Hsensitif IgE - Full
Diunggah oleh
Vivi ZainuddinJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Hsensitif IgE - Full
Diunggah oleh
Vivi ZainuddinHak Cipta:
Format Tersedia
Immunopathology / Hypersensitivity Testing for ASPERGILLUS Species IgE
Hypersensitivity Testing for Aspergillus fumigatus IgE Is Significantly More Sensitive Than Testing for Aspergillus niger IgE
Thomas A. Selvaggi, MD,1 Jeremy P. Walco,2 Sujal Parikh,3 and Gary A. Walco, PhD4
Key Words: Immunology; Aspergillus species; IgE; Hypersensitivity testing; Allergy panel testing
DOI: 10.1309/AJCPZYX6SJ8FCLRN
Abstract
We sought to determine if sufficient redundancy exists between specific IgE testing for Aspergillus fumigatus and Aspergillus niger to eliminate one of the assays in determining Aspergillus hypersensitivity. We reviewed regional laboratory results comparing A fumigatusspecific IgE with A nigerspecific IgE using the Pharmacia UniCAP system (Pharmacia, Kalamazoo, MI). By using the Fisher exact test as an index of concordance among paired results, we showed a significant difference between 109 paired samples for the presence of specific IgE to A fumigatus and A niger (P < .0001). Of these specimens, 94 were negative for IgE to both species, 10 were positive for A fumigatus and negative for A niger; no specimen was positive for A niger and negative for A fumigatus. We conclude that A fumigatusspecific IgE is sufficient to detect Aspergillus hypersensitivity. The assay for A nigerspecific IgE is redundant, less sensitive, and unnecessary if the assay for specific IgE for A fumigatus is performed.
Specific IgE testing for Aspergillus is important for determining allergic sensitivities to environmental mold and is crucial in demonstrating serum sensitivity for the diagnosis of allergic bronchopulmonary aspergillosis (ABPA). We noted that some clinicians order specific IgE testing for both Aspergillus fumigatus and Aspergillus niger to detect Aspergillus hypersensitivity. In fact, clinical practice varies widely, with some clinicians testing for a wide array of fungal sensitivity, others testing for a limited number of mold sensitivities, and others testing for only A fumigatus sensitivity.1 We suspected that the presence of specific IgE to A fumigatus was more frequently positive when compared with the presence of specific IgE to A niger in the same specimen, and, therefore, the use of both tests for clinical decision making was unnecessary, with the specific IgE testing for A niger being of no additional benefit when testing for the specific IgE to A fumigatus was performed. We sought to determine if there was sufficient redundancy to allow elimination of one of the assays, thus enhancing clinical efficiency and cost-effectiveness, and if there were specific practice patterns that led to the use of testing for both A fumigatus and A nigerspecific IgE.
Materials and Methods
We reviewed 5 years of allergy testing (2002-2006) performed at the Special Diagnostic Immunology Laboratory, Hackensack University Medical Center, Hackensack, NJ, comparing specific IgE levels to A fumigatus with specific IgE levels to A niger using the Pharmacia UniCAP 100 system (Pharmacia, Kalamazoo, MI). This automated system is an enzyme-linked immunoallergosorbentbased assay calibrated
American Society for Clinical Pathology 203 Am J Clin Pathol 2012;137:203-206
DOI: 10.1309/AJCPZYX6SJ8FCLRN
203 203
Selvaggi et al / Hypersensitivity Testing for ASPERGILLUS Species IgE
against the World Health Organization standard for IgE and expressed in World Health Organization units of kilounits/ liter (kUA/L), with UA indicating an allergen-specific unit. A review of Aspergillus-specific IgE testing revealed 870 specimens in which A fumigatus was tested alone (not paired with A niger) as part of a physician-requested regional environmental panel; 109 specimens for which A fumigatus and A niger were tested, specifically having been ordered as a pair by the requesting physician; and 17 specimens tested for A fumigatus alone on the specific request of the ordering physician. Paired testing for A fumigatus and A nigerspecific IgE represented 10.9% of the requests for Aspergillus IgE. The values of these 109 clinical specimens were evaluated by using the Fisher exact test as an index of concordance comparing the presence of specific IgE to A fumigatus with the presence of specific IgE to A niger for each specimen. For the 15 paired specimens with detectable specific IgE to one or both Aspergillus species, simple means of the respective species-specific IgE levels were calculated with values of less than 0.35 kUA/L set to zero for purposes of the calculation of this mean.
