Autism 2
Diunggah oleh
Pakde Putu HadiHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Autism 2
Diunggah oleh
Pakde Putu HadiHak Cipta:
Format Tersedia
REVIEW ARTICLE
Paediatr Drugs 2000 Jan-Feb; 2 (1): 67-81 1174-5878/00/0001-0067/$20.00/0 Adis International Limited. All rights reserved.
Autism
Current Theories Regarding its Pathogenesis and Implications for Rational Pharmacotherapy
Jan K. Buitelaar and Sophie H.N. Willemsen-Swinkels
Department of Child Psychiatry, University Medical Centre Utrecht, Utrecht, The Netherlands
Contents
Abstract . . . . . . . . . . . . . . . . . . . . . . . . . . 1. Aetiology: Genes and Environment . . . . . . . . . . . 2. Neurobiology . . . . . . . . . . . . . . . . . . . . . . . . 2.1 Postmortem Studies . . . . . . . . . . . . . . . . . 2.2 Brain Morphology . . . . . . . . . . . . . . . . . . . 2.3 Brain Function . . . . . . . . . . . . . . . . . . . . . 2.4 Neurochemistry . . . . . . . . . . . . . . . . . . . . 3. Drug Treatment . . . . . . . . . . . . . . . . . . . . . . . 3.1 Drugs Affecting Serotonergic Neurotransmission . 3.2 Drugs Affecting Dopaminergic Neurotransmission 3.3 Drugs Affecting Peptidergic Systems . . . . . . . . 3.4 Drugs Affecting Noradrenergic Transmission . . . 3.5 Miscellaneous Agents . . . . . . . . . . . . . . . . 4. Clinical Recommendations . . . . . . . . . . . . . . . . 5. Conclusions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 67 68 70 70 71 71 72 73 73 74 76 76 76 76 77
Abstract
Autism is a pervasive developmental disorder that is aetiologically and clinically heterogeneous. Twin and family-genetic studies provide evidence for strong genetic components. An international consortium using an affected sib pair strategy has found a promising linkage to a region on chromosome 7. In 10 to 15% of cases autism is due to associated medical conditions that affect normal brain functioning. Postmortem studies on small case series report cellular abnormalities in the limbic system and cerebellum. Between 10 and 20% of individuals with autism have macrocephalia, which is in accordance with magnetic resonance imaging (MRI) findings of an increased total brain tissue volume and enlargement most prominent in the occipital and parietal lobes. The most robust and well replicated neurobiological abnormality in autism is an elevation of whole blood serotonin (5-hydroxytryptamine; 5-HT) found in over 30% of patients. Pharmacological interventions with serotonin reuptake inhibitors or with atypical neuroleptics that block both dopamine (D2) and serotonin (5-HT2) receptors seem to offer clinical benefit and merit further study.
68
Buitelaar & Willemsen-Swinkels
This review presents the current theories regarding the pathogenesis of autism and draws implications for pharmacotherapy. Autistic disorder (autism) is the prototype of a pervasive developmental disorder (PDD) and is characterised by (1) qualitative impairments in reciprocal social interactions, (2) qualitative impairments in verbal and nonverbal communication, (3) restricted repetitive and stereotyped patterns of behaviour, interests and activities, and (4) onset prior to age 3 years.[1,2] The prevalence of autism is estimated at 2 to 5 per 10 000, with numbers expanding to 10 to 20 per 10 000 if broader definitions are used.[3] The manifestations of autism vary greatly, depending on developmental level and chronological age of the individual. The majority of persons with autism exhibit serious social and communicative handicaps throughout life, but some improve enough to be able to live relatively independently as adults. About 75% of individuals with autism have associated mental retardation. The category of PDD [Diagnostic and Statistical Manual of mental disorders, 4th edition (DSM-IV)[1] includes, along with autism, a number of related conditions, such as Retts disorder, childhood disintegrative disorder, Aspergers disorder and pervasive developmental disorder not otherwise specified (PDD-NOS). Both Retts disorder and childhood disintegrative disorder are rare conditions. Retts disorder has been reported only in females and is characterised by an apparently normal development till age 5 months, followed by deceleration of head growth and by loss of purposeful hand skills and social and communication skills. Childhood disintegrative disorder is marked by significant regression in multiple areas of functioning following a period of at least 2 years of apparently normal development. While this condition is occasionally attributed to a paediatric neurological disease (e.g. metachromatic leucodystrophy), most cases remain of unknown cause. The essential features of Aspergers disorder are impairments in reciprocal social interactions and restricted stereotyped patterns of interest (as in autism), along with relatively
Adis International Limited. All rights reserved.
intact language skills at age 2 and 3 years (in contrast to autism). Additional features may be motor clumsiness and motor delays, and recognition at a somewhat later age than autism, i.e. during the school age period. PDD-NOS is a residual category for individuals who present with severe developmental problems typical of PDD but who fail to meet the criteria of any of the specific PDDs mentioned above. Recent work regarding diagnostic algorithms for PDD-NOS has described the condition as a subthreshold category of autism with at least 4 of the 12 criteria for autism present, including one of the social interaction criteria.[4,5] Although both Aspergers disorder and PDD-NOS appear to be more common than typical autism, precise prevalence estimates are lacking. Since research on the pathogenesis and treatment of PDD has been focused almost exclusively on autism, the remainder of this paper is limited to a discussion of autism. Pathogenesis refers to both the constellation of aetiological factors to which the disorder may be ascribed and the neurobiological processes and abnormalities which may underlie aetiological mechanisms. 1. Aetiology: Genes and Environment There is substantial evidence from twin and family-genetic studies that autism has strong genetic components. The recurrence risk for autism following the birth of an autistic child is 60 to 150 times the population base rate.[6] Epidemiologically based same-gender twin studies have reported much higher concordance rates for autism among identical than among nonidentical twins.[7-9] For example, in one study the pair-wise concordance rate for autism was 69% for identical twins and 0% for nonidentical twins.[9] Furthermore, both family-genetic[10]and twin studies[9] found that the autism phenotype extends well beyond the traditional diagnosis and involves more subtle social, cognitive and communicative handicap that are similar to autism in quality, but differ markedly in degree. The difference in pair-wise concordance rate between identical and nonidentical twins is
Paediatr Drugs 2000 Jan-Feb; 2 (1)
Autism: Pathogenesis and Pharmacotherapy
69
even larger when the broader phenotype rather than a narrow definition of autism is applied, and this results in heritability estimates of about 90%.[9] The mode of genetic transmission is unclear and the marked fall-off in rate of autism which occurs from identical to nonidentical twins or siblings suggests that a small number of interacting genes rather than one single gene is involved.[11] A recent full genome search for susceptibility loci in autism using affected sib pairs has resulted in linkage to a region on chromosome 7q.[12] Replication studies and further fine mapping of this region, including tests for linkage disequilibrium and analysis of candidate genes, are under way. In 10 to 15% of cases, autism is associated with known medical causes that affect normal brain functioning.[13] The level of associated medical conditions is as high as 35% for atypical cases which satisfy the criteria of PDD-NOS and is further a function of the severity of comorbid mental retardation. In part, these medical conditions associated with autism are also (mono-)genetic disorders such as fragile X, tuberous sclerosis, neurofibromatosis and phenylketonuria. Environmental causes such as infections resulting from congenital rubella, cytomegalovirus or herpesvirus have been described occasionally, but are quite infrequent causes of autism in current practice and, if operative, are most likely to give rise to atypical symptomatology. An interesting question, of course, is by which mechanisms these associated medical conditions lead to autistic symptoms. Is autism a nonspecific sequela of mental retardation or is it the result of disruptions in brain circuits which are specifically involved in social and communicative behaviours? Work on tuberous sclerosis suggests that the latter explanation is most likely, and that the extent and localisation of brain lesions is the key variable. Autism is significantly more common in tuberous sclerosis when, in addition to mental retardation, epilepsy is present and lesions are found in the temporal lobes and the limbic areas of the brain.[14] Obstetric complications have for some time been considered as an important environmental cause.
Adis International Limited. All rights reserved.
This view was based on the finding that in discordant identical twin pairs the autistic twin was more affected by obstetric hazards.[7,8] Later findings, however, have strongly modified this view, identifying that obstetric hazards are consequences of genetically influenced abnormal prenatal development rather than independent aetiological factors.[15] These interpretations stress that: (i) the obstetric complications in the twin studies were mostly very minor; (ii) the association between obstetric hazards and autism in singletons is quite weak; (iii) postmortem studies of autism have not detected lesions typical of perinatal brain damage, and (iv) studies of autistic singletons have found that the number of minor congenital anomalies is higher in probands than in siblings or normal controls, which suggests that the early in utero development of autistic individuals may be suboptimal.[16] Recently, attention has been drawn to a report on a consecutive series of 12 children with a history of PDD who were reported to exhibit loss of acquired skills and intestinal symptoms, such as diarrhoea, abdominal pain and food intolerance. Extensive clinical investigations revealed chronic inflammatory bowel disease, associated autism (in 9 children) or related conditions (in 3) and an absence of focal neurological abnormalities.[17] According to the parents, the onset of behavioural symptoms was associated with recent measles, mumps, rubella vaccination in 8 children, with measles infection in 1 child and with otitis media in another child. It was suggested that a dysfunctional intestine played a part in the behavioural changes of these children, possibly as a result of increased permeability to gut-derived peptides from food which in turn may exert central effects and interfere with neuroregulatory processes. Treatment of the intestinal pathology, by prevention of constipation and administration of aminosalicylates, led to behavioural improvements in several children. The idea that some cases of PDD may be linked to a form of inflammatory bowel disease merits further research and confirmation.
