EMA Protocols
Diunggah oleh
MattHak Cipta
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
EMA Protocols
Diunggah oleh
MattHak Cipta:
Glycemia Protocol
l ndic3tion
In the situation that trauma is not a primary cause for. and patient who has: Decreased level of
consciousness, OR
Acute change in neurological functions in terms of speech ability, motor and/or cognitive status, OR
Evidence/reason that leads to suspicion of hypoglycemia or hyperglycemia. AND
The reading of blood glucose is: 4 mmol/L or less; OR > 20 mmol/L
Contraindication
Patient under 12 years of age.
Guidelines for Glvccmia Protocol
Speeech disability (may incl ude but not limited to the following): according to Paramedic Protocol
FS Manual (Operational) Part II - Ambulance Services
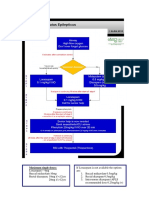
Glyc emia Protocol Flow Chart
~ I D C B A
RBS Skin Oitygen I
I
Secondary Survey: History, vital signs & capillary blood sample Decision Point
~
I
H'stiit > 20 mmoVL
I
I
H'stix S 4 mmoVL
I
I
I
Transport
I
T
HAS airway problems or swallowing
Init iate IV NS at 200 ml/hr
problems or risk of aspiration
Continue with assessment
+
and tm1tment
Failure to establish
Initiate IV glucose
r+
,,
preparation, 100 ml full rate
IV infusion of glucose
preparation
NO airway problems. NO risk of
... (Max. attempt should
aspiration AND CAN swallow by
Administer 50 mg
be limited to 3)
him/herself
Thiamine JM to deltoid
t
+
muscle before dextrose
Administer I mg
infusion is compl eted
glucagon IM/SC
Oral glucose drinks (e.g.
1 OOml glucose preparation solution)
I
Transport & continue with
...
assessment and treatment
Transport & continue
I
T
with assessment and
No or incomplete
treatment
improvement of acutely
impaired mental status
H
I Repeart H'stix (2..i H'stiit) I
Improved to former I usual
best mental status +
..
H'stix S 4 mmoVL
I
I
H'stix > 4 mmoVL
Administer 2" 100 ml glucose
preparation full rate IV infusion
- Continue with assessment and
Administer IV glucose
-
treatment
prepiration I 00 ml/hr
.
Continue with assessment
and treatment
- ,
Glucagon Protocol
I ndicntion
Decreased level of consciousness and with signs and symptoms of Hypoglycemia
The reading of blood glucose is 4 mmol/L or less, and
3 attempts in establishing intravenous infusion of DI OW have fail ed.
Contraindicatfon
Patient under 12 years of age.
History of allergy to glucagon preparation
3) Insulinoma
4) Glucagonoma
5) Phaeochromocytoma
6) Contraindications for IM injection
Initiate Hypoglyce1nia Protocol
3 attempts in establishing IV infusion of D 1 OW have failed
Administer 1 mg glucagon hydrochloride IM to deltoid muscle
Initiate RAPID Transport
Continue with assessment and monitor ABC en-route
If patient regains FULL consciousness with GCS= 15,
DI OW by mouth, max.200c.c.
.
gives
Nitroglycerin Protocol
l ndic3ti on
I) Patient whose presentation is chest pain/discomfort of cardiac ori gin; and
2) Patient who has a history of heart disease and would normally take his/her
prescribed Nitroglycerin (NTG) for chest pain/discomfort.
Contraindi cation
I) Patient has taken dn1gs alleged to increase sex potency in the past 72 hourst e.g.
Phosphodiesterase 5 Inhibitor deri vatives: Sildenafi l (Viagra), Tadalafil (Cialis).
2) Patient whose SBP < 1 OOmmHg.
3) Hypersensitivity to nitrates.
