Cycloplegic Refraction in Optometric Practice 1337594763401 2
Diunggah oleh
Strauss de LangeDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Cycloplegic Refraction in Optometric Practice 1337594763401 2
Diunggah oleh
Strauss de LangeHak Cipta:
Format Tersedia
Optometry in Practice Vol 6 (2005) 107120
Cycloplegic Refraction in Optometric Practice
Frank Eperjesi PhD and Karen Jones BSc
Division of Optometry, School of Life and Health Sciences, Aston University, Birmingham Date of acceptance 29 July 2005
Introduction
Although new methods of refraction have been developed over the years, cycloplegic refraction has remained a timetested, reliable and valid procedure for obtaining refraction data. In non-communicative or uncooperative patients, those with functional visual problems or whose visual acuity (VA) cannot be corrected to an expected level, cycloplegia is often essential for an accurate assessment of refractive error. Also, cycloplegia is often necessary in patients with inconsistent responses or symptoms, and in patients with media opacities or aberrations (Amos 2001). Without cycloplegia, determining the refractive status of young patients with accommodative esotropia, pseudomyopia or latent hyperopia would be much more difficult. An ideal cycloplegic would have no ocular or systemic side effects; it would be able to produce a rapid onset of cycloplegia, inhibit accommodation completely for an adequate period of time and then swiftly restore effective accommodation. It would also have the capacity for safe administration in general practice by appropriately qualified personnel. There is no single cycloplegic drug that covers all these requirements (Amos 2001), but some agents do satisfactorily achieve the desired clinical result with minimum disadvantages. Here we review drug mechanisms, instillation techniques and the uses and adverse reactions of common drugs that can be used in cycloplegic refraction.
were used for a broad search. In the second stage all abstracts were examined to identify articles pertinent to our review. Copies of the entire articles were obtained. Bibliographies of the articles retrieved were manually searched using the same search guidelines. Key textbooks were also searched. In the third stage, articles were reviewed and information relating to the use of cycloplegic drugs in optometric practice was incorporated into the manuscript.
Drug Mechanism
Cycloplegic drugs block the actions of the parasympathetic nervous system. Pharmacologically they are known as antimuscarinics, anticholinergics, cholinergic antagonists, muscarinic antagonists, parasympathetic antagonists or parasympatholytics. The muscarinic receptors are normally stimulated by the release of acetylcholine from the nerve endings of the parasympathetic system. When stimulated, the ciliary muscle contracts, pulling the ciliary body forward. This relieves the tension in the suspensory ligaments, which support the lens. Consequently, the lens becomes more convex, which results in an increase in refractive power to produce accommodation. During cycloplegia, when the receptors of the ciliary muscle are blocked they are no longer receptive to acetylcholine and accommodation is not possible (Bloom 1998, Titcomb 2003, Viner 2004). The end result is that the contraction of the ciliary muscle is blocked and the iris sphincter muscle is relaxed, resulting in cycloplegia and mydriasis.
Method of Literature Search
Pertinent articles on cycloplegic drugs published in peerreviewed journals were identified through a multistaged, systematic approach. In the first stage, a computerised search of the PubMed database (National Library of Medicine) was performed to identify all articles about cycloplegic drugs published up to March 2005. The terms cycloplegics, cycloplegia, paediatric and pediatric, cyclopentolate, atropine, homatropine and tropicamide
Instillation Techniques Pre-instillation assessment
Before any cycloplegic agent is administered, a satisfactory pre-instillation ocular evaluation should be performed. This practice not only protects the practitioner legally but also gives valuable information on potential contraindications to the intended cycloplegic as well as obtaining baseline clinical information that may not be
Address for correspondence: Dr F Eperjesi, Division of Optometry, School of Life and Health Sciences, Aston University, Aston Triangle, Birmingham, UK
2005 The College of Optometrists
107
F Eperjesi & K Jones
obtainable under cycloplegia. The following information could be taken before drug instillation: a full and detailed history, including visual, general medical, allergy, drug and family history distance and near VA pupillary reflexes refraction slit-lamp examination, paying particular attention to anterior angle configuration tonometry, where the patient might be at risk of closure of the anterior chamber angle Obtaining patient or parental consent before administering any cycloplegic drug is recommended (Bartlett 1978); this could be in the form of a verbal consent followed by an appropriate entry in the patient records or a more formal signed consent form. The College of Optometrists provides information sheets on the instillation of cycloplegic drugs (www.college-optometrists.org/professional/ cyclopentolate.htm and www.college-optometrists.org/ professional/tropicamide.htm) and these could easily be adapted into a consent form.
lasts for 1025 minutes (Havener 1983). Therefore, proxymetacaine 0.5% is becoming the anaesthetic of choice (Leat et al. 1999, Shah et al. 1997, Sutherland & Young 2001), despite the fact that it is also acidified with hydrochloric acid to a similar pH as cyclopentolate and can cause discomfort. The reasons for instilling a topical local anaesthetic before the cycloplegic are twofold. Firstly, if the cornea is anaesthetised, the stinging, irritation and lacrimation due to the second drop, the cycloplegic, will be diminished (Shah et al. 1997); this is particularly useful if more than one drop of cyclopentolate is required. In a group of 29 adult subjects there was a highly statistically significant reduction in total discomfort with cyclopentolate instilled after premedication with proxymetacaine compared with the use of cyclopentolate instilled after a placebo (Sutherland & Young 2001). Secondly, the local anaesthetic may increase the absorption of the cycloplegic agent (Viner 2004). The disadvantage of this technique in a paediatric population is that if the child is adverse to the first set of drops, he or she may make it extremely difficult for the second, more important drugs to be instilled (Bartlett 1978, Leat et al. 1999, Viner 2004). Proxymetacaine 0.5% should be used with caution as it may cause epithelial and stromal keratitis if used repeatedly over a period of a few hours (Doughty & Field 2005).
Drop instillation
The procedure for instilling topical medication into the eye consists essentially of inclining the head backwards so that the optical axis is as nearly vertical as possible. The lower lid is then retracted, and the upper lid held back with the thumb or forefinger. Patients should then be asked to look over their head in order to move the cornea away from the instillation site to minimise the blink reflex. The drop should then be instilled into the lower conjunctival sac, keeping the bottle tip away from the globe to avoid contact contamination. The lids can then be gently closed and the head brought forward. Children can become very distressed during this procedure; the level of distress can sometimes be minimised by careful explanation of the instillation process.
Spray instillation
Ismail et al. (1994) found that spraying cyclopentolate on to the eyelashes of a gently closed upper lid resulted in an easier application with no compromise to the cycloplegic effects. Goodman et al. (1999) also tested a spray instillation technique and found that patient discomfort associated with the spray was slightly greater that that of eye drops but this was not clinically significant. Paradoxically, the spray was better received by the parents.
Use of anaesthetics
The most commonly used cycloplegic is cyclopentolate 1% (see below). Because it is unstable at neutral pH, preparations are acidified with dilute hydrochloric acid to around pH 4 and this leads to stinging on instillation (Sutherland & Young 2001). It has been suggested that instilling a local anaesthetic before a cycloplegic agent can lead to more successful and less stressful drug instillation (Leat et al. 1999). The topical local anaesthetic proxymetacaine 0.5% stings considerably less than other anaesthetics, takes less than 30 seconds to anaesthetise the eye (Boozan & Cohen 1953) and the anaesthetic effect
Dosage
The dosage for all cycloplegics should be the minimal concentration that will achieve the clinical task satisfactorily. To overmedicate when maximum cycloplegia has been reached increases the probability of systemic absorption and therefore intensifies the side effects. In other words, using several drops of a cycloplegic when one drop is sufficient is poor practice (Amos 1978). As with all ocular drugs, the chances of systemic side effects can be reduced by occluding the eyelid puncta for a few seconds after drug instillation (Chang 1978, Viner 2004), although this is not always possible with children.
