Severe To Profound Permanent Hearing Loss in Children Aetiological Investigation BAAP BAPA Guideline 2008
Diunggah oleh
bebibebihoJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Severe To Profound Permanent Hearing Loss in Children Aetiological Investigation BAAP BAPA Guideline 2008
Diunggah oleh
bebibebihoHak Cipta:
Format Tersedia
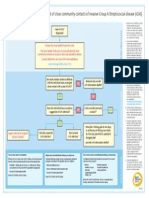
Aetiological investigation into severe to profound permanent hearing loss in children.
Produced by the British Association of Audiovestibular Physicians and British Association of Paediatricians in Audiology October 2008
Aims
The aim of these guidelines is to update the evidence based approach to the investigation of the cause of deafness in children. Guidelines are ' systematically developed statements to assist decisions about appropriate care for specific clinical circumstances' based on systematic reviews of research literature (1, 2, 3). Guidelines are not intended to restrict clinical freedom, but practitioners are expected to use the recommendations as a basis for their practice. Where possible recommendations are based on, and linked to the evidence that supports them. Areas lacking in evidence are highlighted and may form a basis for future research. This is an update to the original BAAP/BACDA guidelines on aetiological investigation into severe to profound permanent hearing loss in children (2002)
Categories of evidence:
Ia Ib IIa IIb lII IV Evidence from meta-analysis of randomised controlled trials Evidence from at least one randomised controlled trial Evidence from at least one controlled study without randomisation Evidence from at least one other type of quasi-experimental study Evidence from non-experimental descriptive studies, such as comparative studies, correlation studies, and case-control studies Evidence from expert committee reports, or opinions or clinical experience of respected authorities, or both Strength of recommendations is expressed thus:
A directly based on category I evidence B directly based on category II evidence or extrapolated recommendation from category I evidence C directly based on category III evidence or extrapolated recommendation from category I or II evidence D directly based on category IV evidence or extrapolated recommendation from category I, II, or III evidence
Why investigate hearing loss?
There are several reasons why it is important to investigate deafness: 1. To try and answer parents who ask "Why is my child deaf? " 2. To identify and treat medical conditions e.g. 8th nerve aplasia congenital infection, Jervell and Lange-Nielsen syndrome, Alport's syndrome, Neurofibromatosis type 2, Ushers Syndrome, and vestibular hypofunction. 3. The results of investigations can assist the family in making decisions about the most appropriate communication mode, educational placement and counselling on cochlear implantation e.g. in 8th nerve aplasia, Ushers syndrome etc. 4. To inform genetic counselling 5. The information from investigation of childhood deafness informs epidemiological research
Subjects
All children with bilateral permanent hearing loss and thresholds over 70 dBHL in the better ear averaged across 500, 1000, 2000 and 4000Hz.
Guidelines for Good Practice
Level 1 investigations:
Level 1 investigations should be considered for every child. Timing will depend on several factors, including the familys agreement to proceed with tests, availability of local test facilities and how well the child can cooperate with tests. In cases where aetiology has not been diagnosed then further aetiological investigations may need to be arranged and some repeated. 1) Paediatric history: Detailed history of : onset of symptoms, pregnancy, delivery and postnatal period
3 developmental milestones including speech, language, motor milestones as well as social development
History of exposure to risk factors e.g. noise ototoxic medications/ radiation head injury ear disease meningitis bacterial and viral illness immunisation status
Family history of deafness or risk factors associated with hearing loss in first and second degree relatives. History of consanguinity and ethnic origin 2) Clinical Examination: Should include height, weight and head circumference. Inspection of craniofacial region and physical measurements. Examination of the ears, neck, skin and nails, limbs, chest, abdomen and gait. Developmental assessment 3) Family audiograms: Parents and first degree relatives.(5) 4) Electrocardiography (ECG): for prolongation of the (corrected) QT interval, this is essential in children with evidence of vestibular hypofunction which may manifest as delayed motor milestones e.g. head lag, delayed sitting without support and walking. (6) (7). Please liaise with your local Cardiologist regarding the QTc interval norms. At Great Ormond Street Hospital is QTC of more than 460ms in girls and 450 ms in boys is considered as abnormal. 5) Ophthalmological assessment: assessment of visual acuity and fundoscopy discussion of electro-retinography with ophthalmologist if motor milestones are delayed (8, 9, 10, 11, 12) to detect Usher type 1 UNLESS child has adequate explanation for vestibular problems i.e. Vestibular malformation 6) Urine examination (labstix) for microscopic haematuria (13, 14, 15) 7) *CMV screen (16, 17,18) < 1year of age Urine CMV DNA PCR x 2 (separate occasions): if positive, request Guthrie card for CMV DNA testing*