Acetyl salicylic Acid
(ASA)
Aspirin
::!: 12 years: AND
Cardiac chest pain/discomfort
presentation
< 12 years; or
Inability to swallow; or
Pregnant: or
Hypersensitive to ASA or
NSAIDs; or
NSATDs include but not Jimite.d to:-
Hx of Perforated Peptic Ulcer
Ibuprofen (Brufen)
confinned by OGD
Naproxen (Naprosyn)
(Oesophagogastroduodenoscopy) /
l ndomethacin (lndocid)
GI Bleeding; or
Mefenamic Acid (Ponstan)
Currently on Warfarin
Diclofenac (Voltaren/Cataflam)
Methyl Salicylate (Analgesic balm)
r Secondary Survey: History & Vital s i g n s ~
SBP < I OOmm Hg SBP ~ lOOmm Hg
RSE
'Y
LOC
I
'Y
DCBA
'Y
RBS
'Y
Skin
I Oxygen I
'Y
I
I Decision Point I
'Y
-Administer one dose ofNTG spray
I
I
-Load and transport
-Continue with assessment and treatment
-Reassess at eve 5 minutes
SBP < IOOmm Hg
SBP ~ I OOmm Hg and pain/discomfort is
not completely relieved
-Administer one dose of NTG spray
I I
-Continue with assessment and treatment
-Reassess at every 5 minutes
Maximum 3 NTG doses
Respiratory Protocol-(MDI with spacer)
Snlhulamol lndicalion
Chief complaint of shortness of breath (SOB)in a patient :
Who has a history of asthma or chroni c obstructi ve airway/ pulmonary disease (COAD/CO PD) OR
Who has a hi story of lung disease and is currently prescribed by doctor withP2 - agonist e.g. Salbutarnol OR
Who has an exposure history to ans/or has inhaled chemical agent and is presenting with signs and syptoms of
btonchoconstriction(i.c. lower airway obstruction)
Contraindicati on .,
Known Salbutamol allergy
lpratropium Indicati on
Patient is ~ 12 years old; and Chief complaint of SOB in a patjent who has history of lung disease or asthma or
chronic obstructive airway/pulmonary disease (COAD/COPD) AND is currently prescribed by doctor with
Ipratropium Bromide (Atrovent)
Con traindicut ion
Patient is in acute glaucoma attack; or RSE
Patient is allergic to lpratropium Bromide/ Atropine, or l'
.-------.
Patient is allergic to soya lecithin orrelated products LOC
e.g. soybean nndpeanut l'
( 1) Salbutamol
DCBA
l'
RBS
l'
Skin
l'
I Oxygen
l'
Begin Secondary Survey
- History
-Vita si
l'
!Decision Poinij
l'
~ 2to< 5 yr old : 200mcg (2 puffs)
~ Sto< 12 yr old : 300mcg (3 puffs)
~ ~ 12yr old : 400mcg (4 puffs)
(2) lpratropium Bromide ,where applicable:
If respiration is inadequate (low
RR and/or shallow respiration),
support ventilation by BVM
and high flow oxygen. Then
LOAD AND GO
~ add 40 mcg lpratropium Bromide (2 puffs)
(3) Resume Oxygen therapy
Satisfactoril y Improved
Contjnue oxygen therapy
...
Transport
T
Continue with assessment
Notimprovingomotsatisfactorily improved
-Consider administering 2nd 3rd or 4m dose of
Salbutamol at 5 minutes apart
(No lpratropium Bromidt In substqutnt
treatment)
I
Suspected Narcotic Overdose Protocol
Indication
Decreased LOC in a patient with a history that suggests narcotic overdose,
Respiratory rate < 10 per minute and I or shallow respiration, and
Difficulty in maintaining the patient's airway
(All t hree criteria must be met)
Contra indicntion
Known naloxone allergy
Patient under 12 years of age
Patient maintains bis/her own airway well.
The EMA II ambulance supervisor bas no difficulty in maintaining the patient's airway
(e.g. patients accepts OPA well and has no resistance to bagging)
RSE
...
LOC
...
DCBA
...
RBS
...
Skin
...
Oxygen
...
I
I
I Decision Point I
...
Secondary Survey:
History
Vital Signs
Administer 0.4 mg naloxone hydrochloride IM to deltoid muscle
Continue with assessment
No improvement Improvement
- Maintain ABC and assist
ventilation.
Maintain ABC and 0 2
- Haemoglucostix; if 4 mmol/L or
less, follow the Hypoglycemia
therapy
Protocol (even if history of DM
cannot be obtained).
I I
..
