Urinary Tract Infection
Diunggah oleh
dinapurpleloversHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Urinary Tract Infection
Diunggah oleh
dinapurpleloversHak Cipta:
Format Tersedia
Starship Childrens Health Clinical Guideline
Note: The electronic version of this guideline is the version currently in use. Any printed version can not be assumed to be current. Please remember to read our disclaimer.
URINARY TRACT INFECTION
Introduction Definitions Diagnosis Management Prevention
Investigations Outpatient Clinic referrals References Appendix: Methods of Urine Collection & Interpretation of results
Introduction
Urinary tract infection (UTI) is one of the most common infections of childhood, with an incidence of around 5% across populations. Practice in the past has been to investigate every child on the assumption that finding vesico ureteric reflux (VUR) and giving prophylaxis would prevent further infection and what was thought to be renal scarring" i.e. damage from further infection. The renal abnormalities found in conjunction with high grade reflux are now known to usually be congenital , not acquired. Comparison of the numbers of children who suffer a UTI (approx 50,000 per million children), compared to those who are thought to have end stage kidney disease from reflux nephropathy (approx 5 per million) show a weak association at best. UTI may be a marker for underlying renal and urological structural abnormality but it is seldom the cause. Although urinary tract infections may not lead to chronic kidney disease they may be a marker for previously undetected renal malformations, particularly in younger children. In older children it is often a marker for bladder &/or bowel dysfunction. Emphasis has moved to making a correct diagnosis, providing appropriate treatment, and targeting investigations to a selected group of children. The publication of the NICE guideline in 2007, the AAP guidelines in 2011 and the Italian guidelines in 2012 all support a reduction in investigations, and do not support the routine use of prophylaxis. All guidelines agree on reducing invasive imaging of children after their first febrile UTI (specifically, reducing the use of micturating cystourethrogram, MCU). These publications were based on a combination of evidence based care, consensus view and awareness of local population trends. The following guidelines take these into account, and were reviewed by the different departments involved in the care of these children.
Definitions
Febrile UTI/ Pyelonephritis Infection of the upper (kidney) and lower urinary tract with fever. Cystitis Infection of the lower urinary tract (bladder) without fever. Atypical UTI UTI associated with sepsis or bacteraemia Concern regarding obstructive uropathy Failure to respond to antibiotics within 48 hours Associated impaired renal function Infection with a non E. coli organism
Author: Editor: Drs Kara, Campanella, Price, Williams Dr Raewyn Gavin Service: Date Reviewed: Page: Renal, Gen Paeds, Surgery, CED November 2012 1 of 8
Urinary Tract Infection
Starship Childrens Health Clinical Guideline
Note: The electronic version of this guideline is the version currently in use. Any printed version can not be assumed to be current. Please remember to read our disclaimer.
URINARY TRACT INFECTION
Recurrent UTI Two or more episodes of febrile UTI One episode of febrile UTI and one or more episodes of cystitis Three or more episodes of cystitis Asymptomatic bacteriuria Bacteriuria in the absence of pyuria. This is most often found in school aged and older girls but can also occur in infancy. Sterile Pyuria Presence of inflammatory cells/ white cells on microscopy with negative culture.
Diagnosis
The diagnosis of UTI is made on the basis of a quantitative urine culture in addition to pyuria and bacteriuria. N.B. The colonies/ ml that are reported as a positive culture may vary between laboratories. A clean specimen is required for the diagnosis of UTI. Methods of collection are discussed in detail in the appendix. Bag specimens have an unacceptably high rate of contamination and may lead to unnecessary and invasive investigations. They can be used to exclude infection but not to diagnose it. Leucocytes can be found in the urine with any febrile illness and are non specific for UTI. It is rare to find a true urine infection in the absence of significant pyuria, and the possibility of asymptomatic bacteriuria or a contaminated specimen should be considered.
