Nursing Care Plans for Acute Pain, Hyperthermia, Activity Intolerance, and Infection Risk
Diunggah oleh
Nursidar Pascual MukattilDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Nursing Care Plans for Acute Pain, Hyperthermia, Activity Intolerance, and Infection Risk
Diunggah oleh
Nursidar Pascual MukattilHak Cipta:
Format Tersedia
I.
II. B. PLANNING (NURSING CARE PLANS)
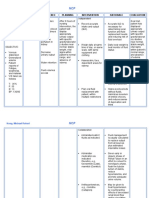
Problem # 1: ACUTE PAIN Assessm ent S: O O: The patient may manifest: > Pain on the gastric area >pain scale of 8/10 >(+) facial grimaces >(+) guarded behavior >restless ness >cold clammy skin >limited movemen t Nursing Diagnosis Acute pain Scientific Explanation acute pain starts with the stimulation of one or more of the many special sense receptors, called nociceptors, in the skin. These receptors receive information about tissue trauma or other events that can cause body damage. Two types of nerve fibers carry this information from the nociceptors to the spinal cord: Adelta fibers, which transmit information quickly and appear to be responsible for the acute sense of pain; and C-type fibers, which transmit impulses Objectives Short term: After 4 hours of nursing interventions, the patient will be able to verbalize a reduction of pain AEB decreased pain scale of 8/10 to 4/10, reduction of facial grimaces, guarding behavior ()cold clammy skin, and () restlessness. Intervention >Establish rapport. Rationale >To facilitate health care intervention and promote participation and compliance to treatment regimen. >To get baseline data and to note progress of patients condition. >To assist the client to explore methods of alleviation or control of pain. Listening to the patient respectfully and implying an alliance against pain help reduce anxiety. Expected outcome Short term: The patient shall have verbalized a reduction of pain AEB decreased pain scale of 6/10 to 4/10, reduction of facial grimaces, guarding behavior ()cold clammy skin, and () restlessness. Long term: The patient shall have verbalized a total relief of pain AEB absence of pain, ()
>Assess, monitor and record vital signs. >Encourage verbalization of feelings about the pain.
Long term: After 2 weeks of
>selffocusing >narrowe d focus
more slowly and may cause the nagging sense of pain. At the spinal cord, messages from nociceptors may be modulated by other spinal nerves that enhance or, more frequently, diminish the intensity of the pain stimulus. The impulse then travels to several parts of the brain. Some brain areas determine where the pain is and what is causing it, while other areas integrate the sensory information with the total state of the organism and produce the emotional sensation called pain.
nursing interventions, the patient will be able to verbalize a total relief of pain AEB absence of pain, () facial grimaces, () guarding behavior, can totally move without experiencing pain, () cold clammy skin and () restlessness.
>Note nonverbal pain cues.
>Non verbal cues may be both physiologic and psychological and may be used in conjunction with verbal cues to evaluate extent or severity of the problem. >Helpful in establishing diagnosis and treatment needs. >Careful analysis of pain characteristics aids in the differential diagnosis of pain. Systemic analysis prevents hasty and possibly inaccurate conclusions
facial grimaces, () guarding behavior, can totally move without experiencing pain, () cold clammy skin and () restlessness.
>Review factors.
>Analyze and document pain characteristics: precipitators, quality, region and radiation, severity, and time (frequency and duration).
about the quality or probable cause of pain. Standardized pain rating improves accuracy. >Work with the patient to identify the most effective ways to control pain. >Involving the patient in paincontrol strategies promotes a sense of mastery that reduces fears of helplessness or loss of control. >Patient may experience an exaggeration in pain or a decreased ability to tolerate painful stimuli if environmental, intrapersonal, or intrapsychic factors are further stressing
>Eliminate additional stressors or source of discomfort like environmental factors whenever possible.
>Provide rest
periods to facilitate comfort, sleep, and relaxation.
her. >Feeling wellrested increases tolerance of pain and the ability to cope with it. A quiet and clean environment is a measure geared towards facilitating rest. >Hot, moist compress has a penetrating effect. The warmth rushes blood to the surrounding area to promote healing. A cold compress may reduce total edema and promote numbing, thereby promoting comfort. >These
>Provide comfort measures such as hot or cold compress.