Paediatr Drugs 2000 Jan-Feb; 2 (1)
70
Buitelaar & Willemsen-Swinkels
Among other issues, the following should be clarified: what percentage of children with inflammatory bowel disease present neuropsychiatric symptoms, in order to control for selection bias; and to what extent these children exhibit typical rather than atypical autistic symptoms. Conversely, studies indicate that a significant proportion of individuals with PDD have gastrointestinal symptoms, such as abdominal distension, constipation and chronic diarrhoea, which may be due to altered intestinal permeability.[18] A key question to be answered, of course, is whether children with PDD without intestinal complaints should be referred to paediatric gastroenterologists for further investigations. The second idea of this report, the suggestion of a relationship between bowel disease/autism and vaccinations or viral infections is much more problematic and unsubstantiated, since the relationship may well be merely coincidental and not causal.[19] The potential importance of a brain-gastrointestinal axis in autism has been further emphasised by case reports on dramatic improvements of social and language skills of children with autism following administration of secretin.[20] Secretin is a polypeptide that is present in the so-called S cells in the mucosa of the upper small intestine in an inactive form, prosecretin. When acid chyme with pH <4.5 to 5.0 enters the duodenum, secretin is released into the blood. Secretin causes the pancreas to secrete large quantities of fluid that contains a high concentration of bicarbonate ions. This provides an appropriate pH in the duodenum for the digestive action of the pancreatic enzymes. Although inflated by media claims and reports on the Internet (http://secretin.com and http://autism.com/ari), the available evidence of the effects of secretin in autism is rather limited and preliminary. Limitations include small sample sizes, inadequately characterised patients, poorly defined outcome measures and the absence of placebo-controlled and double-blind designs. Furthermore, in addition to reports of dramatic improvements, it should be appreciated that other cases do not show positive responses and some
Adis International Limited. All rights reserved.
cases even show behavioural regression. Moreover, the risks of secretin administration are unknown. However, this does not detract from the merit of thinking about biological mechanisms which may be involved in the effects of secretin and which may underlie autism. For example, secretin receptors are present in the hippocampus, and secretin has also been found to bind to receptors of another peptide (vasoactive intestinal peptide) in the hypothalamus, cortex and hippocampus. In addition to a direct neuropeptidergic action of secretin, indirect influences may be involved as well, such as on the activity of brain neurotransmitter systems, brain circulation, or gastrointestinal permeability.[20] 2. Neurobiology There is overwhelming evidence that abnormalities of brain structure and function underlie the autistic syndrome. However, the following points are also clear: reported abnormalities are rather heterogeneous and based on studies of small samples; most reported abnormalities have not been replicated; findings specific to the core social and communicative deficits have not yet been demarcated from nonspecific findings; and neurobiological abnormalities have not been examined in a genetic perspective, leaving it open whether, where and to what extent genetic influences on autism produce aberrant brain morphology or brain function. In this section the focus is on recent findings from postmortem and brain imaging studies and on neurochemical evaluations. Neuropsychological, neurophysiological and cognitive studies fall outside the scope of this paper, and interested readers may consult other recent reviews.[9,21]
2.1 Postmortem Studies
To date, there have been only a few autopsy studies in autism. Reduced cell size and increased cell packing density have been observed bilaterally in the hippocampus, amygdala, entorhinal cortex, mammillary body, medial septal nucleus and anterior cingulate gyrus.[22,23] These structures are known to be connected to each other by interrelated circuits and constitute a major portion of the limbic
Paediatr Drugs 2000 Jan-Feb; 2 (1)
Autism: Pathogenesis and Pharmacotherapy
71
system of the brain. In the cerebellum, a marked reduction in the number of Purkinje cells has been found, along with a preservation of olivary neurons. This suggests that these brain lesions are of prenatal origin. Since it is now recognised that the cerebellum is involved in a variety of cognitive and affective processes, abnormalities of the limbic system and cerebellum may be linked to the core social and communicative deficits in autism. Another report, however, while replicating the reduction in Purkinje cells, did not substantiate the elevated neuronal density in the hippocampus and found more widespread abnormalities in the cortex and brainstem.[24]
2.2 Brain Morphology
Recent evidence using different samples has shown that macrocephaly occurs in 10 to 20% of autistic individuals.[9,10,25] This is an important finding, since the mean head circumference of mentally retarded individuals in general is 2 or more standard deviations below the mean of normal children and adults. The age at which macrocephaly develops in autistic children is not yet known. An explorative study found abnormal rates of head growth in early and middle childhood in some (37%) children with autism, with only a few children being macrocephalic at birth.[26] Important questions for further research are at what age macrocephaly develops, and whether rates of head growth in autism are related to clinical course and/or distinguish subtypes of autism. It should further be clarified to what extent macrocephaly is familial and to what extent it occurs in family members who do not themselves have autism. Qualitative magnetic resonance imaging (MRI) has revealed, in some individuals with autism, cortical malformations that might indicate possible neuronal migration defects.[27] Furthermore, consistent with head circumference findings, a number of MRI studies of persons with autism have found an increased total brain tissue volume (excluding CSF), which was regional and not generalised, with the greatest enlargement in the posterior regions of the brain, i.e. the occipital and parietal lobes.[28-30]
Adis International Limited. All rights reserved.
An area of controversy over the past several years has involved quantitative MRI of the size of the cerebellum and brainstem. Earlier claims of neocerebellar hypoplasia[31,32] have not been replicated. On the contrary, total cerebellar volume was recently found to be greater in individuals with autism than in controls, with the increase being proportionate to the increase in total brain volume.[33] Findings that the pons, midbrain and medulla are significantly smaller in autistic individuals[34-36] are not in accordance with reports from other groups[37,38] and are probably due to concomitant mental retardation rather than to autism. The size of the body and posterior subregions, but not of the anterior subregions, of the corpus callosum was noted to be smaller in individuals with autism than in controls.[39] Although the posterior localisation of the abnormal size of the corpus callosum is consistent with the reports of volume abnormalities cited above, the direction of the size differences is opposite to what might have been predicted. All in all, the presence of brain enlargement may provide important clues to underlying abnormalities in brain development, and further clarification of the timing of brain enlargement through longitudinal studies is called for. Three possible mechanisms have been proposed to explain brain enlargement: increased neurogenesis, decreased neuronal death and increased production of nonneuronal brain tissue. The finding of head circumference at birth being within the normal range and accelerated brain growth in the early postnatal period would be most consistent with the mechanism of decreased programmed cell death, since neurogenesis occurs foremost in the prenatal period.
2.3 Brain Function
A number of recent functional brain imaging studies in autism point to the frontal lobes as an area of the brain potentially involved in the pathophysiology of the disorder. A Single Photo Emission Computer Tomography (SPECT) study of regional cerebral blood flow reported frontal hypoperfusion in children with autism at the age of 3 to 4 years, which was found to be no longer presPaediatr Drugs 2000 Jan-Feb; 2 (1)
72
Buitelaar & Willemsen-Swinkels
ent at re-examination 3 years later.[40] A 31P MRI spectroscopy study in adolescents and adults with autism provided evidence for an abnormal pattern of phospholipid metabolism in the dorsolateral prefrontal cortex.[41] The severity of metabolic abnormality was found to be significantly correlated with executive function and language deficits.
