Blood Sugar Testing Overview
Diunggah oleh
Apple RamosHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Blood Sugar Testing Overview
Diunggah oleh
Apple RamosHak Cipta:
Format Tersedia
BLOOD SUGAR TESTING OVERVIEW If you have diabetes, you have an important role in your own medical care,
and testing your blood glucose (also called blood sugar) is an opportunity for you to take control of your health. Although diabetes is a chronic condition, it can usually be controlled with lifestyle changes and medication. The main goal of treatment is to keep blood sugar levels in the normal or nearnormal range. Checking your blood sugar is one of the best ways to know how well your diabetes treatment plan is working. Continuous glucose monitors have also become popular, especially for people who use an insulin pump. (See 'Continuous glucose monitoring' below.) A healthcare provider will periodically order a laboratory blood test to determine your blood sugar levels and hemoglobin A1c (A1C). This test gives an overall sense of how blood sugar levels are controlled since it indicates your average blood sugar level of the past two to three months (table 1). However, fine-tuning of blood sugar levels and treatment also requires that you monitor your own blood sugar levels on a day-to-day basis. Self-blood glucose monitoring allows you to know your blood glucose level at any time and helps prevent the consequences of very high or very low blood sugar. Monitoring also enables tighter blood sugar control, which decreases the long-term risks of diabetic complications. HOW TO PERFORM BLOOD SUGAR TESTING The following steps include general guidelines for testing blood sugar levels; you should get specific details for your blood glucose monitors from the package insert or your healthcare provider. Never share blood glucose monitoring equipment or fingerstick lancing devices. Sharing of this equipment could result in transmission of infection, such as hepatitis B.
Wash hands with soap and warm water. Dry hands. Prepare the lancing device by inserting a fresh lancet. Lancets that are used more than once are not as sharp as a new lancet, and can cause more pain and injury to the skin. Prepare the blood glucose meter and test strip (instructions for this depend upon the type of glucose meter used). Use the lancing device to obtain a small drop of blood from your fingertip or alternate site (like the skin of the forearm) (picture 1). Alternate sites are often less painful than the fingertip. However, results from alternate sites are not as accurate as fingertip samples when the blood glucose is rising or falling rapidly (picture 2). If you have difficulty getting a good drop of blood from the fingertip, try rinsing your fingers with warm water, shaking the hand below the waist, or squeezing ("milking") the fingertip. Apply the blood drop to the test strip in the blood glucose meter. The results will be displayed on the meter after several seconds. Dispose of the used lancet in a puncture-resistant sharps container (not in household trash).
FREQUENCY OF BLOOD SUGAR TESTING Studies have proven that people with type 1 and 2 diabetes who maintain normal or near normal blood sugar levels have a lower risk of diabetes-related complications than those who have high blood sugar levels. How frequently you test will depend upon the type of diabetes you have (1 or 2) and which treatment(s) you use (insulin versus oral medications or lifestyle changes). Type 1 diabetes For people with type 1 diabetes, frequent testing is the only way to safely and effectively manage blood sugar levels. (See "Patient information: Diabetes mellitus type 1: Overview".) Most people need to test at least four times per day. If you use an insulin pump, give three or more insulin injections per day, or are a women with type 1 diabetes who is pregnant, you may need to test as many as seven times per day or more. (See "Patient information: Care during pregnancy for women with type 1 or 2 diabetes mellitus".) People who test frequently, especially those using intensive insulin therapy, may consider purchasing several blood glucose monitors to keep at home, work, school, or in a purse or backpack. This allows easier access to testing equipment, which can increase testing frequency and therefore improve blood sugar control. Type 2 diabetes Blood sugar monitoring is also important for people with type 2 diabetes. The recommendations for how often you should test are based upon individual factors such as type of treatment (diet versus oral medication versus insulin), level of hemoglobin A1c (A1C), and treatment goals. A healthcare provider can help you determine how frequently to test. (See "Patient information: Diabetes mellitus type 2: Overview".) INTERPRETING BLO
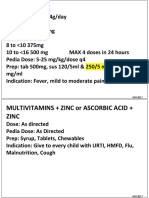
Blood Glucose Monitoring Definition
Blood glucose monitoring is a method of assessing the concentration of glucose in the blood. Tests are performed rapidly and easily by using a reagent strip (e.g. Glucostix) where a minute drop of capillary blood is obtained from the clients digits (finger or toe), earlobe or heel. On the condition where the patient has all the equipments this test can be performed at home, office, hospitals, clinics and even when travelling. Purpose Blood glucose tests detect blood glucose levels in people with the following conditions: 1. 2. 3. 4. Diabetes Mellitus (Type 1, Type 2) Gestational diabetes Neonatal hypoglycemia Diabetic Coma
During the test, a portable blood glucose meter (e.g. Glucometer or One Touch) is used to give numerical data or measurement of a patients serum glucose level by inserting the blood stained plastic strip. Some meters are installed with memory application helpful in storing the sequence of test results obtained for easy evaluation.
