Nasal Continuous Positive Airway Pressure For Neonates & Infants
Diunggah oleh
Ywagar YwagarDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Nasal Continuous Positive Airway Pressure For Neonates & Infants
Diunggah oleh
Ywagar YwagarHak Cipta:
Format Tersedia
Tasmanian Health Organisation - North
NEONATAL UNIT LGH SDMS Id No.: P2012/0451-001 Procedure No: 4.26/12WACS
Nasal Continuous Positive Airway Pressure (NCPAP) for Neonates and Infants Procedure
Application: Approved by: Effective Date: Custodian and Review Responsibility: Review Date: Version: Registered/Enrolled Nurses/Medical Staff, QVMU Director of Paediatrics, LGH 2 August 2012 Quality and Clinical Improvement Nurse Paediatrics/Neonates
2 August 2015 Version No. 1 Policy No: 4.26
Background
Tasmanian infants from 30 weeks gestation are currently able to be managed at the Launceston General Hospital (LGH) in accordance with the Neonatal and Paediatric ICU, Tasmania Admission Guideline. NCPAP is used as one of the modalities for the management of respiratory distress of neonates and it is the purpose of this document to provide guidelines for NCPAP at the LGH, with input from the Neonatologists at the RHH. The use of NCPAP in a level 2 unit such as the LGH reduces the need for transfer, but is relatively resource intensive in regards to equipment, medical staff availability and skilled nursing care. This guideline will cover 3 main areas: 1 A clinical protocol with indication, contraindications, technique, assessment of success/failure, discontinuation, complications, and monitoring requirements. Medical staff resources Nursing staff resources
2 3
This document will NOT describe the total care related to a sick baby, but only aspects of care relevant to NCPAP.
Procedure
Causes of respiratory distress in neonates
Note: PLEASE DESTROY PRINTED COPIES. The electronic version of this Procedure is the approved and current version and is located on the departments intranet. Any printed version is uncontrolled and therefore not current. Page
1 of 5
Respiratory distress syndrome (HMD) Transient tachypnoea of the neonate (TTN)
Congenital pneumonia (carefully evaluate suitability of ongoing NCPAP at LGH, depending on clinical course as these babies are at an increased risk of requiring intubation and ventilation) Meconium aspiration (carefully evaluate suitability for NCPAP) Pneumothorax (not suitable for NCPAP) Congenital abnormalities (not suitable for ongoing NCPAP at LGH, discuss with RHH) o o o o Pulmonary hypoplasia Diaphragmatic hernia Airway obstruction Congenital cardiac disease
Indications for NCPAP at LGH
Infants should meet the following criteria: Gestation > 30 weeks Clinical signs of respiratory distress (nasal flare, tachypnoea, grunt, recession) Oxygen requirement of >30% to keep oxygen saturation 92-96% A CXR consistent with respiratory disease
Contraindications
Gestation < 30 weeks (does not preclude using NCPAP as a pretransfer modality for these babies) Insufficient medical or nursing resources Rising FiO2 > 0.4 (i.e. 40%oxygen) (discuss with RHH) Significant apnoea
Technique and monitoring required
The recommended starting level of NCPAP is 5-7cm H20 and titrated to patients condition. The maximum level of NCPAP pressure is 8cm H20. Maintenance intravenous fluids are required Expressed colostrum can be given at the discretion of the paediatrician Continuous pulse oximetry and oxygen saturation monitoring Indwelling arterial line for BP and intermittent blood gas estimations if FiO2 > 0.4 is recommended
Page
Note: PLEASE DESTROY PRINTED COPIES. The electronic version of this Procedure is the approved and current version and is located on the departments intranet. Any printed version is uncontrolled and therefore not current.
2 of 5
Standard cardio respiratory monitoring including blood pressure Regular inspection of the ventilatory circuit and equipment which includes 1 2 3 4 prong position and orientation the need for a chin strap water in circuit is the expiratory limb bubbling?
Assessment of failure of NCPAP
FiO2 rising above 0.4 Ongoing respiratory acidosis ph < 7.25, PaCO2 > 50 mmHg Recurrent apnoea requiring stimulation Recurrent episodes of significant desaturation (<90% for >20 sec) Worsening sternal and intercostal recession/grunt/tachypnoea Agitation not relieved by simple measures (comforting, paracetamol) Development of pneumothorax.