2.4 Neurochemistry
Current interest in the neurochemistry of autism is focused predominantly on serotonin (5-hydroxytryptamine: 5-HT) and peptidergic systems. Studies of the dopaminergic and noradrenergic systems in autism have failed to reveal consistent abnormalities. The potential relevance of the dopaminergic system for understanding the pathophysiology of autism comes from observations in animal studies in which the dopaminergic system was found to be involved in hyperactivity and stereotyped behaviours. Neurochemical research in autism has included the measurement of the major metabolite of dopamine, homovanillic acid (HVA), in body fluids. The HVA levels in CSF[42-46] and in urine[47-51] of individuals with autism have been found to be equal as well as increased, when compared with those of control and contrast groups. The excretion of dopamine in urine has been reported to be lowered, whereas higher levels of dopamine were measured in whole blood of individuals with autism.[50] A recent positron emission tomography (PET) scan study suggested low activity of the frontal dopamine system in autism.[52] Elevation of the level of serotonin in whole blood of individuals with autism compared with normal controls is one of the most robust and well replicated findings in the neurobiology of autism.[53-55] The elevation is commonly observed in >30% of all individuals with autism, and the magnitude of the difference in mean level is about 25%. The importance of hyperserotonaemia in autism, however, had remained unclear for at least 2 reasons. First, the CSF levels of 5-hydroxyindoleacetic acid (5-HIAA), the breakdown product of serotonin, were not found to differ between individuals with autism and controls.[43-46] Second,
Adis International Limited. All rights reserved.
hyperserotonaemia has also been reported in nonautistic individuals with mental handicaps.[56] Arecent attempt to resolve these inconsistencies regarding hyperserotonaemia in autism pointed to the importance of pubertal and racial factors when interpreting serotonin levels.[57] Hyperserotonaemia appears to be a function of pubertal status (measured in prepubertal but not in postpubertal autistic individuals) and was not found to be present in mentally retarded or cognitively impaired control individuals without autism.[57] Although the mechanisms underlying hyperserotonaemia have not been fully clarified, increased activity of the serotonin transporter of platelets and decreased binding to the serotonin 5-HT2 receptor have been observed.[58] Preliminary findings from candidate-gene studies indicate that the short variant of the promoter of the serotonin transporter gene in one report,[59] the long variant in another report[60] but not a polymorphism of the serotonin 5-HT2 receptor gene have been significantly associated with autism.[61] The clinical relevance of hyperserotonaemia for autism is further strengthened by reports of positive correlations of whole blood serotonin levels with clinical severity[61] and negative correlations with verbal-expressive abilities in autistic probands and their first degree relatives.[62] Findings concerning the central activity of serotonin metabolism are mixed. Measurements of serotonin metabolites in the CSF of autistic individuals have failed to demonstrate consistent abnormalities,[46] but neuroendocrine responses to pharmacological probes of the serotonin system were found to be blunted,[63,64] suggesting a low central tonus of the serotonin system. Using radioactive tryptophan as a tracer for serotonin synthesis with PET, unilateral alterations of serotonin synthesis in the dentatothalamocortical pathway in autistic boys were observed.[65] Furthermore, acute dietary depletion of tryptophan, a precursor of serotonin, was associated with an exacerbation of stereotyped behaviours rather than with changes of social unrelatedness in drug-free adults with autism.[66] Any implication of serotonin in the pathogenesis of autism would be
Paediatr Drugs 2000 Jan-Feb; 2 (1)
Autism: Pathogenesis and Pharmacotherapy
73
of great interest, given the critical role of serotonin during embryogenesis and maturation of the brain and its modulatory effects on a variety of important processes, such as sensory perception, motor function, learning and memory, and sleep, which are all often perturbed in autism. Since opioids have been found to be involved in maternal-infant attachment in animal studies by influencing feelings of social comfort and blocking separation distress reactions, it has been hypothesised that excessive activity of opioid systems in the brain would prevent the formation of normal social bonding in humans and contribute to the genesis and maintenance of autistic symptoms.[67] However, research on -endorphin levels in CSF and plasma of individuals with autism has yielded inconsistent results.[68,69] The finding that the levels of both -endorphin and corticotropin were increased in the plasma of individuals with severe autism in the absence of changes in plasma levels of cortisol most likely indicates that there is a heightened response to acute stressors rather than a chronic alteration of the basal level of functioning of these systems.[69] Another peptide that has been implicated in maternal-infant bonding and affiliative behaviour is oxytocin.[70,71] The potential relevance of oxytocin for the pathophysiology of autism is reflected in recent findings that plasma levels of oxytocin were significantly lower in individuals with autism than in normal controls, and that the pattern of associations with clinical measures was different for the autistic and the normal sample.[72] It should be appreciated, however, that attachment behaviour and social bonding per se are not abnormal in individuals with autism and that any neurobiological account of autism should explain why some social and communicative behaviours are impaired whereas others are relatively intact.[73] 3. Drug Treatment Given that the neurochemical basis of autism is unknown, there is as yet no place for pharmacotherapy based on defined pathogenesis of the core social and communicative deficits. The exception,
Adis International Limited. All rights reserved.
perhaps, is intervention in the serotonin neurotransmitter system, which may be based on evidence for abnormalities in serotonin metabolism in a subgroup of individuals with autism. Other interventions of clinical utility have been developed more from a pragmatic perspective. This is not to play down the importance of medications for individuals with autism in the treatment of distressing or maladaptive target symptoms, such as hyperactivity, aggression, excitement, negativism and ritualised, stereotyped or self-injurious behaviours. Furthermore, clinicians should not hesitate to treat comorbid disorders, such as major depressive disorder or bipolar disorder, appropriately with medications. Drug treatment, however, should never be considered as a single intervention, and should always be part of a comprehensive, multidisciplinary treatment approach. When starting with medication, it is important to select appropriate targets of treatment and to monitor efficacy and adverse effects on a regular basis. A comprehensive approach to the treatment of individuals with autism usually includes a combination of structured and special educational techniques, individual behaviour modification, home training, family counselling, and placement in special schools or daycare centres. Detailed information about the principles, indications and effectiveness of behavioural and psychological treatment interventions may be found elsewhere.[74,75]
3.1 Drugs Affecting Serotonergic Neurotransmission
Early studies with fenfluramine, a halogenated amphetamine which promotes the release and inhibits the reuptake of serotonin and blocks dopamine receptors, reported dramatic improvements.[76,77] The results of a subsequent large-scale multicentre trial and a number of independent controlled trials, however, were mixed and initial claims could not be supported. In combination with the potential neurotoxity of fenfluramine[78] and reports of serious adverse effects,[79] this is sufficient reason not to recommend fenfluramine for clinical use.[80] Moreover, in many countries fenfluramine has
Paediatr Drugs 2000 Jan-Feb; 2 (1)
74
Buitelaar & Willemsen-Swinkels
now been withdrawn from the market because of these concerns over its tolerability. Clomipramine is a tricyclic antidepressant and a potent nonselective serotonin reuptake inhibitor. Treatment with clomipramine led to improvements of social relatedness, obsessive-compulsive symptoms and aggressive and impulsive behaviour in 4 out of 5 autistic patients aged 13 to 33 years in an open-label study.[81] These findings have been extended in another open-label study with clomipramine in 35 adults with PDD.[82] About 55% of these patients showed a significant treatment response and improvement in repetitive thoughts and rituals, aggression and social behaviour. In a controlled study in autistic children and adolescents aged between 6 and 18 years the response to clomipramine was compared with that of desipramine, a tricyclic noradrenergic uptake inhibitor.[83] Clomipramine was found to be superior to desipramine in improving social relatedness and anger/uncooperativeness, and both drugs were superior to placebo in decreasing symptoms of hyperactivity. Since treatment with clomipramine may result in troublesome and potentially serious adverse effects (such as a grand mal seizure because of the lowered seizure threshold), anticholinergic and cardiovascular adverse effects and behavioural toxicity,[84] our recommendation is to use this medication judiciously in children with autism. Fluvoxamine, a selective serotonin reuptake inhibitor (SSRI), proved significantly more effective than placebo in a recent 12-week double-blind, placebo-controlled trial with 30 autistic adults.[85] Of the 15 patients who received fluvoxamine, 8 were categorised as responders. Apart from mild sedation and nausea, fluvoxamine was well tolerated. A similar study with fluvoxamine in autistic individuals younger than 18 years, however, could not establish a significant treatment response but documented a high rate of adverse effects and adverse behavioural activation.[86] Since fluvoxamine given in similar dosages to youngsters with obsessivecompulsive disorder (OCD) was found to be devoid of distressing behavioural activation,[87] children with PDD may be particularly sensitive to
Adis International Limited. All rights reserved.
