Abdominal Pain in Children and The Diagnosis of Appendicitis
Diunggah oleh
vali2013Deskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Abdominal Pain in Children and The Diagnosis of Appendicitis
Diunggah oleh
vali2013Hak Cipta:
Format Tersedia
..................................
Best Practice
EVIDENCE-BASED CASE REVIEWS
Abdominal pain in children and the diagnosis of appendicitis
..................................................................................................
Carolyn A Paris Eileen J Klein
.........................................................................................................
Department of Pediatrics University of Washington and Childrens Hospital and Regional Medical Center 4800 Sand Point Way NE (Mailstop CH-04) Seattle, WA 98105 Correspondence to:
Dr Paris
cparis@chmc.org
Competing interests:
None declared West J Med 2002;176:104-107
A 5-year-old girl presents to the emergency department (ED) because of vomiting, abdominal pain, and fever for the past 36 hours. The pain is periumbilical and cramping in nature, and its location has not changed since onset. The child does not have diarrhea, rash, dysuria, sore throat, or upper respiratory tract symptoms. Her temperature is 38.7C (101.7F), and abdominal examination reveals diffuse tenderness to deep palpation with notable rebound tenderness. There is guarding, and the pain does not decrease when the patient is distracted. The findings of the examination are otherwise normal. Plain abdominal radiographs show no abnormalities. The white blood cell (WBC) count is 16.9 109/L (16,900/L) with 0.88 (88%) neutrophils. The patient is unable to provide a urine specimen. You are concerned that this child might have acute appendicitis and question the value of the history, examination, and preliminary investigations in confirming this diagnosis.
.........................................................................................................
Summary points
Pain duration by history should not influence the decision to operate on a patient with abdominal pain, but pain present for a short (<7 hours) or a long duration (>48 hours) is unlikely to be due to appendicitis In isolation, a history of vomiting does not help make the diagnosis of appendicitis. However, in combination with historical and physical findings (such as right lower quadrant pain or abdominal tenderness or guarding), vomiting may help predict appendicitis Rebound tenderness on physical examination may be a useful predictor of appendicitis in a child with a high probability of having acute appendicitis. Furthermore, in a patient with few other findings that suggest appendicitis, a lack of guarding on physical examination may indicate that observation, rather than operation, would be prudent Appendicitis is unlikely to be present when the white blood cell count is low, unless the pretest probability of appendicitis is high. A high white blood cell count for age increases suspicion for acute appendicitis, although whether there is an upper limit is unclear Ultrasonography is most helpful for ruling in appendicitis, primarily in patients with equivocal clinical findings Computed tomography is most helpful in patients who have a nonconclusive ultrasonogram and in whom there is still concern about the diagnosis of appendicitis. No studies have shown it to be clearly superior to ultrasonography
Appendicitis is among the most serious causes of acute abdominal pain and is the most common indication for emergency abdominal surgery in children. Its incidence varies with age, sex, and clinical setting in which patients are evaluated. The prevalence of abdominal pain among pediatric ED or outpatient clinic patients is 3.0% to 5.1% for pain of less than 3 days duration and 8.1% for pain of any duration. Appendicitis explains 1% of abdominal pain episodes, and the incidence peaks in older children and adolescents, with an estimated rate of 23.3 per 10,000 population per year in persons aged 10 to 19 years. The male-to-female ratio is 1.4:1.1,2 Of children undergoing appendectomy for presumed appendicitis, 10% to 40% have a normal appendix and usually a nonsurgical explanation for their abdominal pain.3-10 In 15% to 40% of those undergoing appendectomy who do have appendicitis, it will have progressed to perforation3,5,7,9,10; this proportion is even higher (71%100%) in children younger than 6 years.10,11 Perforation rates are higher in boys. Negative appendectomies occur more commonly in postpubertal girlsthe threshold for
104 wjm Volume 176 March 2002
surgery is lower in girls because of the risk of infertility associated with untreated peritonitis.3,6 Mortality has declined since the recognition of appendicitis in the 1800s; currently it is a cause of death in 0.02% to 0.8% of general populations studied.5,12 In one US community, death from undetected appendicitis in early childhood occurred in 4.5 per million children at risk per year.13 Prompt and accurate diagnosis of appendicitis remains the key to reducing morbidity and mortality. You wish to use an evidence-based approach to answer your questions about the diagnosis of appendicitis in children with abdominal pain. You start by looking for highquality evidence syntheses and evidence-based guidelines to answer your questions but are unable to find any systematic reviews of the diagnostic issues in question. Thus, you look for primary studies that compare findings with the standard for the diagnosis: histologically confirmed
www.ewjm.com
..................................