Results
In the clinical patient samples that showed a detectable specific IgE to A fumigatus and/or A niger, there was a significant difference in the comparison of the presence of specific IgE to A fumigatus and A niger (P < .0001). Ten specimens were positive for specific IgE to A fumigatus and negative
for specific IgE to A niger. No specimens that were positive for specific IgE to A niger were negative for specific IgE to A fumigatus. Of the specimens, 95 had the same IgE class (Pharmacia-determined class ranges: class 0, <0.35 kUA/L; class 1, 0.35-0.69 kUA/L; class 2, 0.70-3.49 kUA/L; class 3, 3.50-17.49 kUA/L; class 4, 17.5-49.9 kUA/L; class 5, 50.0100 kUA/L; class 6, >100 kUA/L) for both species. Of the 109 specimens, 15 (13.8%) were positive to A fumigatus and only 5 (4.6%) of 109 specimens were positive to A niger. In 13 specimens, the IgE class was higher in A fumigatus, differing by 1 class level in 6, 2 class levels in 3, 3 class levels in 3, and 4 class levels in 1 Table 1. Of 109 specimens, 1 had the same class level for A fumigatus and A niger (class 2), and 1 of 109 showed a higher class level in A niger, differing by 1 class (class 3 vs 4). For the 15 specimens with a detectable specific IgE level to either Aspergillus species, the mean specific IgE level to A fumigatus was 5.88 kUA/L and the mean specific IgE level to A niger was 1.96 kUA/L. Only 2 of the 15 specimens showed a higher level of measured specific IgE antibody to A niger. The most common associated diagnosis for which a positive result was obtained was allergic rhinitis (n = 6), with sinusitis (acute or chronic) the second most frequent diagnosis (n = 4). The latter diagnosis was always associated with a concomitant diagnosis of allergic rhinitis (Table 1). More than half the testing for any Aspergillus IgE (about 57%) was ordered by 2 of 106 physicians, both of whom were allergists. The majority of Aspergillus-specific IgE testing was for A fumigatus alone; 870 of these assays were performed as part of a regional environmental allergy panel, in which
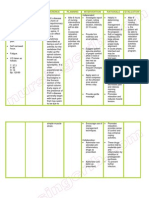
Table 1 Characteristics of the Subset of Serum Samples With Detectable Aspergillus-Specific IgE to Aspergillus fumigatus and/or Aspergillus niger
Sample No. 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 A fumigatus + + + + + + + + + + + + + + + A niger + + + + + A fumigatus (kUA/L) 0.38 14.3 0.71 1.58 1.02 27.8 9.75 0.47 4.58 3.93 13.1 0.4 5.02 0.39 4.73 A niger (kUA/L) <0.35 0.45 <0.35 <0.35 2.74 <0.35 <0.35 <0.35 1.39 23.4 <0.35 <0.35 <0.35 <0.35 1.45 A fumigatus Class* 1 3 2 2 2 4 3 1 3 3 3 1 3 1 3 A niger Class* 0 1 0 0 2 0 0 0 2 4 0 0 0 0 2 Diagnosis Aspergillosis, bronchiectasis Allergic rhinitis, acute sinusitis, chronic pharyngitis, nasal sinus polyp Unknown Allergic rhinitis, chronic sinusitis Allergic rhinitis, chronic sinusitis, asthma Urticaria, upper respiratory infection Sarcoidosis, bronchiectasis Allergic rhinitis Allergic rhinitis Allergic rhinitis, sinusitis Cystic fibrosis Chronic pharyngitis, unspecified immune deficiency Unspecified respiratory abnormality Unknown Unknown
kUA /L, kilounits per liter, with UA indicating an allergen-specific unit; +, present; , absent. * The Pharmacia (Kalamazoo, MI)-determined IgE classes are defined as follows: class 0, <0.35 kU /L; class 1, 0.35-0.69 kU /L; class 2, 0.70-3.49 kU /L; class 3, 3.50-17.49 A A A kUA /L; class 4, 17.5-49.9 kUA /L; class 5, 50.0-100 kUA /L; class 6, >100 kUA /L.
