 halamanPractical 12. Reuploadhawaalia534Belum ada peringkat
- Reupload Skin Graft ManagementDokumen20 halamanReupload Skin Graft Managementhawaalia534100% (1)
- FOUR Score Instruction Guide For Application On MISH ICUDokumen2 halamanFOUR Score Instruction Guide For Application On MISH ICUMohamed Farouk El-FaresyBelum ada peringkat
- Test de Hormona ProlactinaDokumen31 halamanTest de Hormona ProlactinakemitaBelum ada peringkat
- Acupuncture With Manual and Electrical Stimulation For Labour Pain: A Two Month Follow Up of Recollection of Pain and Birth ExperienceDokumen9 halamanAcupuncture With Manual and Electrical Stimulation For Labour Pain: A Two Month Follow Up of Recollection of Pain and Birth ExperiencejayaBelum ada peringkat
- S O C R A T E S: History TakingDokumen5 halamanS O C R A T E S: History Takingsnanan100% (1)
- A Brief About Legal Services Authorities Act, 1987Dokumen3 halamanA Brief About Legal Services Authorities Act, 1987MINNU MINHAZBelum ada peringkat
- Arcadia Reptile 2018Dokumen32 halamanArcadia Reptile 2018marianpcbBelum ada peringkat
- Gejala Klinis Dan Diagnosis Banding MSDokumen33 halamanGejala Klinis Dan Diagnosis Banding MSEva FadilaBelum ada peringkat
- June 2022 Set 1 Test Paper - Do Not Let Parents DecideDokumen11 halamanJune 2022 Set 1 Test Paper - Do Not Let Parents DecideAISYAH ABDULLAHBelum ada peringkat
- Cartilage and OsteoarthritisDokumen374 halamanCartilage and OsteoarthritisItai IzhakBelum ada peringkat
- A Guide To Radio Frequency Hazards With Electric DetonatorsDokumen37 halamanA Guide To Radio Frequency Hazards With Electric Detonatorszix013Belum ada peringkat
- Admission MDS First CounsellingDokumen3 halamanAdmission MDS First CounsellingavninderBelum ada peringkat
- Topic: Magnesium Sulphate (Mgso4: Group 5Dokumen11 halamanTopic: Magnesium Sulphate (Mgso4: Group 5Wan Ahmad FaizFaizalBelum ada peringkat
- A-Plus Early Criticalcare Brochure Full 20130529 FinalDokumen18 halamanA-Plus Early Criticalcare Brochure Full 20130529 Finalnusthe2745Belum ada peringkat
- Etiology of Eating DisorderDokumen5 halamanEtiology of Eating DisorderCecillia Primawaty100% (1)
- Husky Air Compressor Operator ManualDokumen60 halamanHusky Air Compressor Operator ManualJ DavisBelum ada peringkat
- Tripod FractureDokumen45 halamanTripod Fracturekenn ParrochoBelum ada peringkat
- ONDANSENTRONDokumen2 halamanONDANSENTRONErza GenatrikaBelum ada peringkat
- CH 04 The Skeletal System (New)Dokumen85 halamanCH 04 The Skeletal System (New)alyssa bananBelum ada peringkat
- STP120 Instruction Manual 387718Dokumen42 halamanSTP120 Instruction Manual 387718Ottoniel HernándezBelum ada peringkat
- NIOS Sec PsychologyDokumen383 halamanNIOS Sec PsychologySujitha DhanarajBelum ada peringkat
- The Independent 21 February 2016Dokumen60 halamanThe Independent 21 February 2016artedlcBelum ada peringkat
- National Seminar BrochureDokumen2 halamanNational Seminar BrochureRamachandran ThalaBelum ada peringkat
- Local Honey Might Help Your AllergiesDokumen3 halamanLocal Honey Might Help Your AllergiesDaniel JadeBelum ada peringkat
- Parallel Session 1 The Disengagement of Statutory Instrument No.971 Allan SmillieDokumen12 halamanParallel Session 1 The Disengagement of Statutory Instrument No.971 Allan SmillieasdasdBelum ada peringkat
- Health Policy Notes: Harmonize and Strengthen Health Information SystemsDokumen6 halamanHealth Policy Notes: Harmonize and Strengthen Health Information SystemsJeffrey AngBelum ada peringkat
- Tendinopathy CourseDokumen3 halamanTendinopathy CourseGoranMarkovicBelum ada peringkat
- EPA Emission StandardsDokumen5 halamanEPA Emission StandardsSyed Zain AhmadBelum ada peringkat