Management
Treatment of acute infection: Admission for IV antibiotics is recommended for children under 3 months old and should be considered for those under 6 months old. Infants are at greater risk for septicaemia, and more likely to have anatomic abnormalities. Children with known anatomic abnormality of the urinary tract or systemic symptoms are also likely to require admission and IV therapy. Older children who are not able to tolerate oral antibiotics due to vomiting, or who are clinically unwell may also require IV therapy. Consider a full sepsis screen including CSF analysis in infants under 3 months old prior to starting antibiotics. Where CNS sepsis cannot be excluded, amoxycillin and cefotaxime should be the initial therapy in this age group. Any child unwell enough to be admitted for IV therapy should have their renal function and electrolytes checked at admission. Discuss these children with the Consultant or Registrar. Children may be changed to oral antibiotics when clinically appropriate to complete their course. The suggested minimum duration of antibiotics is 7 days. Oral antibiotic treatment can be considered for children over 6 months old who are not toxic or septic and are able to tolerate oral antibiotics treatment. Oral antibiotics may also be considered in children over 3 months old who are clinically well, after discussion with a registrar or consultant.
Author: Editor: Drs Kara, Campanella, Price, Williams Dr Raewyn Gavin Service: Date Reviewed: Page: Renal, Gen Paeds, Surgery, CED November 2012 2 of 8
Urinary Tract Infection
Starship Childrens Health Clinical Guideline
Note: The electronic version of this guideline is the version currently in use. Any printed version can not be assumed to be current. Please remember to read our disclaimer.
URINARY TRACT INFECTION
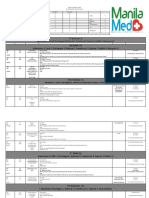
Initial IV therapy (Modify the antibiotics according to the sensitivities when available). Indication
Under 3 months of age CNS sepsis not excluded
IV Antibiotic (in order of preference)
Amoxycillin + Cefotaxime
Dosage
Amox - 50mg/kg/dose Q6H Cefotax - Load 100mg/kg, then 50mg/kg/dose Q12H - 1st week of life Q6H - >1 week of age Amox - 50mg/kg/dose Q8H - 1st week of life Q6H - >1 week of age. Gent 7 mg/kg/dose Q24H Gent - 7 mg/kg/dose Q24H (max dose 240-360mg)
Under 3 months of age CNS sepsis excluded
Amoxycillin + Gentamicin*
Over 3 months of age
Gentamicin* OR Cefuroxime
Cefurox - 25-30 mg/kg/dose (max 1500mg/dose)
*For those who require gentamicin document renal function and electrolytes at start of therapy, and modify gentamicin dosing and frequency of renal function testing if the result suggests a reduced GFR. If renal function was normal at admission and a short course of Gentamicin (<72 hours) is used, no further monitoring is required. For longer courses check trough level and creatinine before 2nd dose. Caution should be exercised with the administration of other nephrotoxic agents in children on gentamicin, who may also be volume depleted. See Aminoglycoside guideline
Oral therapy. Oral antibiotics are usually sufficient in older children in the absence of atypical infection, and may be considered in those under 6 months old. There is no single oral antibiotic that will reliably cover all episodes of UTI and local antibiotic sensitivity patterns should be taken into account.
Oral Antibiotic (in order of preference) Amoxicillin + Clavulanate
Cotrimoxazole
Cephalosporin (Cefaclor)
Dosage 10mg/kg/dose of amoxicillin component (max. 500 mg/dose) Three times daily 4mg/kg/dose of Trimethoprim component (0.5ml/kg/dose of Cotrimoxazole suspension). Twice daily Comes as suspension (240 mg Cotrimoxazole / 5ml) or 480 mg tabs. Maximum dose of Cotrimoxazole is 20 ml of suspension or 960 mg 10mg/kg/dose, (max. 500 mg/dose) Three times daily
Advantages Palatability
Disadvantages Diarrhoea
Can be used as prophylaxis
Small risk of blood dyscrasia NOTE: 30% of all EColi isolates are resistant
Palatability
serum sickness, propensity to select for ESBL* organisms. Renal, Gen Paeds, Surgery, CED November 2012 3 of 8
* Extended spectrum beta lactamase resistant organisms
Author: Editor: Drs Kara, Campanella, Price, Williams Dr Raewyn Gavin Service: Date Reviewed: Page:
Urinary Tract Infection
Starship Childrens Health Clinical Guideline
Note: The electronic version of this guideline is the version currently in use. Any printed version can not be assumed to be current. Please remember to read our disclaimer.
URINARY TRACT INFECTION
Clinical progress and antibiotic sensitivities should be checked, therefore arrange follow up (either by hospital staff or GP) within 2 days of commencing antibiotics. Telephone follow-up may be adequate if the child is getting better. Repeat urine tests are not necessary in children who respond well to treatment.