SSRIs. This suggests that the serotonergic system is differentially involved in PDD compared with OCD. Two other SSRIs, fluoxetine and sertraline, have been studied in autism. Fluoxetine was reported to improve 15 of 23 adolescents and adults with autism in an open-label study.[88] In a placebocontrolled study of 5 autistic individuals aged 10 to 30 years, only one improved moderately in compulsive symptoms on 20mg fluoxetine per day. Results from open-label studies of sertraline in autism have also been promising, with 24 of 42 adults rated as markedly improved following treatment with 50 to 200mg sertraline for 12 weeks.[89] The results with the SSRIs are encouraging in adults with autism who are characterised by strong behavioural rigidity and OCD-like symptoms. In contrast, children and adolescents seem to be very sensitive to the stimulating adverse effects of SSRIs and have a much lower response rate. Buspirone, an agonist of the serotonin 5-HT1A receptor with anxiolytic and mildly antidepressant effects, has been reported only in open studies. Buspirone 5mg 3 times daily for 4 weeks was given to 4 autistic children aged 9 to 10 years.[90] Two children showed clinical improvements, and no significant adverse effects were reported. Developmentally disabled adults with autism were treated in an open-label study with buspirone in dosages of 15 to 45 mg/day and showed a decrease of anxiety, temper tantrums, aggression and self-injurious behaviour.[91,92] We have successfully used buspirone 15 to 30 mg/day as an adjuvant in the residential treatment of disorganised and hyperaroused children with autism. Positive drug responses consisted of a reduction in affective lability and a decrease in anxieties and sleeping problems.[93]
3.2 Drugs Affecting Dopaminergic Neurotransmission
Of the classic neuroleptic drugs, haloperidol has been studied intensively for its effects and tolerability in autism. In a series of controlled investigations, haloperidol in dosages of 0.25 to 4.0 mg/day for 4 weeks was significantly effective in
Paediatr Drugs 2000 Jan-Feb; 2 (1)
Autism: Pathogenesis and Pharmacotherapy
75
decreasing motor stereotypies, hyperactivity, withdrawal and negativism in a group of 2- to 8-yearold autistic children.[94,95] After 6 months of continuation treatment, haloperidol remained effective with 71.5% of the children, but left 20% unchanged and 8.5% worsened.[96] Short term adverse effects include dystonic reactions, acute dyskinesias, parkinsonism, akathisia, and autonomous and cardiovascular signs and symptoms. The long term efficacy of haloperidol is not well documented, however, and the risk for serious long term adverse effects such as tardive dyskinesias, induction of anxiety and depression, and weight gain is of great concern. In a prospective study of 82 autistic children treated with haloperidol, 24 children were found to develop dyskinesias.[97] The design of the study included a 6-month period of haloperidol treatment, followed by a 4-week period of placebo. In 5 cases tardive dyskinesias occurred, and in 19 cases withdrawal dyskinesias. All the dyskinesia symptoms disappeared spontaneously or after discontinuation of haloperidol. Pimozide, in dosages ranging from 0.25 to 4 mg/day, proved to be as effective as haloperidol in a multicentre controlled trial[98] and was found to decrease hypoactivity in autistic children.[99] The newer or atypical neuroleptics have received much interest over recent years, given their lower propensity to induce extrapyramidal adverse effects at therapeutic doses. In addition, the positive effects of the atypical neuroleptics on the negative symptoms of schizophrenic patients seem promising as a potential strategy to improve the core social deficits of individuals with autism. Pharmacologically, these newer neuroleptics block both dopamine (D2) and serotonin (5-HT2) receptor systems. To the best of our knowledge, clozapine has not been investigated in autism. A series of open-label studies in children, adolescents and adults have documented promising clinical improvements following treatment with risperidone.[100-105] For example, 20 children and adolescents with a developmental disorder refractory to other psychotropic treatments were successfully treated with
Adis International Limited. All rights reserved.
risperidone in dosages ranging from 1.5 to 10 mg/day.[100] Common adverse effects of risperidone are weight gain and sedation. However, the risk of extrapyramidal adverse effects and tardive dyskinesias with risperidone is not totally absent and necessitates low dosage treatment, preferably in the range of 0.5 to 4.0 mg/day. In our clinical practice we recently treated 2 boys with autism who developed tardive dyskinesia when on risperidone. Both boys had symptoms in the oro-buccal region which disappeared over a period of some weeks after risperidone had been discontinued. It is further recommended to monitor weight gain carefully. Occasionally, an increase of hepatic enzymes and fatty infiltration has been reported following risperidone treatment.[106,107] National Institutes of Health (NIH)-sponsored placebo-controlled multicentre studies regarding the efficacy and tolerability of risperidone in children with autism are ongoing. A placebo-controlled parallel study in adults with autism and PDDNOS indicated that risperidone in dosages of 1.0 to 6.0 mg/day for 12 weeks was superior to placebo in improving irritability, aggression, and repetitive and affective symptoms.[108] Objective changes in social and communicative behaviour were not observed. The drug was well tolerated, the most prominent adverse effect being mild transient sedation. Psychostimulants are the first-line treatment of symptoms of hyperactivity, inattentiveness and impulsivity. Since individuals with autism are often hyperactive and highly distractible, treatment with stimulants would appear an obvious strategy. Earlier studies found that methylphenidate worsened symptoms such as stereotypies when used in hyperactive children with autism.[109,110] A recent double-blind crossover study in 10 autistic children aged 7 to 11 years, using placebo and 2 doses of methylphenidate (10mg and 20mg twice daily), showed that both doses of methylphenidate resulted in a significant decrease in hyperactivity. Troublesome adverse effects were found to be absent, particularly the worsening of stereotypic
Paediatr Drugs 2000 Jan-Feb; 2 (1)
76
Buitelaar & Willemsen-Swinkels
movements.[111] Negative effects of stimulants are thought to occur mostly with mentally retarded children with IQ below 45 or mental age below 4.5 years.[112]
3.3 Drugs Affecting Peptidergic Systems
The results of placebo-controlled studies in children with autism treated with naltrexone, an opiate antagonist which can be orally administered, were overall disappointing.[113-118] Although treatment with naltrexone in a dosage of about 1.0 mg/kg/day was consistently associated with a significant but modest reduction of hyperactivity, the social and communicative deficits and the stereotyped behaviours at group level were not ameliorated. Openlabel continuation treatment for a period of 6 months of 5 autistic children, who showed a clear individual response to naltrexone in the 4-week trial, did not reveal therapeutic effects on social and communicative functioning.[119] Furthermore, in a double-blind, placebo-controlled, crossover study in mentally retarded adults with autism and/or selfinjurious behaviour, naltrexone failed to affect self-injurious and autistic behaviour in a positive way.[120] Naltrexone has a bitter taste which can give rise to compliance problems. Adverse effects of naltrexone are mild and transient. On balance, we would not advocate naltrexone for the treatment of autism on a routine basis. The use of secretin for individuals with autism (see section 1) should at this stage be restricted to approved research protocols.
3.4 Drugs Affecting Noradrenergic Transmission
In open trials propranolol, a lipophilic blocker, was used to treat aggression, self-injury and impulsivity in developmental disorders.[122,123] It is necessary to perform an ECG before starting treatment to check for pre-existing cardiac conduction anomalies, and to monitor heart rate and blood pressure regularly because of the risk of bradycardia and hypotension. Contraindications to the use of -blockers are, among others, comorbid diabetes mellitus, obstructive pulmonary diseases and cardiovascular diseases.
3.5 Miscellaneous Agents
When the symptoms of a child show a cyclic pattern, or when for instance a bipolar mood disorder is suspected, treatment with lithium can be helpful. Successful treatments in autistic patients with periodic increases in symptomatology have been described.[124,125] Lithium can also be used in the treatment of aggressive and self-injurious behaviour in autistic patients.[126] Some 20 to 30% of children with autistic disorder also have epilepsy. Therefore anticonvulsants can play a role in the management of the disease. Carbamazepine is reported to have, as well as an anticonvulsive effect, positive effects on mood disorders and on aggressive, irritative or explosive behaviour in autistic children.[127] Open-label treatment with valproate also produced an improvement in behavioural symptoms associated with autism.[128] 4. Clinical Recommendations Medication may be considered for individuals with autism when target symptoms such as hyperactivity, aggression and self-injury, stereotypies and rigidity, and anxieties interfere with psychosocial adaptation or negatively influence the effectiveness of psychological and behavioural treatment approaches. For a number of these target behaviours, environmental manipulations and focused behavioural interventions may be as effective as medication.[74,75,129] Furthermore, incidental or episodic comorbid disorders such as depressive conditions may be a focus of pharmacotherapy. The
Paediatr Drugs 2000 Jan-Feb; 2 (1)
Two controlled studies[121] reported on the use of clonidine, a presynaptic 2-adrenergic receptor agonist. Clonidine was able to reduce hyperactivity, impulsivity and irritability on a short term basis. Clinical experience, however, indicates that many patients develop tolerance to the therapeutic effects of clonidine, which seems to limit its applicability in clinical practice. Reported adverse effects are an increase in drowsiness, decreased activity and hypotension.
Adis International Limited. All rights reserved.