An immediate medical assessment and CXR is required and the consultant notified. Consideration should be given to notifying the RHH neonatologist of the babys condition. A positive response to NCPAP includes a reduction in respiratory rate, resolution of grunting, stabilization or reduction of FiO2, and reduction in recession.
Discontinuation
Once a babys respiratory rate falls below 60/minute, the Fi02 is < 0.3 and the baby is breathing with less effort, the CPAP and FiO2 can be weaned and stopped. There is no clear evidence as to the best weaning strategy, but once the FiO2 is 0.210.23 the CPAP could be reduced by 1 cm H2O every 6-12 hours, until stable at 5 Cm H2O, and then trialled off. It is not uncommon to see a slight increase in respiratory rate and FiO2 in the 1st hour after discontinuation.
Complications
Pneumothorax Agitation Continued deterioration Nasal trauma Abdominal distension
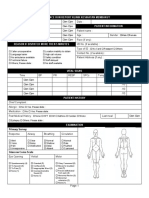
Documentation
Observation chart for hourly recording of: Vital signs and work of breathing
Note: PLEASE DESTROY PRINTED COPIES. The electronic version of this Procedure is the approved and current version and is located on the departments intranet. Any printed version is uncontrolled and therefore not current. Page
3 of 5
FiO2 CPAP pressure Gas flow Humidifier and circuit temperature Water level in humidifier
Medical resources
A baby should not be started on NCPAP without the involvement of the Consultant Paediatrician. 24 hour registrar cover must be available on site or within 10 minutes
The registrar must have recognised neonatal resuscitation training Knowledge about the indications for NCPAP Knowledge about the complications of NCPAP Knowledge about the expected course of neonates on NCPAP The Consultant Paediatrician must be immediately contactable by phone, and no more than 30 minutes away, experienced in the use of CPAP and able to manage the complications ie: drainage of pneumothorax, intubation and ventilation.
Nursing Resources
Completed LGH resuscitation education The nurse to patient ratio should be 1:1 and able to be maintained for duration of care There needs to be agreement between the nursing and medical staff that 1:1 nursing would be available for the patient on NCPAP (typically for 24-72 hours) Competent in care of baby with CPAP Knowledgeable of the indications for and contraindications of commencing a neonate on CPAP Knowledgeable of the expected course of neonates on CPAP
When should NETS (RHH) be notified:
Any baby not following the expected course on NCPAP Failure of NCPAP as above Babies under 30 weeks gestational age Babies not managing enteral nutrition and requiring parental nutrition
Note: PLEASE DESTROY PRINTED COPIES. The electronic version of this Procedure is the approved and current version and is located on the departments intranet. Any printed version is uncontrolled and therefore not current. Page
4 of 5
There is the potential for babies over 30 weeks gestational age, from the North West Regional Hospital and Mersey Community Hospital with respiratory distress, to be managed with NCPAP at the LGH. This would need to be in discussion with both the LGH Paediatrician as well as the RHH Neonatologist, as the risk that they might need ventilation and thus further retrieval to RHH needs to be assessed.
Responsibilities/Delegations
Nursing and Medical Staff Neonatal Nursery LGH, QVMU.