>Explore various behavioral pain-control
strategies including relaxation techniques and distraction techniques.
>Encourage to have adequate fluid intake and of nutritious foods rich in vitamin C, iron and protein. >Administer and document analgesics as ordered.
techniques reduce muscle tension, enhance rest, and promote a sense of wellbeing by stimulating the relaxation response. Distraction is helpful for brief episodes of pain, but may increase pain perception and fatigue after the distracting stimulus is removed. >Promotes faster wound healing.
>Nonnarcotic analgesics work peripherally, inhibiting
formation of prostaglandins and bradykinins. These are used to maintain acceptable level of pain.
PROBLEM #2: HYPERTHERMIA ASSESSMENT NURSING DIAGNOSIS Hyperthermi a SCIENTIFIC EXPLAINATIO N When the causative agent enters the body and invades the respiratory system, the inflammatory process is triggered releasing platelets, WBC, RBC, which produces exudates of fibrin, which enhances the spread of microorganism , causing infection. In response to infection, the individual WBC release pyrogens. OBJECTIVES INTERVENTIO NS 1. Establish Rapport RATIONALE EXPECTED OUTCOME Short term: After 4 of NI, the pts temperature shall drop 2. To establish baseline data of the pts from 38.4 C to 37 C.
S>
O> the patient manifested >Flushed skin >skin warm to touch >with body temperature of 38.4C -The patient may manifest >dehydration >Irritability
Short term: After 4 of NI, the pts temperature will drop from 38.4 C to 37 C
1. To gain trust and have a nurse patient relationship
2. Monitor VS q 4.
3. Provide TSB as a measure. Long term: After 2-3 days of NI, the patient will be free from hyperthermia. 4. Instruct SO to provide with loose clothing. 4. To release heat and to provide comfort 3. To lower pts temperature Long term: After 2-3 days of NI, the patient shall be free from hyperthermia.
5. Assess skin
These pyrogens affect the body temperatureregulating mechanism in the hypothalamus of the brain. As a consequence, heat production and conservation increase, a body temperature increases. Fever promotes activities of the immune system, such as phagocytosis, inhibits the growth of some microorganism .
temperature and color. 5. Warm, dry, flushed skin may indicate a fever.
6. Monitor WBC count. 6.Leucocytes indicate an inflammatory and infectious process presence. 7. Encourage fluid intake orally or intravenously as ordered. 8. Measure intake and 8. Determine 7. Replaces fluid lost by insensible loss and perspiration.
output.
fluid balance and need to increase fluid intake.
Problem #3 ACTIVITY INTOLERANCE r/t generalize weakness Assessme nt Nursing Diagnosis Scientific Explanation Objectives Intervention Rationale Expected outcome
S: O: Patient may manifest >limited movement >report of pain and discomfort upon movement >inability to perform self-care activities >weaknes s >fatigue
Activity Intolerance r/t generalize weakness
There is a limitation in independent, purposeful physical movement of the body or of one or more extremities due to weakness that the patient experiences brought about by decreased oxygen delivered to body tissues. This limits the patients mobility and is often exacerbated by movement leading to activity intolerance.
Short-term: After 4 hours of nursing interventions, the patient will be able to use identified techniques to enhance activity tolerance AEB decreased limited movement, and can perform selfcare activities with assistance.
>Establish rapport.
>To facilitate health care intervention and promote participation and compliance to treatment regimen. >To get baseline data and to note progress of patients condition. >To assess factors affecting current situation. >Pain limits mobility and is often exacerbated by movement. > To conserve energy and promote
>Assess, monitor and record vital signs.
The patient shall have identified techniques to enhance activity tolerance AEB decreased limited movement, and can perform self-care activities with assistance. Long-term: the patient shall have reported a measurabl e increase in activity tolerance AEB absence of limited movement, and can perform self-care
>Identify factors that could affect desired level of activity.
Long-term: After 2 weeks of nursing interventions, the patient will be able to report a measurable increase in activity tolerance AEB
>Before activity, observe for and if possible treat pain.