TRANSPORT
Continue with treatment and assessment
Hypovolemia Protocol
Indication
1) Evidence of loss of a significant quantity of blood.
2) Presence of clinical signs of shock, OR shock is anticipated because of the mechanism
of injury, the nature and extent of the injuries, or the patient 's condition.
Contraindication
Peripheral IVs.iare contraindicated
Patients under 12 years. RSE
I
I
...
LOC
...
DCBA
...
RBS
...
Skin
...
I Oxygen I
...
I Decision Point I
...
Transport
r Secondary Survey: History & Vital s i g n s ~
If SBP ~ 90 mmHg I I If SBP < 90 mmHg
Obtai n IV access
Administer IV N/S at lOOml/hr
...
Obtain IV access
Administer 500ml N/S rapid infusion
...
Continue with assessment and treatment
Continue with assessment and treatment
If SBP falls< 90 mmHg,
Follow " IF SBP
<90mmHg" infusion
Method
SBP2! 90
mm Hg,
administer IV
N/S at 500 ml/hr
SBP < 90
mmHg,
administer IV
N/S at 500 ml
rapid infusion
Administer IV N/S
at 500 ml/hr
After 1000 ml rapid
infusion
Automated External Defihrillat ion (FR2+ AEO) Protocol
I.Indication
Patient in cardiac arrest not primarily due to trauma
2.Contraindication
2. 1 Traumatic arrest (Cardiac arrest primarily due to trauma)
2.2 Newborn (Any infant at the time of birth in the pre-hospital setting).
RSE
LOC
DCBA
Witnessed Arrest
CPR and immediately use I apply AED
& defibrillation ads
Unwitnessed Arrest
2-min CPR and prepare
AED & defibrillation ads
AED analysis
EAD ECG rh thm
No
Shock
Indi cated
Check Pulse
Pulse Absent I I Pulse present I
Shock indicated
Press to Shock
2-min CPR
(Nopulsecheck
AED analysis
READ ECG rh thm)
.............
Shock indicated
Press to Shock
Load and transport L Load and transport
(:issist venti lation+
AED monitoring+
S 2 monitorin )
r - - - ~ - - - 1
(movin CPR) -+'!
Analyze every 2-3 mins
When a licable
I Re-arrest ..-
-------
Paediatric Seizure Protocol
I n<lication
Patient has on-going generalized convulsion with loss of consciousness continuously for more than
5 minutes by witness or by a reliable history AND
Patient who is ~ 12 years old.
Contraindication
Patient is older tJian 12 years of age.
Patient with history of hypersensitivity to diazepam.
Patient' s convulsion has stopped.
Patient has received benzodiazepines for termination of convulsion (e.g.TV/PR Diazepam, IV Lorazepam)
in the preeding period of less than 5 minutes.
Consideration to give treatment should be raised again after this 5-minute period has lapsed per patient's
condition.
Anti-epilepsy prophylactic agents (usually taken by the oral route) should not be counted as drug for
termination of convulsion.
RES
LOC
...
DCBA
RBS I
...
Oxygen
DECISION POINT
Secondary Survey
Critical History & Vital Signs
Administer Rectal Diazepam
<D 0 to <l year old: 2.5mg
<D I to <6 years old: Smg
<D 6 to 12 years old: IOmg
Transport
Continue with Assessment
Tramadol Protocol
Indi cation
Conscious and fully oriented patient suffering from acut severe pain arising from trauma to the trunk
and.for limbs; AND
\\'hen the use ofEntonx is contrnindicated,impracticable, ineffective or not feasible.
Contrnindicntion
Patient whose SBP < 90mmHg (Hypotension)
Patient with history of Epilepsy or seizure.
Patient under 12 years of Age.
Patient on any Drugs in the past 2 weeks.
Pregnant Patient.
Patient with history of drug/opioid Abuse.
Patient with acut Intoxi cation with alcohol.
Known hi story of hypersensitivity to Narcotics.
A mnemonic for easy memory of contraindications HEAD PAI N.
Spinal precaution as indicated
Control bemorrbage as indicated
Treat soft tissue and/or skeletal injuries as indicated
Secondary Survey: -
e Critical History of CIC
e Vital Signs
Pain Assessment
e Rule out Contraindications
e Explain side-effects to patient
Administer Tramadol IMI
< 50kg: 50 mg
~ 50kg: 75mg
Reassessment
Activated Charcoal Protocol
Indication
Patient has ingested toxic substance AND/OR medication exceeding the prescribed amount
and the time of ingestion is within 2 hours.
