Osteomyelitis
Diunggah oleh
Marius Clifford BilledoHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Osteomyelitis
Diunggah oleh
Marius Clifford BilledoHak Cipta:
Format Tersedia
BONE INFECTIONS: OSTEOMYELITIS
Bone infections are difficult to treat and eradicate. Their effects can be devastating; they can cause pain, disability, and deformity. Chronic bone infections may drain for years because of a sinus tract. This occurs when a passageway develops from an abscess or cavity within the bone to an opening through the skin.
What is Osteomyelitis? It is an infection in the bone that results in inflammation, necrosis, and formation of new bone. osteo refers to bones; and, myelo refers to marrow cavity. Thus, both of which are involved in the disease. It can be caused by a variety of microbial agents (most common in staphylococcus aureus) and situations, including:
An open injury to the bone, such as an open fracture with the bone ends piercing the skin. An infection from elsewhere in the body, such as pneumonia or a urinary tract infection that has spread to the bone through the blood (bacteremia, sepsis). A minor trauma, which can lead to a blood clot around the bone and then a secondary infection from seeding of bacteria. Bacteria in the bloodstream bacteremia (poor dentition), which is deposited in a focal (localized) area of the bone. This bacterial site in the bone then grows, resulting in destruction of the bone. However, new bone often forms around the site. A chronic open wound or soft tissue infection can eventually extend down to the bone surface, leading to a secondary bone infection.
Clinical Epidemiology: Osteomyelitis affects about two out of every 10,000 people. If left untreated, the infection can become chronic and cause a loss of blood supply to the affected bone. When this happens, it can lead to the eventual death of the bone tissue. Osteomyelitis can affect both adults and children. The bacteria or fungus that can cause osteomyelitis, however, differs among age groups. In adults, osteomyelitis often affects the vertebrae and the pelvis. In children, osteomyelitis usually affects the adjacent ends of long bones. Long bones (bones of the limbs) are large, dense bones that provide strength, structure, and mobility. They include the femur and tibia in the legs and the humerus and radius in the arms
A. Theory- Based Pathophysiology PREDISPOSING FACTOR > Age elderly
PRECIPITATING FACTOR > Obese or under nourished > Immuno-compromised > Medication:Long-term corticosteriod > Post operative surgical infection
Soft Tissue Infection
Direct bone contamination
Hematogenous spread
Warm Pain and tender Inflammation septicemia
Vascularity Swollen Edema
O: Fever S: Chills
Rapid pulse
General malaise
Thrombosis
Occlusion of BV
Ischemia
(Pressure) Necrosis (Sequetrum)
Abscess formation
Pulsating pain
Not easily liquefy and drain Extends to the periosteum
Infection up to adjacent soft tissue and joints
does not heal
Involucrum forms Athralgia Chronic Osteomyelitis
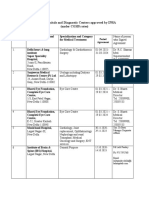
III. DIAGNOSTIC EXAMS To diagnose osteomyelitis, the doctor will first perform a history, review of systems, and a complete physical examination. In doing so, the physician will look for signs or symptoms of soft tissue and bone tenderness and possibly swelling and redness. The doctor will also ask you to describe your symptoms and will evaluate your personal and family medical history. The doctor can then order any of the following tests to assist in confirming the diagnosis: Blood tests: When testing the blood, measurements are taken to confirm an infection: a CBC (complete blood count), which will show if there is an increased white blood cell count; an ESR (erythrocyte sedimentation rate); and/or CRP (C-reactive protein) in the bloodstream, which detects and measures inflammation in the body. Blood culture: A blood culture is a test used to detect bacteria. A sample of blood is taken and then