Prevention:
There is increased understanding that UTI, VUR and bladder / bowel dysfunction are linked. Children with voiding dysfunction and constipation are more likely to suffer recurrent infection. Antibiotic prophylaxis is no longer routinely recommended and has not been shown to be of benefit in the majority of children including those with VUR, and there is a risk of developing resistant organisms. Antibiotic prophylaxis may be considered in: Some children with recurrent UTIs (discuss with consultant) Some children with significant urological conditions (discuss with urology) Infants who are not on prophylaxis, and undergo an MCU should be treated with a three day course of antibiotics (at treatment dose) commencing the day prior to the MCU.
Antibiotic for prophylaxis (In order of preference) Cotrimoxazole
Cefaclor
Dose 2mg/kg of trimethoprim component (0.25ml/kg of Cotrimoxazole mixture) at night. Max. dose of Cotrimoxazole 10 ml or 480 mg. 5-10mg/kg (max. 250 500 mg/dose) at night
Investigations:
These depend on the age of the child, the severity of infection and past history. Ultrasonography (US) Inpatient/acute ultrasonography is indicated for: Children admitted with atypical UTI Children admitted and not responding to treatment within 48 hours Infants admitted under 3 months old. Outpatient Ultrasonography within 6 weeks (unless done as an inpatient): Children under 12 months old with first febrile UTI All children with: o severe illness o recurrent febrile UTI o atypical history (at discretion of the treating doctor)
Author: Editor: Drs Kara, Campanella, Price, Williams Dr Raewyn Gavin Service: Date Reviewed: Page: Renal, Gen Paeds, Surgery, CED November 2012 4 of 8
Urinary Tract Infection
Starship Childrens Health Clinical Guideline
Note: The electronic version of this guideline is the version currently in use. Any printed version can not be assumed to be current. Please remember to read our disclaimer.
URINARY TRACT INFECTION
Asymptomatic bacteriuria does not require routine imaging. Scans should include evaluation of renal size, parenchymal pattern, renal collecting systems, ureters, and bladder (pre and post voiding when possible as voiding dysfunction is associated with UTI in older children). It is helpful to request that a copy of the US report is sent to the GP. Follow up US one year later: Changes in kidney size and shape and transient ureteric dilatation may be seen on imaging done during acute infection. Children with parenchymal abnormalities seen on initial US should have a follow up US one year later. If abnormalities persist then nuclear medicine imaging should be considered. MCU There is no evidence of benefit from detecting VUR for the majority of children and for this reason MCU is no longer a routine recommendation. The request for an MCU should come from within hospital only. MCU should be considered for infants under 3 months with US abnormalities after their first febrile UTI and /or atypical UTI for children under 6 months with recurrent febrile UTI and / or abnormal US for male infants where there is concern regarding obstructive uropathy on US DMSA/ DTPA Nuclear medicine imaging is the most sensitive means of detecting renal parenchymal abnormalities. Indications include; asymmetry in renal size, abnormal renal size for age, and a suspicion of a parenchymal defect or scarring on US. Persistent parenchymal abnormality may represent renal dysplasia and / or acquired damage and should be followed up.
Outpatient Clinic Referrals:
Referrals should include details of history, any previous imaging, method of urine collection, microscopy and culture result and treatment. The following children should be considered for follow up: Children with abnormal imaging results Children admitted with UTI with atypical infection Children with recurrent UTI. These children should be referred in the first instance to the General Paediatric service in their own DHB. For children with major abnormalities on imaging, discuss with consultant regarding referral directly to renal or urology clinic.
Author: Editor: Drs Kara, Campanella, Price, Williams Dr Raewyn Gavin Service: Date Reviewed: Page: Renal, Gen Paeds, Surgery, CED November 2012 5 of 8
Urinary Tract Infection
Starship Childrens Health Clinical Guideline
Note: The electronic version of this guideline is the version currently in use. Any printed version can not be assumed to be current. Please remember to read our disclaimer.
URINARY TRACT INFECTION
Consider referral directly to Urology (Paediatric Surgical Service) for infants & children with: significant renal pelvic dilatation (>15mm or >10mm if bilateral) concerns regarding obstruction if unsure whether a clinic referral is warranted you can ask that the radiology is reviewed by the urologists first. Consider referral directly to Nephrology (Paediatric Renal service) for children with: renal impairment renal dysplasia or parenchymal defect.