204 204
Am J Clin Pathol 2012;137:203-206
DOI: 10.1309/AJCPZYX6SJ8FCLRN
American Society for Clinical Pathology
Immunopathology / Original Article
A nigerspecific IgE was not included. When ordered as individually selected tests, 86.5% of the time, A fumigatus and A niger were ordered together. Allergists requested 96 (88.1%) of the 109 paired specimens.
Discussion
The determination of the presence of specific IgE to Aspergillus species is clinically relevant for detecting sensitivities in perennial allergic rhinitis, allergic asthma, or ABPA. In the present environment of limited resources for medical diagnosis, elimination of redundant testing is essential. To our knowledge, this is the largest study of Aspergillus hypersensitivity comparing the sensitivity of A fumigatus with A niger. We demonstrated statistically significant greater sensitivity of the specific IgE assay for A fumigatus in detecting allergic sensitivity to Aspergillus compared with the specific IgE assay for A niger. In fact, in this study, the use of specific IgE to A niger alone would have missed two thirds of the Aspergillus sensitivity detected by the specific IgE assay to A fumigatus if a single assay had been used. Furthermore, when both assays are used, we have shown that there is no case in which sensitivity to A fumigatus is not detected when a sensitivity to A niger is detected. We do not believe this is strictly a geographic regional effect, although A niger germination is greatly affected by humidity, with a failure to germinate at a humidity of less than 76%. We believe this difference in sensitivity is more than likely a physiologic effect, with colonization of A niger in the lung being more difficult to establish than A fumigatus. This is likely related to exquisite sensitivity to pH, with A niger requiring a pH of 4.5 for optimal germination and germ tube length. Also, structural differences between Aspergillus species such as conidial size make alveolar space penetration more difficult for A niger.2,3 There are only rare reports of aspergillosis in which A niger is the pathogen, and these usually involve an immunocompromised state, such as in patients with bone marrow transplantation or lung transplantation.4,5 In addition, A nigerassociated aspergillosis has been seen in patients with diabetes mellitus, which is thought to create an acidic environment conducive to survival of A niger with its affinity for low pH.2,6,7 In fact, in our series, the 2 patients with higher specific IgE levels of A niger compared with specific IgE levels of A fumigatus had a history of diabetes mellitus (Mary A. Michelis, MD, unpublished data, personal communication, January 2011). Hoshino et al8 reported a case of ABPA associated with A niger isolated from sputum. In this case, the patient had a positive skin test to A fumigatus, likely as part of the clinical criteria for diagnosis of ABPA, thus demonstrating an in vivo cross-sensitivity between A fumigatus and A niger in this
American Society for Clinical Pathology
patient. Lake et al9 reported a case of mixed allergic bronchopulmonary fungal disease with Aspergillus terreus isolated from bronchoscopy sputum. In this case, A terreus induced a positive skin test response (7-mm wheal) with a cross-reacting skin test response to A fumigatus (6-mm wheal), the latter of which was twice the size of the cross-reacting skin test reaction to A niger (3-mm wheal). This suggests, in this one patient, the generation of a more robust in vivo response of specific IgE to A fumigatus compared with A niger, resulting in a greater sensitivity of the A fumigatus in vivo skin test compared with A niger. Although assays for IgE to Aspergillus are classically associated with aspergillosis, only one of the positive samples was ordered with a diagnosis of aspergillosis. As noted, the most common diagnosis associated with the positive Aspergillus IgE result in the paired testing in this study was allergic rhinitis (Table 1) and likely reflects that the majority of the physicians requesting this testing were allergists, compared with their colleagues in the specialties of pulmonology, pediatrics, and internal medicine (data on file) who tended to order A fumigatus testing alone, when not ordered as part of a panel, but as a specific query for the presence of Aspergillus hypersensitivity. This finding suggests the pattern of requesting multiple Aspergillus species IgE assays evolved according to specialty and/or local convention. We conclude, in general, that