> Instruct client in unfamiliar activities
absence of limited movement, and can perform selfcare activities without assistance.
and in alternative ways of doing familiar activities. > Assist client/SO(s) with planning for changes that may become necessary. > Identify and discuss symptoms for which client needs to seek medical assistance/evaluation . > Refer to appropriate sources for assistance and/or equipments as needed. >Encourage to perform passive ROM exercises at least 2x a day.
safety. >To promote wellness.
activities without assistance.
> To provide for timely intervention.
> To sustain activity level.
>Inactivity rapidly contributed to muscle shortening and changes in periarticular and cartilaginous joint structure. These factors contribute to contracture and limitation
of movement. >To reduce fatigue. >Provide adequate rest periods. >Provide ample time to perform mobilityrelated tasks. >Encourage to participate in selfcare activities. >Limits fatigue, maximizing participation. >Enhances self-concept and sense of independence.
Problem# 4: RISK FOR INFECTION Assessem ent Nursing Diagnosi s Scientific Explanati on Objectives Intervention Rationale Evaluation
S:O O: Patient manifested : >(+) cold clammy skin > c low hemoglobi n and hematocrit count >poor personal hygiene Patient may manifest: >increased temperatur e >chills
Risk for spread of infection r/t inadequat e secondary defenses as evidenced by low hematocri t and hemoglobi n count.
Due to low count of hematocrit and hemoglobi n and poor hygiene, risk for infection is greater. The skin, which is the bodys first line of defense, wherein whose natural defense mechanis ms are inadequat e to protect the patient from exposures that occur throughout the course of living. Risk for
Short-term: After 4 hours of nursing interventions, the patient will be able to verbalize understanding of individual risk factors to prevent/reduce risk of infection AEB patient has demonstrated techniques/lifest yle changes to prevent/reduce risk of infection by improving personal hygiene, ()cold clammy skin Long-term: After 2 weeks of nursing interventions, the patient will be free from signs/symptoms of infection AEB maintenance of good personal
>Establish rapport.
>To facilitate health care intervention and promote participation and compliance to treatment regimen. >To get baseline data and to note progress of patients condition. >To assess causative/contributi ng factors. > A first-line defense against nosocomial infections.
>Assess, monitor and record vital signs. >Note risk factors for occurrence of infection. >Stress proper handwashing techniques by all caregivers between therapies/clients. > Monitor visitors/caregiver s. >Administer and monitor medication regimen and note the clients
Short-term: the patient shall have verbalized understanding of individual risk factors to prevent/reduce risk of infection AEB patient has demonstrated techniques/lifest yle changes to prevent/reduce risk of infection by improving personal hygiene, ()cold clammy skin
>To prevent exposure of the client. > To determine the effectiveness of therapy/presence of
Long-term: the patient shall have been free from signs/symptoms of infection AEB maintenance of good personal hygiene, () cold clammy skin
infection may occur when an organism invades a susceptibl e host.
hygiene, () cold clammy skin
response. > Administer prophylactic antibiotic. > Review individual nutritional needs and need for rest. >Instruct client/SO(s) in techniques to prevent the spread/occurrenc e of infection.
side-effects.
>To reduce/correct existing factors. >To promote wellness.
>To promote wellness.
Problem #5 RISK FOR IMBALANCED NUTRITION: LESS THAN BODY REQUIREMENTS
CUES S: O: The patient manifested: lack of appetit e inadeq uate intake of nutriti ous food >patients SO verbalization of a decrease in patients body weight r appear s pale and weak Patient may manifest: poo
NURSING DIAGNOSIS Risk for imbalanced nutrition: less than body requirement s
SCIENTIFIC EXPLANATION loss of appetite may also develop due to anemia, the demand for energy . Increase in the number of immature and ineffective lymphocytes will utilize the nutrients intended for the bodys needs, thus causing weight loss. Condition presented put the patient to the problem of risk for altered nutrition: less than body requirement related to anorexia.
DESIRED OUTCOME Short term: After 4 hrs of nursing interventions, the patient will demonstrate an increase in appetite AEB increased fluid and food intake. Long term: After 1 week of nursing interventions, the client will maintain optimal nutritious status AEB stabilized weight and increased fluid and food intake.
NURSING INTERVENTIONS Note patients daily total intake.