References
Prevalence of urinary tract infection in childhood: a meta analysis. Pediatr Infect Dis J. 2008; 27 (4) 302-308. Does treatment of vesicoureteric reflux in childhood prevent end stage kidney disease attributable to reflux nephropathy? Pediatrics. 2000; 105 (6): 1236-1241. Childhood urinary tract infections as a cause of chronic kidney disease. Pediatrics 2011; 128(5): 840-847. Diagnosis and management of urinary tract infection in children: summary of NICE guidance. BMJ 2007; 333: 395-7. Clinical Practice Guideline for the diagnosis and management of the initial UTI in febrile infants and children 2-24 months. Pediatrics 2011; 128: 595-610. Febrile urinary tract infections in children: recommendations for the diagnosis, treatment and follow up. Acta Pediatr 2012; 101:451-457. Febrile urinary tract infections in children. NEJM 2011; 365: 239-250. The Swedish reflux trial in children: IV . Renal damage. J Urol 2010; 184: 292-297. Antibiotic prophylaxis and recurrent urinary tract infection in children. NEJM 2009; 361:1748-1759.
Author: Editor:
Drs Kara, Campanella, Price, Williams Dr Raewyn Gavin
Service: Date Reviewed: Page:
Renal, Gen Paeds, Surgery, CED November 2012 6 of 8
Urinary Tract Infection
Starship Childrens Health Clinical Guideline
Note: The electronic version of this guideline is the version currently in use. Any printed version can not be assumed to be current. Please remember to read our disclaimer.
URINARY TRACT INFECTION
Appendix: Methods of Urine Collection & Interpretation of Results
Plastic Urine Bag This is useful as a screening test only in children who cannot void on request (usually under 3 years). The genitalia should be washed with chlorhexidine gluconate 4.5 mg and cetrimide 45mg/30 mls irrigation solution and dried before application of the bag. Urine collected in the bag should be tested with a urine dipstick for leucocytes or nitrates. If the dipstick is positive (i.e. 1+ or more), obtain a definitive urine sample (catheter or suprapubic aspirate). The rate of contamination is too high to diagnose a UTI from a bag sample, however they may be used to rule out infection in some situations. Do not send bag urines for culture: this often gives a false positive result (85% in some studies). Bag urine which is normal on the dipstick should be discarded if clinical suspicion is low. There is a 2-3% chance of missing a UTI using a dipstick alone. If clinical suspicion is high a definitive urine specimen is required. Do not collect a bag urine. Do not give antibiotics unless a definitive urine specimen has been obtained. In infants less than 3 months of age bag urine specimens are less sensitive as a screening test, and UTI is potentially more serious in the very young. For these reasons dipstick testing of a bag urine specimen should not be used to rule out UTI in this age group.
Clean Catch Clean catch urine has been demonstrated to have relatively high sensitivity and specificity and is an alternative to catheter or supra-pubic urine collection in non-toilet trained children (except neonates and those who are very unwell). It involves having a caregiver catch a sample of urine in a specimen pot once spontaneous urine flow starts. This method relies on caregiver co-operation and alertness and requires the infant or young child to spend some time without a nappy. A 10% contamination rate has been reported. Midstream Urine (MSU) Can be obtained from children who void on request (usually >3 years old). There is no need to clean the perineum first. In uncircumcised boys, if possible collect urine with foreskin retracted (do not apply force when retracting). The first few millilitres are discarded, then a specimen obtained. Interpretation of MSU culture result: Pure bacterial growth of >108 colony forming organisms (CFU)/l with pyuria means infection. Any growth <107 CFU/L makes infection unlikely. A mixed growth of >108 CFU/L, or intermediate pure growth (105 -108 CFU/L) requires repeating the procedure as this may indicate early infection. Interpret culture results considering both clinical factors and urine microscopy results.
Author: Editor:
Drs Kara, Campanella, Price, Williams Dr Raewyn Gavin
Service: Date Reviewed: Page:
Renal, Gen Paeds, Surgery, CED November 2012 7 of 8
Urinary Tract Infection
Starship Childrens Health Clinical Guideline
Note: The electronic version of this guideline is the version currently in use. Any printed version can not be assumed to be current. Please remember to read our disclaimer.