there is no clinical usefulness or relevance for the A nigerspecific IgE assay in determining Aspergillus sensitivity because the A fumigatusspecific IgE assay has a statistically significant superior sensitivity for making this determination. However, certain rare exceptions may exist in specific occupations in which proteolytic enzymes isolated from A niger are used, such as phytase, a phosphatase derived from A niger used by animal feed additive manufacturers, which is an identified allergen in reported cases of occupational asthma in these workers. Serum of phytase-sensitized workers showed enzyme immunoassay inhibition for IgE specifically to A niger but not to other molds.10 Flaviastase, another proteolytic enzyme isolated from A niger, is implicated in inducing occupational asthma in pharmacy workers.11 In these various occupational exposures, the specific evaluation for specific IgE to A niger has the potential to contribute to confirming the origin of the occupational exposure, depending on the actual allergen(s) and the ability to detect them with the assay. In addition, the potential general exposure to A niger derived gene product in certain genetically engineered foods such as soybeans may lead to clinical hypersensitivities to unique allergens, depending on the allergenicity of the product expressed.12 Since current detection of A niger sensitivity in the isolation of enzymes from A niger is likely the result of antigen impurities in the isolation, the use of the A niger specific IgE assay in genetically engineered foods or products
Am J Clin Pathol 2012;137:203-206 205
DOI: 10.1309/AJCPZYX6SJ8FCLRN
205 205
Selvaggi et al / Hypersensitivity Testing for ASPERGILLUS Species IgE
may not be relevant as the impurities of the original source of the gene may not be present. For example, the expression of Aspergillus-derived -amylase genes in Saccharomyces cerevisiae13 may generate sensitivities to -amylase and/or S cerevisiae rather than the Aspergillus species of origin. Future considerations regarding genetic engineering need to address certain modes of sensitivity, eg, ingested vs inhaled, leading to different clinical expression of allergic hypersensitivity, and the creation of neoantigens leading to diagnostic conundrums such as the development of clinical allergy hypersensitivity to altered soybeans but with negative specific IgE testing to natural soybeans. These scenarios highlight the importance of a detailed history of exposures when deciding on confirmatory assays to avoid unnecessary testing and the importance of understanding the availability of the testing repertoire and the relevance of the potentially requested assay. While both A fumigatus and A niger specific IgE tests are offered with the Pharmacia ImmunoCAP systems and are not considered analyte-specific reagents, difficulties may arise in the context of other Aspergillus sensitivities encountered in other specific scenarios, such as exposure of industrial bakers using endoxylanase X24 derived from Aspergillus nidulans and -amylase derived from Aspergillus oryzae,13 for which these Aspergillus-specific IgE tests are not available. However, depending on the history, one could simply obtain a specific IgE test for -amylase or, as noted, S cerevisiae, as applicable, which are available as tests in the current analyzer used in this study and are not considered analyte-specific reagents. However, significant cost considerations remain given the rarity of these testing requests. As noted, there is little justification for the additional cost of conducting both A fumigatus and A nigerspecific IgE assays as additional diagnostic information is generally not obtained since the A fumigatusspecific IgE assay is the most sensitive test when evaluating for Aspergillus sensitivity in most clinical settings. Conversely, in the rare clinical situation in which A nigerspecific IgE testing is indicated, the addition of A fumigatusspecific IgE testing would likely not add direct relevant specific data to the clinical evaluation. Further studies are recommended to assess whether currently entrenched practice patterns lead to duplicate or irrelevant allergy testing in other clinical manifestations of allergy hypersensitivity that can be evaluated for cost savings. This is particularly relevant when selecting the components of allergy testing panels, which themselves can be subject to reduced reimbursement due to caps on the allowable number of tests covered for payment by third-party payers.