RATIONALE Reveal changes that should be made in patients dietary intake. Bowel sound may be diminished/ absent if the infection process is severe/ prolonged. Abdominal distention may occur as a result of air swallowing or reflect the influence of bacterial toxins on the GI tract. These measures may enhance intake even though appetite may be slow to return.
Auscultate bowel sounds. Observe/palpate for abnormalities distension.
EXPECTED OUTCOME Short term: the patient shall have demonstrated an increase in appetite AEB increased fluid and food intake. Long term: the client shall have maintained optimal nutritious status AEB stabilized weight and increased fluid and food intake.
Other than encouraging milk feeding, Provide small, frequent juices that are appealing to the patient. Evaluate general
r mu scl e ton e cap illar y fra gilit y
nutritional state, obtain baseline weight.
Presence of chronic condition or financial limitation can contribute to malnutrition, lowered resistance to infection, and/or delayed response to therapy. To enhance intake by decreasing negative stimuli. May have a negative effect on appetite. Rest decreases metabolic needs. There are increased metabolic needs secondary to fever and infectious process.
Promote pleasant, relaxing environment. Prevent/minimiz e unpleasant odors/sights. Limit activities.
Provide oral care
before drinking and after coughing.
Sputum can be foul tasting and decrease appetite.
Problem #6 : DISTURBED SLEEP PATTERN CUES NURSING DIAGNOSIS SCIENTIFIC EXPLANATION DESIRED OUTCOME NURSING INTERVENTIONS RATIONALE EXPECTED OUTCOME
S: O: pt. may manifest: >verbal complaints of difficulty falling asleep >restlessnes s >altered facial _expression (fatigued appearance) >verbal complaints of not feeling rested >irritability >dozing >yawning >difficulty in arousal >change in activity level
Disturbed sleep pattern r/t environmen tal factors e.g. noise AEB verbalizatio n of difficulty of sleeping.
Sleep is required to provide energy for physical and mental activities. The sleep-wake cycle is complex, consisting of different stages of consciousness. Disruption in the individuals usual diurnal pattern of sleep and wakefulness may be temporary or chronic. Such disruptions may result in both subjective distress and apparent impairment in functional activities. Sleep patterns can be affected by environment,
SHORT TERM: After 3 hours of NI, patient will able to have adequate rest AEB verbalization of feeling rested, and improvement in sleep pattern. LONG TERM: After 3 days of NI, patient will achieve optimal amounts of sleep AEB rested appearance, verbalization of feeling rested, and improvement in sleep pattern
Establish rapport.
To facilitate health care intervention and promote participation and compliance to treatment regimen. To have a comparative/bas eline data to note progress of condition. To assess sleeping pattern and problems encountered by the patient
Assess, monitor vital signs.
SHORT TERM: The patient shall have had adequate rest AEB verbalization of feeling rested, and improvement in sleep pattern. LONG TERM: The patient Shall have achieved optimal amounts of sleep AEB rested appearance, verbalization of feeling rested, and improvement in sleep pattern
Assess past patterns of sleep in normal environment: amount, bedtime rituals, depth, length, positions, aids and interfering agents. Identify factors that may facilitate or interfere with normal patterns. Instruct patients to follow a
To identify appropriate nursing interventions To facilitate sleeping patterns
especially in hospital critical care units.