Autism: Pathogenesis and Pharmacotherapy
77
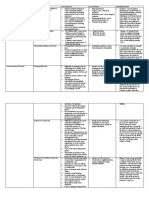
Table I. Clinical guidelines for pharmacotherapy in autism Target Hyperactivity, impulsiveness Medications Methylphenidate or other stimulants Atypical antipsychotics Clonidine Naltrexone Rigidity, rituals Selective serotonin reuptake inhibitors Atypical antipsychotics Aggression, self-injury Atypical antipsychotics Lithium
-Blockers
Anticonvulsants Clonidine Anxiety, affective symptoms Buspirone Atypical antipsychotics Clonidine
guidelines and dosages for the pharmacotherapy of autism are summarised in tables I and II. Hyperactivity and inattentiveness in a task-related context similar to that observed in attention-deficit hyperactivity disorder may be responsive to stimulant treatment, and should be differentiated from a lack of social attention associated with joint attention deficits and from being absorbed in preoccupations and interests. Clinical experience suggests that SSRIs are particularly effective in treating rigidity, rituals and stereotyped patterns of behaviour when interruption of these behaviours is accompanied by aggression or increased anxiety. 5. Conclusions Autism is a an aetiologically and clinically heterogeneous disorder, for which, as yet, no consistent neuroanatomical, neurophysiological or neurochemical abnormality has been found. Internationally concerted efforts are being made to unravel the genetic mechanisms of autism and to localise and ultimately identify genes involved. This has the prospect of potentially documenting new biochemical pathways to normal and abnormal social and
clinician should make a careful assessment of the risks and benefits of medications, since the database of well performed and controlled medication studies in autism is limited and our knowledge of, particularly, long term effectiveness and tolerability of drug treatment is incomplete. This should be communicated to the patient and/or their family in the process of obtaining informed consent. Clinical
Table II. Medication regimens for treatment of autism Medications Stimulants methylphenidate dexamfetamine Clonidine Naltrexone Atypical antipsychotics risperidone olanzapine Lithium 0.25-3 mg/day in 1-2 doses 2.5-15 mg/day in 1-2 doses Dosages
Comments Low dose regimen; be aware of induction of stereotypies and of psychotic decompensation
0.3-0.7 mg/kg/day (5-60 mg/day) in 2-4 doses 0.15-0.35 mg/kg/day (2.5-40 mg/day) in 2-4 doses Approximately 4 g/kg/day in 2-3 doses 0.5-2.0 mg/kg/day in 2-3 doses
Bitter taste Low dose regimen; be aware of weight gain, behavioural activation and extrapyramidal symptoms
To a serum concentration of 0.8-1.2 mEq/L 20-300 mg/day in 3-4 doses 25-300 mg/day in 1-2 doses 5-80 mg/day in 1-2 doses 25-200 mg/day in 1-2 doses 15-60 mg/day in 3 doses To a blood concentration of 4-12 mg/L To a blood concentration of 50-100 mg/L Low dose regimen; be aware of behavioural activation
-Blocking agents
propranolol SSRIs fluvoxamine fluoxetine sertraline Buspirone Anticonvulsants carbamazepine valproate
SSRIs = selective serotonin reuptake inhibitors.
Adis International Limited. All rights reserved.
Paediatr Drugs 2000 Jan-Feb; 2 (1)
78
Buitelaar & Willemsen-Swinkels
communicative behaviour. In turn, this may give new clues to developing effective and well tolerated medications for individuals with autism. Over recent decades, unfortunately, little progress has been made in developing new and effective pharmacotherapies for autism. Medication research in autism has evolved in the slipstream of the psychopharmacology of the major psychiatric problems of adult age rather than as a result of investigational activities well focused on the specifics of the disorder. References
1. American Psychiatric Association (APA), Diagnostic and statistical manual of mental disorders, 4th ed. (DSM-IV). Washington DC: APA, 1994 2. World Health Organization. ICD-10. Classification of mental and behavioural disorders. Clinical description and diagnostic guidelines. Geneva: WHO, 1992 3. Lord C, Rutter M. Autism and pervasive developmental disorders. In: Rutter M, Taylor E, Hersov L, editors. Child and adolescent psychiatry, modern approaches. Oxford: Blackwell Science, 1995: 569-93 4. Buitelaar JK, Van der Gaag RJ, Klin A, et al. Exploring the boundaries of PDD-NOS: analyses of data from the DSM-IV autistic disorder field trial. J Autism Dev Disord 1999; 29: 33-43 5. Buitelaar JK, Van der Gaag RJ. Diagnostic rules for children with PDD-NOS and multiple complex developmental disorder. J Child Psychol Psychiatry 1998; 39: 911-20 6. Smalley SL. Genetic influences in childhood-onset psychiatric disorders: autism and attention-deficit/hyperactivity disorder. Am J Hum Genet 1997; 60: 1276-82 7. Folstein S, Rutter ML. Infantile autism: a genetic study of 21 twin pairs. J Child Psychol Psychiatry 1977; 18: 297-312 8. Steffenburg S, Gillberg C, Helgren L, et al. A twin study of autism in Denmark, Finland, Iceland, Norway and Sweden. J Child Psychol Psychiatry 1989; 30: 405-16 9. Bailey A, Le Couteur A, Gottesman I, et al. Autism as a strongly genetic disorder: evidence from a British twin study. Psychol Med 1995; 25: 63-77 10. Bolton P, Macdonald H, Pickles A, et al. A case-control family history study of autism. J Child Psychol Psychiatry 1994; 35: 877-900 11. Pickles A, Bolton P, Macdonald H, et al. Latent-class analysis of recurrence risks for complex phenotypes with selection and measurement error: a twin and family history study of autism. Am J Hum Genet 1995; 57: 717-26 12. International Molecular Genetic Study of Autism Consortium. A full genome screen for autism with evidence for linkage to a region on chromosome 7q. Hum Mol Genet 1998; 7: 571-8 13. Rutter M, Bailey A, Bolton P, et al. Autism and known medical conditions: myth and substance. J Child Psychol Psychiatry 1994; 35: 311-22 14. Bolton PF, Griffiths PD. Association of tuberous sclerosis of temporal lobes with autism and atypical autism [see comments]. Lancet 1997; 349: 392-5
15. Bolton PF, Murphy M, Macdonald H, et al. Obstetric complications in autism: consequences or causes of the condition? J Am Acad Child Adolesc Psychiatry 1997; 36: 272-81 16. Bailey A, Phillips W, Rutter M. Autism: towards an integration of clinical, genetic, neuropsychological, and neurobiological perspectives. J Child Psychol Psychiatry 1996; 37: 89-126 17. Wakefield AJ, Murch SH, Anthony A, et al. Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet 1998; 351: 637-41 18. DEufeinia P. Abnormal intestinal permeability in children with autism. Acta Paediatrica 1996; 85: 1076-9 19. Chen RT, DeStephano F. Vaccine adverse events; causal or coincidental? Lancet 1998; 351: 611-2 20. Horvath K, Stefanatos G, Sokolski K, et al. Improved social and language skills after secretin administration in patients with autistic spectrum disorders. J Assoc Acad Minor Physicians 1998; 9: 9-15 21. Happe F, Frith U. The neuropsychology of autism. Brain 1996; 119: 1377-400 22. Bauman ML. Brief report: neuroanatomic observations of the brain in pervasive developmental disorders. J Autism Dev Disord 1996; 26: 199-203 23. Kemper TL, Bauman ML. The contribution of neuropathologic studies to the understanding of autism. Neurol Clin 1993; 11: 175-87 24. Bailey A, Luthert P, Dean A, et al. A clinicopathological study of autism. Brain 1998; 121: 889-905 25. Woodhouse W, Bailey A, Rutter M, et al. Head circumference in autism and other pervasive developmental disorders. J Child Psychol Psychiatry 1996; 37: 665-71 26. Lainhart JE, Piven J, Wzorek M, et al. Macrocephaly in children and adults with autism. J Am Acad Child Adolesc Psychiatry 1997; 36: 282-90 27. Piven J, Berthier ML, Starkstein SE, et al. Magnetic resonance imaging evidence for a defect of cerebral cortical development in autism. Am J Psychiat 1990; 147: 734-9 28. Piven J, Arndt S, Bailey J, et al. An MRI study of brain size in autism. Am J Psychiatry 1995; 152: 1145-9 29. Piven J, Arndt S, Bailey J, et al. Regional brain enlargement in autism: a magnetic resonance imaging study. J Am Acad Child Adolesc Psychiatry 1996; 35: 530-6 30. Filipek PA. Brief report: neuroimaging in autism: the state of the science 1995. J Autism Dev Disord 1996; 26: 211-5 31. Courchesne E, Yeung-Courchesne R, Press GA, et al. Hypoplasia of cerebellar vermal lobules VI and VII in autism. N Engl J Med 1988; 318: 1349-54 32. Courchesne E, Saitoh O, Townsend JP, et al. Cerebellar hypoplasia and hyperplasia in infantile autism. Lancet 1994; 343: 63-4 33. Piven J, Saliba K, Bailey J, et al. An MRI study of autism: the cerebellum revisited. Neurology 1997; 49: 546-51 34. Hashimoto T, Tayama M, Miyazaki M, et al. Reduced brainstem size in children with autism. Brain Dev 1992; 14: 94-7 35. Hashimoto T, Tayama M, Miyazaki M, et al. Brainstem and cerebellar vermis involvement in autistic children. J Child Neurol 1993; 8: 149-52 36. Hashimoto T, Tayama M, Murakawa K, et al. Development of the brainstem and cerebellum in autistic patients. J Autism Dev Disord 1995; 25: 1-18 37. Piven J, Nehme E, Barta P, et al. Magnetic resonance imaging in autism: measurement of the cerebellum, pons, and fourth ventricle. Biol Psychiatry 1992; 31: 491-504
Adis International Limited. All rights reserved.