>1 year of age
Urine CMV DNA PCR: and or IgG if either positive, request Guthrie card for CMV DNA testing*
Any age: consider testing mothers CMV IgG if not already known
If sending for Guthries consent from parents should be obtained 8) Blood test for Connexin 26 mutation (19, 20, 21, 22) with consent from parents, an explanation that DNA is stored afterwards in lab, that genetic testing can take a long time and permission to share results with other family members/professionals (see guidelines for consent for genetic testing (23) 9) MRI of Internal Auditory meati or CT Scan of Petrous Temporal bone (24, 25, 26, 27, 28, 29)
Level 2 investigations
Level 2 investigations will be indicated from history and clinical findings. As with level 1 investigations, timing will depend on the family's readiness to proceed with tests, availability of local test facilities and how well the child can cooperate with tests. 1) Serology: to exclude congenital infection to include maternal stored (booking) serum 2) Haematology and Biochemistry where clinically indicated e.g. Thyroid Function tests indicated if: 1) Family history of thyroid disease 2) Goitre present 3) Widened vestibular aqueduct or Mondini deformity of Cochlea (30) 4) Investigation into autoimmune diseases where clinically indicated (31) 5) Metabolic Screen on blood and urine: where clinically indicated 6) Renal ultrasound: 1) If child has preauricular pits or sinuses, deformity of ear, branchial cleft or cysts 2) Mondini defect on imaging. 3) Permanent conductive or mixed hearing loss
5 7) Clinical photography 8) Chromosomal studies: History of developmental delay Dysmorphic features (Follow Child Development Team protocol) 9) Further genetic testing if indicated after discussion with the Geneticist Consider referral to Clinical Geneticist especially if the parents are consanguineous, a syndrome is suspected, child has multiple problems, parental request opinion required on interpretation of genetic mutation testing After completion of investigations if a genetic disorder is diagnosed or no cause has been identified. 10) Vestibular investigations: Consider in all cases where motor milestones are delayed or where there is progressive deafness.
Working Group Members for BAAP & BAPA: Dr K Rajput Dr M Bitner-Glindzicz Dr S Fonseca Dr B Mac Ardle
References 1. Clinical Governance: Quality in the new NHS. HSC 1999/065. 2. resources.bmj.com/bmj/authors/checklists-forms/clinicalmanagement-guidelines 3. Committee to Advise the Public Health Service on Clinical Practice Guidelines. Field MJ, Lohr KN, eds. Clinical Practice Guidelines: Directions for a new Program. Washington DC. National Academy Press 1990. 4. Quality Standards in the Early Years: Guidelines on working with deaf children under two years old and their families. NDCS 2002. 5. Stephens D (2001) Audiometric investigation of first- degree relatives. In: Martini A, Mazzoli M, Stephens, D, Read A, ed. Definitions, Protocols & Guidelines in Genetic Hearing Impairment. London: Whurr Publishers, 32-33. 6. Bitner-Glindzicz M, Tranebjoerg L. The Jervell and Lange-Nielsen Syndrome. Adv Otorhinolaryngol 2000; 5645-5652. 7. Schwartz PJ, Spazzolini C, Crotti L, Bathen J, Amlie JP, Timothy K, Shkolnikova M, Berul CI, Bitner-Glindzicz M, Toivonen L, Horie M, Schulze-Bahr E, Denjoy I.(2006) The Jervell and Lange-Nielsen syndrome: natural history, molecular basis, and clinical outcome. Circulation. 14;113(6):783-90. 8. Calzolari E, Sensi A, Gualandi F (2001) Protocol for syndromal disorders associated with hearing loss. In: Martini A, Mazzoli M, Stephens, D, Read A, ed. Definitions, Protocols & Guidelines in Genetic Hearing Impairment. London: Whurr Publishers, 50 - 71. 9. Siatkowski RM, Flynn JT, Hodges AV, Balkany TJ (1994) Ophthalmologic abnormalities in the pediatric cochlear implant population. American Journal of Ophthalmology; 118: 70-76. 10. Armitage IM, Burke JP, Buffin JT (1995) Visual impairment in severe and profound sensorineural deafness. Archives of Diseases in Childhood; 75: 53-56. 11. Young NM, Mets MB, Hain TC. (1996) Early diagnosis of Usher syndrome in infants and children. American Journal of Otology: 17(1): 30-4.