consistent daily schedule for retiring and arising as possible. Instruct to avoid heavy meals, alcohol, caffeine, or smoking before retiring. Instruct to avoid large fluid intake before bedtime. This can alter in promoting sleep
To avoid in between waking at night and promote rest and sleep
Anda mungkin juga menyukai
- Journey To A DiagnosisDokumen4 halamanJourney To A DiagnosisMark HayesBelum ada peringkat
- Endocrine Disease Review NotesDokumen6 halamanEndocrine Disease Review NotesNursidar Pascual Mukattil100% (2)
- Personal Data SheetDokumen4 halamanPersonal Data SheetLeonil Estaño100% (7)
- Fluid Volume Excess (CRF)Dokumen4 halamanFluid Volume Excess (CRF)NursesLabs.com100% (1)
- Medical Abbreviation GuideDokumen2 halamanMedical Abbreviation GuideNursidar Pascual MukattilBelum ada peringkat
- NCPDokumen9 halamanNCPTracy Camille EscobarBelum ada peringkat
- Nursing Scientific Planning EvaluationDokumen10 halamanNursing Scientific Planning EvaluationCharmz_asherah100% (9)
- NCP TahbsoDokumen18 halamanNCP TahbsoKe EjieBelum ada peringkat
- Diabetes Mellitus: Global Burden and ManagementDokumen27 halamanDiabetes Mellitus: Global Burden and ManagementNursidar Pascual MukattilBelum ada peringkat
- Nursing Care Plan 1 DiagDokumen4 halamanNursing Care Plan 1 Diagguysornngam100% (1)
- NCPDokumen5 halamanNCPJusTin Cargason100% (1)
- Easy Way To Learn ABGsDokumen13 halamanEasy Way To Learn ABGsMunaim TahirBelum ada peringkat
- NCPDokumen7 halamanNCPMarius Clifford BilledoBelum ada peringkat
- Risk For Decreased Cardiac OutputDokumen3 halamanRisk For Decreased Cardiac OutputSid Artemis FriasBelum ada peringkat
- NCPDokumen3 halamanNCPranee diane0% (1)
- Diagnosis Planning Intervention Rationale EvaluationDokumen5 halamanDiagnosis Planning Intervention Rationale EvaluationMel Christian Baldoz100% (2)
- MSU-Sulu Nursing Informatics Guide to Computer HardwareDokumen13 halamanMSU-Sulu Nursing Informatics Guide to Computer HardwareNursidar Pascual MukattilBelum ada peringkat
- Nursing Theory Integration Enhances PracticeDokumen3 halamanNursing Theory Integration Enhances PracticeNursidar Pascual Mukattil100% (1)
- Step 2-3-Clinical Checklist: Behavioral Science (8 Videos 2 Hours 9 Minutes)Dokumen14 halamanStep 2-3-Clinical Checklist: Behavioral Science (8 Videos 2 Hours 9 Minutes)MILTHON DAVID DIAZ PUENTES67% (3)
- Mary Mount School of Koronadal Incorporated: Clinic CalendarDokumen2 halamanMary Mount School of Koronadal Incorporated: Clinic CalendarTeàcher Peach100% (2)
- NCP Liver CirrhosisDokumen7 halamanNCP Liver CirrhosisIris Jimenez-BuanBelum ada peringkat
- Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDokumen2 halamanAssessment Diagnosis Inference Planning Intervention Rationale EvaluationMr. whiteBelum ada peringkat
- NCP AnemiaDokumen1 halamanNCP Anemiamashup100% (3)
- NCP - Deficient Fluid VolumeDokumen2 halamanNCP - Deficient Fluid VolumerobbychuaBelum ada peringkat
- Osteomyelitis NCPDokumen5 halamanOsteomyelitis NCPFranzes Janina Sacramento Gabriel100% (8)
- NCP BleedingDokumen3 halamanNCP Bleedingapi-316491996Belum ada peringkat
- NURSING CARE PLAN - Myocardial Infarction Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDokumen4 halamanNURSING CARE PLAN - Myocardial Infarction Assessment Diagnosis Inference Planning Intervention Rationale Evaluationsweethoney220% (1)
- SDL1 NCP Case2Dokumen3 halamanSDL1 NCP Case2Alec AnonBelum ada peringkat