placed into an environment that will support the growth of bacteria. By allowing the bacteria to grow, the infectious agent can then be identified and tested against different antibiotics in hopes of finding the most effective treatment. Needle aspiration: During this test, a needle is used to remove a sample of fluid and cells from the vertebral space, or bony area. It is then sent to the lab to be evaluated by allowing the infectious agent to grow on media. Biopsy: A biopsy (tissue sample) of the infected bone PREVENTION OF OSTEOMYELITIS may be taken and tested for signs of an invading Prevention of osteomyelitis is the organism. goal. Elective orthopedic surgery should Bone scan: During this test, a small amount of be postponed if the patient has a current Technetium-99 pyrophosphate, a radioactive infection (eg, urinary tract infection, sore material, is injected intravenously into the body. If throat) or a recent history of infection. the bone tissue is healthy, the material will spread in During orthopedic surgery, a uniform fashion. However, a tumor or infection in careful attention is paid to the surgical the bone will absorb the material and show an environment and to techniques to increased concentration of the radioactive material, decrease direct bone contamination. which can be seen with a special camera that Prophylactic antibiotics, administered to produces the images on a computer screen. The scan achieve adequate tissue levels at the time can help your doctor detect these abnormalities in of surgery and for 24 hours after surgery, their early stages, when X-ray findings may only are helpful. Urinary catheters and drains show normal findings. are removed as soon as possible to decrease the incidence of hematogenous IV. MANAGEMENT spread of infection. A. Medical Management Treatment of focal infections The initial goal of therapy is to control and halt the diminishes hematogenous spread. Aseptic infective process. Antibiotic therapy depends on the results postoperative wound care reduces the of blood and wound cultures. Frequently, the infection is incidence of superficial infections and caused by more than one pathogen. General supportive osteomyelitis. Prompt management of measures (eg, hydration, diet high in vitamins and protein, soft tissue infections reduces extension of correction of anemia) should be instituted. infection to the bone. The area affected with osteomyelitis is immobilized to When patients who have had decrease discomfort and to prevent pathologic fracture of joint replacement surgery undergo dental the weakened bone. Warm wet soaks for 20 minutes several procedures or other invasive procedures times a day may be prescribed to increase circulation. (eg, cystoscopy), prophylactic antibiotics are frequently recommended. PHARMACOLOGIC THERAPY As soon as the culture specimens are obtained, IV antibiotic therapy begins, based on the assumption that infection results from a staphylococcal organism that is sensitive to a semisynthetic penicillin or cephalosporin. The aim is to control the infection before the blood supply to the area diminishes as a result of thrombosis. Around-the-clock dosing is necessary to achieve a sustained high therapeutic blood level of the antibiotic. An
antibiotic to which the causative organism is sensitive is prescribed after results of the culture and sensitivity studies are known. IV antibiotic therapy continues for 3 to 6 weeks. After the infection appears to be controlled, the antibiotic may be administered orally for up to 3 months. To enhance absorption of the orally administered medication, antibiotics should not be administered with food. B. Surgical Management If the patient does not respond to antibiotic therapy, the infected bone is surgically exposed, the purulent and necrotic material is removed, and the area is irrigated with sterile saline solution. Antibiotic-impregnated beads may be placed in the wound for direct application of