108
Cycloplegic Refraction in Optometric Practice
Degree of cycloplegia
After the cycloplegic has been instilled and the time limit for maximum cycloplegia has been reached (see below), the optometrist must then decide whether the degree of cycloplegia is adequate to permit a reliable refraction. Mydriasis is not necessarily a good indicator of when full cycloplegia has taken place; therefore it is best to check for cycloplegia by looking at the reflex with a retinoscope. If cycloplegia is complete, a non-fluctuating retinoscopy reflex is observed. If accommodation is active, then fluctuation of the retinoscopy reflex will be seen. If fluctuation is present, there are two options: use another drop of cyclopentolate, or wait for a few more minutes and check the retinoscopy reflex again (Moore 1997). Another way of assessing monocular residual accommodation would be to obtain a subjective response on the clarity of a near-text target, although in many children performing this type of check test is impossible.
atropine allergy. Instilling three drops of 1% cyclopentolate 10 minutes apart produces retinoscopy values comparable to those obtained when children are atropinised for 3 days; using more than three drops in one session increases the chances of side effects (Moore 1997). Cyclopentolate does not produce complete cycloplegia, but leaves a residual amount of accommodation of about 1.50D or less (Leat et al. 1999). However, this depth of cycloplegia is adequate for most cases and also means that a tonus allowance does not normally need to be considered when calculating the final prescription (Viner 2004). It has been reported that if residual accommodation exceeds 2.00D, cycloplegic refraction may be unreliable and inaccurate (Amos 2001). One randomised masked study reported that 1% cyclopentolate produced adequate cycloplegia in a group of 313-year-olds (Goodman et al. 1999).
Atropine
Atropine sulphate is a solanaceous alkaloid derived from Atropa belladonna. Atropine has been known since biblical times. It is an organic ester of tropic acid and tropine and is the most potent of the antimuscarinic drugs (Titcomb 2003). It is classified as a POM, while changes to the range of medicines that can be sold, supplied or administered by optometrists have classified atropine in exemption level 2. This means that atropine is only accessible to optometrists who have undergone appropriate additional training and are accredited by the General Optical Council. Atropine is rarely used in optometric practice. It has a slow action and a duration of 12 weeks. Atropines length of action completely rules out its use in infants under the age of 3 months because of the risk of stimulus deprivation amblyopia and it is associated with a significant number of possible side effects in children (Viner 2004). Its use now seems to be mainly confined to the Hospital Eye Service and a few specialised optometry practices. It is available in the form of 0.5% or 1% drops or ointment. The ointment form provides longer drug contact time with less systemic absorption than drops but, like most ocular ointments, often causes smeary vision and has the added disadvantage of being more likely to cause contact dermatitis and inhibition of corneal epithelial mitosis (Rengstorff & Doughty 1982). It should be stored between 8C and 25C. To reduce the likelihood of systemic effects, patients younger than 12 months should receive the 0.5% formulation (Mehta 1999). Atropine 0.5% is recommended in lightly pigmented irises while atropine 1% is indicated in the refraction of children with darkly pigmented irises, those with a constant strabismus with a suspected accommodative element or when cyclopentolate has proved to be ineffective (Ansons & Davis 2001, Moore
Types of Cycloplegic Drugs Cyclopentolate
Cyclopentolate is a synthetically derived antimuscarinic and is formulated as a hydrochloride salt solution. It is classified as a prescription-only medicine (POM) that can be used and supplied by an optometrist provided it is in the course of professional practice and in an emergency (exemption level 1). Cyclopentolate should be instilled 3040 minutes before refraction (Moore 1997) and a further drop can follow after 515 minutes if necessary, particularly in patients with heavily pigmented irises. It rapidly produces cycloplegia of short duration with maximum cycloplegia after 1560 minutes (longer onset in dark pigmented irises) and the effects last between 8 and 24 hours (Ansons & Davis 2001, Chang 1978, Moore 1997, Titcomb 2003). This drug seems to be the eye care professionals drug of choice for cycloplegic refraction (Ansons & Davis 2001, Shah et al. 1997), probably because of its rapid action and minimal side effects. It is considered to be highly effective in most cases provided retinoscopy is timed to coincide with its maximum action. Cyclopentolate is available in 0.5% and 1% strengths in Minim form and in 2% strength in a dropper bottle form, although this dosage is not routinely used as it is very likely to result in side effects. To reduce the chances of systemic effects, patients under 1 year old should receive the 0.5% formulation (Mehta 1999, Scheiman et al. 1997). All forms should be kept between 2C and 8C. Cyclopentolate is structurally different to atropine (see below) and can therefore be used when a patient has an
109
F Eperjesi & K Jones
1997). Interestingly, Rosenbaum et al. (1981) found that atropine revealed a mean difference of only 0.34D more hypermetropia than cyclopentolate in a sample of esotropic Caucasian children. When using atropine for refraction in children under 30 months, it is recommended that one drop of 0.5% atropine is instilled three times a day for 3 days before refraction and once more on the morning of the refraction. For refractions in children between 30 months and 5 years, one drop of 1.0% atropine is instilled three times a day for 3 days and then once on the morning of the refraction (Ansons & Davis 2001). When using the ointment, however, it is not usually instilled on the day of the examination because it takes about 2 hours for the ointment to dissipate and even a thin layer of unabsorbed ointment may interfere with the refractive procedures (Ansons & Davis 2001). The instillation (three times a day for 3 days) is done at home and is probably excessive, as maximum cycloplegia is achieved by the second day. This does however allow for missed instillations and also ensures effective relaxation of accommodation in even the most resistant eyes (Amos 1978, Bartlett 1978, Chang 1978). The use of atropine also generally requires a tonus allowance of about 1.00DS to be made to the final prescription, because atropine completely abolishes all accommodative tonus, and when the cycloplegic effects wear off, if no allowance is made, the resultant prescription will be over-plussed.
Tropicamide
Tropicamide is a synthetic derivative of tropic acid. It is a level 1 POM available in Minim form in 0.5% and 1% dosages. Tropicamide has a faster onset, 1530 minutes, and shorter duration of action, 46 hours, compared with other antimuscarinic agents. This is due to its greater diffusibility and a higher proportion of unionised drug that is available for corneal penetration. The 0.5% dosage produces mydriasis only, with ineffective cycloplegia. With the 1% dosage maximum cycloplegia is produced 25 minutes after instillation and lasts only about 1520 minutes, after which the cycloplegia is unreliable. Although it takes up to 6 hours for cycloplegia to wear off totally, most patients will be able to read 24 hours after instillation (Bloom 1998, Chang 1978, Titcomb 2003). Tropicamide has been described as unsuitable for cycloplegic refraction in children (Leat et al. 1999) and as clinically useless in all but those patients with very light irises and in cases of hypersensitivity to cholinergic agents, eg patients with Downs syndrome (Moore 1997). Interestingly, however, one study (Twelker et al. 2001) reported less than 1.00D difference between cycloplegic retinoscopy results obtained with two drops of cyclopentolate 1% and two drops of tropicamide 1% on a group of infants with an average age of 5.7 months. If used for cycloplegic refraction and if retinoscopy is delayed beyond 35 minutes after instillation, a further drop is advised (Bloom 1998).
Homatropine
Homatropine hydrobromide is a semisynthetic alkaloid formed by combining mandelic acid with tropine. It is a POM and has also been classified as an exemption level 2 drug. It is not as potent as atropine and does not last as long, although it does last slightly longer than cyclopentolate. It should also be stored between 8C and 25C. For homatropine to produce satisfactory cycloplegia, one drop of 2% homatropine is required every 10 minutes up to a total of three drops or one drop of 1% homatropine every 10 minutes for an hour (Chang 1978). Maximum cycloplegia occurs in 3060 minutes and may last 12 days (Chang 1978, Titcomb 2003). Because it needs to be administered several times before adequate cycloplegia is achieved, homatropine is not considered to be suitable for cycloplegic refraction in young children and only becomes an option in patients who are in their late teens or older. It has been replaced by cyclopentolate in clinical use (Titcomb 2003).
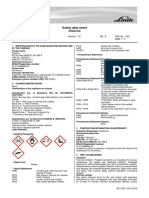
Other drugs
Two other cycloplegic agents, scopolamine (also known as hyoscine) and oxyphenonium bromide, are not commonly used in optometric practice so will not be discussed further here. Table 1 summarises the main cycloplegic properties of the common cycloplegic drugs.