- Nursing Care Plan (NCP) For A Patient With Acute Renal FailureDokumen3 halamanNursing Care Plan (NCP) For A Patient With Acute Renal FailureKian HerreraBelum ada peringkat
- Renal Failure NCPDokumen3 halamanRenal Failure NCPJet Ray-Ann GaringanBelum ada peringkat
- Nursing Care Plan for Acute Renal FailureDokumen3 halamanNursing Care Plan for Acute Renal FailureKian Herrera100% (1)
- Hypertension Nursing Care PlanDokumen3 halamanHypertension Nursing Care PlanAsylla PajijiBelum ada peringkat
- Improve Activity Tolerance and Manage Nursing DiagnosesDokumen14 halamanImprove Activity Tolerance and Manage Nursing DiagnosesIbrahimWages100% (4)
- Nursing Care Plan 2Dokumen2 halamanNursing Care Plan 2Isabel Barredo Del MundoBelum ada peringkat
- Nursing Care Plan For AIDS HIVDokumen3 halamanNursing Care Plan For AIDS HIVFARAH MAE MEDINA100% (2)
- NCP - Activity IntoleranceDokumen3 halamanNCP - Activity Intolerancejanelee2824Belum ada peringkat
- Nursing Care Plan for Vitamin Deficiency AnemiaDokumen7 halamanNursing Care Plan for Vitamin Deficiency AnemiaShane Aileen Angeles100% (2)
- NCP Cholecystectomy RevisedDokumen7 halamanNCP Cholecystectomy RevisedMariquita Buenafe100% (4)
- NCP 2 and Soapie 1Dokumen5 halamanNCP 2 and Soapie 1narsD100% (1)
- Novilyn C. Pataray BSN - Ii Thalassemia Major: St. Paul College of Ilocos SurDokumen1 halamanNovilyn C. Pataray BSN - Ii Thalassemia Major: St. Paul College of Ilocos SurCharina Aubrey0% (1)
- Nur81 NCP GastroDokumen4 halamanNur81 NCP GastroJordan Gonzales100% (1)
- Nursing Assessment and Interventions for Acute Chest PainDokumen3 halamanNursing Assessment and Interventions for Acute Chest PainAjay SupanBelum ada peringkat
- CHED Handbook On Typology, OBE and ISADokumen90 halamanCHED Handbook On Typology, OBE and ISAAlfonse Sarmiento100% (2)
- NCPDokumen10 halamanNCPbabycheska08Belum ada peringkat
- NCP DRDokumen3 halamanNCP DRRhuwelyn Parantar PilapilBelum ada peringkat
- A Renal Failure (NCP)Dokumen2 halamanA Renal Failure (NCP)Julie Aranda Hapin100% (1)
- Novilyn C. Pataray BSN - Ii Sickle Cell Anemia: St. Paul College of Ilocos SurDokumen1 halamanNovilyn C. Pataray BSN - Ii Sickle Cell Anemia: St. Paul College of Ilocos SurCharina AubreyBelum ada peringkat
- Hyperthermia NCPDokumen3 halamanHyperthermia NCPJayr DiazBelum ada peringkat
- Nursing Care Plan Renal FailureDokumen11 halamanNursing Care Plan Renal Failurenosevad88850% (2)
- NCP Chest PainDokumen2 halamanNCP Chest PainCG Patron BamboBelum ada peringkat
- Care Plan ExampleDokumen2 halamanCare Plan Exampleincess27100% (1)
- Body Weakness NCPDokumen1 halamanBody Weakness NCPtwicetrashBelum ada peringkat
- Anemia NCPDokumen6 halamanAnemia NCPApril Jumawan ManzanoBelum ada peringkat
- Ncp-Ineffective Tissue Perfusion (Aortic Stenosis)Dokumen2 halamanNcp-Ineffective Tissue Perfusion (Aortic Stenosis)Daniel Vergara Arce67% (3)
- Risk For Fluid ImbalanceDokumen8 halamanRisk For Fluid Imbalanceapi-277522722100% (1)
- Assessment Explanation Planning Interventions Rationale Evaluation (AEPPIREDokumen11 halamanAssessment Explanation Planning Interventions Rationale Evaluation (AEPPIREGrape JuiceBelum ada peringkat
- Hypertension Nursing Care PlanDokumen1 halamanHypertension Nursing Care PlanSheila Mae Cabahug100% (1)
- NCP PROPER Pain and Decreased Cardiac OutputDokumen3 halamanNCP PROPER Pain and Decreased Cardiac OutputErienne Lae Manangan - CadalsoBelum ada peringkat
- NCPDokumen6 halamanNCPyupipsjamBelum ada peringkat
- NCPDokumen6 halamanNCPKyla Carbonel100% (1)