antibiotics for 2 to 4 weeks. IV antibiotic therapy is continued. In chronic osteomyelitis, antibiotics are adjunctive therapy to surgical dbridement. A sequestrectomy (removal of enough involucrum to enable the surgeon to remove the sequestrum) is performed. In many cases, sufficient bone is removed to convert a deep cavity into a shallow saucer (saucerization). All dead, infected bone and cartilage must be removed before permanent healing can occur. A closed suction irrigation system may be used to remove debris. Wound irrigation using sterile physiologic saline solution may be performed for 7 to 8 days. The wound is either closed tightly to obliterate the dead space or packed and closed later by granulation or possibly by grafting. The dbrided cavity may be packed with cancellous bone graft to stimulate healing. With a large defect, the cavity may be filled with a vascularized bone transfer or muscle flap (in which a muscle is moved from an adjacent area with blood supply intact). These microsurgery techniques enhance the blood supply. The improved blood supply facilitates bone healing and eradication of the infection. These surgical procedures may be staged over time to ensure healing. Because surgical dbridement weakens the bone, internal fixation or external supportive devices may be needed to stabilize or support the bone to prevent pathologic fracture. C. Nursing Management NURSING PROCESS IN OSTEOMYELITIS Assessment The patient reports an acute onset of signs and symptoms (eg, localized pain, swelling, erythema, fever) or recurrent drainage of an infected sinus with associated pain, swelling, and low-grade fever. The nurse assesses the patient for risk factors (eg, older age, diabetes, long-term corticosteroid therapy) and for a history of previous injury, infection, or orthopedic surgery. The patient avoids pressure on the area and guards movement. In acute hematogenous osteomyelitis, the patient exhibits generalized weakness due to the systemic reaction to the infection. Physical examination reveals an inflamed, markedly swollen, warm area that is tender. Purulent drainage may be noted. The patient has an elevated temperature. With chronic osteomyelitis, the temperature elevation may be minimal, occurring in the afternoon or evening. Nursing Diagnoses Based on the nursing assessment data, nursing diagnoses for the patient with osteomyelitis may include the following: Acute pain related to inflammation and swelling Impaired physical mobility related to pain, use of immobilization devices, and weight-bearing limitations Risk for extension of infection: bone abscess formation Deficient knowledge related to the treatment regimen Planning and Goals The patients goals may include relief of pain, improved physical mobility within therapeutic limitations, control and eradication of infection, and knowledge of treatment regimen. Nursing Interventions
RELIEVING PAIN The affected part may be immobilized with a splint to decrease pain and muscle spasm. The nurse monitors the neurovascular status of the affected extremity. The wounds are frequently very painful, and the extremity must be handled with great care and gentleness. Elevation reduces swelling and associated discomfort. Pain is controlled with prescribed analgesics and other pain reducing techniques. IMPROVING PHYSICAL MOBILITY Treatment regimens restrict activity. The bone is weakened by the infective process and must be protected by immobilization devices and by avoidance of stress on the bone. The patient must understand the rationale for the activity restrictions. The joints above and below the affected part should be gently placed through their range of motion. The nurse encourages full participation in ADLs within the physical limitations to promote general well-being. CONTROLLING THE INFECTIOUS PROCESS The nurse monitors the patients response to antibiotic therapy and observes the IV access site for evidence of phlebitis, infection, or