Determination of refractive error
The main reason for using cycloplegic drugs in optometric practice is to obtain an accurate assessment of refractive error. Without cycloplegic drugs active accommodation may affect retinoscopy results. Furthermore, cycloplegic refraction has been described as an essential part of the paediatric ophthalmic assessment (Shah et al. 1997) and the cornerstone of strabismus evaluation (Mehta 1999). As well as aiding refraction, instilling the cycloplegic drug also allows a better view of the fundus during ophthalmoscopy; this is important since retinal lesions may produce visual loss and strabismus.
110
Cycloplegic Refraction in Optometric Practice
Table 1. Summary of the main antimuscarinic agents and their strengths, duration and indications (Titcomb 2003) Drug Forms and strengths available Multidose eye drops 0.5%, 1% Single-dose eye drops 0.5%, 1% Multidose eye drops 1%, 2% Single-dose eye drops 2% Multidose eye drops 0.5%, 1% Single-dose eye drops 0.5%, 1% Time to maximum effect 1560 minutes Duration of action Indications
Cyclopentolate
24 hours
Anterior uveitis Cycloplegic refraction Fundus photography Ophthalmoscopy Anterior uveitis
Homatropine
3060 minutes
12 days
Tropicamide
25 minutes
6 hours
Fundus photography Ophthalmoscopy
Some eye care professionals advocate cycloplegic refraction of all children on their first visit to an optometrist. However, it is probably more appropriate to select certain groups of patients for whom a cycloplegic refraction is essential: those who are poorly cooperative with near or distance retinoscopy patients with fluctuating non-cycloplegic retinoscopy reflex unexplained reduced VA in children individuals with manifest strabismus, particularly an esotropia those with significant or unstable esophoria children with a family history of strabismus, amblyopia or high hyperopia patients with suspected pseudomyopia children with a history of strabismus observed by a parent or guardian children with anisometropia greater than 1.00DS cases of reduced accommodation in high hyperopia in a child of < 2 years those with suspected latent hyperopia in variable and inconsistent subjective responses patients with suspected non-organic visual loss in symptoms unrelated to the nature or degree of the manifest refractive error (Evans 2002, Jones & Hodes 1991, Leat et al. 1999, Moore 1997, Viner 2004) Poor cooperation may have several causes, such as mental or physical constraints or through an obstreperous disposition where the child is noisily aggressive and stubborn (Viner 2004).
Advantages and disadvantages
In general, the advantages of cycloplegic refraction are: accurate patient fixation is less crucial accurate retinoscopy can be achieved more easily latent hyperopia is revealed refractive error can be confirmed (Viner 2004) there is a better view of the fundus during ophthalmoscopy
In general, the disadvantages of cycloplegic refraction are: distress to the patient on instillation of drops subsequent breakdown in childclinician relationship photophobia caused by dilated pupils decreased ability in close-work tasks a risk of ocular and systemic side effects and adverse reactions (Tables 2 and 3) difficulty in assessing axes in the presence of aberrations resulting from a large pupil diameter (Leat et al. 1999, Viner 2004) Furthermore, with atropine, the extended period of induced blur can act as an effective dissociating device and may cause patients with an esophoria or intermittent esotropia accompanied by uncorrected hypermetropia to lose control of their already fragile binocularity and lapse into a state of constant esotropia (Mallett 1994, Viner 2004). This will not occur with cyclopentolate (Mallett 1994).
111
F Eperjesi & K Jones
Table 2. Ocular and systemic adverse reactions associated with cyclopentolate (Manny & Jaanus 2001) Ocular Irritation Lacrimation Conjunctival hyperaemia Allergic blepharoconjunctivitis Elevated intraocular pressure Systemic Drowsiness Ataxia Disorientation Incoherent speech Restlessness Visual hallucination
Wide dilation of the pupil can also create excessive spherical aberration in the ocular media, resulting in difficult retinoscopy and refraction. The best guideline for retinoscopy is to neutralise the central 4mm of the pupil, ignoring the periphery. Also, a retinoscope light of low to medium intensity helps to reduce any aberrations. In addition, an allowance for ciliary tonus is sometimes necessary, and the practitioner must consider this allowance to determine the appropriate refractive correction for each patient (Amos 2001, Viner 2004).
Strabismus
When a young patient has an esotropia, cycloplegics can be used to determine whether the esotropia is fully accommodative or not. When a cycloplegic is instilled into the eyes, the eyes often converge more because accommodation is incompletely relaxed, and if the patient tries to overcome this, the cycloplegic convergence becomes overstimulated. If cycloplegia is complete and the eyes straighten, this indicates that it is a fully accommodative esotropia and glasses will hold the eyes straight. In accommodative esotropia, it is essential to determine the full amount of hyperopia as it is vital to prescribe the correct plus-power lenses to relieve the effort placed on the accommodative convergence system (Amos 2001, Morgan & Arstikaitis 1967). In the presence of a constant or intermittent strabismus, it is often necessary to occlude one eye. The non-occluded eye maintains fixation and retinoscopy can be performed on axis with less chance of error (Moore 1997).
Table 3. Systemic adverse reactions associated with atropine in children (Manny & Jaanus 2001) Diffuse cutaneous flush Depressed salivation / thirst Fever Urinary retention Tachycardia Somnolence Excitement / restlessness and hallucinations Speech disturbances Ataxia Convulsions
Residual accommodation
Gettes & Belmont (1961) determined residual accommodation to measure the efficiency of cycloplegic drugs. They investigated atropine 1%, cyclopentolate 1%, tropicamide 1% and homatropine 4% with 1% paredrine. Efficiencies of 100% for atropine, 92% for cyclopentolate, 80% for tropicamide and 54% for homatropine with paredrine were noted. Table 4 shows the residual accommodation after drug instillation.
Table 4. The residual accommodation, in dioptres, after instillation of two drops of 1% tropicamide in one eye and 1% cyclopentolate or 5% homatropine in the fellow eye (Gettes & Belmont 1961) Age Tropicamide Cyclopentolate Homatropine (years) at 30 minutes at 60 minutes at 60 minutes 09 1014 6.25 (n = 6) 3.65 (n = 20) (0) 1.6 (n = 5) 2.5 (n = 6) 2.6 (n = 15)
Near-fixation retinoscopy (Mohindra technique)
There are some potential adverse reactions, side effects and legal issues on the use of cycloplegic drugs (see below). Alternatives to using drugs have been suggested. One such method is near-fixation retinoscopy (often referred to as the Mohindra technique: Mohindra 1977a, b). This technique relies on the fact that young children are likely to be attracted to a retinoscope light in a darkened room.
112
Cycloplegic Refraction in Optometric Practice
To keep infants attentive it has been suggested that feeding them can help; feeding also helps to relax the accommodation and widens the palpebral aperture (Mohindra 1975). Retinoscopy is carried out at 50cm on one eye while the examiner or a carer occludes the other eye. It is assumed that the eye undergoing retinoscopy is at its resting accommodation level when the retinoscopy light is maintained at a minimum. In an adult population the accommodative response under these conditions has been shown to remain stable at 0.70D (Owens et al. 1980). The American Optometric Association recommends near noncycloplegic retinoscopy when frequent follow-up is necessary, when the child is extremely anxious about instillation of cycloplegic agents and when the child has had or is at risk of an adverse reaction to cyclopentolate or tropicamide (Scheiman et al. 1997). Retinoscopy is performed by neutralising the retinal reflex in the two primary meridians of the eye using loose trial lenses. The gross sphere cylinder form is then calculated from the meridional findings. Mohindra (1977b) has indicated that 1.25D should be added to the spherical component of the gross sphere cylinder findings. This adjustment factor was found by comparing subjective refraction and near retinoscopy results on 27 adults; it takes into account both the 2.00D working distance and 0.75D residual accommodation (Saunders & Westall 1992). Results from a study using a larger sample size and infant subjects indicated greater agreement between near and cycloplegic retinoscopy (two drops of 1% cyclopentolate) when 1.00D is subtracted from the spherical component of the gross retinoscopy result for those patients less than 2 years of age and 0.75D subtracted for those over the age of 2 years (Saunders & Westall 1992). Good reliability (Mohindra 1975) and validity (Mohindra 1977b) of the near retinoscopy technique have been reported but some concerns have also been expressed. Opinions vary as to the accuracy of this technique; if, during retinoscopy, the light does not provide a stimulus to accommodation and the eye assumes its normal resting state of accommodation, it would seem that the results from this technique would be reasonably reliable. However, it has been proposed that tonus is dependent on the type of refractive error present, with hyperopes having a greater amount. If this were true then it would result in the Mohindra technique underestimating the amount of hyperopia seen (Viner 2004). Borghi & Rouse (1985) reported that cycloplegic retinoscopy found on average 0.500.75D more hyperopia than near non-cycloplegic retinoscopy and Twelker & Mutti (2001) found an average difference of 1.04D. However, Wesson et al. (1990) found in their infant group an average of 2.12D more hyperopia using cycloplegic retinoscopy with cyclopentolate compared with the near
non-cycloplegic technique and recommended caution when substituting near non-cycloplegic retinoscopy for cycloplegic refraction. Interestingly, Chan & Edwards (1994) reported that for Chinese children (aged 3.55 years), multiplying the spherical component of the refraction result obtained by static non-cycloplegic retinoscopy (fixing at 6m) by 1.45, adding 0.39 to the product while keeping the astigmatic power unchanged, the total refractive error (ie the error that would be found using cyclopentolate 1%) can be accurately estimated.