Related Documents/Legislation
1 http://www.health.vic.gov.au/neonatal/nasalcpapguidelines.pdf
Dr Ingrid Els Malcolm Gulliver Chris Coker Chris Bailey Consultant Paediatrician Position Title Nurse Unit Manager Paeds Exec 6348 8991 6348 7374 6348 8944 6348 8974 June 2012 June 2012 June 2012 2 August 2012 Prepared by Through Through Cleared by
Note: PLEASE DESTROY PRINTED COPIES. The electronic version of this Procedure is the approved and current version and is located on the departments intranet. Any printed version is uncontrolled and therefore not current. Page
5 of 5
Anda mungkin juga menyukai
- Walhalla Gold MineDokumen1 halamanWalhalla Gold MineYwagar YwagarBelum ada peringkat
- Sydney 2008 MarchDokumen8 halamanSydney 2008 MarchYwagar YwagarBelum ada peringkat
- Clinical Recall 17 May 2008 Melbourne: AMC Feedback: Sudden Infant Death SyndromeDokumen14 halamanClinical Recall 17 May 2008 Melbourne: AMC Feedback: Sudden Infant Death SyndromeYwagar YwagarBelum ada peringkat
- AMC Clinical Exam Recall 8 Sep 2008 Melbourne Retest 1Dokumen7 halamanAMC Clinical Exam Recall 8 Sep 2008 Melbourne Retest 1Ywagar YwagarBelum ada peringkat
- Adelaide, 5 April, 2008: PaediatricsDokumen17 halamanAdelaide, 5 April, 2008: PaediatricsYwagar YwagarBelum ada peringkat
- Recall Brisbane February 2008Dokumen7 halamanRecall Brisbane February 2008Ywagar YwagarBelum ada peringkat
- GPDokumen3 halamanGPYwagar YwagarBelum ada peringkat
- Brisbane July 2008 RecallDokumen11 halamanBrisbane July 2008 RecallYwagar YwagarBelum ada peringkat
- Gold Coast 2008Dokumen1 halamanGold Coast 2008Ywagar YwagarBelum ada peringkat
- Draft May 08 WES ProgramDokumen2 halamanDraft May 08 WES ProgramYwagar YwagarBelum ada peringkat
- Dr CAI clinical cases under 40 charsDokumen31 halamanDr CAI clinical cases under 40 charsYwagar Ywagar100% (1)
- Adelaide April 2008Dokumen16 halamanAdelaide April 2008Ywagar YwagarBelum ada peringkat
- Melbourne 2008 Nov 8Dokumen10 halamanMelbourne 2008 Nov 8Ywagar YwagarBelum ada peringkat
- Adelaide 13th September 2008Dokumen16 halamanAdelaide 13th September 2008Ywagar YwagarBelum ada peringkat
- Adelaide 13th September 2008Dokumen16 halamanAdelaide 13th September 2008Ywagar YwagarBelum ada peringkat
- Syd 1Dokumen11 halamanSyd 1Ywagar YwagarBelum ada peringkat
- Adel 2Dokumen24 halamanAdel 2Ywagar YwagarBelum ada peringkat
- Adelaide 13th September 2008Dokumen16 halamanAdelaide 13th September 2008Ywagar YwagarBelum ada peringkat
- Paediatrics:: Case 1nsionDokumen16 halamanPaediatrics:: Case 1nsionYwagar YwagarBelum ada peringkat
- Melb RetestDokumen6 halamanMelb RetestYwagar YwagarBelum ada peringkat
- MelbDokumen9 halamanMelbYwagar YwagarBelum ada peringkat
- ACln2007!09!08MEL Retest Wd97Dokumen6 halamanACln2007!09!08MEL Retest Wd97Ywagar YwagarBelum ada peringkat
- Brisbane, 11th October 2008Dokumen6 halamanBrisbane, 11th October 2008Ywagar YwagarBelum ada peringkat
- Melb RetestDokumen2 halamanMelb RetestYwagar YwagarBelum ada peringkat
- To ReviseAug 22 AdelaideDokumen4 halamanTo ReviseAug 22 AdelaideYwagar YwagarBelum ada peringkat
- BrisDokumen9 halamanBrisYwagar YwagarBelum ada peringkat
- Brisbane, 11th October 2008Dokumen6 halamanBrisbane, 11th October 2008Ywagar YwagarBelum ada peringkat
- Melb RetestDokumen4 halamanMelb RetestYwagar YwagarBelum ada peringkat
- 9 August 08 Melbourne Clinical Exam RecallDokumen6 halaman9 August 08 Melbourne Clinical Exam RecallYwagar YwagarBelum ada peringkat
- Clinical Recall 17 May 2008 Melbourne: AMC Feedback: Sudden Infant Death SyndromeDokumen14 halamanClinical Recall 17 May 2008 Melbourne: AMC Feedback: Sudden Infant Death SyndromeYwagar YwagarBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Physioex Ex 7 AnswersDokumen5 halamanPhysioex Ex 7 AnswersTin-tinBelum ada peringkat