- NCP For DM1Dokumen2 halamanNCP For DM1Pau Hipol MadriagaBelum ada peringkat
- Myocardial Infarction NCPDokumen3 halamanMyocardial Infarction NCPlapistolero33% (3)
- CP Intestinal Obstruction Nursing Care PlanDokumen7 halamanCP Intestinal Obstruction Nursing Care PlanShiella Heart MalanaBelum ada peringkat
- NCP DobDokumen3 halamanNCP DobLester BuhayBelum ada peringkat
- CA - Amniotic Fluid EmbolismDokumen13 halamanCA - Amniotic Fluid EmbolismRodelen Maraño100% (2)
- Nursing care plan for client with UTI and feverDokumen3 halamanNursing care plan for client with UTI and feverTheresa AbrilloBelum ada peringkat
- Nursing Care PlanDokumen13 halamanNursing Care PlanCris Solis33% (3)
- Nursing Care Plan: IndependentDokumen2 halamanNursing Care Plan: IndependentAdhaBelum ada peringkat
- NCPDokumen3 halamanNCPWendy EscalanteBelum ada peringkat
- NCP For FrostbiteDokumen2 halamanNCP For FrostbiteRommar RomeroBelum ada peringkat
- Post-Op Pain Management Nursing Care PlanDokumen7 halamanPost-Op Pain Management Nursing Care Planمالك مناصرةBelum ada peringkat
- Nursing Care for Impaired MobilityTITLEPreventing Peripheral Neurovascular Issues TITLERelieving Acute Pain from InflammationDokumen4 halamanNursing Care for Impaired MobilityTITLEPreventing Peripheral Neurovascular Issues TITLERelieving Acute Pain from InflammationDaniel Garraton0% (1)
- Data AnalysisDokumen1 halamanData AnalysisNursidar Pascual MukattilBelum ada peringkat
- Data AnalysisDokumen1 halamanData AnalysisNursidar Pascual MukattilBelum ada peringkat
- Stats HandoutDokumen1 halamanStats HandoutNursidar Pascual MukattilBelum ada peringkat
- Pathophysilogy of CvaDokumen3 halamanPathophysilogy of CvaNursidar Pascual MukattilBelum ada peringkat
- Understanding Renal Failure and Its TypesDokumen17 halamanUnderstanding Renal Failure and Its TypesNursidar Pascual MukattilBelum ada peringkat
- LET Reviewer MathDokumen8 halamanLET Reviewer MathNursidar Pascual MukattilBelum ada peringkat
- November 2015 NLE Performance of SchoolsDokumen17 halamanNovember 2015 NLE Performance of SchoolsPRC Board100% (1)
- Two Types of Diabetes MellitusDokumen1 halamanTwo Types of Diabetes MellitusNursidar Pascual MukattilBelum ada peringkat
- StatisticsDokumen3 halamanStatisticsNursidar Pascual MukattilBelum ada peringkat
- Computers and NursingDokumen5 halamanComputers and NursingNursidar Pascual MukattilBelum ada peringkat
- Overview of Computers and Nursing Nursing InformaticsDokumen2 halamanOverview of Computers and Nursing Nursing InformaticsNursidar Pascual MukattilBelum ada peringkat
- OBE Presentation Department of NursingDokumen2 halamanOBE Presentation Department of NursingNursidar Pascual MukattilBelum ada peringkat
- Snellen Eye ExamDokumen5 halamanSnellen Eye ExamNursidar Pascual MukattilBelum ada peringkat
- OBE Presentation Department of NursingDokumen2 halamanOBE Presentation Department of NursingNursidar Pascual MukattilBelum ada peringkat
- Nursing InformaticsDokumen5 halamanNursing InformaticsNursidar Pascual MukattilBelum ada peringkat
- Computer 101Dokumen4 halamanComputer 101Nursidar Pascual MukattilBelum ada peringkat
- Blood Type Compatibility A, B, AB, ODokumen2 halamanBlood Type Compatibility A, B, AB, ONursidar Pascual MukattilBelum ada peringkat
- News Broadcasting ScriptDokumen8 halamanNews Broadcasting ScriptNursidar Pascual MukattilBelum ada peringkat
- Classroom Rules and RegulationsDokumen8 halamanClassroom Rules and RegulationsNursidar Pascual MukattilBelum ada peringkat