Best Practice
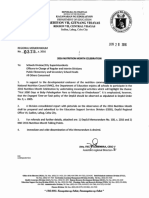
Search strategy by which to pursue answers to clinical scenario-generated questions
Question
Will historical details (ie, duration of pain, vomiting) help in the diagnosis of acute appendicitis? Will specific physical findings (ie, pain location, rebound tenderness) help in the diagnosis of acute appendicitis? Will laboratory measures of inflammation (eg, leukocyte count) help in the diagnosis of acute appendicitis? Will radiographic studies (ie, ultrasonography, computed tomographic scanning) help in the diagnosis of acute appendicitis?
*Limit to English-language journals, human subjects, and prospective studies for each. exp = explode/expand
Search strategy*
Appendicitis: diagnosis AND (exp: abdomen OR exp: pain) AND duration AND time factors Appendicitis: diagnosis AND (vomiting or nausea) Appendicitis: diagnosis AND exp: pain; limit children Appendicitis: diagnosis AND exp: leukocyte count Appendicitis: diagnosis AND ultrasonography Appendicitis: diagnosis AND computed tomography
appendicitis. The Table summarizes your questions and search strategies. HISTORICAL FINDINGS OShea and colleagues prospectively studied 246 patients aged between 3 and 18 years who had abdominal pain for less than 1 week.9 The standard for a diagnosis of appendicitis was the pathologic appearance of the appendix or patient status 1 week after the ED visit. The likelihood ratio (LR) for appendicitis for pain less than 12 hours versus greater than 12 hours was 0.64; for pain less than versus greater than 24 hours, the LR was 0.83. Andersson and colleagues prospectively evaluated 502 patients (aged 10-86 years) admitted to the hospital with abdominal pain and possible appendicitis for duration of pain and vomiting, dividing the pain duration into 6-hour increments up to 72 hours.14 The greatest LR was 1.7 at a pain duration of 7 to 12 hours (95% confidence interval [CI], 1.1-2.6). The LR for appendicitis in a patient with vomiting compared with no vomiting was 1.8 (95% CI, 1.4-2.4). If pain migrated to the right lower quadrant, the LR for appendicitis was 1.45 (95% CI, 1.07-1.99). If the pain did not migrate to the right lower quadrant, the LR was 0.74 (95% CI, 0.55-0.95). Reynolds and Jaffe prospectively studied 377 children (aged 2-16 years) seen in an ED with abdominal pain.15 In this study, the presence of two of four findings vomiting, right lower quadrant pain, abdominal tenderness, and abdominal guardinghad a sensitivity of 0.96 and a specificity of 0.72, which produces an LR of 3.4 for two or more of four predictors and an LR of 0.08 for having less than two of these four findings. Therefore, a patient with only one or none of these predictors is unlikely to have appendicitis. PHYSICAL FINDINGS Golledge and colleagues prospectively evaluated 100 patients (aged 4-81 years) who had right lower quadrant pain and possible appendicitis.16 The only findings with
www.ewjm.com
an LR of greater than 3.0 were rebound tenderness (LR, 7.4) and percussion tenderness (LR, 4.1) in the right lower quadrant. Alshehri and associates found less impressive results in 130 patients with suspected appendicitis (LR, 1.2) because 80% of their patients who did not have appendicitis also had rebound tenderness (20% specificity).17 They found similar LRs for guarding (1.2), Rovsings sign (1.5), and rigidity (1.7). The high sensitivities of these peritoneal signs (ie, probability of being present in patients who have appendicitis) mean that the absence of these signs may be more useful in ruling out the diagnosis of acute appendicitis. The lack of rebound tenderness gives a negative LR of 0.3 and lack of guarding, 0.06. The physical examination findings in the studies by OShea and colleagues and Reynolds and Jaffe provide insufficient information to influence your clinical practice and decision making.11,15 You conclude that rebound tenderness may be a useful predictor of appendicitis, but a lack of guarding on physical examination may sway you to observe, rather than operate on, a patient with few other findings that suggest appendicitis.