infiltration. With long-term, intensive antibiotic therapy, the nurse monitors the patient for signs of superinfection (eg, oral or vaginal candidiasis, loose or foul-smelling stools). If surgery was necessary, the nurse takes measures to ensure adequate circulation (wound suction to prevent fluid accumulation, elevation of the area to promote venous drainage, avoidance of pressure on grafted area), to maintain needed immobility, and to comply with weight-bearing restrictions. The nurse changes dressings using aseptic technique to promote healing and to prevent cross-contamination. The nurse continues to monitor the general health and nutrition of the patient. A diet high in protein and vitamin C ensures a positive nitrogen balance and promotes healing. The nurse encourages adequate hydration as well. PROMOTING HOME AND COMMUNITY-BASED CARE Teaching Patients Self-Care The patient and family must learn and recognize the importance of strictly adhering to the therapeutic regimen of antibiotics and preventing falls or other injuries that could result in bone fracture. The patient needs to know how to maintain and manage the IV access and IV administration equipment in the home. Medication education includes medication name, dosage, frequency, administration rate, safe storage and handling, adverse reactions, and necessary laboratory monitoring. In addition, aseptic dressing and warm compress techniques are taught. The nurse carefully monitors the patient for the development of additional painful areas or sudden increases in body temperature. The nurse instructs the patient and family to observe and report elevated temperature, drainage, odor, increased inflammation, adverse reactions, and signs of superinfection. Continuing Care Management of osteomyelitis, including wound care and IV antibiotic therapy, is usually performed at home. The patient must be medically stable, physically able, and motivated to adhere strictly to the therapeutic regimen of antibiotic therapy. The home care environment needs to be conducive to promotion of health and to the requirements of the therapeutic regimen. If warranted, the nurse completes a home assessment to determine the patients and familys abilities regarding continuation of the therapeutic regimen. If the patients support system is questionable or if the patient lives alone, a home care nurse may be needed to assist with intravenous administration of the antibiotics. The nurse monitors the patient for response to the treatment, signs and symptoms of superinfections, and adverse drug reactions. The nurse stresses the importance of follow-up health care appointments. Evaluation EXPECTED PATIENT OUTCOMES Expected patient outcomes may include:
1. Experiences pain relief a. Reports decreased pain b. Experiences no tenderness at site of previous infection c. Experiences no discomfort with movement 2. Increases physical mobility a. Participates in self-care activities b. Maintains full function of unimpaired extremities c. Demonstrates safe use of immobilizing and assistive devices d. Modifies environment to promote safety and to avoid falls 3. Shows absence of infection a. Takes antibiotic as prescribed b. Reports normal temperature c. Exhibits no swelling d. Reports absence of drainage e. Laboratory results indicate normal white blood cell count and sedimentation rate f. Wound cultures are negative 4. Complies with therapeutic plan a. Takes medications as prescribed b. Protects weakened bones c. Demonstrates proper wound care d. Reports signs and symptoms of complications promptly e. Eats a diet that is high in protein and vitamin C f. Keeps follow-up health appointments g. Reports increased strength h. Reports no elevation of temperature or recurrence of pain, swelling, or other symptoms at the site
References / Sources: Smeltzer, Suzzane C., et. al. 2010, Brunner and Suddarths Textbook of Medical- Surgical Nursing. 12th edition, Lippincott Williams and Wilkins. http://www.nlm.nih.gov/medlineplus/ency/article/000437.htm http://healthfiles.net/disease/category/o/
