Acute Stroke - Management Made Simple
Diunggah oleh
Rosa SelviaDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Acute Stroke - Management Made Simple
Diunggah oleh
Rosa SelviaHak Cipta:
Format Tersedia
STROKE
Acute Stroke Unit
Guidelines for care of acute stroke patients
The following are basic guides to managing medical issues with stroke patients. The list is far from exhaustive and you may need to reference other texts or access senior advice.
GENERAL MANAGEMENT
HYDRATION Maintaining hydration in stroke patients is of supreme importance. As their plasma osmolarity increases so there is a concomitant increase in the infarct size. Given the hospital temperature they need at least 2litres of fluids a day if not more. If in any doubt measure the plasma and urinary osmolality. Initially it is best to give normal saline. FEEDING Food is good for people and helps them recover. People who cannot swallow should be fed as quickly as it becomes apparent that they will not be able to eat. This will usually be done through a naso-gastric tube. Feeding should commence within 72 hours unless clinical reasons prevail. Early referral for PEG is unusual and only where nasogastric tubes are repeatedly unsuccessful and dysphagia continues. PEG insertion is a procedure with associated mortality and morbidity. Most dysphagic patients will recover their swallow within a few weeks. Drugs can be given through the naso-gastric tube if necessary. DVT PROPHYLAXSIS Heparin is not appropriate for routine prophylaxsis of DVT. TED stockings are not to be used routinely following CLOTS trial (2009). VTE risk assessment should be carried out bearing this in mind. CONSTIPATION Common and uncomfortable for the patients. May be linked to hydration and eating. Easily managed through apperients or enemas. Bowel charts should be kept on all patients and interventions to avoid constipation should be made within 3 days of no bowel action. PYREXIA Common in stroke either from the stroke itself or infection/DVT etc. Look for the source but treat aggressively as slight increases in temperature result in cell death. Paracetamol orally, via naso-gastric or rectally along with fan therapy etcc is recommended. HYPOXIA It is important that oxygen saturation are maintained as high as possible (>98%). Monitoring should be regular and in some cases continuous with pulse oximeters. Oxygen should be given to ensure adequate saturation. If in any doubt then blood gasses should be checked.
Dr David Sandler / Peter Carr Jan 2007 / review Jan 2008/2009/2010
STROKE
INVESTIGATIONS
CT SCANNING All strokes should be scanned unless there is a good identifiable reason for not doing so. Scanning should be achieved within 24 hours to ensure antiplatelet therapy can be started soonest for maximum benefit. CT scanning is at present the best resource for excluding haemorrhage and space occupiers acutely and at this juncture MR has little role acutely. . CAROTID DUPLEX SCANNING Acute Duplex scanning has little role routinely unless there is the possibility of surgery for crescendo TIAs or there is the possibility of a dissected carotid artery and treatment with anticoagulants is planned. LABORATORY REQUESTS As per most acute admissions. FBC, U&Es, Glucose, LFTS, cholesterol and CPK are routine as a few percent of strokes will also have had MI at the same time (~5%). Routine clotting is not necessary young strokes will have their clotting screens done during the rehab phase of their disease. An exception is if the patient is on warfarin/heparin on admission. ECG All patients should have an ECG on admission. CHEST X-RAY Not as a routine but if suspicion of SOL or indeed other problems then will be required URINE No reason for routine urinalysis unless otherwise indicated
DRUGS
ANTIPLATELETS All patients that can tolerate aspirin should be given 300mg daily for 2 weeks it after an ischaemic stroke (~85%). Prior to this they should have a CT scan (within 24-48 hours), have no evidence of bleed or any medical contraindication. PPI cover may be given if the patient is deemed to be at high risk of stomach ulceration. If the patient is already on aspirin (~ 40-50% of patients at time of first stroke) then you may consider adding dipyridamole MR 200mg twice daily if they can tolerate it. Same criteria apply re scanning. Clopidrogel can be used if aspirin intolerant or high risk of GI bleeding and the risks of no antiplatelet therapy outweighs the risks of GI haemorrhage. There is little evidence for the use of aspirin/clopidrogel combination routinely in stroke/TIA (though in the presence of ischaemic heart disease it may be appropriate.)