Adverse Reactions
All cycloplegics have the potential to cause significant adverse reactions. All the antimuscarinic drugs abolish normal pupil reflexes to light and near vision and therefore result in photophobia and a decreased ability to perform near-work tasks. Photophobia can be reduced by the use of sunglasses or a brimmed hat. It is also prudent to warn the parent or carer of a school-aged child that near-work tasks will prove more difficult until the effects of the drug have worn off. Also, cycloplegia is contraindicated in all patients with a history of angle-closure glaucoma (Amos 2001, Bloom 1998, Viner 2004). From the clinical perspective, reactions associated with topically applied cycloplegic agents may be classified as allergic or toxic. A variety of predisposing factors for adverse allergic or toxic reactions exist, and these include use of high concentrations, overdosage and ocular and systemic conditions allowing increased systemic drug absorption. Adherence to certain general principles will reduce the risk of adverse reactions to cycloplegic agents (Bartlett 1978): All medications should be kept out of the reach of children: as few as 20 drops of 1% atropine can be fatal if taken internally The ointment form of atropine will decrease the risk of systemic absorption Excessive solution or ointment should be wiped from the eye after instillation The lowest concentration and least dosage frequency consistent with the diagnostic purpose of the drug should be used; most adverse reactions from cyclopentolate have followed the administration of a higher than recommended dose A conservative approach should be taken in drug instillation in patients with injected conjunctiva as hyperaemia increases the rate of systemic absorption
113
F Eperjesi & K Jones
Before the drug is administered, consideration should be given to its potential adverse effects relative to its potential diagnostic benefit to the patient Patients, or their parents, given atropine ointment for home use should be cautioned to use only as directed; in contrast to what some patients or parents may expect, no additional benefit results from receiving more than the prescribed amount of drug Any known sensitivity to a specific cycloplegic agent can often be bypassed by substituting another cycloplegic
Iris colour
The efficacy of these drugs is influenced by the amount of iris pigmentation, which is reflected in the colour of the iris. Until recently the classification of iris colour was imprecise, and iris pigmentation has been defined in broad categories such as light or dark, or blue or brown. Subjective comparisons to standard photographs or to painted glass eyes have resulted in greater standardisation and a better understanding of the effect of iris pigmentation. With new computer technologies, objective determinations of iris pigmentation promise improved accuracy in predicting the response and perhaps the dosage of cycloplegic drugs in individual patients (Manny & Jaanus 2001).
and therefore extra care should be taken to prevent an overdose. Cyclopentolate is available in a 2% solution, although this is not recommended for normal usage since it may produce psychotic reactions in some individuals. Central nervous system (CNS) effects are usually reported after a higher than recommended dose. Compared with atropine, cyclopentolate causes more CNS effects, such as confusion, difficulty in speaking, disorientation, aimless wandering, schizophrenia-like behaviour, restlessness, apprehension, amnesia and hallucinations (Beswick 1962, Binkhorst et al. 1963, Kennerdell & Wucher 1972, Mark 1963). Fortunately, none of these lasts for more than a few hours or leaves permanent problems (Jones & Hodes 1991). Allergic responses to cyclopentolate are rare and may go unrecognised. Jones & Hodes (1991) described two paediatric cases of hypersensitivity involving the development of a facial and upper-body rash that spread to the arms and legs 46 hours after instillation of two drops of cyclopentolate 1%. Signs and symptoms had resolved by the next day. Table 2 summarises the potential ocular and systemic adverse reactions associated with cyclopentolate.
Atropine
Atropine and homatropine have the potential to cause more significant systemic side effects than the other antimuscarinics. Large amounts of atropine absorbed systemically are toxic or even lethal. The fatal dose of atropine is about 10mg for children (Mauger & Craig 1996). Adverse reactions due to the topical use of atropine include dry mouth, dryness and flushing of the skin, thirst, restlessness, irritability and disorientation. A more substantial side effect of atropine may manifest itself as an allergic contact dermatitis of the lids, producing erythema, pruritus and oedema. Allergic papillary conjunctivitis and keratitis have also been reported (Manny & Jaanus 2001). Atropine can also produce an increase in intraocular pressure, respiratory depression, tachycardia (an abnormally rapid heart rate: over 100 beats per minute), closed-angle glaucoma, altered mental state and cardiovascular effects. These adverse reactions to atropine are typically described as rendering the patient: as blind as a bat, because of the cycloplegia as dry as a bone, through inhibition of sweat and salivary glands as red as a beetroot, through increased vasodilation of the blood vessels of the skin as the body tries to reduce its temperature by an alternative means as mad as a hatter, as the CNS effects, including hallucinations, ataxia (inability to coordinate voluntary muscle movements, unsteadiness, staggering) and
Cyclopentolate
Adverse reactions from this drug include stinging on instillation, reduced VA and glare. Adult patients should be advised not to drive or operate machinery until the effects of cycloplegia and mydriasis have worn off. The only time that a miotic drug should be used to reverse the effects of mydriasis would be if the patient suffered an acute attack of closed-angle glaucoma following instillation of the cycloplegic agent. A miotic drug could then be instilled to reduce intraocular pressure. None of the antimuscarinic drugs should be used on any patient with a narrow anterior-chamber angle because of the increased risk of angle closure (Bloom 1998). In the general population the risk of precipitating such an attack has been reported as 1 in 183 000 (Keller 1975). Adverse reactions related to the use of cyclopentolate and tropicamide are less common and less severe than those associated with other cycloplegic drugs such as atropine and homatropine, although there have been significant isolated reports of cases of altered mental state, raised intraocular pressure and closed-angle glaucoma with cyclopentolate. Furthermore, heavily pigmented eyes (dark irises) do not dilate readily (Priestly & Medine 1951)
114
Cycloplegic Refraction in Optometric Practice
psychotic reactions manifest themselves; these symptoms indicate an advanced stage of poisoning. In severe intoxication states, the CNS stimulation and psychotic phenomena may be followed by depression, circulatory collapse, coma and death (Bartlett 1978) Cramp (1976) reported that atropine used therapeutically might cause a local sensitivity reaction, which is occasionally violent enough to cause an intensely injected eye with chemosis along with eczema involving almost all the face. Atropine should be used with great caution in patients with Downs syndrome and in patients receiving systemic anticholinergic drugs because of potential adverse CNS side effects (Manny & Jaanus 2001). Table 3 summarises potential systemic adverse reactions to atropine in children.
be the safest agent (as indexed by changes in blood pressure and heart rate) for dilated retinal examinations in neonates (Manny & Jaanus 2001). Gray (1979) has made several recommendations on reducing the risk of ocular and systemic side effects associated with use of cycloplegic drugs: Avoid overdosage consensus suggests that best practice is two drops from a Minim separated by 5 minutes, although it is not always possible in clinical practice to instil two drops into each eye because of the resistance of the child following the first drop. This will reduce the amount overflowing on to the cheek and being systemically absorbed in the nasolacrimal duct Occlude the puncta for 30 seconds following instillation (Hill et al. 1974) Choose the least toxic drug available that will give the desired cycloplegia. For example, cyclopentolate 1% is less likely to cause side effects than atropine, while tropicamide is less likely to cause side effects than cyclopentolate (Wahl 1969), but its cycloplegic properties are questionable Be able to recognise adverse systemic reactions Be aware of predisposing factors for adverse systemic reactions, such as fair children (Walsh & Hoyt 1969) and patients with Downs syndrome (Harris & Goodman 1968) Avoid high room temperatures and humidity (Hoefnagel 1961)
Homatropine
The side effects and adverse reactions from homatropine are very similar to those of atropine, although they are not usually as severe. Homatropine is approximately one-tenth as potent as atropine. Hoefnagel (1961) reported four cases of ataxia, hallucinations and speech difficulty in children aged 91/212 years following one drop of 2% homatropine repeated five to six times at 10-minute intervals. One of these patients required hospitalisation to manage his combative behaviour and tachycardia, which persisted for 3 days, and hallucinations that persisted for 5 days. Other reported toxic effects include constant muttering, shouting and singing, and periods of relative quiet, insomnia, restlessness, confusion and nausea. Allergic reactions to homatropine can be seen in the form of lid oedema and conjunctivitis (Bartlett 1978).