URINARY TRACT INFECTION
Catheter Specimens Catheter specimens are useful in children who are too young to provide a MSU, who have a positive bag urine, or are unwell with a high probability of UTI and warrant a more invasive and urgent approach to investigation. Catheter specimens are preferred to supra-pubic aspiration. Position the child in a "frog-leg" position, clean the genitalia with chlorhexidine gluconate 4.5 mg and cetrimide 45mg/30 mls irrigation solution. Wear sterile gloves and use a sterile drape to avoid contaminating the catheter. Introduce a small Nelaton catheter coated with sterile lubricating jelly into the urethral meatus, and advance until urine flows. Discard the first few ml of urine, then collect a specimen. Where age appropriate procedural sedation is available this can reduce the distress of the procedure and should be considered. Interpretation of catheter specimen culture result : >108 CFU/L 107 CFU/L 108 CFU/ L 106 CFU/L - 107 CFU/L <106 CFU/L 95% chance of infection. infection is likely. if clinical suspicion high, repeat urine specimen. infection is unlikely.
Pyuria is usually present in a genuine UTI. Absence of pyuria makes the diagnosis equivocal.
Supra-Pubic Aspiration (SPA) This is no longer in common use, but may be considered for children in whom for some reason obtaining urine byby catheter is inappropriate or cannot be obtained. Offer the child a drink. Aspirate when you percuss the bladder >3 cm above the pubic symphysis. This is usually about 60 minutes after the last voiding. Clean the skin (chlorhexidine solution or alcohol) and allow to dry. Insert a 22G needle on a 5 ml syringe 1-2 cm above the symphysis in the midline perpendicular to the skin. Aspirate gently as you advance to a depth of 2-3 cm. If no urine is obtained, remove the needle. Avoid repeated probing (change to a catheter specimen, as this is more likely to be successful with a low volume of urine in the bladder). Have an assistant ready to make a clean catch if the child voids during the procedure. Interpretation of SPA culture result: Any growth from SPA urine indicates infection. However note the possibility of contamination of the specimen with skin commensal flora, or with faecal flora if multiple probing with the needle has passed through the bowel. NB: Both CSU and SPA require presence of urine in the bladder the child must be hydrated and give consideration to use of a bladder scanner if available to confirm presence of urine. This will improve diagnostic yield.
Author: Editor:
Drs Kara, Campanella, Price, Williams Dr Raewyn Gavin
Service: Date Reviewed: Page:
Renal, Gen Paeds, Surgery, CED November 2012 8 of 8
Urinary Tract Infection
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Med Surg Nurse Brain SheetDokumen2 halamanMed Surg Nurse Brain SheetJan Marcus95% (20)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Wet Cell and Radial DeviceDokumen21 halamanWet Cell and Radial DeviceChava Chavous100% (1)
- FRACP Written Exam Otago MCQ Book 2016Dokumen470 halamanFRACP Written Exam Otago MCQ Book 2016Qiliang Liu100% (2)
- 6th Central Pay Commission Salary CalculatorDokumen15 halaman6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Detailed Lesson Plan in Quarter 4 WK 1 Digestive ProcessDokumen10 halamanDetailed Lesson Plan in Quarter 4 WK 1 Digestive ProcessmalouBelum ada peringkat
- Praktik Dalam Keperawatan: ReferensiDokumen1 halamanPraktik Dalam Keperawatan: ReferensidinapurpleloversBelum ada peringkat
- SD ArticleDokumen6 halamanSD ArticledinapurpleloversBelum ada peringkat
- Daftar PustakaDokumen7 halamanDaftar PustakadinapurpleloversBelum ada peringkat
- Prosedure Specific Gravity ADokumen5 halamanProsedure Specific Gravity AdinapurpleloversBelum ada peringkat
- Abnormal Labor/Dystocia: Dystocia (Antonym Eutocia Greek: Tokos "Childbirth") Is An Abnormal orDokumen12 halamanAbnormal Labor/Dystocia: Dystocia (Antonym Eutocia Greek: Tokos "Childbirth") Is An Abnormal ordinapurpleloversBelum ada peringkat