Dr David Sandler / Peter Carr Jan 2007 / review Jan 2008/2009/2010
STROKE
HEPARIN/WARFARIN Heparin/lmwh are currently not indicated routinely in stroke. They may be necessary in the presence of prosthetic heart valves but seek advice before prescribing. They are not to be routinely used as DVT prophylaxsis in acute stroke. There may be a role in recurrent TIA awaiting surgery again seek advice before prescribing, as this is not a routine situation. Monitoring as per guidelines from haematology. Warfarin needs careful monitoring in stroke as there is significant risk of haemorrhagic transformation. Patients on warfarin may need to be transferred onto heparin. All patients should be scanned acutely if they have a stroke on warfarin. Management should be discussed with Registrar or above. THROMBOLYTICS
Thrombolysis is not to be undertaken under any circumstances without the involvement of the stroke team
STATINS Should be prescribed to all patients where practical and appropriate to achieve a total cholesterol of as close to 3.8 as possible. Obviously common sense needs to play a part in prescription namely ensuring that the patients will benefit from the intervention. Simvastatin at 20mg at night is a good starting off point. ACE INHIBITORS Are good drugs for people with cardiovascular/vascular disease. At present new prescription of ACEs/A2RA should probably not be instituted within the first week to ten days of the stroke. If previously on an ACE and cardiovascularly stable with a good blood pressure then unless there are other issues related to the ACE then medication can be restarted. The evidence would suggest that some ACEs (perindopril) do not alter cerebral perfusion in stroke.
MANAGEMENT OF MEDICAL COMPLICATIONS
RESTROKE Not uncommon. Treat as per new admission in terms of assessment. Document event, new neurology and manage as new event. In particular stop aspirin if started consider rescanning if deteriorating especially if on anticoagulants. Attention to swallow, chest and cardiovascular status important. Ensure new laboratory samples taken including blood sugar (stick test in the interim). ASPIRATION Not uncommon again especially in large strokes or those with posterior circulatory events. Examine the patient, document the event especially if there are factors that might be preventable namely positioning, feeding etc. Ensure observations are done recheck bloods, chest x-ray and start on antibiotics. If naso-gastric fed or PEG fed stop feed. If orally fed ask therapists to review swallow. If need be start intravenous drip. Sputum samples and blood cultures may be necessary.
Dr David Sandler / Peter Carr Jan 2007 / review Jan 2008/2009/2010
STROKE
HYPERTENSION/HYPOTENSION During the acute phase observe intervene ONLY IF potential for neurological deterioration or appears to be in accelerated phase. Ensure drugs that might be contributing to situation are reviewed. If intervention is necessary then seek advice of Registrar or above but treatment will need to be titrated or infused slowly namely GTN. Nitroprusside is probably not a good drug to use in this situation. Monitoring will have to be undertaken closely. Hypotension should be avoided stop hypotensive drugs. Rectify correctable factors and if need be give fluids to bring blood pressure up. Treat underlying cause if not stroke related. HYPERGLYCAEMIA Should be avoided. Treat in the same way as in acute coronary artery syndromes initially at least. If blood sugar over 15 on admission put on sliding scale and continue until levels return to normal. If not able to eat patient will require fluids. Sliding scale advice can be accessed from the intranet HYPOGLYCAEMIA Give glucose which ever route is appropriate at the time. Treat the cause of hypo. If you cannot get access to give glucose/dextrose then remember glucagon IM/IV/SC PULMONARY EMBOLISM/DVT High index of suspicion necessary. Try to confirm clinical diagnosis with confirmatory testing namely, FDPs, doppler, VQ or CT angio. If starting on heparin should have a negative CT scan already ie. Infarct with no transformation. Will need close monitoring in terms of anticoagulation i.e. APTT after 6 hours then dependant on results. If cerebral haemorrhage then a filter may be necessary do not start heparin without prior discussion with Registrar or above. SEPTICAEMIA Not uncommon in stroke patients. Look for source clinically blood work, cultures and chest x-ray. Ensure appropriate fluid balance and observations. Resuscitate as appropriate with fluids and broad spectrum antibiotics. If problems managing fluids/pressure then involve critical care outreach (p2341). SEIZURES If short and isolated then observe. Put on fit chart but dont intervene. If prolonged and patient is compromised then titrate diazemuls as per BNF guidelines. For maintenance oral therapy is best namely phenytoin or valproate. If IV treatment then phenytoin with appropriate monitoring whilst infused and levels because of its zero order kinetics. Usual nursing precautions and observations MOOD ASSESSMENT Mood should be assessed as it is quite common that following stroke patients may become low in mood and some may become depressed. The Yale Single Question or The Geriatric Depression Scale can be used to clarify the situation if a member of the MDT or someone close to the patient suggests the patient may be low in mood or depressed. If depression is indicated then the medical team responsible for the patient should be advised and a treatment plan agreed.