Paraphernalia 1. 2. 3. 4. 5. 6. 7. Reagent strips or test strip Clean Gloves Alcohol pads Lancets or lancing device Portable glucose meter Watch (with second hand) Pen and Logbook for documentation
Procedure 1. Identify the patient by asking the patient to state his/her name. Also check the clients identification band. ( confirm patients identity using two patient identifiers, based on the hospital protocol) 2. Explain the procedure to the patient or parents (if patient is a child) to gain cooperation.
3. Choose the puncture site. For adults and children fingertips and earlobe can be use. For infants, the tip of the great toe or heel can be the site of puncture. 4. Wash hands and don clean gloves. 5. If glucometer is used, load the strip into the device beforehand. 6. Swab alcohol pad to the chosen puncture site. Use sterile/clean gauze to dry it thoroughly. Piecing the skin with a wet skin (alcohol) allows the chemical to pass through the outer layer of the skin thus, causing the procedure more painful and uncomfortable. 7. To collect a blood sample, position the lancet (pricking needle) at the side of the site. To minimize pain and patients anxiety pierce the skin sharply and briefly. This technique also increases blood flow. For better results, some agencies are using a lancing device (mechanical blood-letting device) wherein the lancets are simply loaded in the spring of the equipment. (Its like using a spring-loaded pen, once you click the button the spring releases the lancet and immediately retracts it after piercing the skin). However, be sure to load an unused lancet before using to prevent spread of blood-transmitted diseases.
8. Dont squeeze the puncture site to prevent diluting the sample with fluids from tissues. 9. Cover the entire patch of strip with blood. 10. Place gauze over the punctured area and briefly apply pressure until the bleeding stops. Ask the parents of a child to do this. 11. If using a reagent strip, leave the blood on the strip for 1 minute (60 seconds). And watch the color change on the strip while comparing it to the standardized color chart of the product container. 12. If glucometer is used, simply follow the manufacturers instruction. 13. Apply an adhesive bandage once the bleeding on the puncture site has stopped. 14. Remove gloves and record the resulting glucose level from the digital display for glucometer or from the color of reagent strip to the standardized chart. Common Errors in Blood Glucose Monitoring 1. Dropping a very small amount of blood 2. Inappropriate timing ( the test is usually performed before meals and at bedtime, or whenever hypoglycemia or hyperglycemia occurs) 3. Squeezing the puncture site too hard allowing tissue fluids to mix with the sample
4. Improper maintenance of glucometers (dust or blood accumulation on the digital display)
Anda mungkin juga menyukai
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- FORTRESS EUROPE by Ryan BartekDokumen358 halamanFORTRESS EUROPE by Ryan BartekRyan Bartek100% (1)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Cambridge English First Fce From 2015 Reading and Use of English Part 7Dokumen5 halamanCambridge English First Fce From 2015 Reading and Use of English Part 7JunanBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Presentation On HR Department of Mobilink.Dokumen18 halamanPresentation On HR Department of Mobilink.Sadaf YaqoobBelum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- 20 Great American Short Stories: Favorite Short Story Collections The Short Story LibraryDokumen10 halaman20 Great American Short Stories: Favorite Short Story Collections The Short Story Librarywileyh100% (1)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Effective Communication Chapter11Dokumen9 halamanEffective Communication Chapter11kamaljeet70Belum ada peringkat