From the 1Special Diagnostic Immunology Laboratory, Department of Medicine, Hackensack University Medical Center, Hackensack, NJ; 2University of Louisville School of Medicine, Louisville, KY; 3St Georges University School of Medicine, Grenada, West Indies; and 4Department of Anesthesiology and Pain Medicine, Seattle Childrens Hospital, University of Washington School of Medicine, Seattle. Address reprint requests to Dr Selvaggi: Special Diagnostic Immunology Laboratory, Dept of Medicine, Hackensack University Medical Center, 30 Prospect Ave Rm 1936, Hackensack, NJ 07601.
References
1. Denning D, ODriscoll BR, Hogaboam CM, et al. The link between fungi and severe asthma: a summary of the evidence. Eur Respir J. 2006;27:615-626. 2. Abdel-Rahim AM, Arbab HA. Factors affecting spore germination in Aspergillus niger. Mycopathologia. 1985;89:7579. 3. Severo L, Geyer G, Porto N, et al. Pulmonary Aspergillus niger intracavitary colonization: report of 23 cases and a review of the literature. Rev Iberoam Micol. 1997;14:104-110. 4. Luce J, Ostenson RC, Springmeyer SC, et al. Invasive aspergillosis presenting as pericarditis and cardiac tamponade. Chest. 1979;76:703-705. 5. Xavier M, Sales MU, Camargo JP, et al. Aspergillus niger causing tracheobronchitis and invasive pulmonary aspergillosis in a lung transplant recipient: case report. Rev Soc Bras Med Trop. 2008;41:200-201. 6. Cleland W, Johnson MJ. Studies on the formation of oxalic acid by Aspergillus niger. J Biol Chem. 1956;220:595-606. 7. Emiliani E, Bekes P. Enzymatic oxalate decarboxylation in Aspergillus niger. Arch Biochem Biophys. 1964;105:488-493. 8. Hoshino H, Tagaki S, Kon H, et al. Allergic bronchopulmonary aspergillosis due to Aspergillus niger without bronchial asthma. Respiration. 1999;66:369-372. 9. Lake F, Tribe A, McAleer R, et al. Mixed allergic bronchopulmonary fungal disease due to Pseudallescheria boydii and Aspergillus. Thorax. 1990;45:489-492. 10. Doekes G, Kamminga N, Helwegen L, et al. Occupational IgE sensitization to phytase, a phosphatase derived from Aspergillus niger. Occup Environ Med. 1999;56:454-459. 11. Pauwels R, Devos M, Callens L, et al. Respiratory hazards from proteolytic enzymes [letter]. Lancet. 1978;1:669. 12. Lei X, Stahl C. Biotechnological development of effective phytases for mineral nutrition and environmental protection. Appl Microbiol Biotechnol. 2001;57:474-481. 13. Monfort A, Blasco A, Prieto J, et al. Combined expression of Aspergillus nidulans endoxylanase X24 and Aspergillus oryzae -amylase in industrial bakers yeast and their use in bread making. Appl Environ Microbiol. 1996;62:3712-3715.