Dr David Sandler / Peter Carr Jan 2007 / review Jan 2008/2009/2010
STROKE
NURSING ASSESSMENT
OBSERVATIONS BP / Pulse & heart rhythm / Resps & O2 sats / Temp / BM. Review protocols if any recordings are outside normal limits. (MEWS) Continue 4hrly if within normal limits. ASSESSMENTS GLASGOW COMA SCALE If 15/15 - discontinue unless condition alters. If less or fluctuating - record hrly for 2hours if stable 4hrly. If fluctuating or reducing inform Doctor immediately. NIHSS Record on admission to & transfer from ASU. STRICT FLUID BALANCE AND BOWEL CHARTS Strict fluid balance to be recorded on all patients. Incontinence should be managed with the least invasive method available as this may be transient. Continence assessments to be completed if prolonged. Catheterisation to be avoided where possible. If BNO for 48hrs discuss with Doctor regarding intervention at 72hrs. If BNO for 72hrs highlight as a concern with the medical team. SWALLOW Ensure assessment is completed. Follow guidelines. Refer to SALT if any concerns. NUTRITION Ensure assessment is completed. Follow guidelines. Refer to dietician if any concerns. MANUAL HANDLING Ensure assessment is completed. Follow guidelines Refer to neuro-physio if any concerns. PRE-MORBID ASSESSMENT Record pre-morbid Rankin score. Record social circumstances and health history. REVIEW A&E STROKE FRONTSHEET & SENTINEL AUDIT FORM Check that all sections have been completed and that the data is entered on the assessment sheet and audit form. Omissions should be highlighted and/or rectified. POSITIONING Refer to Shoulder Protocol & Positioning Guidelines. If there is any reduced function / weakness in limbs / posture concerns follow guidelines & refer to neurophysio for more specific advice.
Dr David Sandler / Peter Carr Jan 2007 / review Jan 2008/2009/2010
STROKE
SUMMARY OF NURSING INTERVENTIONS FOR COMPLICATIONS
Complication Pyrexia Suggested intervention Paracetamol 1G considered [ ] Hydration assessed [ ] Minimum 4hrly vital signs until pyrexia corrected [ ] Inform medical team to consider reason for pyrexia and treat accordingly [ ] Commence O2 at 2-6L [ ] Constant Sats% monitoring until corrected [ ] Inform medical team to consider reason for reduced Sats% and treat accordingly [ ] Waterlow assessed and acted upon [ ] Profile bed considered [ ] / Pressure relief considered [ ] Positioning considered [ ] Bowel chart commenced [ ] Swallow screen completed [ ] Referral to Speech Therapy considered [ ] IVI considered [ ] / NGT considered [ ] Medications reviewed [ ] Strict fluid balance commenced [ ] Mouth care commenced [ ] Patient / family informed of NBM decision / reasons for this / risks associated [ ] Strict Bowel chart [ ] BNO 48hrs Inform medical team - consider reason - treat accordingly [ ] Consider hydration / medications etc [ ] BNO 72hrs Intervention required Consider PR / enema [ ] Daily records in notes until constipation corrected [ ] Inform medical team immediately - consider reason for deterioration - treat accordingly [ ] Full set of vital signs and monitor continuously [ ] Blood sugar [ ] GCS hrly to commence [ ] Consider repeat CT [ ] Consider alternative reason for deterioration [ ] Reassess swallow / mobility etc [ ] Consider stopping antiplatelets [ ] Inform medical team immediately [ ] Nil-by-mouth [ ] Follow NMB guidelines [ ] Stop NG / PEG feed until reassessed [ ] Consider urgent SLT review if orally fed [ ] Monitor BP continuously [ ] Inform medical team set parameters for repeat calls - record in the medical notes [ ] Medications reviewed [ ] Consider raising foot of bed in short-term (hypotension) [ ] Inform medical team if BM outside normal limits [ ] Consider Hypostop if very low BM [ ] Consider sliding scale if high or uncontrolled [ ] If short & isolated record and start fit chart [ ] If prolonged / 2nd event / patient compromised inform medical team for urgent intervention [ ]
Hypoxia (O2 Sats less than 98%) Bed Bound / Bed Rest
Nil-by-mouth (Feeding must commence within 72hrs or documentation of reason why not is in medical records) Constipation
Deterioration - ?Restroke
Suspected Aspiration
Hypertension / Hypotension
Blood sugar control
Seizure
Dr David Sandler / Peter Carr Jan 2007 / review Jan 2008/2009/2010
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- QD 002 - Quality Manual 2022 - Feb22-Rev2.6 - RBDokumen35 halamanQD 002 - Quality Manual 2022 - Feb22-Rev2.6 - RBAjibade SukuratBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Rheumatoid Arthritis Skin ManifestationsDokumen2 halamanRheumatoid Arthritis Skin ManifestationsRiena Austine Leonor NarcillaBelum ada peringkat
- A Christian Perspective of Acupuncture: A Research Paper Submitted To DR Keith WarringtonDokumen33 halamanA Christian Perspective of Acupuncture: A Research Paper Submitted To DR Keith WarringtonEric TBelum ada peringkat
- 5 - DystociaDokumen43 halaman5 - DystociaMara Medina - BorleoBelum ada peringkat
- Obstruksi Usus (Bowel Obstruction)Dokumen7 halamanObstruksi Usus (Bowel Obstruction)bhatubimBelum ada peringkat
- Obstruksi Usus (Bowel Obstruction)Dokumen7 halamanObstruksi Usus (Bowel Obstruction)bhatubimBelum ada peringkat
- Miethke DualSwitch Valve in Lumboperitoneal ShuntsDokumen9 halamanMiethke DualSwitch Valve in Lumboperitoneal ShuntsRosa SelviaBelum ada peringkat
- Changes in The Volumes of The Brain and Cerebrospinal Fluid Spaces After ShuntDokumen6 halamanChanges in The Volumes of The Brain and Cerebrospinal Fluid Spaces After ShuntRosa SelviaBelum ada peringkat
- HHD LVHDokumen10 halamanHHD LVHRosa SelviaBelum ada peringkat
- Changes in The Volumes of The Brain and Cerebrospinal Fluid Spaces After ShuntDokumen6 halamanChanges in The Volumes of The Brain and Cerebrospinal Fluid Spaces After ShuntRosa SelviaBelum ada peringkat
- Headaches in Patients With Shunts RekateDokumen4 halamanHeadaches in Patients With Shunts RekateRosa SelviaBelum ada peringkat
- ContentDokumen8 halamanContentRosa SelviaBelum ada peringkat
- Stroke Model of CareDokumen83 halamanStroke Model of CareRosa SelviaBelum ada peringkat
- Acute Stroke GuidelineDokumen36 halamanAcute Stroke GuidelineRosa SelviaBelum ada peringkat
- Office Management & Administration Skills Training Course - GLOMACSDokumen4 halamanOffice Management & Administration Skills Training Course - GLOMACSKyaw Min HanBelum ada peringkat
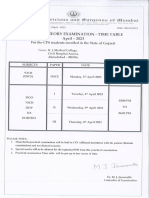