- Lung conditions: Atelectasis, tuberculosis, abscess and pleural effusionDokumen14 halamanLung conditions: Atelectasis, tuberculosis, abscess and pleural effusionSasha IfahmyBelum ada peringkat
- Ecografia Pulmonar NeonatalDokumen12 halamanEcografia Pulmonar NeonatalJorge CastroBelum ada peringkat
- Emergency Nursing (Medical Emergencies - ABC) - StudentsDokumen19 halamanEmergency Nursing (Medical Emergencies - ABC) - StudentsAngielyn Ramos OlorazaBelum ada peringkat
- Pulmonology Exam: Comprehensive Chest AssessmentDokumen33 halamanPulmonology Exam: Comprehensive Chest AssessmentSagit Nauman81Belum ada peringkat
- AtlsDokumen23 halamanAtlsvivi chanBelum ada peringkat
- Ear ReconstructionDokumen15 halamanEar ReconstructionENDAH RAMADHATININGSIH 1Belum ada peringkat
- Rare Lung Disease Affecting Women: LymphangioleiomyomatosisDokumen11 halamanRare Lung Disease Affecting Women: LymphangioleiomyomatosisAbuzdea AlexBelum ada peringkat
- Orthopaedics & Trauma: SamsonDokumen17 halamanOrthopaedics & Trauma: Samsonزكريا عمرBelum ada peringkat
- Pneumocystis Carinii PneumoniaDokumen16 halamanPneumocystis Carinii PneumoniaHera HeraBelum ada peringkat
- Thoracostomy Tubes and Catheters: Indications and Tube Selection in Adults and ChildrenDokumen20 halamanThoracostomy Tubes and Catheters: Indications and Tube Selection in Adults and ChildrenaraBelum ada peringkat
- Endobronchial ValvesDokumen11 halamanEndobronchial ValvesMad MadBelum ada peringkat
- Trauma Assessment Initial Trauma AssessmentDokumen6 halamanTrauma Assessment Initial Trauma Assessmentrika100% (1)
- S Tahel 2005Dokumen12 halamanS Tahel 2005Catherine MorrisBelum ada peringkat
- Approach To The Patient With DyspneaDokumen22 halamanApproach To The Patient With DyspneaLuis Gerardo Alcalá GonzálezBelum ada peringkat
- Left Pneumothorax CaseDokumen2 halamanLeft Pneumothorax CaseAnonymous iOpPt7sIoBelum ada peringkat
- Disorders of The PleuraDokumen31 halamanDisorders of The PleuraKathleen Dela CruzBelum ada peringkat
- Meconium Aspiration Syndrome, Management ofDokumen9 halamanMeconium Aspiration Syndrome, Management ofGinaJaraBelum ada peringkat
- Kaplan Decision Tree and All Nurses NotesDokumen103 halamanKaplan Decision Tree and All Nurses NotesTravel Junky100% (1)
- Cirugia ToraxDokumen117 halamanCirugia ToraxErwin GuerreroBelum ada peringkat
- TV MCQ Pertanyaan TokDokumen5 halamanTV MCQ Pertanyaan TokdhinahafizBelum ada peringkat
- Neonatal Autopsy Technique Special Dissection ProceduresDokumen55 halamanNeonatal Autopsy Technique Special Dissection ProceduresRoman MamunBelum ada peringkat
- Pathophysiology of pneumothorax and hemothoraxDokumen3 halamanPathophysiology of pneumothorax and hemothoraxAllana RayosBelum ada peringkat
- Unusual Presentations of Child Abuse, A Report of Two Cases and The Role of ImagingDokumen5 halamanUnusual Presentations of Child Abuse, A Report of Two Cases and The Role of ImaginggeaninalexaBelum ada peringkat
- Nursing Test 3 (NP Iii)Dokumen17 halamanNursing Test 3 (NP Iii)Yuxin LiuBelum ada peringkat
- PRE Test 1Dokumen15 halamanPRE Test 1Naomi VirtudazoBelum ada peringkat
- UHS-OSPE of Medicine (Annual 2009Dokumen13 halamanUHS-OSPE of Medicine (Annual 2009Latif RanaBelum ada peringkat
- Borang Ambulans CallDokumen2 halamanBorang Ambulans Callleo89azman100% (1)
- Oxygenation NCM 103Dokumen10 halamanOxygenation NCM 103Richmond LacadenBelum ada peringkat
- Blue ProtocolDokumen11 halamanBlue Protocoloana florianaBelum ada peringkat