12. Quality Standards in Vision Care for Deaf Children and Young People (2004) www.sense.org.uk 13. Pajari H, Kaariainen H, Muhonen T, Koskimies O. (1996) Alport's syndrome in 78 patients: epidemiological and clinical study. Acta Paediatrica. 85(11): 1300-6. 14. Flinter F. (1997) Alport's syndrome. Journal of Medical Genetics; 34: 326-330. 15. Wester DC, Atkin CL, Gregory MC. (1995) Alport syndrome: Clinical Update. Journal of the American Academy of Audiology; 6: 7379. 16. Peckham CS 1987, Stark O, Dudgeon JA, Martin JA, Hawkins G. Congenital cytomegalovirus infection: a cause of sensorineural hearing loss. Arch Dis Child. Dec;62(12):1233-7 17. Barbi M ,Binda S, Primache V, Caroppo S, Dido P, Guidotti P, Corbetta C, Melotti D. (2000) Cytomegalovirus DNA detection in Guthrie cards: a powerful tool for diagnosing congenital infection. J Clin Virol. Sep 1;17(3):159-65. 18. Griffiths PD ,Walter S (2005) Cytomegalovirus Curr Opin Infect Dis. Jun; 18(3): 241-5 19. Mueller R (2001) Connexin 26 (GJB2) deafness homepage (URL: http://www.iro.es/cx26deaf.html editors - X Estivill, P Gasparini, N Lench) In: Martini A, Mazzoli M, Stephens, D, Read A, ed. Definitions, Protocols & Guidelines in Genetic Hearing Impairment. London: Whurr Publishers, 176 -180. 20. Lench NJ, Houseman M, Newton V, Van Camp G, Mueller RF (1998) Connexin 26 mutations in sporadic non-syndromal sensorineural deafness. Lancet 351:415. 21. Denoyelle F, Weil D, Maw MA, Wilcox SA, Lench NJ, Allen- Powell DR, Osborn AH, Dahl H-HM, Middleton A,Houseman MJ, Dode C, Marlin S, Boulila-ElGaied A, Grati M, Ayadi H, BenArab S, Bitoun P, Lina-Grande G, Godet J, Levillers J, Garabedian EN, Mueller RF, Gardner RJM, Petit C (1997) Prelingual deafness high prevalence of a 30 delG mutation in the connexin 26 gene. Human Molecular Genetics 6: 2173-7. 22. Kessell DP, Dunlop J, Lench NJ, Liang JN, Parry G, Mueller RF. Leigh IM (1997) Connexin 26 mutations in hereditary non-syndromic, sensorineural hearing deafness. Nature 387: 80- 83. 23. Consent and confidentiality in genetic practice. Guidance on
8 genetic testing and sharing genetic information (2006).A report of the Joint Committee on Medical Genetics. www.bshg.org.uk 24. Bamiou D, Worth S, Phelps P, Sirimanna T, Rajput K (2001) Eighth Nerve Aplasia and Hypoplasia in Cochlear Implant Candidates: The Clinical Perspective. Otology and Neuro-otology; 22: 492-496. 25. Bamiou D, Phelps P, Sirimanna T. (2000) Temporal bone computed tomography findings in bilateral sensorineural hearing loss Archives of Diseases in Childhood, 82(3): 257-60. 26. Antonelli PJ, Varela AE, Mancuso AA. (1999) Diagnostic yield of high-resolution computed tomography for paediatric sensorineural hearing loss.
27. Mafong DD, Shin EJ, Lalwani AK. Laryngoscope.(2002) Use of Laboratory and Radiologic Imaging in the Diagnostic Evaluation of Children with Sensorineural Hearing Loss .112(1):1-7. 28. Hone SW, SmithRJ. (2002) Medical evaluation of pediatric hearing loss. Laboratory, radiographic and genetic testing Otolaryngol Clin N Am .35: 751-756 29. Preciado DA, Lawson L, Madden C et al Improved Diagnostic Effectiveness with a sequential diagnostic paradigm in idiopathic paediatric sensorineural hearing loss .Otology and Neurotology 26:610-615, 2005
30. Bogazzi F, Russo D, Raggi F, Ultimieri F, Berrettini S, Forli F, Grasso L, Ceccarelli C, Mariotti S, Pinchera A, Bartalena L, Martino E. (2004)Mutations in the SLC26A4 (pendrin) gene in patients with sensorineural deafness and enlarged vestibular aqueduct. J Endocrinol Invest : 27(5):430-5. 31. Reddy MV, Satyanarayana VV, Hemabindu L, Rani PU, Reddy PP, Lakshmi VS. Immunological studies in children with hearing impairment. J Indian Med Assoc. 2005 Oct:103(10):520-1.