- DCH Time TableDokumen1 halamanDCH Time TableGane HospitalBelum ada peringkat
- Webinar - I-WPS OfficeDokumen31 halamanWebinar - I-WPS OfficeGayathri sundarajanBelum ada peringkat
- Albatex® CoDokumen16 halamanAlbatex® CoMahbubul HasanBelum ada peringkat
- Highcontainment BiolabsDokumen84 halamanHighcontainment Biolabshansley cookBelum ada peringkat
- الاشتريه في الوزاريات 6 اعدادي اشتر احمد 2023 كونيكاDokumen132 halamanالاشتريه في الوزاريات 6 اعدادي اشتر احمد 2023 كونيكاSajad HussienBelum ada peringkat
- Brokenshire College Socsksargen, Inc.: NCM 100-Theorerical Foundations in NursingDokumen8 halamanBrokenshire College Socsksargen, Inc.: NCM 100-Theorerical Foundations in NursingKeren Happuch EspirituBelum ada peringkat
- Skoll World Forum Panel - FINALDokumen16 halamanSkoll World Forum Panel - FINALNara E AíBelum ada peringkat
- Job Satisfaction ProjectDokumen8 halamanJob Satisfaction ProjectSwetha Reddy Lingala100% (2)
- 19th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation AssociationDokumen3 halaman19th Annual Scientific Meeting of Indonesian Physical Medicine and Rehabilitation AssociationNia Kania HapsyahBelum ada peringkat
- Readiness, Barriers and Potential Strenght of Nursing in Implementing Evidence-Based PracticeDokumen9 halamanReadiness, Barriers and Potential Strenght of Nursing in Implementing Evidence-Based PracticeWahyu HidayatBelum ada peringkat
- Tbf-531Bodyfat Monitor/Scale: Instruction ManualDokumen13 halamanTbf-531Bodyfat Monitor/Scale: Instruction ManualJose JimenoBelum ada peringkat
- Better BalanceDokumen13 halamanBetter BalanceMiriam NovoBelum ada peringkat
- Orthogold100 Ow100usDokumen70 halamanOrthogold100 Ow100uslumitransBelum ada peringkat
- Reflection Paper1 Psy111-1 A41Dokumen1 halamanReflection Paper1 Psy111-1 A41owyyyBelum ada peringkat
- Theme 4 - Fixation and Stabilization of PRADDokumen3 halamanTheme 4 - Fixation and Stabilization of PRADShany SchwarzwaldBelum ada peringkat
- 32 SMS - Cleaning Vessel (Air Line)Dokumen6 halaman32 SMS - Cleaning Vessel (Air Line)Mohd KhaidirBelum ada peringkat
- The Hahnemannian Monthly1879pdfDokumen831 halamanThe Hahnemannian Monthly1879pdfBruntBelum ada peringkat
- Eyes RETDEMDokumen2 halamanEyes RETDEMRenz Kier L. ComaBelum ada peringkat
- Pharma - M6L2 - Drug Therapy For OA and Gouty ArthritisDokumen8 halamanPharma - M6L2 - Drug Therapy For OA and Gouty ArthritisAngelaTrinidadBelum ada peringkat
- Calculating Pediatric Medication and Fluid DosagesDokumen5 halamanCalculating Pediatric Medication and Fluid DosagesMayank KumarBelum ada peringkat
- 02 - February RsmiDokumen123 halaman02 - February RsmiAlex SibalBelum ada peringkat
- Sitting Kills, Moving Heals. An Interview With Dr. Joan VernikosDokumen25 halamanSitting Kills, Moving Heals. An Interview With Dr. Joan Vernikosjayjonbeach100% (1)
- Test BFQDokumen13 halamanTest BFQChristian100% (3)
- BCM School BasantAv enueDugr iLudhi ana Cl ass-V. Subj ect-Sci ence Apti tudeWor ksheet and Honey beesDokumen6 halamanBCM School BasantAv enueDugr iLudhi ana Cl ass-V. Subj ect-Sci ence Apti tudeWor ksheet and Honey beesParam stationersBelum ada peringkat
- Sample Writing Practice Test 2Dokumen6 halamanSample Writing Practice Test 2Hồ TrânBelum ada peringkat