Appendicitis explains 1% of abdominal pain episodes in young children
Volume 176 March 2002 wjm 105
..................................
Best Practice
Laboratory findings Andersson and colleagues also studied the WBC count and found an LR for appendicitis of 0.16 for a total WBC count of less than 8.0 109/L (<8,000/L).14 The LR increased with rising WBC counts, to a maximum of 7.0 for a WBC count of 15.0 109/L (15,000/L) or more. The likelihood ratios and 95% confidence intervals for different levels of total WBC counts demonstrate that only at the extremes of the WBC count is this test clinically useful. Dueholm and associates reported the findings of a blind, prospective study that evaluated the usefulness of WBC count, neutrophil count, and C-reactive protein level in 237 patients (aged 15-45 years) with possible appendicitis.18 Using single cutoff values rather than stratified values of WBC means that information from individual strata are pooled, which results in smaller LRs. Izbicki and colleagues conducted a retrospective evaluation of 536 patients followed by a prospective evaluation of 150 patients with the presumed diagnosis of appendicitis.7,19 They also used single cutoff values, none of which are as useful as the stratified values evaluated by Andersson and co-workers. However, all of the available studies give consistent results and suggest that the diagnosis of appendicitis is unlikely when the WBC count is low, unless there is a high pretest probability.
Abdominal ultrasonography A properly performed systematic review by Orr and colleagues summarized 17 studies that assessed the role of ultrasonography in 3,358 adults and children suspected of having appendicitis (37% had the disease).20 The LR for acute appendicitis with a positive scan was 10.7, and the LR with a negative scan was 0.17, based on pooled sensitivity and specificity of 85% (95% CI, 81.0%-87.8%) and 92% (95% CI, 88.0%-95.2%). This suggests that patients with equivocal clinical findings will benefit from ultrasonography, but for those in whom the diagnosis is either very unlikely or very likely, the change in probability of disease after ultrasonography is not likely to change clinical management. Five studies specifically addressed the use of ultrasonography in children.21-25 You exclude two for methodologic reasons, the first because it included only patients with clinical evidence supporting operative intervention regardless of ultrasonographic findings. This populations pretest probability of having appendicitis is 95%, resulting in LRs closer to 1.0 than a test used in the population of interest, children in whom the diagnosis is uncertain.21 You exclude the second because you are concerned that the availability of a second confirmatory test (the computed tomographic [CT] scan) may have biased ultrasonographic readings and led to a misclassification bias.25
106 wjm Volume 176 March 2002
Considering the remaining three studies, you conclude that the most accurate estimate of LRs ranges from 8.5 to 30 for positive findings to 0.10 to 0.07 for negative findings.22-24 Sources of bias in these studies include the use of different types of ultrasound machines, the skill levels of the radiologists performing the examination (some including radiology residents and surgeons), and the criteria used for defining appendicitis by ultrasonography. Few studies clearly state how patients with inconclusive results or findings consistent with an alternative diagnosis were handled. Variation in the patient populations and in the follow-up routines also may have introduced bias. Given these caveats, it can be concluded that patients with strong clinical evidence of appendicitis should be referred to a surgeon without an ultrasonogram, given the large number of false-negative results when this is used as a diagnostic test. Patients with a low probability of appendicitis on clinical grounds should not undergo ultrasonography, given the large number of false-positive results obtained. The ultrasonogram is most useful in patients in whom the diagnosis is uncertain, but it still does not definitively rule the disease in or out. Douglas and colleagues conducted a randomized controlled trial of ultrasonography in diagnosing appendicitis.26 They compared clinical diagnosis with ultrasonographic diagnosis of appendicitis in patients with an intermediate probability of appendicitis based on the Alvarado score (10-point clinical scoring system). The authors concluded that ultrasonography is an accurate procedure that reduces time to operation, but there were no differences in the important outcomes of mean hospital stay or adverse outcomes, including the proportion of patients undergoing a nontherapeutic operation or delayed treatment in association with perforation. Unfortunately, you recall reading articles that reported higher diagnostic accuracy of clinical examination over the Alvarado scoring system in children. Thus, it is unclear if the failure to find improved outcomes using ultrasonography is a failure of the ultrasonogram or the selection criteria for the patient population receiving the ultrasonogram.