Paediatr Drugs 2000 Jan-Feb; 2 (1)
Autism: Pathogenesis and Pharmacotherapy
79
38. Hsu M, Yeung-Courchesne R, Courchesne E, et al. Absence of magnetic resonance imaging evidence of pontine abnormality in infantile autism. Arch Neurol 1991; 48: 1160-3 39. Piven J, Bailey J, Ranson BJ, et al. An MRI study of the corpus callosum in autism. Am J Psychiatry 1997; 154: 1051-6 40. Zilbovicius M, Garreau B, Samson Y, et al. Delayed maturation of the frontal cortex in childhood autism. Am J Psychiatry 1995; 152: 248-52 41. Minshew NJ, Goldstein G, Dombrowski SM, et al. A preliminary 31P MRS study of autism: evidence for undersynthesis and increased degradation of brain membranes. Biol Psychiatry 1993; 33: 762-73 42. Cohen DJ, Caparulo BK, Shaywitz BA, et al. Dopamine and serotonin metabolism in neuropsychiatrically disturbed children: CSF homovanillic acid and 5-hydroxy-indoleacetic acid. Arch Gen Psychiatry 1977; 34: 545-50 43. Gillberg C, Svennerholm L, Hamilton-Hellberg C. Childhood psychosis and monoamine metabolites in spinal fluid. J Autism Dev Dis 1983; 13: 383-96 44. Ross DL, Klykylo WM, Anderson GM. Cerebrospinal fluid indolamines and monoamine effects in fenfluramine treatment of autism. Ann Neurol 1985; 18: 394-6 45. Gillberg C, Svennerholm L. CSF monoamines in autistic syndromes and other pervasive developmental disorders of early childhood. Br J Psychiatry 1987; 151: 89-94 46. Narayan M, Srinath S, Anderson GM, et al. Cerebrospinal fluid levels of homovanillic acid and 5-hydroxyindoleacetic acid in autism. Biol Psychiatry 1993; 33: 630-5 47. Launay JM, Bursztejn C, Ferrari P, et al. Catecholamine metabolism in infantile autism: a controlled study of 22 autistic children. J Autism Dev Dis 1987; 17: 553-6 48. Garreau B, Barthlmy C, Jouve J, et al. Urinary homovanillic acid levels of autistic children. Dev Med Child Neurol 1988; 30: 93-8 49. Minderaa RB, Anderson GM, Volkmar FR, et al. Neurochemical study of dopamine functioning in autistic and normal subjects. J Am Acad Child Adolesc Psychiatry 1989; 28: 190-4 50. Martineau J, Herault J, Petit E, et al. Catecholaminergic metabolism and autism. J Autism Dev Disord 1994; 36: 688-97 51. Hameury L, Roux S, Barthelemy C, et al. Quantified multidimensional assessment of autism and other pervasive developmental disorders. Application for bioclinical research. Eur Child Adolesc Psychiatry 1995; 4: 123-35 52. Ernst M, Zametkin AJ, Matochik JA, et al. Low medial prefrontal dopaminergic activity in autistic children [letter]. Lancet 1997; 350: 638 53. Minderaa RB, Anderson GM, Volkmar FR, et al. Whole blood serotonin and tryptophan in autism: temporal stability and the effects of medication. J Autism Dev Disord 1989; 19: 129-36 54. Anderson GM, Horne WC, Chatterjee D, et al. The hyperserotonemia of autism. Ann NY Acad Sci 1990; 600: 331-42 55. Cook EHJ, Leventhal BL, Heller W, et al. Autistic children and their first-degree relatives: relationships between serotonin and norepinephrine levels and intelligence. J Neuropsychiatry Clin Neurosci 1990; 2: 268-74 56. Partington MW, Tu JB, Wong CY. Blood serotonin levels in severe mental retardation. Dev Med Child Neurol 1973; 15: 616-27 57. McBride PA, Anderson GM, Hertzig ME, et al. Effects of diagnosis, race, and puberty on platelet serotonin levels in autism and mental retardation. J Am Acad Child Adolesc Psychiatry 1998; 37: 767-76 58. Cook EH, Leventhal BL. The serotonin system in autism. Curr Opin Pediatr 1996; 8: 348-54
59. Cook Jr EH, Courchesne R, Lord C, et al. Evidence of linkage between the serotonin transporter and autistic disorder. Mol Psychiatry 1997; 2: 247-50 60. Klauck SM, Poustka F, Benner A, et al. Serotonin transporter (5-HTT) gene variants associated with autism? Hum Mol Genet 1997; 6: 2233-8 61. Herault J, Petit E, Martineau J, et al. Serotonin and autism: biochemical and molecular biology features. Psychiatry Res 1996; 65: 33-43 62. Cuccaro ML, Wright HH, Abramson RK, et al. Whole blood serotonin and cognitive functioning in autistic individuals and their first-degree relatives. J Neuropsychiatry Clin Neurosci 1993; 2: 268-74 63. Hoshino Y, Tachibana R, Watanabe M, et al. Serotonin metabolism and hypothalamic-pituitary function in children with infantile autism and minimal brain dysfunction. Jpn J Psychiatry Neurol 1984; 26: 937-45 64. McBride PA, Anderson GM, Hertzig ME, et al. Serotonergic responsivity in male young adults with autistic disorder. Arch Gen Psychiatry 1989; 46: 213-21 65. Chugani DC, Muzik O, Rothermel R, et al. Altered serotonin synthesis in the dentatothalamocortical pathway in autistic boys. Ann Neurol 1997; 42: 666-9 66. McDougle CJ, Naylor ST, Cohen DJ, et al. Effects of tryptophan depletion in drug-free adults with autistic disorder. Arch Gen Psychiatry 1996; 53: 993-1000 67. Panksepp J. A neurochemical theory of autism. Trends Neurosci 1979; 2: 174-7 68. Willemsen-Swinkels SHN, Buitelaar JK, Weijnen FG, et al. Plasma beta-endorphin concentrations in people with learning disability and self-injurious and/or autistic behaviour. Br J Psychiatry 1996; 168: 105-9 69. Tordjman S, Anderson GM, McBride PA, et al. Plasma betaendorphin, adrenocorticotropic hormone, and cortisol in autism. J Child Psychol Psychiatry 1997; 38: 705-15 70. Insel TR. A neurobiological basis of social attachment. Am J Psychiatry 1997; 154: 726-35 71. Freeman WJ. Neurohumoral brain dynamics of social group formation. Implications for autism. Ann N Y Acad Sci 1997; 807: 501-3 72. Modahl C, Green L, Fein D, et al. Plasma oxytocin levels in autistic children. Biol Psychiatry 1998; 43: 270-7 73. Buitelaar JK. Attachment and social withdrawal in autism: hypotheses and findings. Behaviour 1995; 132: 319-50 74. Howlin P, Rutter M. Treatment of autistic children. New York: Wiley & Sons, 1987 75. Howlin P. Practitioner review: psychological and educational treatments for autism. J Child Psychol Psychiatry 1998; 39: 307-22 76. Geller E, Ritvo ER, Freeman BJ. Preliminary observations on the effects of fenfluramine on blood serotonin and symptoms in three autistic boys. N Engl J Med 1982; 307: 165-9 77. Ritvo ER, Freeman BJ, Geller E, et al. Effects of fenfluramine on 14 outpatients with the syndrome of autism. J Am Acad Child Psychiatry 1983; 22: 549-58 78. Schuster CR, Lewis M, Seiden LS. Fenfluramine: neurotoxicity. Psychopharmacol Bull 1986; 22: 148-51 79. Realmuto GM, Jensen J, Klykylo W, et al. Untoward effects of fenfluramine in autistic children. J Clin Psychopharmacol 1986; 6: 350-5 80. Buitelaar JK. Psychopharmacological approaches to childhood psychotic disorders. In: Den Boer JA, Westenberg HGM, Van Praag HM, editors. Advances in the neurobiology of schizophrenia. London: Wiley & Sons, 1995: 429-57
Adis International Limited. All rights reserved.