Use of Miotics
To reduce the time taken for the effects of a cycloplegic to wear off naturally, some clinicians advise the use of a miotic, such as pilocarpine, after the cycloplegic examination. However, miotic administration can cause ciliary spasm, brow ache and an increased risk of angleclosure glaucoma by the pupillary block mechanism. Furthermore, the effects of 2% pilocarpine have been assessed in countering cycloplegia. It was found that there was no significant effect in the decrease of pupil size or the rate of return of accommodation. In some subjects, distance VA worsened. Dispensing disposable mydriatic sunglasses to the patient and allowing the cycloplegic effect to run its natural course appears to be the best method (Amos 2001).
Tropicamide
Tropicamide does not cause many side effects, although it has the potential to produce an increase in intraocular pressure, especially for those patients with open-angle glaucoma (Portney & Purcell 1975) and also an attack of closed-angle glaucoma, although this is very rare (Keller 1975). Wahl (1969) also reported one case in which a 10year-old boy developed an anaphylactic shock reaction following instillation of 0.5% tropicamide drops. It was reported that immediately after instillation of one drop of 0.5% tropicamide in each eye, the boy fell from his chair to the floor unconscious. This was followed by generalised muscular rigidity, opisthotonos, pallor and cyanosis. He was fully recovered 1 hour later except for residual drowsiness. This appears to represent an acute hypersensitivity reaction to 0.5% tropicamide. Adverse effects to tropicamide like this one are extremely rare (Bloom 1998, Wahl 1969). Tropicamide has been shown to
Legislation
The following are guidelines that have been drawn up by the College of Optometrists regarding the general use of
115
F Eperjesi & K Jones
drugs in UK practice; these can be applied to the use of cycloplegic drugs (College of Optometrists 2005): The optometrist has a duty to take due care in the use of drugs in optometric practice Practitioners should always act in accordance with the current medicines legislation controlling the use of drugs in optometric practice Practitioners should not consider using a drug or group of drugs unless they are satisfied that they possess the knowledge and skills to do so. This is especially important when a new drug is added to the Optometrists Formulary To protect the patient an optometrist has a duty to maintain a reasonable level of knowledge of drugs and their actions through a commitment to appropriate continuing professional development Practitioners are encouraged to support adverse drug reactions reporting schemes The patients general medical practitioner (GMP) should be informed of any suspected adverse reaction When using any diagnostic drug, patients should be made aware of the effects and possible side effects of the drug. If the practitioner will not be available to deal with any emergency that may arise following instillation of the drug, he should instruct the patient to attend the local Accident and Emergency department should any adverse reaction occur More specific guidelines (College of Optometrists 2005) on the use of cycloplegia are short and to the point. Section 19.03 states: Use of a cycloplegic should be considered for the following reasons: (a) To have an accurate assessment of the refractive error (the major factor in amblyopia and/or squint; (b) To have the best possible view of the fundus within the limits of cooperation associated with the age of the child.
those with CNS anomalies and the 1% dosage on other patients. Even though adverse reactions are very rare and the effects are transient, it is important for the optometrist to be aware of these and of the types of patients who are likely to have a negative response to the instillation of cycloplegic drugs.
References
Amos DM (1978) Cycloplegics for refraction. Am J Optom Physiol Opt 55, 23225 Amos JF (2001) Clinical Ocular Pharmacology, 4th edn. Oxford: Butterworth-Heinemann, pp. 4259 Ansons AM, Davis H (2001) Diagnosis and Management of Ocular Motility Disorders, 3rd edn. Oxford: Blackwell Science, pp. 27, 28 Bartlett JD (1978) Administration of and adverse reactions to cycloplegic agents. Am J Optom Physiol Opt 55, 22732 Beswick JA (1962) Psychosis from cyclopentolate. Am J Ophthalmol 53, 87980 Binkhorst RD, Weinstein GW, Baretz RM, Clahane AC (1963) Psychotic reaction induced by cyclopentolate (Cyclogyl). Results of pilot study and a double-blind study. Am J Ophthalmol 55, 12435 Bloom J (1998) The College Formulary, pp. 1315. Available online at: w w w. c o l l e g e - o p t o m e t r i s t s . o r g / p r o f e s s i o n a l / o p t o m e t r i s t s %27%20formulary.pdf. Accessed October 2004 Boozan CW, Cohen IJ (1953) Ophthaine, a new topical anesthetic for the eye. Am J Ophthalmol 36, 161921 Borghi RA, Rouse MW (1985) Comparison of refraction obtained by near retinoscopy and retinoscopy under cycloplegia. Am J Optom Physiol Opt 62, 16972 Chan OY, Edwards M (1994) Comparison of cycloplegic and noncycloplegic retinoscopy in Chinese pre-school children. Optom Vis Sci 71, 31218 Chang FW (1978) The pharmacology of cycloplegics. Am J Optom Physiol Opt 55, 21922 College of Optometrists (2005) Colleges Guidelines for Professional Conduct June 2005. Section 40.05-08. Available online at: w w w. c o l l e g e - o p t o m e t r i s t s . o r g / p r o f e s s i o n a l / g u i d e l i n e s / june2005/guidelinesTOC.html. Accessed 29 July 2005 Cramp J (1976) Reported cases of reactions and side effects of the drugs which optometrists use. Aust J Optom 59, 1325 Doughty M, Field A (2005) Minims proxymetacaine. Available online at: www.academy.org.uk/pharmacy/nopain.htm. Accessed 25 July 2005 Evans BJW (2002) Pickwells Binocular Vision Anomalies, 4th edn. Oxford: Butterworth-Heinemann, pp. 37, 57 Gettes BC, Belmont O (1961) Tropicamide: comparative cycloplegic effects. Arch Ophthalmol 66, 33640 Goodman CR, Hunter DG, Repka MX (1999) A randomized comparison study of drop versus spray topical cycloplegic application. Binocul Vis Strabismus Q 14, 10710 Gray LG (1979) Avoiding adverse effects of cycloplegics in infants and children. J Am Optom Assoc 50, 46570 Harris WS, Goodman RM (1968) Hyper-reactivity to atropine in Downs syndrome. N Engl J Med 279, 40710 Havener WH (1983) Ocular Pharmacology, vol. 5. St Louis: Mosby Hill JC, Bethell W, Smirmaul HJ (1974) Lacrimal drainage a dynamic evaluation. Part I mechanics of tear transport. Can J Ophthalmol 9, 41116
Conclusions
Cycloplegic refraction can be of great use in optometric practice, especially for cases involving latent hyperopia, esotropia and non-organic visual loss. Non-cycloplegic near retinoscopy may be appropriate in some cases where retinoscopy using a distance target has proved ineffective, but if there is any doubt as to the accuracy of the results a cycloplegic refraction should be carried out. The most appropriate cycloplegic agent is cyclopentolate hydrochloride, preferably in Minim form; the 0.5% dosage should be used for infants younger than 12 months and
116
Cycloplegic Refraction in Optometric Practice