Patient is fully co,pscious. cooperative AND has no difficulties with self drinking and swallowing.
Patient has clear airway and no choking or vomiting.
Contraindication
Patient with history of hypersensitivity to charcoal preparation.
Patient with decreased level of consciousness. uncooperative, has difficulties with self
drinking and swallowing, whose airway is not clear or has choking or vomiting.
Patient has ingested the substance for more than 2 hours.
Patient < 12 'l..ears of ~ .
RSE
...
LOC
...
I DCBA I
...
I
RBS
I
...
I
Skin
I
...
1ore 1
Decision Point
Secondary Survey:
History
Vital Signs
Administer 50g Activat ed Charcoal
Continue with assessment and treatment
;
Adrenaline for Anaphylaxis
Indications Contraindications Side effects
I
1+2 < 12 years of age Tachycardia
I
l + 3
c present SIS of CHF
Palpitation
1+2+3
A Allergy to Adrenaline
Intracrainial
Skin - urticaria,
s Hx of Stroke (CV A)
Haemorrhage
1 generalized flushing
HT at present
or angioedcma
H
(SBP> 180&/ or Hypertension
DBP> l 10)
2
Airway obstruction-
M
Hx of MI/ coronary artery Ml,
Upper/ lower disease anginal pain
Hx of VF I life threatening
Arrhythmia requiring IV
Shock
A medication I defibrillation/
VF / VT
3 (SBP < 90 mmHg)
cardioverson to tenninate
Distributive I hypovolaemic
D
Implantable Cardioverter Other
Defibrillator arrhvthmia
Indications Drug Dosage Max
I + 2 or I + 3 or
Adrenaline
0.3mg (= 0.3 ml)SC
l dose
I + 2 + 3 & NO
( I: !OOO solution)
contraindications
Piriton !Omg(=l ml)IMl I dose
Lower airway
Ventolin
2 to < 5 years of age
obstruction
(enroute
5 to < 12 years of age 300 mcg
4 doses
(wheezing or
rhonchi)
by spacer)
> 12 years of age 400 mcg
On car if B P ~ 9 0 = 100 ml/hr.
All anaphylactic
On car ifSBP < 90 ' I
1
500 ml FR.
patient (Shock: N/S
After SBP < 90 = 2'
10
500 ml FR.
2 bolus
SBP < 90 or (enroute
I SI FR
S B P ~ 9 0 = 500 ml/hr.
of 500
anticipitated via IV) ml
shock SBPf'. 90)
After 2"d FR = 500 ml/hr
Drug Adrenaline
set Duration Elimination
5-10 mlns S-10 mlns Metabolized by enzymes in blood, liver
And other ti ssues, and excreted in urine
SC Contraindications Local skin infection Existing local injuries
lM I Contraindications Local skin infection Existing local injuries
Coagulopathy Anti-coagulant
Anaphvlaxis Flowchart
RSE
_.
Note MOI & clues of anaphylaxis
LOC
_.
A / V / P / U
-!
D
c
-.f
No radial pulse = low BP =shock
B
~
02 orBVM
~ Lower A obstnLction - wheezing
A
_.
~ Upper A obstruction-Stridor,
hoarseness, difficult swallowing
RBS
_.
Note any skin manifestation
(urticaria, generalized flushing
Skin _.
or angioedema)
~ Remove allergen if any
Decision
Bassline Vital
NO EpiPen
EpiPen available
Available
Self-injected <5 rnins
Not yet inject or
Load & go
Load & go
Self-injected another ;:::s mins
5 mins since last Epipen
~ EpiPen Contr aindication
Improved !Not imporoved
- CASHMAD + IMI complication
IMI EpiPen:
0.1 Srng Child; 0.3rng Adult
SC Adrenaline; 0.3mg (0.3ml)
LOAD&20
If > 12 years, IMI Chlorpgeniramine : 1 Omg (l ml)
(Rule out Chlorpheniramine allergy & IMI contraindication)
If lower A obstruction
Reassess SOB, lung sound, RR & Sp02
If SOB not relieved, V entolin via spacer
max 4 doses with 5 mins in between .