CT scanning Most studies that evaluate the diagnostic accuracy of CT in diagnosing appendicitis have been conducted in adult patients. Sources of bias are similar to those identified for ultrasonography, in addition to different types of contrast being used. The range of LRs found was 5.5 to infinity for positive findings and 0.1 to less than 0.001 for negative findings. The study by Pena and associates focused on children and has results consistent with those of adult studies. Scanwww.ewjm.com
..................................
Best Practice
ning with CT identified appendicitis in 28 of the 29 patients with appendicitis; 74 patients without appendicitis had normal (negative) CT results.25 The authors conservatively treated patients with equivocal CT results as falsepositives (if they did not have appendicitis) and falsenegatives (if they did have appendicitis), for a total of 1 false-negative result and 5 false-positive results. Thus, you derive a positive LR of 16.2 and a negative LR of 0.03. The studys objective was to determine the diagnostic value of a protocol involving ultrasonography followed by CT scanning in the diagnosis of appendicitis; thus you cannot directly compare the accuracy of CT scanning with that of ultrasonography. Although the study authors conclude that a CT scan following ultrasonography is highly accurate in diagnosing appendicitis in children, concern remains that this additional test may involve delays in diagnosis, radiation exposure, hazards and discomfort from rectal contrast, and possibly an adverse event related to sedation.
.........................................................................................................
WBC count (LR, 7.0) increases this risk to about 65%. This is likely an overestimation because these findings are not independent; however, there is no suggestion of an alternative diagnosis. You are unwilling to send the child to the operating room without further information, so you arrange an abdominal ultrasonogram. This reveals a dilated tubular structure in the right lower quadrant, consistent with acute appendicitis. The likelihood of appendicitis is now greater than 94%. This exceeds your threshold for surgical intervention, so you do not request a CT scan. The consulting surgeon takes the child to the operating room, where a nonperforated, thickened, inflamed appendix is removed. The patient recovers without complication.
.........................................................................................................
About 1% of children evaluated in the ED for abdominal pain have appendicitis. Vomiting and abdominal tenderness represent two of the four predictors from the Reynolds and Jaffe study (LR, 3.4), modifying this patients likelihood of appendicitis to about 3.4%14; the finding of rebound tenderness (LR, 7.0) modifies the risk to about 20%. Additional information from the
This article was edited by Virginia A Moyer, Department of Pediatrics, University of Texas Health Science Center at Houston. Articles in this series are based on chapters from Moyer VA, Elliott EJ, Davis RL, et al, eds. Evidence-Based Pediatrics and Child Health. London: BMJ Books; 2000.
See this article on our web site for the complete list of references
www.ewjm.com
Volume 176 March 2002 wjm 107
Anda mungkin juga menyukai
- August 2003: East African Medical Journal 411Dokumen4 halamanAugust 2003: East African Medical Journal 411vali2013Belum ada peringkat
- RIPASA Score For Diagnosis of AADokumen6 halamanRIPASA Score For Diagnosis of AANico CabreraBelum ada peringkat
- Modified Alvorado ScoreDokumen4 halamanModified Alvorado Scorevali2013Belum ada peringkat