206 206
Am J Clin Pathol 2012;137:203-206
DOI: 10.1309/AJCPZYX6SJ8FCLRN
American Society for Clinical Pathology
Anda mungkin juga menyukai
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Ethical Considerations From Prisoners inDokumen17 halamanEthical Considerations From Prisoners inNino MdinaradzeBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- Global Manual On Surveillance of AEFIDokumen128 halamanGlobal Manual On Surveillance of AEFIHarold JeffersonBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- FNCP-Presence of Breeding or Resting Sites of Vectors of DiseasesDokumen5 halamanFNCP-Presence of Breeding or Resting Sites of Vectors of DiseasesAlessa Marie BadonBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- 109 513 1 PB PDFDokumen11 halaman109 513 1 PB PDFKolu koyBelum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Invos System Improving Patient Outcomes Cerebral Somatic Oximetry BrochureDokumen6 halamanInvos System Improving Patient Outcomes Cerebral Somatic Oximetry Brochuremihalcea alinBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Mental Health Class NotesDokumen3 halamanMental Health Class Notessuz100% (4)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hippocratic WritingsDokumen385 halamanHippocratic WritingsPratyaksha Sinha100% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- At Merienda - Individual ActivityDokumen6 halamanAt Merienda - Individual ActivityMoreno, John Gil F.Belum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Unknown Bacteria Lab ReportDokumen13 halamanUnknown Bacteria Lab Reportapi-529628802Belum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Bioassay For AntidiabetesDokumen39 halamanBioassay For AntidiabetesNita TriadistiBelum ada peringkat
- Nursing Care Plan Pott's DiseaseDokumen2 halamanNursing Care Plan Pott's Diseasederic95% (21)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Clinical Microbiology and Infection: Original ArticleDokumen6 halamanClinical Microbiology and Infection: Original ArticleAkira Masumi100% (1)
- Stress Management Strategies Adopted by Teachers in Public Primary Schools in Obio/Akpor Local Government Area of Rivers State, Nigeria.Dokumen94 halamanStress Management Strategies Adopted by Teachers in Public Primary Schools in Obio/Akpor Local Government Area of Rivers State, Nigeria.sorbariBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Devil You Know PDFDokumen269 halamanDevil You Know PDFElissaBelum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Kuliah PF Jantung Prof IIDokumen32 halamanKuliah PF Jantung Prof IIannis100% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- English Composition II 1Dokumen11 halamanEnglish Composition II 1api-548473407Belum ada peringkat
- Second Hand Smoke Fact SheetDokumen9 halamanSecond Hand Smoke Fact Sheetwesa77Belum ada peringkat
- How To Implement Health Technology Assessment - 230715 - 093605Dokumen10 halamanHow To Implement Health Technology Assessment - 230715 - 093605Nour ElsabahBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Causes of Metabolic AcidosisDokumen10 halamanCauses of Metabolic AcidosisKimberly Anne SP PadillaBelum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- DNA and ChromosomeDokumen15 halamanDNA and ChromosomeYudha OkpriandaBelum ada peringkat
- FWD Medical Rider enDokumen12 halamanFWD Medical Rider enKhairul HMSBBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- K2 - Strongyloides StercoralisDokumen16 halamanK2 - Strongyloides StercoraliswirputBelum ada peringkat
- Case Study Presentation-Mindy Duran-FinalDokumen30 halamanCase Study Presentation-Mindy Duran-Finalapi-278622211Belum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Normal Periodontium 1Dokumen49 halamanNormal Periodontium 1mdio midoBelum ada peringkat
- Vent Web HandoutDokumen41 halamanVent Web Handoutwaqas_xsBelum ada peringkat
- Michael H. Antoni, Roselyn Smith-Stress Management Intervention For Women With Breast Cancer-Amer Psychological Assn (2003)Dokumen222 halamanMichael H. Antoni, Roselyn Smith-Stress Management Intervention For Women With Breast Cancer-Amer Psychological Assn (2003)KmoespinoBelum ada peringkat
- Yasir Waheed CV For HECDokumen4 halamanYasir Waheed CV For HECمحمد بلال سرورBelum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Gen EdDokumen14 halamanGen EdMark Julius G AlmadinBelum ada peringkat
- Can I Live Without A Corpus CallosumDokumen6 halamanCan I Live Without A Corpus CallosumMitali BiswasBelum ada peringkat
- CHN Practice Exam 1Dokumen7 halamanCHN Practice Exam 1Domeyeg, Clyde Mae W.100% (1)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)