All anaphylactic patient, reassess SBP on car
If SBP < 90 If SBP f 90
IV N/S 500 ml @ FR
l st FR completed
~ SBP f 90 - 500 ml/hr
~ SBP < 90 - 2"d 500 ml FR
2 n FR completed - 5001nl/hr
IV N/S I 00 ml/hr
Continue assessment &
reassess as needed.
Adult Seizure Protocol (Important: This advanced protocol is acluslvt!/y ust!d by
trained EMAii ambulanct! supt!rvisors who havt! bt!t!n authorh.ed to USt! Midarolam.)
J.n\lg;at1on
Patient has on-going generalized convulsion continuously for more than 5 minutes with loss of
consciousness by witness or by a reliable history. AND
Patient who is > I 2 years old (or, in case the age is NOT known, a patient whose height is
greater than 130 cm).
Contraindication of Milia10la111
Patient with history of hypersensitivity to Midazolam.
Patient's convulsion bas stopped.
Patient has received Benzodiazepines for termination of convulsion (e.g. IV IPR Diazepam, IV /IM
Midazolam, IV Lorazepam) in a period of less than 5 minutes
Consideration to give treatment should be raised again after this S minute period has lapsed per
patient's condition.
Anti-epileptic prophylactic agents (usually taken by the oral route on a regular basis) should not
be counted as drug for termination of convulsion.
Transport
RSE
LOC
...
I DCBA I
...
I RBS
I
Skin
I Decision Point I
...
2 survey:-
Critical Hx & vital signs
...
lMl Midazolam
BW < 50 kg :7.5 mg
B W ~ 50 kg: 10 mg
I Continue to assess vitals
.._ _____ (ABC I BP I P I RR I GCS I Sp02 / Skin)
Other paramedic protocols as necessary
Continue re-assessment
(Cancelled Call) ABC
A. , , :
B.
c.
. o.
:
E.
R
0
tt : c cancelled Call)
0
4
3
2
1
5t
Glasgo\v Coma Scale ( GCS )
&.J.t NL if; f/J
5
6
4
5
&!!: 3
1:10 Ell
4
2 1' tffi!H!WUB'f :g. 3
fiB
1
2 .f-JJW fill][
1
Anda mungkin juga menyukai
- SP50 Cardiac Stress-Exercise Testing (Adult, Peds)Dokumen8 halamanSP50 Cardiac Stress-Exercise Testing (Adult, Peds)Sonu JacobBelum ada peringkat
- Using The ACLS Bradycardia Algorithm For Managing BradycardiaDokumen2 halamanUsing The ACLS Bradycardia Algorithm For Managing BradycardiasetiamegaBelum ada peringkat
- Salbutamol Drug Study Generic Name: Brand NameDokumen4 halamanSalbutamol Drug Study Generic Name: Brand NameLyn ConsingBelum ada peringkat
- Preparing For The Prescribing Safety AssessmentDokumen36 halamanPreparing For The Prescribing Safety AssessmentChAndrewBelum ada peringkat
- CovidDokumen31 halamanCovidShaheen SultanBelum ada peringkat
- Paediatric Clinical GuidelinesDokumen7 halamanPaediatric Clinical GuidelinesAndriBelum ada peringkat
- ABCDE Approach to Hypoglycaemia ManagementDokumen11 halamanABCDE Approach to Hypoglycaemia ManagementSSBelum ada peringkat
- MRCP 1 On Examination ITU: Haemoglobin 130 White Cell Count 3.2 ×10 Platelets MCVDokumen17 halamanMRCP 1 On Examination ITU: Haemoglobin 130 White Cell Count 3.2 ×10 Platelets MCVCherryBelum ada peringkat
- Assessment of The Acutely Ill PatientDokumen10 halamanAssessment of The Acutely Ill PatientZacmilo Dela TorreBelum ada peringkat
- Medicine ManagementsDokumen87 halamanMedicine ManagementsMohamed LibanBelum ada peringkat
- PBLS - Pediatric Basic Life Support and Pediatric Advance Cardiac Life SupportDokumen135 halamanPBLS - Pediatric Basic Life Support and Pediatric Advance Cardiac Life SupportSteffiBelum ada peringkat