Hoefnagel D (1961) Toxic effects of atropine and homatropine eyedrops in children. N Engl J Med 264, 16871 Ismail EE, Rouse MW, De Land PN (1994) A comparison of drop instillation and spray application of 1% cyclopentolate hydrochloride. Optom Vis Sci 71, 23541 Jones LW, Hodes DT (1991) Possible allergic reactions to cyclopentolate hydrochloride: case reports with literature review of uses and adverse reactions. Ophthalm Physiol Opt 1, 1621 Keller JT (1975) The risk of angle closure glaucoma from the use of mydriatics. J Am Optom Soc Assoc 46, 1921 Kennerdell JS, Wucher FP (1972) Cyclopentolate associated with two cases of grand mal seizure. Arch Ophthalmol 87, 6345 Leat SJ, Shute RH, Westall CA (1999) Assessing Childrens Vision: A Handbook. Oxford: Butterworth-Heinemann, pp. 1435, 243 Mallett RF (1994) Use of atropine. Optom Today 34, 4 Manny RE, Jaanus SD (2001) Cycloplegics. In: Bartlett JD, Jaanus SD (eds) Clinical Ocular Pharmacology, 4th edn. Oxford: ButterworthHeinemann, pp. 1501, 154, 158, 161 Mark HH (1963) Psychotogenic properties of cyclopentolate. JAMA 186, 4301 Mauger TF, Craig EL (1996) Mosbys Ocular Drug Handbook. St. Louis: Mosby, p. 93 Mehta A (1999) Chief complaint, history, and physical examination. In: Rosenbaum Al, Santiago AP (eds) Clinical Strabismus Management. Philadelphia: Saunders, p. 18 Mohindra I (1975) A technique for infant vision examination. Am J Optom Physiol Opt 52, 86770 Mohindra I (1977a) A non-cycloplegic refraction technique for infants and young children. J Am Optom Assoc 48, 51823 Mohindra I (1977b) Comparison of near retinoscopy and subjective refraction in adults. Am J Optom Physiol Opt 543, 1922 Moore BD (1997) Eye Care for Infants and Young Children. Boston: Butterworth-Heinemann, pp. 50, 195 Morgan AL, Arstikatis M (1967) Strabismus. In: The Eye in Childhood. Chicago: Year Book Medical, p. 36 Owens DA, Mohindra I, Held R (1980) The effectiveness of a retinoscope beam as an accommodative stimulus. Invest Ophthalmol Vis Sci 19, 9429
Portney GL, Purcell TW (1975) The influence of tropicamide on intraocular pressure. Ann Ophthalmol 7, 314 Priestly M, Medine MM (1951) New mydriatic and cycloplegic drug (compound 75 GT). Am J Ophthalmol 34, 6389 Rengstorff RH, Doughty CB (1982) Mydriatic and cycloplegic drugs: a review of ocular and systemic complications. Am J Optom Physiol Opt 59, 16277 Rosenbaum AL, Bateman JB, Bremer DL et al. (1981) Cycloplegic refraction in esotropic children. Cyclopentolate versus atropine. Ophthalmology 88, 10314 Saunders KJ, Westall CA (1992) Comparison between near retinoscopy and cycloplegic retinoscopy in the refraction of infants and children. Optom Vis Sci 69, 61522 Scheiman MM, Amos CS, Ciner EB et al. (1997) Pediatric Eye and Vision Examination. Reference Guide for Clinicians, 2nd edn. Optometric Clinical Practice Guidelines. St Louis: American Optometric Association Shah P, Jacks AS, Adams GG (1997) Paediatric cycloplegia: a new approach. Eye 11, 8456 Sutherland MS, Young JD (2001) Does instilling proxymetacaine before cyclopentolate significantly reduce stinging? The implications of paediatric cycloplegia. Br J Ophthalmol 85, 2445 Titcomb L (2003) Use of drugs in optometric practice. Optom Today April 18, 2634 Twelker JD, Mutti DO (2001) Retinoscopy in infants using a near noncycloplegic technique, cycloplegia with tropicamide 1%, and cycloplegia with cyclopentolate 1%. Optom Vis Sci 78, 21522 Viner C (2004) Refractive examination. In: Harvey W, Gilmartin B (eds) Paediatric Optometry. Edinburgh: Butterworth-Heinemann, pp. 224 Wahl JW (1969) Systemic reaction to tropicamide. Arch Ophthalmol 82, 320 Walsh FB, Hoyt WF (1969) Clinical Neuro-ophthalmology, 3rd edn, vol. 3. Baltimore: Williams & Wilkins, p. 2662 Wesson MD, Mann KR, Bray NW (1990) A comparison of cycloplegic refraction to the near retinoscopy technique for refractive error determination. J Am Optom Assoc 61, 6804
117
F Eperjesi & K Jones
Multiple Choice Questions
This paper is reference C-2001, CET number EV-6280. Three credits are available. Please use the inserted answer sheet. Copies can be obtained from Optometry in Practice Administration, PO Box 6, Skelmersdale, Lancashire WN8 9FW. There is only one correct answer for each question.
1. (a) (b) (c) (d) 2. (a) (b) (c) (d) 3. (a) (b) (c) (d) 4. (a) (b) (c) (d) 5.
Which one of the following is not a characteristic of an ideal cycloplegic drug? rapid onset of cycloplegia partial accommodation inhibition swift accommodation restoration easy administration Cycloplegic drugs act on the: parasympathetic nervous system sympathetic nervous system iris dilator muscle Mllers muscle Which of the following is useful to know before instillation of a cycloplegic agent? K readings refractive error colour vision status cup-to-disc ratio Cyclopentolate 1% stings on instillation because: it has a pH of 6 it is mixed with anaesthetic it is diluted with hydrochloric acid it reacts with melanin granules in the iris The chances of a systemic adverse reaction following on from instillation of a cycloplegic drug are reduced if: an anaesthetic drop is instilled first the practitioner waits 5 minutes before instilling the agent into the other eye eyelid puncta are occluded the iris is well pigmented In young children the level of cycloplegia is best judged by: the amount of mydriasis accommodative amplitude clarity of near text retinoscopy reflex fluctuation In a patient with lightly pigmented irises, maximum cycloplegia following instillation of cyclopentolate 1% would occur after: 1560 minutes less than 60 minutes between 60 and 80 minutes more than 80 minutes
8.
(a) (b) (c) (d) 9.
The cycloplegic drug of choice for most primary eye care practitioners when examining healthy children over the age of 12 months is: atropine 1% cyclopentolate 0.5% tropicamide 1% cyclopentolate 1% How much residual accommodation is cyclopentolate 1% considered to leave when maximum cycloplegia has been achieved? +0.50D +1.00D +1.50D +2.00D
(a) (b) (c) (d)
10. According to one study, approximately how much more hypermetropia did atropine reveal compared to cyclopentolate? (a) 0.25D (b) 0.34D (c) 0.44D (d) 0.55D 11. With respect to tropicamide 1%, which one of the following is true? (a) Maximum cycloplegia lasts 1520 minutes. (b) Maximum cycloplegia is produced after 1 hour. (c) It can be used on all children as a replacement for cyclopentolate. (d) It frequently results in systemic adverse reactions. 12. Which one of the following is the most appropriate correction factor to apply when using the Mohindra technique on a child less than 2 years old? (a) +0.25D (b) +0.50D (c) +0.75D (d) +1.00D 13. Which one of the following is not a known adverse reaction to cyclopentolate? (a) altered mental state (b) upper-body skin rash (c) restlessness (d) brachycardia
(a) (b) (c) (d) 6. (a) (b) (c) (d) 7.
(a) (b) (c) (d)
118
Cycloplegic Refraction in Optometric Practice
14. Which one of the following approximately relates to the risk of developing acute closed-angle glaucoma following dilation? (a) 1 in 85 000 (b) 1 in 185 000 (c) 1 in 285 000 (d) 1 in 500 000 15. With regard to the use of pilocarpine as a miotic following the instillation of a cycloplegic agent, which one of the following is true? (a) Pupil size quickly returns to normal. (b) There is an increased rate of return of accommodation. (c) Distance visual acuity improves following instillation. (d) There is no significant effect on pupil size.