Anda mungkin juga menyukai
- Emr408 A2 KL MarkedDokumen21 halamanEmr408 A2 KL Markedapi-547396509Belum ada peringkat
- Casestudy OsteomyelitisDokumen52 halamanCasestudy OsteomyelitisMJ Amarillo84% (19)
- Ans KeyDokumen36 halamanAns KeyMarius Clifford BilledoBelum ada peringkat
- 2013 Observer - Applicant FormsDokumen11 halaman2013 Observer - Applicant FormsshengzhoumiBelum ada peringkat
- OsteomyelitisDokumen8 halamanOsteomyelitisMargarette Lopez0% (1)
- OSTEOMYELITISDokumen3 halamanOSTEOMYELITISsweetangelBelum ada peringkat
- IntroductionDokumen12 halamanIntroductionKenn yahweexBelum ada peringkat
- Osteomyelitis Report Orthopedic NursingDokumen15 halamanOsteomyelitis Report Orthopedic NursingSienaBelum ada peringkat
- Case Study MHPTDokumen10 halamanCase Study MHPTHalfIeyzBelum ada peringkat
- OsteomyelitisDokumen9 halamanOsteomyelitisTineLawrenceBelum ada peringkat
- OsteomelitisDokumen4 halamanOsteomelitisHidayu AliasBelum ada peringkat
- OsteomyelitisDokumen7 halamanOsteomyelitis4kscribd100% (1)
- Osteomyelitis2 200610201550Dokumen46 halamanOsteomyelitis2 200610201550Lolo Toto100% (1)
- OSTEOMYELITISDokumen28 halamanOSTEOMYELITISMuhammed sherbinBelum ada peringkat
- OSTEOMYELITISDokumen4 halamanOSTEOMYELITISGanah PeterBelum ada peringkat
- OsteomyelitisDokumen23 halamanOsteomyelitisGail ZantuaBelum ada peringkat
- Osteomyelitis: ClassificationDokumen5 halamanOsteomyelitis: Classificationthanuja mathewBelum ada peringkat
- Bone DisordersDokumen4 halamanBone Disorderskierz23Belum ada peringkat
- Osteomyelitis 2Dokumen11 halamanOsteomyelitis 2Ivan OngBelum ada peringkat
- What Is Osteomyelitis?: Staphylococcus AureusDokumen3 halamanWhat Is Osteomyelitis?: Staphylococcus AureusWilliam D. NarvaezBelum ada peringkat
- Definition of OsteomyelitisDokumen3 halamanDefinition of OsteomyelitisRey Gabriel Advincula GranadaBelum ada peringkat
- OsteomyelitisDokumen3 halamanOsteomyelitisHabib IrwanBelum ada peringkat
- Acute Chronic: OsteomyelitisDokumen5 halamanAcute Chronic: OsteomyelitisRizma AdliaBelum ada peringkat
- MOR 2152 SiapDokumen11 halamanMOR 2152 SiapMohamad RaisBelum ada peringkat
- OsteomyelitisDokumen5 halamanOsteomyelitisCarlo CautonBelum ada peringkat
- OsteomielitisDokumen104 halamanOsteomielitisConstantia Rosa PattiselannoBelum ada peringkat
- OsteomyelitisDokumen11 halamanOsteomyelitisLorebell100% (7)
- Salter EnglishDokumen3 halamanSalter EnglishAndyno SanjayaBelum ada peringkat
- Septic ArthritisDokumen8 halamanSeptic ArthritisLorebell100% (2)
- Septic Arthritis & OsteomyelitisDokumen42 halamanSeptic Arthritis & OsteomyelitisCabdi WaliBelum ada peringkat
- OsteomyelitisDokumen3 halamanOsteomyelitisCamille Lacson CayabyabBelum ada peringkat
- OsteomyelitisDokumen47 halamanOsteomyelitisArmand Al HaraaniBelum ada peringkat
- Etiology: Acute Hematogenous Osteomyelitis Subacute Osteomyelitis Chronic OsteomyelitisDokumen42 halamanEtiology: Acute Hematogenous Osteomyelitis Subacute Osteomyelitis Chronic OsteomyelitisNoe-pal DynmBelum ada peringkat
- OsteomyelitisDokumen3 halamanOsteomyelitisIanne Merh100% (1)
- Osteomyelitis: Dr. Sunil Pahari 2 Year Resident Department of Orthopedics Yangtze UniversityDokumen48 halamanOsteomyelitis: Dr. Sunil Pahari 2 Year Resident Department of Orthopedics Yangtze UniversityPercy Linares MorilloBelum ada peringkat
- Septicarthritis 110426090729 Phpapp02Dokumen21 halamanSepticarthritis 110426090729 Phpapp02Diana MayasariBelum ada peringkat
- Askep OsteomielitisDokumen13 halamanAskep Osteomielitisuciha_herhyBelum ada peringkat
- Lo MSK 5-2Dokumen5 halamanLo MSK 5-2FirmanHidayatBelum ada peringkat
- Osteomyelitis Word FileDokumen6 halamanOsteomyelitis Word FileCxarina RamirezBelum ada peringkat
- Osteomyelitis HandoutDokumen4 halamanOsteomyelitis HandoutJazzmin Angel ComalingBelum ada peringkat
- VV V V V VV V VVVVVVVV VVVVVVVV V VVVVV VVVVVV VDokumen4 halamanVV V V V VV V VVVVVVVV VVVVVVVV V VVVVV VVVVVV VCedie BarcaBelum ada peringkat