- Clinical evaluation and diagnosis of shockDokumen3 halamanClinical evaluation and diagnosis of shockStephen CrossBelum ada peringkat
- Abcde ApproachDokumen3 halamanAbcde ApproachMaria Isabel Medina MesaBelum ada peringkat
- Medically Compromised PaftientsDokumen21 halamanMedically Compromised PaftientsLedjon KaciBelum ada peringkat
- Management of Hypertension in Children: Carlos A. Delgado, M.D.FAAPDokumen54 halamanManagement of Hypertension in Children: Carlos A. Delgado, M.D.FAAPMateen ShukriBelum ada peringkat
- 1210 DIASTOLIC HypertensionDokumen44 halaman1210 DIASTOLIC HypertensionBoysz TheBestBelum ada peringkat
- CCU HandoverDokumen9 halamanCCU Handoverapi-192342497Belum ada peringkat
- INTERNAL MEDICINE: TROPICAL INFECTIONS AND DENGUEDokumen209 halamanINTERNAL MEDICINE: TROPICAL INFECTIONS AND DENGUESilvi Qiro'atul AiniBelum ada peringkat
- KGD 2 IvanDokumen92 halamanKGD 2 IvanrikarikaBelum ada peringkat
- FINAL COVID19 1 April 2021Dokumen14 halamanFINAL COVID19 1 April 2021Wleed KhledBelum ada peringkat
- An Update Management of Acute Ischemic Stroke: SurotoDokumen36 halamanAn Update Management of Acute Ischemic Stroke: SurotoShinta DianBelum ada peringkat
- Severe Sepsis Screening Tool NhsDokumen2 halamanSevere Sepsis Screening Tool NhsDavide Antonelli LaghiBelum ada peringkat
- Pediatric Mock Resuscitation ScenariosDokumen6 halamanPediatric Mock Resuscitation ScenariosdinkytinkBelum ada peringkat
- Chapter 3: Perioperative ManagementDokumen14 halamanChapter 3: Perioperative ManagementpoddataBelum ada peringkat
- 3amali TR 2Dokumen7 halaman3amali TR 2Arsh KaiwanBelum ada peringkat
- Pediatric Protokol EmergencyDokumen19 halamanPediatric Protokol EmergencyChristian RobbyBelum ada peringkat
- Current Clinical Strategies: Handbook of AnesthesiologyDokumen180 halamanCurrent Clinical Strategies: Handbook of AnesthesiologydramaganaBelum ada peringkat
- Algoritma BradikardiaDokumen2 halamanAlgoritma BradikardiaDaniel SitungkirBelum ada peringkat
- Saudi CPR Guidlines in EnglishDokumen16 halamanSaudi CPR Guidlines in EnglishpiyushbamsBelum ada peringkat
- Management Guidelines For COVID 19 in Resource Limited Settings - MOH - NUG July 2021Dokumen11 halamanManagement Guidelines For COVID 19 in Resource Limited Settings - MOH - NUG July 2021MYo OoBelum ada peringkat
- VF PediDokumen6 halamanVF PedixiphoideusBelum ada peringkat
- AKI in The Critically IllDokumen47 halamanAKI in The Critically IllMalaka AtapattuBelum ada peringkat
- Passmedicine MRCP Mcqs-Clinical Pharmacology and ToxicologyDokumen135 halamanPassmedicine MRCP Mcqs-Clinical Pharmacology and ToxicologyHashim Ahmad100% (1)
- 5 - Endocrinology Passmedicine Q. Bank PART I 2017Dokumen366 halaman5 - Endocrinology Passmedicine Q. Bank PART I 2017'محمد علي' محمد لافي100% (1)
- Et Oh Withdrawl GuidelineDokumen2 halamanEt Oh Withdrawl GuidelineKrittin NaravejsakulBelum ada peringkat
- COVID-19 Management of Critical Care Cases PDFDokumen6 halamanCOVID-19 Management of Critical Care Cases PDFLubna AliBelum ada peringkat
- Cardiac Arrest Circular AlgorithmDokumen6 halamanCardiac Arrest Circular Algorithmno_spam_mang80% (5)
- Afib Protocol Exclusion CriteriaDokumen3 halamanAfib Protocol Exclusion CriteriaJesse M. MassieBelum ada peringkat