Anda mungkin juga menyukai
- Carpal Tunnel Syndrome - A ReviewDokumen10 halamanCarpal Tunnel Syndrome - A ReviewkenthepaBelum ada peringkat
- Brosur Diet HTDokumen1 halamanBrosur Diet HTbebibebihoBelum ada peringkat
- Hypospadias - Psychosos, Sexual, and Reproductive Consequences in Adult LifeDokumen6 halamanHypospadias - Psychosos, Sexual, and Reproductive Consequences in Adult LifebebibebihoBelum ada peringkat
- Varicella Fact Sheet PDFDokumen6 halamanVaricella Fact Sheet PDFgodeapBelum ada peringkat
- Sutton Current Opinion Femtosecond Cataract SurgeryDokumen6 halamanSutton Current Opinion Femtosecond Cataract SurgerybebibebihoBelum ada peringkat
- Drug Induced Arousal PVS NeuroRehabilitation 2006 ClaussDokumen7 halamanDrug Induced Arousal PVS NeuroRehabilitation 2006 ClaussbebibebihoBelum ada peringkat
- Lens and Cataract Guide by Dr. Sanjay DhawanDokumen24 halamanLens and Cataract Guide by Dr. Sanjay DhawanVISS11100% (1)
- Syringomyelia: A Literature ReviewDokumen1 halamanSyringomyelia: A Literature ReviewbebibebihoBelum ada peringkat
- Laser StarkDokumen7 halamanLaser StarkbebibebihoBelum ada peringkat
- 05 EcceDokumen9 halaman05 EccebebibebihoBelum ada peringkat
- SomethingDokumen1 halamanSomethingbebibebihoBelum ada peringkat
- Jurnal MataDokumen5 halamanJurnal MatabebibebihoBelum ada peringkat
- Hypospadias in BriefDokumen3 halamanHypospadias in BriefbebibebihoBelum ada peringkat
- Askep CancerDokumen5 halamanAskep CancerAyu ZiboloboloBelum ada peringkat
- 367 Full PDFDokumen4 halaman367 Full PDFbebibebihoBelum ada peringkat
- Daftar PustakaDokumen9 halamanDaftar PustakabebibebihoBelum ada peringkat
- Reading CT Scan of Human BrainDokumen12 halamanReading CT Scan of Human BrainSumit RoyBelum ada peringkat
- Daftar PustakaDokumen9 halamanDaftar PustakabebibebihoBelum ada peringkat
- Blood-Immunosuppressive Therapy For AA in ChildrenDokumen4 halamanBlood-Immunosuppressive Therapy For AA in ChildrenbebibebihoBelum ada peringkat
- Aplastic Anemia: Review of Etiology and TreatmentDokumen7 halamanAplastic Anemia: Review of Etiology and TreatmentCleber MaiaBelum ada peringkat
- Tuli KongenitalDokumen4 halamanTuli KongenitalbebibebihoBelum ada peringkat
- Hematology 2005 Guinan 104 9Dokumen6 halamanHematology 2005 Guinan 104 9bebibebihoBelum ada peringkat
- The Pathophisiology of Acquired Anemia AplastiDokumen8 halamanThe Pathophisiology of Acquired Anemia AplastibebibebihoBelum ada peringkat
- Journal Reading Dokter Muda SMF THTDokumen1 halamanJournal Reading Dokter Muda SMF THTbebibebihoBelum ada peringkat
- AA, Pediatric AspectsDokumen6 halamanAA, Pediatric AspectsbebibebihoBelum ada peringkat
- Genetics HearingGuidelinesDokumen10 halamanGenetics HearingGuidelinesbebibebihoBelum ada peringkat
- Role of The Medic in NHSP Team July 2008 EndorsedDokumen2 halamanRole of The Medic in NHSP Team July 2008 EndorsedbebibebihoBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Trans Pulmopatho ColoredDokumen8 halamanTrans Pulmopatho Colored2012Belum ada peringkat
- BOT205 - Lec1 - 2018 2019 Sem 1Dokumen21 halamanBOT205 - Lec1 - 2018 2019 Sem 1Nur HananiBelum ada peringkat
- Rincian Kewenangan Klinis Dokter Spesialis Anak: Congenital DisordersDokumen6 halamanRincian Kewenangan Klinis Dokter Spesialis Anak: Congenital DisordersIMELDA ARCANBelum ada peringkat
- Igas Flow ChartDokumen1 halamanIgas Flow ChartYi Wei KoBelum ada peringkat
- Viral Hemorrhagic Fevers Causes Symptoms TreatmentDokumen58 halamanViral Hemorrhagic Fevers Causes Symptoms Treatmentodhiambo samwelBelum ada peringkat