- Casestudy OsteomyelitisDokumen52 halamanCasestudy OsteomyelitisJoshua Caacbay PaningbatanBelum ada peringkat
- Chapter 10Dokumen32 halamanChapter 10Henderi SaputraBelum ada peringkat
- Septic Arthritis: Briones, Hershey C. BSN - IiiDokumen8 halamanSeptic Arthritis: Briones, Hershey C. BSN - IiiHershey Cordero BrionesBelum ada peringkat
- OsteomylitisDokumen11 halamanOsteomylitisSri AgustinaBelum ada peringkat
- Casestudy OsteomyelitisDokumen52 halamanCasestudy OsteomyelitisMrLarry DolorBelum ada peringkat
- Bone Infection & TumorDokumen49 halamanBone Infection & TumorAhmed AbdurahmanBelum ada peringkat
- OsteomyelitisDokumen32 halamanOsteomyelitisAndi Wija Indrawan PangerangBelum ada peringkat
- Acute and Chronic Osteomyelitis-1Dokumen63 halamanAcute and Chronic Osteomyelitis-1Cati Moraru100% (1)
- Osteomylities DonDokumen32 halamanOsteomylities DonNatunga RonaldBelum ada peringkat
- OsteomylitisDokumen48 halamanOsteomylitissamar yousif mohamed100% (1)
- Case Report Suppurative OsteomyelitisDokumen5 halamanCase Report Suppurative OsteomyelitisAngela KartonoBelum ada peringkat
- Neonatal Surgical InfectionDokumen43 halamanNeonatal Surgical InfectionAhmad Abu KushBelum ada peringkat
- Mss InfectionDokumen41 halamanMss InfectionZelalem AbrhamBelum ada peringkat
- General OrthopaedicsDokumen50 halamanGeneral Orthopaedicsضبيان فرحانBelum ada peringkat
- Infeksi Dalam OrthopaediDokumen35 halamanInfeksi Dalam OrthopaediFarry DoankBelum ada peringkat
- Bone Infection, (Osteomyelitis) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandBone Infection, (Osteomyelitis) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Peri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentDari EverandPeri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentBelum ada peringkat
- Bone and Joint Infections: From Microbiology to Diagnostics and TreatmentDari EverandBone and Joint Infections: From Microbiology to Diagnostics and TreatmentBelum ada peringkat
- Female Urinary Tract Infections in Clinical PracticeDari EverandFemale Urinary Tract Infections in Clinical PracticeBob YangBelum ada peringkat
- Transverse Myelitis, A Simple Guide To The Condition, Treatment And Related DiseasesDari EverandTransverse Myelitis, A Simple Guide To The Condition, Treatment And Related DiseasesPenilaian: 5 dari 5 bintang5/5 (1)
- Fashion ShowDokumen2 halamanFashion ShowMarius Clifford BilledoBelum ada peringkat
- Date/ Time Activity Venue Persons Involve: Barangay PoblacionDokumen5 halamanDate/ Time Activity Venue Persons Involve: Barangay PoblacionMarius Clifford BilledoBelum ada peringkat
- Mr. Romeo Calderon and Mrs. Perla Caldero. Mr. Emanual Peralta Sr. and Mrs. Josefina PeraltaDokumen4 halamanMr. Romeo Calderon and Mrs. Perla Caldero. Mr. Emanual Peralta Sr. and Mrs. Josefina PeraltaMarius Clifford BilledoBelum ada peringkat
- 15 Health Indicators SeptemberDokumen1 halaman15 Health Indicators SeptemberMarius Clifford BilledoBelum ada peringkat
- 2016 June Case StudyDokumen8 halaman2016 June Case StudyMarius Clifford BilledoBelum ada peringkat
- Evaluation Form For GPBP Project Briefs (DOH) : Name of LGUDokumen3 halamanEvaluation Form For GPBP Project Briefs (DOH) : Name of LGUMarius Clifford BilledoBelum ada peringkat
- Nursing Care Plan: ProblemDokumen4 halamanNursing Care Plan: ProblemMarius Clifford BilledoBelum ada peringkat
- NCPDokumen4 halamanNCPMarius Clifford BilledoBelum ada peringkat
- Ans KeyDokumen63 halamanAns KeyMarius Clifford BilledoBelum ada peringkat
- Peer Facis - bencHMARKING (BSAccountancy)Dokumen7 halamanPeer Facis - bencHMARKING (BSAccountancy)Marius Clifford BilledoBelum ada peringkat
- DRUG Study FormatDokumen1 halamanDRUG Study FormatMarius Clifford BilledoBelum ada peringkat
- NCPDokumen4 halamanNCPMarius Clifford BilledoBelum ada peringkat
- DedicationDokumen1 halamanDedicationMarius Clifford BilledoBelum ada peringkat