- Management of Symptomatic Bradycardia and TachycardiaDokumen55 halamanManagement of Symptomatic Bradycardia and TachycardiaDewintha Airene NoviantiBelum ada peringkat
- Plab 2 MaterialDokumen24 halamanPlab 2 MaterialradugaBelum ada peringkat
- Diabetic Foot Case PresentationDokumen58 halamanDiabetic Foot Case PresentationMissoSandoqji100% (1)
- Shock ManagementDokumen26 halamanShock ManagementMuhammad Irfanuddin Bin IbrahimBelum ada peringkat
- Paediatric Septic Shock Management GuideDokumen37 halamanPaediatric Septic Shock Management GuideJavedgouri GouriBelum ada peringkat
- Fever: DengueDokumen95 halamanFever: DengueAnonymous RNMJmeu8tBelum ada peringkat
- Medical Scenario 1Dokumen42 halamanMedical Scenario 1murphy 1087Belum ada peringkat
- Status Epilepticus - APLSDokumen3 halamanStatus Epilepticus - APLSMuhammadafif SholehuddinBelum ada peringkat
- Intensive Care Unit (ICU) Manual 2020-21Dokumen146 halamanIntensive Care Unit (ICU) Manual 2020-21anithaBelum ada peringkat
- ACLS NotesDokumen9 halamanACLS Notestasha0% (1)
- ACLS Class Preparation GuideDokumen9 halamanACLS Class Preparation GuideThe Print shopBelum ada peringkat
- Client Information Sheet (CIS)Dokumen10 halamanClient Information Sheet (CIS)Christine RombawaBelum ada peringkat
- Primary Care Guidelines For The Treatment of Chronic Stable Angina PectorisDokumen8 halamanPrimary Care Guidelines For The Treatment of Chronic Stable Angina PectoriserhaarahmiBelum ada peringkat
- Diabetic Foot Case PresentationDokumen58 halamanDiabetic Foot Case PresentationZH. omg sarBelum ada peringkat
- Coagulation Disorders in PregnancyDokumen20 halamanCoagulation Disorders in PregnancyHannaTashiaClaudiaBelum ada peringkat
- Ho Notes Part 1 - Medical Emergencies Notes 2.0Dokumen7 halamanHo Notes Part 1 - Medical Emergencies Notes 2.0Amin MasromBelum ada peringkat
- PracticeExam 2 QsDokumen24 halamanPracticeExam 2 QsBehrouz YariBelum ada peringkat
- Severe TBI 2017Dokumen18 halamanSevere TBI 2017DM internaBelum ada peringkat
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesDari EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesPenilaian: 4 dari 5 bintang4/5 (2)
- LSU Directions For UseDokumen12 halamanLSU Directions For UseMattBelum ada peringkat
- User Manual For Ferno Compact Carrying ChairDokumen13 halamanUser Manual For Ferno Compact Carrying ChairMattBelum ada peringkat
- Cardiac Science AED G3 Operation and Service ManualDokumen57 halamanCardiac Science AED G3 Operation and Service ManualMattBelum ada peringkat
- Advanced Life Support (Training Manual)Dokumen74 halamanAdvanced Life Support (Training Manual)Matt100% (25)
- Lifepak CR Plus Lifepak Express: Operating InstructionsDokumen78 halamanLifepak CR Plus Lifepak Express: Operating InstructionsMattBelum ada peringkat
- FERNO 35A Users' ManualDokumen30 halamanFERNO 35A Users' ManualMattBelum ada peringkat
- Colin BP-S510 Patient Monitor - User ManualDokumen137 halamanColin BP-S510 Patient Monitor - User ManualMattBelum ada peringkat
- NCP Ineffective Tissue PerfusionDokumen1 halamanNCP Ineffective Tissue PerfusionLEONELLGABRIEL RAGUINDINBelum ada peringkat
- Diseases Caused by MicroorganismsDokumen9 halamanDiseases Caused by MicroorganismsKhushbuGuptaBelum ada peringkat