- Basic ISO Setting For DSLRDokumen1 halamanBasic ISO Setting For DSLRNursidar Pascual MukattilBelum ada peringkat
- Phenomenological Studies: Qualitative ResearchDokumen21 halamanPhenomenological Studies: Qualitative Researchshaer_nahyarBelum ada peringkat
- ABG Analysis in Simple WayDokumen1 halamanABG Analysis in Simple WayNursidar Pascual MukattilBelum ada peringkat
- Chapter 1 Lesson 1Dokumen8 halamanChapter 1 Lesson 1Aizel ManiagoBelum ada peringkat
- Occlusal Variations For Reconstructing The Natural DentitionDokumen5 halamanOcclusal Variations For Reconstructing The Natural DentitionPablo Gutiérrez Da VeneziaBelum ada peringkat
- S1.2 PPT DR - Taufik SungkarDokumen32 halamanS1.2 PPT DR - Taufik SungkarMuhammadIkhsanFadillahBelum ada peringkat
- ASEAN Minimum Common Competency Standards for Dental EducationDokumen8 halamanASEAN Minimum Common Competency Standards for Dental EducationFimma NaritasariBelum ada peringkat
- Dermatology Secrets Plus 4th Edition ReviewDokumen1 halamanDermatology Secrets Plus 4th Edition ReviewYoga Adi0% (2)
- A Myth About Anastomotic LeakDokumen3 halamanA Myth About Anastomotic LeakAvinash RoyBelum ada peringkat
- HPV: Infection, Prevention and Vaccination in India: Ritesh KumarDokumen6 halamanHPV: Infection, Prevention and Vaccination in India: Ritesh Kumarsandeep raiBelum ada peringkat
- ManuscriptDokumen13 halamanManuscriptMegbaruBelum ada peringkat
- List of Books - Pharmacology TitlesDokumen2 halamanList of Books - Pharmacology TitlesAsiya ZaidiBelum ada peringkat
- 09 Dear DoctorDokumen2 halaman09 Dear DoctorDanielle TorresBelum ada peringkat
- 2.3 Ferry Indriasmoko - CCA Overview Jogja 8AUG19Dokumen12 halaman2.3 Ferry Indriasmoko - CCA Overview Jogja 8AUG19Netty HerawatiBelum ada peringkat
- Treat Infected Fingernails (35 charactersDokumen5 halamanTreat Infected Fingernails (35 charactersNyimas Irina SilvaniBelum ada peringkat
- D-37/1, TTC MIDC, Turbhe, Navi Mumbai-400 703: ThyrocareDokumen1 halamanD-37/1, TTC MIDC, Turbhe, Navi Mumbai-400 703: ThyrocareKaran BaglaBelum ada peringkat
- HEADACHEDokumen3 halamanHEADACHERajithaHirangaBelum ada peringkat
- EudraCT Protocol Related Data DictionaryDokumen412 halamanEudraCT Protocol Related Data DictionaryremovableBelum ada peringkat
- Maternal 8Dokumen15 halamanMaternal 8shanikaBelum ada peringkat
- Caries TimelineDokumen11 halamanCaries TimelineManuelRomeroFBelum ada peringkat
- References DMDokumen2 halamanReferences DMAzka FathiyaBelum ada peringkat
- Prelim ProgrammeDokumen7 halamanPrelim Programmeasalizwa ludlalaBelum ada peringkat
- Nursing Informatics (Terminal Requirement 17)Dokumen1 halamanNursing Informatics (Terminal Requirement 17)Lyza MateoBelum ada peringkat
- Mortalidad Adultos MundoDokumen86 halamanMortalidad Adultos MundoJacob DavisBelum ada peringkat
- Cervical Checks in Labor ExplainedDokumen17 halamanCervical Checks in Labor ExplainedClaire Anne PunsalanBelum ada peringkat
- A-Plus Multi CriticalCare Provides Triple Protection For Up To 3 Critical IllnessesDokumen14 halamanA-Plus Multi CriticalCare Provides Triple Protection For Up To 3 Critical Illnessesnusthe2745Belum ada peringkat
- DACUM Competency Profile For Hemodialysis TechnicianDokumen5 halamanDACUM Competency Profile For Hemodialysis Technicianmanishbabu100% (1)
- Konsulta ItrDokumen1 halamanKonsulta ItrBarangay DanaoBelum ada peringkat
- Grammar in Use: Dentistry. Lecture PART 4Dokumen19 halamanGrammar in Use: Dentistry. Lecture PART 4Ariadne CordeletteBelum ada peringkat