- Pemphigus Subtypes Clinical Features Diagnosis andDokumen23 halamanPemphigus Subtypes Clinical Features Diagnosis andAnonymous bdFllrgorzBelum ada peringkat
- Durability Problems of 20 Century Reinforced Concrete Heritage Structures and Their RestorationsDokumen120 halamanDurability Problems of 20 Century Reinforced Concrete Heritage Structures and Their RestorationsManjunath ShepurBelum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Presentation (AJ)Dokumen28 halamanPresentation (AJ)ronaldBelum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Automated Long-Distance HADR ConfigurationsDokumen73 halamanAutomated Long-Distance HADR ConfigurationsKan DuBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Detailed Lesson Plan in PED 12Dokumen10 halamanDetailed Lesson Plan in PED 12alcomfeloBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Reviewer in Auditing Problems by Reynaldo Ocampo PDFDokumen1 halamanReviewer in Auditing Problems by Reynaldo Ocampo PDFCarlo BalinoBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Basic Catholic Prayer 1Dokumen88 halamanBasic Catholic Prayer 1Josephine PerezBelum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- 9 Prospect EvaluationDokumen40 halaman9 Prospect EvaluationgeorgiadisgBelum ada peringkat
- Caisley, Robert - KissingDokumen53 halamanCaisley, Robert - KissingColleen BrutonBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Caste & PoliticsDokumen4 halamanCaste & PoliticsGIRISHA THAKURBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Functions of Ecgc and Exim BankDokumen12 halamanFunctions of Ecgc and Exim BankbhumishahBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Pengaruh Kompetensi Spiritual Guru Pendidikan Agama Kristen Terhadap Pertumbuhan Iman SiswaDokumen13 halamanPengaruh Kompetensi Spiritual Guru Pendidikan Agama Kristen Terhadap Pertumbuhan Iman SiswaK'lala GrianBelum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Common RHU DrugsDokumen56 halamanCommon RHU DrugsAlna Shelah IbañezBelum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Project Dayan PrathaDokumen29 halamanProject Dayan PrathaSHREYA KUMARIBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Chargezoom Achieves PCI-DSS ComplianceDokumen2 halamanChargezoom Achieves PCI-DSS CompliancePR.comBelum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Datsasheet of LM347 IcDokumen24 halamanDatsasheet of LM347 IcShubhamMittalBelum ada peringkat
- Paper 2Dokumen8 halamanPaper 2Antony BrownBelum ada peringkat
- Fundamentals of Marketing Management: by Prabhat Ranjan Choudhury, Sr. Lecturer, B.J.B (A) College, BhubaneswarDokumen53 halamanFundamentals of Marketing Management: by Prabhat Ranjan Choudhury, Sr. Lecturer, B.J.B (A) College, Bhubaneswarprabhatrc4235Belum ada peringkat
- Mus Culo SkeletalDokumen447 halamanMus Culo SkeletalKristine NicoleBelum ada peringkat
- Theology and Pipe Smoking - 7pDokumen7 halamanTheology and Pipe Smoking - 7pNeimar HahmeierBelum ada peringkat
- Ghosh, D. P., 1971, Inverse Filter Coefficients For The Computation of Apparent Resistivity Standard Curves For A Horizontally Stratified EarthDokumen7 halamanGhosh, D. P., 1971, Inverse Filter Coefficients For The Computation of Apparent Resistivity Standard Curves For A Horizontally Stratified EarthCinthia MtzBelum ada peringkat
- Sample ProposalDokumen2 halamanSample ProposaltoupieBelum ada peringkat
- 08 Night 09 Days Ujjain & Omkareshwar Tour Package - Travel HuntDokumen5 halaman08 Night 09 Days Ujjain & Omkareshwar Tour Package - Travel HuntsalesBelum ada peringkat
- Bad SenarioDokumen19 halamanBad SenarioHussain ElboshyBelum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)