- Profile of Geriatric Care: A Comparison of RSST and RSCMDokumen11 halamanProfile of Geriatric Care: A Comparison of RSST and RSCMDicky HerdanaBelum ada peringkat
- Patient Referral FormDokumen2 halamanPatient Referral Formbasel samBelum ada peringkat
- Occupational HealthDokumen10 halamanOccupational HealthMr AqmahlBelum ada peringkat
- NCP ChoreaDokumen4 halamanNCP Choreanj_pink081794100% (2)
- Pitfallsandprogress Inthediagnosisand Managementof Canineinflammatory BoweldiseaseDokumen18 halamanPitfallsandprogress Inthediagnosisand Managementof Canineinflammatory BoweldiseasemariaBelum ada peringkat
- Kali CarbDokumen12 halamanKali CarbRaveendra Mungara100% (1)
- Renal EmergenciesDokumen11 halamanRenal EmergenciesDemuel Dee L. BertoBelum ada peringkat
- Case StudyDokumen5 halamanCase StudyJhosua RoldanBelum ada peringkat
- Angelmar F. Cordova, RN Jofred M. Martinez, Man, RNDokumen27 halamanAngelmar F. Cordova, RN Jofred M. Martinez, Man, RNAngeline AsuncionBelum ada peringkat
- Tog 12685Dokumen3 halamanTog 12685saeed hasan saeedBelum ada peringkat
- Thyroid Cancer Diagnosis and ManagementDokumen45 halamanThyroid Cancer Diagnosis and Managementapi-3704562100% (1)
- DUTY SDH + CKDDokumen6 halamanDUTY SDH + CKDadelia putri wirandaniBelum ada peringkat
- Management of Pregnancy at RiskDokumen40 halamanManagement of Pregnancy at RiskMA. JYRELL BONITOBelum ada peringkat
- NCPDokumen2 halamanNCPNikai PabayoBelum ada peringkat
- Bacterial Endocarditis and OrthodonticsDokumen6 halamanBacterial Endocarditis and OrthodonticsFourthMolar.comBelum ada peringkat
- PE and HealthDokumen3 halamanPE and HealthRia Ellaine Cornelio LachicaBelum ada peringkat
- Cytokine StormDokumen1 halamanCytokine StormLBelum ada peringkat
- Postpartal Thrombophlebitis: Client Assessment Data Base Activity/RestDokumen8 halamanPostpartal Thrombophlebitis: Client Assessment Data Base Activity/RestLei OrtegaBelum ada peringkat
- How Physiotherapy Helps - Patient StoriesDokumen2 halamanHow Physiotherapy Helps - Patient StoriesDobreanu Bianca100% (1)
- Addison DiseaseDokumen40 halamanAddison DiseaseCindyBelum ada peringkat
- Adjustment DisorderDokumen7 halamanAdjustment DisorderRif'aBelum ada peringkat
- Bates, Chris. 2015. Schizoid Personality Disorder. Cinahl Information System.Dokumen5 halamanBates, Chris. 2015. Schizoid Personality Disorder. Cinahl Information System.hastyBelum ada peringkat
- Pott DiseaseDokumen36 halamanPott DiseaseGiovanna Algu100% (1)
- Morning Case Report: 34yo Female with Amphetamine IntoxicationDokumen15 halamanMorning Case Report: 34yo Female with Amphetamine IntoxicationPradnya ParamithaBelum ada peringkat
- Relapsing Polychondritis Morphology, Etiology, Pathogenesis and TreatmentDokumen1 halamanRelapsing Polychondritis Morphology, Etiology, Pathogenesis and TreatmentRiena Austine Leonor NarcillaBelum ada peringkat
- 8-Hemodynamic Monitoring: Central Venous Pressure (CVP)Dokumen6 halaman8-Hemodynamic Monitoring: Central Venous Pressure (CVP)AsmaaYL100% (1)
- CPR Guide for Adults, Children & BabiesDokumen6 halamanCPR Guide for Adults, Children & Babiesrupali gahalian100% (2)
- 3.4 Balroga - Kaumarbhritya (Ayurvedic Pediatrics)Dokumen4 halaman3.4 Balroga - Kaumarbhritya (Ayurvedic Pediatrics)Dr Thushar T.SBelum ada peringkat