- 07alvorado ScoreDokumen4 halaman07alvorado Scorevali2013Belum ada peringkat
- 07alvorado ScoreDokumen4 halaman07alvorado Scorevali2013Belum ada peringkat
- Additional File: Figure S1Dokumen3 halamanAdditional File: Figure S1vali2013Belum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Hyspin AWH-M 32Dokumen4 halamanHyspin AWH-M 32bboy640Belum ada peringkat
- CROSSBITE According To GraberDokumen29 halamanCROSSBITE According To GraberAslamCv100% (1)
- E Stim PDFDokumen6 halamanE Stim PDFAlvaro Toledo100% (1)
- Is An Ancient Disease That Causes Permanent Physical Disability AmongDokumen6 halamanIs An Ancient Disease That Causes Permanent Physical Disability Amongkian5Belum ada peringkat
- NefIgArd TrialDokumen12 halamanNefIgArd Trialfarah mujtabaBelum ada peringkat
- Migraine and Cluster HeadacheDokumen24 halamanMigraine and Cluster HeadachekhemamettaBelum ada peringkat
- Biosecurity in Poultry Farms: Top PriorityDokumen3 halamanBiosecurity in Poultry Farms: Top PriorityPhénix Atakoun'sBelum ada peringkat
- Mycoplasma Genitalium A4Dokumen1 halamanMycoplasma Genitalium A4Nauli NasirBelum ada peringkat
- Nada Lincomycyn and Espectynomycin Solubleucm061812Dokumen4 halamanNada Lincomycyn and Espectynomycin Solubleucm061812laurz95Belum ada peringkat
- TramadolDokumen19 halamanTramadolanandhra2010Belum ada peringkat
- Critiquing 1Dokumen3 halamanCritiquing 1Nilesh VeerBelum ada peringkat
- 1000 Days Ni Baby PDFDokumen31 halaman1000 Days Ni Baby PDFppantollanaBelum ada peringkat
- Non-Modifiable Risk Factors: Modifiable Risk FactorsDokumen9 halamanNon-Modifiable Risk Factors: Modifiable Risk FactorsKimberly Bomediano100% (1)
- Nucleus DropDokumen1 halamanNucleus DropYovinus DenyBelum ada peringkat
- Rehab-U FreeMobilityEbook PDFDokumen10 halamanRehab-U FreeMobilityEbook PDFTuteraipuni POTHIERBelum ada peringkat
- DR Ambreen Sultana: Professional SummaryDokumen2 halamanDR Ambreen Sultana: Professional SummaryActs N FactsBelum ada peringkat
- Memory Reconsolidation: Updating Memories Through RetrievalDokumen23 halamanMemory Reconsolidation: Updating Memories Through RetrievalRoberto LiaskowskyBelum ada peringkat
- Final Past Papers With Common MCQS: MedicineDokumen17 halamanFinal Past Papers With Common MCQS: MedicineKasun PereraBelum ada peringkat
- Dr. Lazuardhi Dwipa-Simpo Lansia 97Dokumen56 halamanDr. Lazuardhi Dwipa-Simpo Lansia 97radenayulistyaBelum ada peringkat
- FASJ - 2017 - Valisena - TX of Mortons Neuroma - Systematic ReviewDokumen11 halamanFASJ - 2017 - Valisena - TX of Mortons Neuroma - Systematic ReviewJacob DoughertyBelum ada peringkat
- Shiatsu Helps Treat AsthmaDokumen9 halamanShiatsu Helps Treat Asthmaडा. सत्यदेव त्यागी आर्यBelum ada peringkat
- Fast Food Industry ResearchDokumen13 halamanFast Food Industry ResearchNaa Okaikor OkineBelum ada peringkat
- Myopia ManualDokumen337 halamanMyopia ManualRealPurgatory100% (1)
- Asia Pacific October 2022Dokumen24 halamanAsia Pacific October 2022Dhananjay VasuDevaBelum ada peringkat
- Presented By: Bhawna Joshi Msc. Nursing 1 YearDokumen52 halamanPresented By: Bhawna Joshi Msc. Nursing 1 YearBhawna JoshiBelum ada peringkat
- Biperiden (Drug Study)Dokumen3 halamanBiperiden (Drug Study)Mae Ann Bueno CastillonBelum ada peringkat
- DRUG TramadolDokumen2 halamanDRUG TramadolAngelo Cane VillarinoBelum ada peringkat
- EGA Factsheet 01Dokumen1 halamanEGA Factsheet 01Rajeeb Chandra ShahaBelum ada peringkat
- Asthma in PregnancyDokumen40 halamanAsthma in PregnancyKabo75% (4)
- Tel No.: 0141-2721966, Fax No.: 0141-2721919, Email: Mail@ruidp - Gov.in, Web Site: WWW - Ruidp.gov - inDokumen4 halamanTel No.: 0141-2721966, Fax No.: 0141-2721919, Email: Mail@ruidp - Gov.in, Web Site: WWW - Ruidp.gov - inPrasenjit DeyBelum ada peringkat