- MariusDokumen5 halamanMariusMarius Clifford BilledoBelum ada peringkat
- Rabbit HoleDokumen4 halamanRabbit HoleMarius Clifford BilledoBelum ada peringkat
- 3G Standard Bearer Is New SC PrexyDokumen1 halaman3G Standard Bearer Is New SC PrexyMarius Clifford BilledoBelum ada peringkat
- Drug Study: 1.metronidazoleDokumen4 halamanDrug Study: 1.metronidazoleMarius Clifford BilledoBelum ada peringkat
- Kriyakala AvastaDokumen13 halamanKriyakala Avastakundagol100% (1)
- Trypsin ChymotrypsinDokumen6 halamanTrypsin ChymotrypsinKalpana Shubhangi BhedaBelum ada peringkat
- Managerial Epidemiology Concepts and Case, 2d Ed.: Full TextDokumen2 halamanManagerial Epidemiology Concepts and Case, 2d Ed.: Full TextlovesunsetBelum ada peringkat
- Aerobic Exercise Dos and DontsDokumen2 halamanAerobic Exercise Dos and DontsSandy NodadoBelum ada peringkat
- Date/Hour of Shift Focus Note ProgressDokumen2 halamanDate/Hour of Shift Focus Note Progressako at ang exoBelum ada peringkat
- CSHP TEMPLATE (1) - NewDokumen14 halamanCSHP TEMPLATE (1) - NewLucky JavellanaBelum ada peringkat
- June 2021Dokumen90 halamanJune 2021SEIYADU IBRAHIM KBelum ada peringkat
- Mitchell H. Katz-Evaluating Clinical and Public Health Interventions - A Practical Guide To Study Design and Statistics (2010)Dokumen176 halamanMitchell H. Katz-Evaluating Clinical and Public Health Interventions - A Practical Guide To Study Design and Statistics (2010)Lakshmi SethBelum ada peringkat
- 21 Masterclass NLE Gapuz 2 - HANDOUTSDokumen16 halaman21 Masterclass NLE Gapuz 2 - HANDOUTSLimuel dale CaldezBelum ada peringkat
- Jurnal InternasionalDokumen110 halamanJurnal InternasionalRafi DevianaBelum ada peringkat
- Primitive ReflexesDokumen10 halamanPrimitive Reflexesbun_yulianaBelum ada peringkat
- Marriage and Later PartDokumen25 halamanMarriage and Later PartDeepak PoudelBelum ada peringkat
- Msds - AdditiveDokumen9 halamanMsds - AdditivedanalabBelum ada peringkat
- List of Private Hospitals and Diagnostic Centers Approved by INSADokumen16 halamanList of Private Hospitals and Diagnostic Centers Approved by INSAvijay sainiBelum ada peringkat
- MAPEH 7 3rd Summative TestDokumen5 halamanMAPEH 7 3rd Summative TestFerlyn Bautista Pada100% (1)
- NegOr Q4 MAPEH7 Module4a v2Dokumen12 halamanNegOr Q4 MAPEH7 Module4a v2fauralaurenceBelum ada peringkat
- Platelet in DengueDokumen5 halamanPlatelet in Denguekarina nilasariBelum ada peringkat
- DM Infectious DiseasesDokumen20 halamanDM Infectious DiseasesVasishta NadellaBelum ada peringkat
- Education For AllDokumen4 halamanEducation For AllNamrata SaxenaBelum ada peringkat
- Determinan Gejala Mental Emosional Pelajar SMP-SMA Di Indonesia Tahun 2015Dokumen11 halamanDeterminan Gejala Mental Emosional Pelajar SMP-SMA Di Indonesia Tahun 2015NurLestariBelum ada peringkat
- BibliographyDokumen2 halamanBibliographyelvie21Belum ada peringkat
- A. Classification and Characteristics of Diabetes MellitusDokumen6 halamanA. Classification and Characteristics of Diabetes MellitusNicole Villanueva, BSN - Level 3ABelum ada peringkat
- Deep Sleep ExperimentsDokumen12 halamanDeep Sleep ExperimentsCristina Lemoing100% (1)
- Basic Nutrition: Ma - Aileen C. Carating RNDDokumen13 halamanBasic Nutrition: Ma - Aileen C. Carating RNDspaspanBelum ada peringkat
- San Antonio and Bexar County Petition For TRO Against Gov. Abbott Over Local Control of COVID-19 Prevention EffortsDokumen29 halamanSan Antonio and Bexar County Petition For TRO Against Gov. Abbott Over Local Control of COVID-19 Prevention EffortsKENS 5Belum ada peringkat
- Farmakologi Penyakit-Penyakit Degenerasi Tulang Dan SendiDokumen19 halamanFarmakologi Penyakit-Penyakit Degenerasi Tulang Dan SendiCici MastaBelum ada peringkat
- Case 2 - The Global Biopharmaceutical IndustryDokumen5 halamanCase 2 - The Global Biopharmaceutical IndustryTran Bao DuongBelum ada peringkat
- Health Professional Evaluation CertificateDokumen1 halamanHealth Professional Evaluation CertificateWasim UllahBelum ada peringkat