119
F Eperjesi & K Jones
120
Anda mungkin juga menyukai
- Visual Optics 1,2.......Dokumen468 halamanVisual Optics 1,2.......henok birukBelum ada peringkat
- Interpupillary DistanceDokumen22 halamanInterpupillary DistanceJúnior Alves100% (1)
- Module 5 - Ocular Motility - Cover TestDokumen12 halamanModule 5 - Ocular Motility - Cover TestCat Loved KirariBelum ada peringkat
- Convergence: Group 2Dokumen29 halamanConvergence: Group 2Kwenzie FortalezaBelum ada peringkat
- BSV ManualDokumen129 halamanBSV ManualNikhil Maha DevanBelum ada peringkat
- The Handbook of Ophthalmic EmergenciesDari EverandThe Handbook of Ophthalmic EmergenciesPenilaian: 5 dari 5 bintang5/5 (4)
- Corneal TopographyDokumen64 halamanCorneal TopographyDhivya SekarBelum ada peringkat
- Basic Eye ExamDokumen8 halamanBasic Eye ExamLisa AguilarBelum ada peringkat
- Clinical Orthoptics 2019Dokumen97 halamanClinical Orthoptics 2019Joseph IsraelBelum ada peringkat
- Incomitant SquintDokumen41 halamanIncomitant Squintshreeja maheshwari100% (3)
- KERATOCONUSDokumen22 halamanKERATOCONUSAarush DeoraBelum ada peringkat
- Clinical OpticsDokumen88 halamanClinical OpticsKris ArchibaldBelum ada peringkat
- Cycloplegic Refraction in Optometric Practice 1337594763401 2Dokumen14 halamanCycloplegic Refraction in Optometric Practice 1337594763401 2Strauss de LangeBelum ada peringkat
- Cycloplegic Refraction in Optometric Practice 1337594763401 2Dokumen14 halamanCycloplegic Refraction in Optometric Practice 1337594763401 2Strauss de LangeBelum ada peringkat
- Emmetropization Process and Factors ReviewDokumen18 halamanEmmetropization Process and Factors ReviewMwanja MosesBelum ada peringkat
- OPT 303 - Guide to Retinoscopy Techniques & PrinciplesDokumen54 halamanOPT 303 - Guide to Retinoscopy Techniques & PrinciplesEmmanuel AbuBelum ada peringkat
- Golden Dust™: Founded by Marijana GabrielsenDokumen3 halamanGolden Dust™: Founded by Marijana GabrielsenIdil Türe100% (1)
- Pediatric Ophthalmology Anatomy and ExaminationDokumen21 halamanPediatric Ophthalmology Anatomy and ExaminationGlydenne GayamBelum ada peringkat
- RETINOSCOPY: A KEY TO ASSESSING REFRACTIVE ERRORSDokumen33 halamanRETINOSCOPY: A KEY TO ASSESSING REFRACTIVE ERRORSSafa Abdualrahaman Ali HamadBelum ada peringkat
- Objective Refraction Technique: Retinoscopy: Aao ReadingDokumen57 halamanObjective Refraction Technique: Retinoscopy: Aao ReadingKhairunnisaBelum ada peringkat
- Binocular Vision Anomalies: Symptomatic HeterophoriaDokumen10 halamanBinocular Vision Anomalies: Symptomatic HeterophoriaGraham CoffeyBelum ada peringkat
- Optometry PresDokumen31 halamanOptometry Pressafna saleemBelum ada peringkat
- CLP Topic 5 Rigid Gas Permeable (RGP) Lens Fitting EvaluationDokumen26 halamanCLP Topic 5 Rigid Gas Permeable (RGP) Lens Fitting EvaluationRhendy 172019022Belum ada peringkat
- Everything You Need to Know About Strabismus Diagnosis and TreatmentDokumen197 halamanEverything You Need to Know About Strabismus Diagnosis and TreatmentRaluca OpreaBelum ada peringkat
- Pediatric Eye Examination: Seia MahananiDokumen35 halamanPediatric Eye Examination: Seia MahananiRaissaBelum ada peringkat
- Retinal Detachment SlideDokumen54 halamanRetinal Detachment SlideHerin NataliaBelum ada peringkat
- Night MiopiaDokumen8 halamanNight MiopiamurilobsouzaBelum ada peringkat
- Ocular Manifestations of Thyroid DiseaseDokumen20 halamanOcular Manifestations of Thyroid Diseasevivekrajbhilai5850Belum ada peringkat
- Binocular Vision Anomalies Part 1Dokumen10 halamanBinocular Vision Anomalies Part 1irijoaBelum ada peringkat
- The Actions and Uses of Ophthalmic Drugs: A Textbook for Students and PractitionersDari EverandThe Actions and Uses of Ophthalmic Drugs: A Textbook for Students and PractitionersBelum ada peringkat
- Binocular vision anomalies overviewDokumen13 halamanBinocular vision anomalies overviewblueiceBelum ada peringkat
- Measuring Lenses with a Lensometer & Lens Clock/GaugeDokumen53 halamanMeasuring Lenses with a Lensometer & Lens Clock/GaugeManmohan Shah100% (1)
- Investigative Techniques & Ocular Examination - Sandip DoshiDokumen161 halamanInvestigative Techniques & Ocular Examination - Sandip DoshiShifan Abdul MajeedBelum ada peringkat
- Trial Sets and Trial FramesDokumen16 halamanTrial Sets and Trial FramesJúnior AlvesBelum ada peringkat
- Orthoptic Exercises for OptometristsDokumen6 halamanOrthoptic Exercises for OptometristsCatalin GeorgeBelum ada peringkat
- Tinted Lens in Low VisionDokumen10 halamanTinted Lens in Low VisionAmrit PokharelBelum ada peringkat
- Lecture Three Convergence and Accommodation (AC/A) : Mr. Natnael L. (Lecturer) April/2017Dokumen33 halamanLecture Three Convergence and Accommodation (AC/A) : Mr. Natnael L. (Lecturer) April/2017henok birukBelum ada peringkat
- Paediatric Optometry Part 1 exam answersDokumen5 halamanPaediatric Optometry Part 1 exam answersSourav KarmakarBelum ada peringkat
- Keratometer Easy To Understand PDFDokumen2 halamanKeratometer Easy To Understand PDFDanielle SangalangBelum ada peringkat
- Nungki-Esodeviations & ExodeviationsDokumen36 halamanNungki-Esodeviations & ExodeviationsNia RoosdhantiaBelum ada peringkat
- 12 - Objective RefractionDokumen11 halaman12 - Objective RefractionSumon SarkarBelum ada peringkat
- Concomitant SquintDokumen21 halamanConcomitant SquintShivani NairBelum ada peringkat
- MCQ 05 OpticsDokumen14 halamanMCQ 05 OpticsAmr Abdulradi0% (1)
- Third Years Log BookDokumen11 halamanThird Years Log BookMeenakshi Kumar100% (2)
- The Spotty RetinaDokumen5 halamanThe Spotty RetinaJose Luis Mato AhcanBelum ada peringkat
- Cycloplegic Retinoscopy in InfancyDokumen5 halamanCycloplegic Retinoscopy in InfancyStrauss de LangeBelum ada peringkat
- Eye MCQDokumen1 halamanEye MCQLoveKumarBelum ada peringkat
- The Skeffington Perspective of the Behavioral Model of Optometric Data Analysis and Vision CareDari EverandThe Skeffington Perspective of the Behavioral Model of Optometric Data Analysis and Vision CareBelum ada peringkat
- Glaucoma A Symposium Presented at a Meeting of the Chicago Ophthalmological Society, November 17, 1913Dari EverandGlaucoma A Symposium Presented at a Meeting of the Chicago Ophthalmological Society, November 17, 1913Belum ada peringkat
- Development of Binocular Vision: University of Gondar Department of Optometry by Nebiyat FelekeDokumen35 halamanDevelopment of Binocular Vision: University of Gondar Department of Optometry by Nebiyat Felekehenok birukBelum ada peringkat
- AniseikoniaDokumen40 halamanAniseikoniahenok biruk100% (1)
- Measuring Refractive Errors ObjectivelyDokumen36 halamanMeasuring Refractive Errors ObjectivelyMihaela Andrada Dobre75% (4)