- AP Biology 2018 FRQ PDFDokumen12 halamanAP Biology 2018 FRQ PDFJulie MaBelum ada peringkat
- Nosocomial InfectionDokumen16 halamanNosocomial Infectionmarissa ulkhairBelum ada peringkat
- How To Transmit A Covid-19 VirusDokumen2 halamanHow To Transmit A Covid-19 VirusFelica Angelina (P) X.IS.5Belum ada peringkat
- RIZAL TECHNOLOGICAL UNIVERSITY NATIONAL SERVICE TRAINING PROGRAM MODULESDokumen9 halamanRIZAL TECHNOLOGICAL UNIVERSITY NATIONAL SERVICE TRAINING PROGRAM MODULESJULIUS CAEZAR CHAVEZBelum ada peringkat
- MD1187 Recruit Vaccination Form E-Version 13Dokumen2 halamanMD1187 Recruit Vaccination Form E-Version 13Isara Nimcharoen100% (1)
- GA Mongolia Position PaperDokumen3 halamanGA Mongolia Position PaperSri RezekiBelum ada peringkat
- Locomotor System Study GuideDokumen80 halamanLocomotor System Study Guidemartincorbacho100% (1)
- Herbal Approaches for Liver DisordersDokumen45 halamanHerbal Approaches for Liver DisordersRakshit JainBelum ada peringkat
- EMQ Samples MicrobiologyDokumen5 halamanEMQ Samples MicrobiologyHugh JacobsBelum ada peringkat
- Antibacterilal Therapy of MastitisDokumen8 halamanAntibacterilal Therapy of MastitisSunilBelum ada peringkat
- Actinomycosis, Tuberculosis, Leprosy, Syphilis, NomaDokumen37 halamanActinomycosis, Tuberculosis, Leprosy, Syphilis, NomaAroosha MasoodBelum ada peringkat
- Animal InoculationDokumen10 halamanAnimal InoculationAnumol LoranceBelum ada peringkat
- Hidalgo, Rubenjie S. Dela Cruz, Anthony Jericho B. Abary, Claudine D. Tan Hoc, Anne Mei H. Oca, Renx MarkDokumen52 halamanHidalgo, Rubenjie S. Dela Cruz, Anthony Jericho B. Abary, Claudine D. Tan Hoc, Anne Mei H. Oca, Renx MarkEira LopezBelum ada peringkat
- 2020 Safe List: Drugs That Are Considered To Be SAFE For Use in The Acute PorphyriasDokumen2 halaman2020 Safe List: Drugs That Are Considered To Be SAFE For Use in The Acute PorphyriasAlexandra LupuBelum ada peringkat
- The Prevalence of Parasitic Protozoan Diseases in Iraq, 2016Dokumen5 halamanThe Prevalence of Parasitic Protozoan Diseases in Iraq, 2016Jeremia AnkesaBelum ada peringkat
- Immune Response ExplainedDokumen34 halamanImmune Response ExplainedAtanas NaydenovBelum ada peringkat
- Pelvic Fracture (Case Presentation)Dokumen36 halamanPelvic Fracture (Case Presentation)Arce A. CacalBelum ada peringkat
- Naim Oral CareDokumen34 halamanNaim Oral Carenaim157Belum ada peringkat
- Diphtheria, Enterobiasis, FilariasisDokumen2 halamanDiphtheria, Enterobiasis, FilariasisAngel Joy CatalanBelum ada peringkat
- Bacterial identification chartDokumen2 halamanBacterial identification chartKristine PangahinBelum ada peringkat
- Intro To Parasitology PDFDokumen4 halamanIntro To Parasitology PDFMatt M. MendozaBelum ada peringkat
- Hepatitis B and TetanusDokumen27 halamanHepatitis B and TetanusJohn Christian LasalitaBelum ada peringkat
- Phytochemical Analysis and in Vitro Evaluation of The Biological Activity Against Herpes Simplex Virus Type 1 (HSV-1) of Cedrus Libani A. RichDokumen5 halamanPhytochemical Analysis and in Vitro Evaluation of The Biological Activity Against Herpes Simplex Virus Type 1 (HSV-1) of Cedrus Libani A. RichAdibah BahtiarBelum ada peringkat
- General characteristics of fungi: Structure, classification, reproduction and diseasesDokumen5 halamanGeneral characteristics of fungi: Structure, classification, reproduction and diseasesDjdjjd SiisusBelum ada peringkat
- Domain Bacteria 1Dokumen3 halamanDomain Bacteria 1Ezra JungBelum ada peringkat