Paediatr Drugs 2000 Jan-Feb; 2 (1)
80
Buitelaar & Willemsen-Swinkels
81. McDougle CJ, Price LH, Volkmar FR, et al. Clomipramine in autism: preliminary evidence of efficacy (case study). J Am Acad Child Adolesc Psychiatry 1992; 31: 746-50 82. Brodkin ES, McDougle CJ, Naylor ST, et al. Clomipramine in adults with pervasive developmental disorders: a prospective open-label investigation. J Child Adolesc Psychopharmacol 1997; 7: 109-21 83. Gordon CT, State RC, Nelson JE, et al. A double-blind comparison of clomipramine, desipramine, and placebo in the treatment of autistic disorder. Arch Gen Psychiatry 1993; 50: 441-7 84. Sanchez LE, Campbell M, Small AM, et al. A pilot study of clomipramine in young autistic children. J Am Acad Child Adolesc Psychiatry 1996; 35: 537-44 85. McDougle CJ, Naylor ST, Cohen DJ, et al. A double-blind, placebo-controlled study of fluvoxamine in adults with autistic disorder. Arch Gen Psychiatry 1996; 53: 1001-8 86. McDougle CJ. Psychopharmacology of autism (paper presented at XIth Congress of the ECNP). Eur Neuropsychopharmacol 1998; Suppl. 2: S107 87. Riddle M. Fluvoxamine in children and adolescents with OCD. Proceedings X World Congress of Psychiatry, Madrid 1996; 2: 141 88. Cook EH, Rowlett R, Jaselskis C, et al. Fluoxetine treatment of children and adults with autistic disorder and mental retardation. J Am Acad Child Adolesc Psychiatry 1992; 31: 739-45 89. Hellings JA, Kelley LA, Gabrielli WF, et al. Sertraline response in adults with mental retardation and autistic disorder. J Clin Psychiatry 1996; 57: 333-6 90. Realmuto GM, August GJ, Garfinkel BD. Clinical effect of buspirone in autistic children. J Clin Psychopharmacol 1989; 9: 122-5 91. Ratey JJ, Sovner R, Mikkelsen E, et al. Buspirone therapy for maladaptive behavior and anxiety in developmentally disabled persons. J Clin Psychiatry 1989; 50: 382-4 92. Ratey J, Sovner R, Parks A, et al. Buspirone treatment of aggression and anxiety in mentally retarded patients: a multiplebaseline, placebo lead-in study. J Clin Psychiatry 1991; 52: 159-62 93. Buitelaar JK, Van der Gaag RJ, Van der Hoeven J. Effects of buspirone in the management of anxiety and irritability in children with pervasive developmental disorders: open pilot data. J Clin Psychiatry 1998; 59: 56-9 94. Anderson LT, Campbell M, Graga DM, et al. Haloperidol in the treatment of infantile autism: effects on learning and behavioral symptoms. Am J Psychiatry 1984; 141: 1195-202 95. Anderson LT, Campbell M, Adams P, et al. The effects of haloperidol on discrimination learning and behavioral symptoms in autistic children. J Autism Dev Disord 1989; 19: 227-39 96. Perry R, Campbell M, Adams P, et al. Long-term efficacy of haloperidol in autistic children: continuous versus discontinuous administration. J Am Acad Child Adolesc Psychiatry 1989; 28: 87-92 97. Campbell M, Adams P, Perry R, et al. Tardive and withdrawal dyskinesia in autistic children: a prospective study. Psychopharmacol Bull 1988; 24: 251-5 98. Naruse H, Nagahata M, Nakane Y, et al. A multi-center doubleblind trial of pimozide (Orap), haloperidol and placebo in children with behavioral disorders, using cross-over design. Acta Paedopsychiatrica 1982; 48: 173-84 99. Ernst M, Magee HJ, Gonzalez NM, et al. Pimozide in autistic children. Psychopharmacol Bull 1992; 28: 187-91 100. Hardan A, Johnson K, Johnson C, et al. Case study: risperidone treatment of children and adolescents with developmental disorders. J Am Acad Child Adolesc Psychiatry 1996; 35: 1551-6
101. Nicolson R, Awad G, Sloman L. An open trial of risperidone in young autistic children. J Am Acad Child Adolesc Psychiatry 1998; 37: 372-6 102. Perry R, Pataki C, Munoz Silva DM, et al. Risperidone in children and adolescents with pervasive developmental disorder: pilot trial and follow-up. J Child Adolesc Psychopharmacol 1997; 7: 167-79 103. McDougle CJ, Holmes JP, Bronson MR, et al. Risperidone treatment of children and adolescents with pervasive developmental disorders: a prospective open-label study. J Am Acad Child Adolesc Psychiatry 1997; 36: 685-93 104. Fisman S, Steele M. Use of risperidone in pervasive developmental disorders: a case series. J Child Adolesc Psychopharmacol 1996; 6: 177-90 105. Findling RL, Maxwell K, Wiznitzer M. An open clinical trial of risperidone monotherapy in young children with autistic disorder. Psychopharmacol Bull 1997; 33: 155-9 106. Geller WK, Zuiderwijk PB. Risperidone-induced hepatotoxicity? [letter]. J Am Acad Child Adolesc Psychiatry 1998; 37: 246-7 107. Kumra S, Herion D, Jacobsen LK, et al. Case study: risperidoneinduced hepatotoxicity in pediatric patients. J Am Acad Child Adolesc Psychiatry 1997; 36: 701-5 108. McDougle CJ, Holmes JP, Carlson DC, et al. A double-blind, placebo-controlled study of risperidone in adults with autistic disorder and other pervasive developmental disorders. Arch Gen Psychiatry 1998; 55: 633-41 109. Campbell M, Fish B, David R, et al. Response to triiodothyronine and dextroamphetamine: a study of preschool schizophrenic children. J Autism Childhood Schizophr 1972; 2: 343-57 110. Bloom ASR. Methylphenidate-induced delusional disorder in a child with attention deficit disorder with hyperactivity. J Am Acad Child Adolesc Psychiatry 1988; 27 (1): 88-9 111. Quintana H, Birmaher B, Stedge D, et al. Use of methylphenidate in the treatment of children with autistic disorder. J Autism Dev Disord 1995; 25: 283-94 112. Aman MG, Marks RE, Turbott SH, et al. Clinical effects of methylphenidate and thioridazine in intellectually subaverage children. J Am Acad Child Adolesc Psychiatry 1991; 30: 246-56 113. Leboyer M, Bouvard MP, Launay J, et al: brief report: a double-blind study of naltrexone in infantile autism. J Autism Dev Disord 1992; 22: 309-19 114. Campbell M, Anderson LT, Small AM, et al. Naltrexone in autistic children behavioral symptoms and attentional learning. J Am Acad Child Adolesc Psychiatry 1993; 32: 1283-91 115. Kolmen BK, Feldman HM, Handen BL, et al. Naltrexone in young autistic children A double-blind, placebo-controlled crossover study. J Am Acad Child Adolesc Psychiatry 1995; 34: 223-31 116. Kolmen BK, Feldman HM, Handen BL, et al. Naltrexone in young autistic children: replication study and learning measures. J Am Acad Child Adolesc Psychiatry 1997; 36: 1570-8 117. Willemsen-Swinkels SHN, Buitelaar JK, Van Engeland H. The effects of chronic naltrexone treatment in young autistic children: a double-blind placebo-controlled crossover study. Biol Psychiatry 1996; 39: 1023-31 118. Willemsen-Swinkels SHN, Buitelaar JK, Weijnen FG, et al. Placebo-controlled acute dosage naltrexone study in young autistic children. Psychiatry Res 1995; 58: 203-15 119. Willemsen-Swinkels SHN, Buitelaar JK, Van Berckelaer-Onnes IA, et al. Brief report: six-months continuation treatment in naltrexone-responsive children with autism: an open-label case-control design. J Autism Dev Disord 1999; 29: 167-9
Adis International Limited. All rights reserved.
Paediatr Drugs 2000 Jan-Feb; 2 (1)
Autism: Pathogenesis and Pharmacotherapy
81
120. Willemsen-Swinkels SHN, Buitelaar JK, Nijhof G, et al. Failure of naltrexone hydrochloride to reduce self-injurious and autistic behavior in mentally retarded adults. Double-blind placebocontrolled studies. Arch Gen Psychiatry 1995; 52: 766-73 121. Fankhauser MP, Karumanchi VC, German ML, et al. A doubleblind, placebo-controlled study of the efficacy of transdermal clonidine in autism. J Clin Psychiatry 1992; 53: 77-82 122. Ratey JJ, Lindem KJ. Beta-blockers as primary treatment for aggression and self-injury in the developmentally disabled. In: Ratey JJ, editor. Mental retardation. Developing pharmacotherapies. Washington DC: American Psychiatric Press, 1991: 51-82 123. Ratey JJ, Bemporad J, Sorgi P, et al. Brief report: open trial effects of beta-blockers on speech and social behaviors in 8 autistic adults. J Autism Dev Disord 1987; 17: 439-46 124. Komoto JM, Usui S, Hirata J. Infantile autism and affective disorder. J Autism Dev Disord 1984; 14: 81-4 125. Kerbeshian J, Burd L, Fisher W. Lithium carbonate in the treatment of two patients with infantile autism and atypical bipolar symptomatology. J Clin Psychopharmacol 1987; 7: 401-5
126. Buitelaar JK. Self-injurious behavior in retarded children, clinical phenomena and biological mechanisms. Acta Paedopsychiatrica 1993; 56: 105-11 127. Gillberg C. The treatment of epilepsy in autism. J Autism Dev Disord 1991; 21: 61-77 128. Plioplys A. Autism: electroencephalographic abnormalities and clinical improvement with valproic acid. Arch Pediatr Adolesc Med 1994; 148: 220-2 129. Howlin P. Behavioural techniques to reduce self-injurious behaviour in children with autism. Acta Paedopsychiatrica 1993; 56: 75-84
Correspondence and reprints: Prof. Jan K. Buitelaar, Dept. of Child Psychiatry, B.01.324, PO Box 85500, 3508 GA Utrecht, The Netherlands. E-mail: J.K.Buitelaar@psych.azu.nl
Adis International Limited. All rights reserved.