- Interactive Quiz Visual Optics 1: Mcqs. Among The Following Choices One Is CorrectDokumen2 halamanInteractive Quiz Visual Optics 1: Mcqs. Among The Following Choices One Is CorrectALi SaeedBelum ada peringkat
- Case Studies PresbyopiaDokumen33 halamanCase Studies PresbyopiaMalaika ZubairBelum ada peringkat
- Bifocal Contact Lenses PDFDokumen10 halamanBifocal Contact Lenses PDFLauw Dwi AndrikBelum ada peringkat
- Contact Lenses Chemicals, Methods, and Applications PDFDokumen448 halamanContact Lenses Chemicals, Methods, and Applications PDFantonioBelum ada peringkat
- Opthcs 2Dokumen24 halamanOpthcs 2Asma Sukar100% (1)
- Soft Contact Lens DesignDokumen82 halamanSoft Contact Lens DesignRuthi HnamteBelum ada peringkat
- 08 Optical AberrationsDokumen19 halaman08 Optical AberrationsMwanja MosesBelum ada peringkat
- Contact Lens Optics and Visual EffectsDokumen38 halamanContact Lens Optics and Visual EffectsManmohan ShahBelum ada peringkat
- CPG 19Dokumen78 halamanCPG 19anon-24970100% (1)
- Introduction To Spherical Lenses2Dokumen6 halamanIntroduction To Spherical Lenses2Nuon HudaBelum ada peringkat
- Contact Lenses For ChildrenDokumen6 halamanContact Lenses For ChildrenmelikebooksBelum ada peringkat
- Direct OphthalmoscopeDokumen16 halamanDirect OphthalmoscopeMuhammed AbdulmajeedBelum ada peringkat
- List of American Superhero FilmsDokumen181 halamanList of American Superhero FilmsStrauss de LangeBelum ada peringkat
- Health Awareness Poster - CholesterolDokumen1 halamanHealth Awareness Poster - CholesterolStrauss de LangeBelum ada peringkat
- Health Awareness Poster - Retinopathy - LargeDokumen1 halamanHealth Awareness Poster - Retinopathy - LargeStrauss de LangeBelum ada peringkat
- PUB304 Public Health Resource Manual Draft 3 For 20Dokumen126 halamanPUB304 Public Health Resource Manual Draft 3 For 20Strauss de LangeBelum ada peringkat
- Uj Post Dip L Degree Programmes 2010Dokumen123 halamanUj Post Dip L Degree Programmes 2010Strauss de LangeBelum ada peringkat
- PUB304 Public Health Resource Manual Draft 3 For 20Dokumen126 halamanPUB304 Public Health Resource Manual Draft 3 For 20Strauss de LangeBelum ada peringkat
- Health Awareness Poster - Breast CancerDokumen1 halamanHealth Awareness Poster - Breast CancerStrauss de LangeBelum ada peringkat
- IOPDokumen8 halamanIOPStrauss de LangeBelum ada peringkat
- Strauss Case Presentation 2012Dokumen22 halamanStrauss Case Presentation 2012Strauss de LangeBelum ada peringkat
- Ciba Vision Grading ScalesDokumen4 halamanCiba Vision Grading ScalesStrauss de LangeBelum ada peringkat
- Bloem Postgraduate Degrees and DiplomasDokumen155 halamanBloem Postgraduate Degrees and DiplomasStrauss de LangeBelum ada peringkat
- Normal & Abnormal FundussesDokumen17 halamanNormal & Abnormal FundussesStrauss de LangeBelum ada peringkat
- Residency ReportDokumen8 halamanResidency ReportStrauss de LangeBelum ada peringkat
- Overview of Contact LensesDokumen15 halamanOverview of Contact LensesTuyen PhamBelum ada peringkat
- 1a SkullDokumen39 halaman1a SkullStrauss de LangeBelum ada peringkat
- Research TopicsDokumen16 halamanResearch TopicsStrauss de LangeBelum ada peringkat
- Varicella Zoster ADO304 TAAKDokumen7 halamanVaricella Zoster ADO304 TAAKStrauss de LangeBelum ada peringkat
- Ship Safety Signs and Posters Order FormDokumen2 halamanShip Safety Signs and Posters Order FormTarık AkpınarBelum ada peringkat
- Punctate: NumberDokumen6 halamanPunctate: NumberMuhamad Chairul SyahBelum ada peringkat
- HSB Form 5 The EyeDokumen9 halamanHSB Form 5 The Eyekevin maheshBelum ada peringkat
- Amblyopia - Httpsjamanetwork - Comjournalsjamafullarticle2775449Dokumen1 halamanAmblyopia - Httpsjamanetwork - Comjournalsjamafullarticle2775449Rael Rodrigues Dos SantosBelum ada peringkat
- Belajar Diagnosa Mata TCM - 02Dokumen11 halamanBelajar Diagnosa Mata TCM - 02fauzan pintarBelum ada peringkat
- How To Use Low Dose Atropin To Slow Myopic Progression in KidsDokumen3 halamanHow To Use Low Dose Atropin To Slow Myopic Progression in Kidsrak3uBelum ada peringkat
- GlaucomaDokumen18 halamanGlaucomaOncología CdsBelum ada peringkat
- The Space Express: Chapter 1: Wake Up GirlDokumen124 halamanThe Space Express: Chapter 1: Wake Up Girlcebulue1Belum ada peringkat
- Coronavirus Pandemic PEST AnalysisDokumen2 halamanCoronavirus Pandemic PEST AnalysisAneliya ShterevaBelum ada peringkat
- Valon 5G BrochureDokumen12 halamanValon 5G BrochureHaag-Streit UK (HS-UK)100% (1)
- 1.8 ReadingDokumen10 halaman1.8 ReadingMai HiềnBelum ada peringkat
- Opticians Scam People, Just Like The Optician in 2002. My Info Isn't and It's FreeDokumen29 halamanOpticians Scam People, Just Like The Optician in 2002. My Info Isn't and It's FreeKeith Cordier100% (1)
- B-0340 Boysen Paint Thinner 1119Dokumen9 halamanB-0340 Boysen Paint Thinner 1119jeffBelum ada peringkat
- Color Preference of ElderyDokumen3 halamanColor Preference of ElderyJesusa Shane De jesusBelum ada peringkat
- Hipocratic Oath 4Dokumen28 halamanHipocratic Oath 4Hassaan MirzaBelum ada peringkat
- MSDS Yukashu Ap-710Dokumen6 halamanMSDS Yukashu Ap-710Kuro MollandBelum ada peringkat
- Ped - Eye Nasolacrimal Duct Obstruction PDFDokumen1 halamanPed - Eye Nasolacrimal Duct Obstruction PDFAryanto AntoBelum ada peringkat
- MSDS Anh ChlorineDokumen3 halamanMSDS Anh ChlorineSridharBelum ada peringkat
- Lesson Plan For Science 3 (Second Quarter)Dokumen5 halamanLesson Plan For Science 3 (Second Quarter)Dinah DimagibaBelum ada peringkat
- MSDS For DRYFILM LW-2120Dokumen13 halamanMSDS For DRYFILM LW-2120krishportBelum ada peringkat
- Chapter 29: Sensory Function My Nursing Test Banks Chapter 29: Sensory Function Meiner: Gerontologic Nursing, 5th Edition Multiple ChoiceDokumen9 halamanChapter 29: Sensory Function My Nursing Test Banks Chapter 29: Sensory Function Meiner: Gerontologic Nursing, 5th Edition Multiple ChoiceAshley Jane MacapayadBelum ada peringkat
- Rianna's nursing lab safety scoreDokumen2 halamanRianna's nursing lab safety scoreRianna JalmaaniBelum ada peringkat
- MUHS Question BankDokumen23 halamanMUHS Question BanksuhasBelum ada peringkat
- Military Joint Oil Analysis Manual Vol IIDokumen408 halamanMilitary Joint Oil Analysis Manual Vol IIVijay HanagandiBelum ada peringkat
- Use of Intraocular Lenses in Children With Traumatic Cataract in South IndiaDokumen5 halamanUse of Intraocular Lenses in Children With Traumatic Cataract in South IndiaYanjinlkham KhBelum ada peringkat
- A Beautiful Mine - UpgradedDokumen19 halamanA Beautiful Mine - UpgradedalBelum ada peringkat
- Come Morning LightDokumen675 halamanCome Morning LightRyzeBelum ada peringkat
- New-DLP Phase2 Assignment-3 Module-B Final-9.8.18Dokumen6 halamanNew-DLP Phase2 Assignment-3 Module-B Final-9.8.18PBelum ada peringkat