Paediatr Drugs 2000 Jan-Feb; 2 (1)
Anda mungkin juga menyukai
- Icra KakDokumen10 halamanIcra KakPakde Putu HadiBelum ada peringkat
- Lung VolumesDokumen19 halamanLung VolumesPakde Putu HadiBelum ada peringkat
- Biofarma2 Line10Dokumen3 halamanBiofarma2 Line10Pakde Putu HadiBelum ada peringkat
- Hypertension JNC 7Dokumen7 halamanHypertension JNC 7Syahrurrahman BokowBelum ada peringkat
- 45207821Dokumen8 halaman45207821Pakde Putu HadiBelum ada peringkat
- 1471 2334 13 438Dokumen7 halaman1471 2334 13 438Pakde Putu HadiBelum ada peringkat
- Heat StressDokumen15 halamanHeat StressPakde Putu HadiBelum ada peringkat
- 43688688Dokumen14 halaman43688688Pakde Putu HadiBelum ada peringkat
- Point BlankDokumen1 halamanPoint BlankPakde Putu HadiBelum ada peringkat
- BMC Surgery: Laparoscopic Versus Open Left Lateral SegmentectomyDokumen9 halamanBMC Surgery: Laparoscopic Versus Open Left Lateral SegmentectomyyashikiputuhadiBelum ada peringkat
- 34038092Dokumen7 halaman34038092Pakde Putu HadiBelum ada peringkat
- Alien 2 CheatDokumen1 halamanAlien 2 CheatPakde Putu HadiBelum ada peringkat
- Autism SocialDokumen16 halamanAutism SocialPakde Putu HadiBelum ada peringkat
- Barthel IndexDokumen2 halamanBarthel Indexgania100% (1)
- Point BlankDokumen1 halamanPoint BlankPakde Putu HadiBelum ada peringkat
- Alien 2 CheatDokumen1 halamanAlien 2 CheatPakde Putu HadiBelum ada peringkat
- Autism and Autism Spectrum Disorders: Diagnostic Issues For The Coming DecadeDokumen9 halamanAutism and Autism Spectrum Disorders: Diagnostic Issues For The Coming DecadePakde Putu HadiBelum ada peringkat
- Brief Report: Does Eye Contact Induce Contagious Yawning in Children With Autism Spectrum Disorder?Dokumen6 halamanBrief Report: Does Eye Contact Induce Contagious Yawning in Children With Autism Spectrum Disorder?Pakde Putu HadiBelum ada peringkat
- Anatomi Dan FisiologiDokumen13 halamanAnatomi Dan FisiologiPakde Putu HadiBelum ada peringkat
- Alien 2 CheatDokumen1 halamanAlien 2 CheatPakde Putu HadiBelum ada peringkat
- Alien 2 CheatDokumen1 halamanAlien 2 CheatPakde Putu HadiBelum ada peringkat
- Alien 2 CheatDokumen1 halamanAlien 2 CheatPakde Putu HadiBelum ada peringkat
- In Its ClassicDokumen1 halamanIn Its ClassicPakde Putu HadiBelum ada peringkat
- Higher Algebra - Hall & KnightDokumen593 halamanHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Bases Neurobiologicas Dificultades Aprendizaje PDFDokumen5 halamanBases Neurobiologicas Dificultades Aprendizaje PDFMacarena MartínezBelum ada peringkat
- Other Health Impairment Eligibility DeterminationDokumen2 halamanOther Health Impairment Eligibility Determinationapi-539726271Belum ada peringkat
- Review of The Korean Medicine Studies For Attention Deficit Hyperactivity Disorder (ADHD) in ChildrenDokumen13 halamanReview of The Korean Medicine Studies For Attention Deficit Hyperactivity Disorder (ADHD) in Childrenchaitanya gBelum ada peringkat
- Weisz Et Al.2017 PDFDokumen39 halamanWeisz Et Al.2017 PDFDaria PasailaBelum ada peringkat
- Special Educational Needs in English Language Teaching: Towards A Framework For Continuing Professional DevelopmentDokumen9 halamanSpecial Educational Needs in English Language Teaching: Towards A Framework For Continuing Professional DevelopmentjanismoreBelum ada peringkat
- ADHD and DepressionDokumen8 halamanADHD and DepressionVicki B VeeBelum ada peringkat
- 1999 Mirsky Model Attention ADHDDokumen9 halaman1999 Mirsky Model Attention ADHDEduardo CastilloBelum ada peringkat
- PEd 5 MODULE 6-SummerDokumen10 halamanPEd 5 MODULE 6-SummerRebecca CodiamatBelum ada peringkat
- Disability Ncert Publication 2018Dokumen88 halamanDisability Ncert Publication 2018Ikinnou BrahimBelum ada peringkat
- Currentstatusof Cognitivebehavioral Therapyforadult Attention-Deficit Hyperactivity DisorderDokumen13 halamanCurrentstatusof Cognitivebehavioral Therapyforadult Attention-Deficit Hyperactivity Disordershofa nur rahmannisaBelum ada peringkat
- H6 @the Effect of Social Media Addiction On Consumer Behavior - A CultDokumen71 halamanH6 @the Effect of Social Media Addiction On Consumer Behavior - A CultAnindithaptrBelum ada peringkat
- 15-Day-Fix-to-Stop-Defiant-Behavior-in-its-Tracks For ParentsDokumen10 halaman15-Day-Fix-to-Stop-Defiant-Behavior-in-its-Tracks For ParentsAnila OmerBelum ada peringkat
- JAP244 Answer Key 4Dokumen5 halamanJAP244 Answer Key 4Kenneth Sacdalan AdrimisinBelum ada peringkat
- Alicia Marchini CVDokumen5 halamanAlicia Marchini CVapi-290300066Belum ada peringkat
- Neurodevelopmental Disorders FinalDokumen7 halamanNeurodevelopmental Disorders FinalAARON JOHN VIRAYBelum ada peringkat
- The Power of Positive Teaching PDFDokumen127 halamanThe Power of Positive Teaching PDFMohammad Umar RehmanBelum ada peringkat
- NPB 168 Practice Exam 2Dokumen5 halamanNPB 168 Practice Exam 2Kim Wong100% (1)
- (Megan Moore Duncan, Jeanne Holverstott, Brenda SMDokumen540 halaman(Megan Moore Duncan, Jeanne Holverstott, Brenda SMAlejandro PiccoBelum ada peringkat
- Elisa W V City of New York Class Action ComplaintDokumen256 halamanElisa W V City of New York Class Action ComplaintRick ThomaBelum ada peringkat
- Autism Adhd Evaluation PDFDokumen13 halamanAutism Adhd Evaluation PDFShoba MacintyreBelum ada peringkat
- 5 Artikel Special NeedsDokumen19 halaman5 Artikel Special NeedsHisham IbrahimBelum ada peringkat
- Apnea KidsDokumen5 halamanApnea KidsVeenu KhubnaniBelum ada peringkat
- TRF Proficient TeachersDokumen10 halamanTRF Proficient TeachersQuerobin GampayonBelum ada peringkat
- Psychopharmacology - Child and AdolescentDokumen498 halamanPsychopharmacology - Child and AdolescentGabi CerchezBelum ada peringkat
- The Dyslexic Reader 2013 - Issue 63Dokumen32 halamanThe Dyslexic Reader 2013 - Issue 63Davis Dyslexia Association InternationalBelum ada peringkat
- BROMOCRIPTINE in Patients With Attention Deficit Hyperactive DisorderDokumen46 halamanBROMOCRIPTINE in Patients With Attention Deficit Hyperactive DisorderOlayinka Awofodu100% (1)
- Autism-Spectrum-Disorders-an-Intervention-Approach LAO JIDokumen12 halamanAutism-Spectrum-Disorders-an-Intervention-Approach LAO JIErica Alejandra SchumacherBelum ada peringkat
- Depressão e Ansiedade e TdahDokumen185 halamanDepressão e Ansiedade e TdahErika MagalhãesBelum ada peringkat
- Children With Autism and Attention Deficit Hyperactivity Disorder.Dokumen10 halamanChildren With Autism and Attention Deficit Hyperactivity Disorder.Marcelo GuimarãesBelum ada peringkat
- UKA Athletics Coach Induction Pack v2 Jan 2013Dokumen36 halamanUKA Athletics Coach Induction Pack v2 Jan 2013gpitbullBelum ada peringkat