- Jurnal 2Dokumen10 halamanJurnal 2dinapurpleloversBelum ada peringkat
- Human Papillomavirus Infection and TheDokumen7 halamanHuman Papillomavirus Infection and ThedinapurpleloversBelum ada peringkat
- Everyday PracticeDokumen5 halamanEveryday PracticeThoma KumaraBelum ada peringkat
- NCSP Guidelines ALL SmallDokumen60 halamanNCSP Guidelines ALL SmalldinapurpleloversBelum ada peringkat
- FIGOCEDokumen11 halamanFIGOCEAldwin TanuwijayaBelum ada peringkat
- Abnormal BleedingDokumen20 halamanAbnormal BleedingratnacantikBelum ada peringkat
- 18Dokumen9 halaman18dinapurpleloversBelum ada peringkat
- Cervicals Qu AmousDokumen2 halamanCervicals Qu AmousdinapurpleloversBelum ada peringkat
- 2.2 Gyn Pathology OvaryDokumen0 halaman2.2 Gyn Pathology OvarydinapurpleloversBelum ada peringkat
- Basic Radiotherapy Nursing GuideDokumen26 halamanBasic Radiotherapy Nursing GuidedinapurpleloversBelum ada peringkat
- Postpartal Complications GuideDokumen15 halamanPostpartal Complications GuidedinapurpleloversBelum ada peringkat
- 3 7Dokumen14 halaman3 7dinapurpleloversBelum ada peringkat
- Exercise For Daily Test On Grade ViiiDokumen2 halamanExercise For Daily Test On Grade ViiidinapurpleloversBelum ada peringkat
- Exercise For Daily Test On Grade ViiiDokumen2 halamanExercise For Daily Test On Grade ViiidinapurpleloversBelum ada peringkat
- Nephrotic Syndrome PDFDokumen16 halamanNephrotic Syndrome PDFSulabh ShresthaBelum ada peringkat
- RPC Gemel enDokumen8 halamanRPC Gemel endinapurpleloversBelum ada peringkat
- Dysfunctional Labor DystociaDokumen8 halamanDysfunctional Labor Dystociamardsz100% (2)
- RJK Himkajaya NDFDokumen26 halamanRJK Himkajaya NDFdinapurpleloversBelum ada peringkat
- 1 2Dokumen2 halaman1 2dinapurpleloversBelum ada peringkat
- Assessment of PainDokumen1 halamanAssessment of PaindinapurpleloversBelum ada peringkat
- FYIAJIDDArticleNov2009 114.6 PDFDokumen10 halamanFYIAJIDDArticleNov2009 114.6 PDFdinapurpleloversBelum ada peringkat
- Information Needs of Myocardial Infarction PatientsDokumen9 halamanInformation Needs of Myocardial Infarction PatientsdinapurpleloversBelum ada peringkat
- 144 Full PDFDokumen8 halaman144 Full PDFdinapurpleloversBelum ada peringkat
- - - - - شاهينDokumen101 halaman- - - - شاهينDdsa FaaaBelum ada peringkat
- Studies in History and Philosophy of Science: Eliminative Abduction in MedicineDokumen8 halamanStudies in History and Philosophy of Science: Eliminative Abduction in MedicineFede FestaBelum ada peringkat
- A Concise Review On Nerium Oleander L.Dokumen5 halamanA Concise Review On Nerium Oleander L.tatralor100% (1)
- OEC ch25Dokumen10 halamanOEC ch25Phil McLeanBelum ada peringkat
- CADILADokumen75 halamanCADILAKunal Kumar100% (1)
- Choosing the Right PaediatricianDokumen263 halamanChoosing the Right PaediatricianSuneethaVangala100% (1)
- A Novel Lymphocyte Transformation Test (LTT-MELISAR) For Lyme BorreliosisDokumen8 halamanA Novel Lymphocyte Transformation Test (LTT-MELISAR) For Lyme Borreliosisdebnathsuman49Belum ada peringkat
- Hipospadia, PPT Blok 3.1 (English)Dokumen11 halamanHipospadia, PPT Blok 3.1 (English)weniBelum ada peringkat
- Abdominal ExaminationDokumen14 halamanAbdominal ExaminationValeria Guerra CastilloBelum ada peringkat
- Biology 10Th Edition Raven Test Bank Full Chapter PDFDokumen36 halamanBiology 10Th Edition Raven Test Bank Full Chapter PDFlewis.barnes1000100% (12)
- Book of Vile DarknessDokumen25 halamanBook of Vile Darknessv0idless100% (2)
- Target Client List For NCD Prevention and Control SERVICES (Part 1)Dokumen9 halamanTarget Client List For NCD Prevention and Control SERVICES (Part 1)Lchg KrvyBelum ada peringkat
- Abortion, Anc, and CS: Focus+ Lecture SeriesDokumen24 halamanAbortion, Anc, and CS: Focus+ Lecture SeriesTianah davisBelum ada peringkat
- Irritablebowelsyndrome: What Treatments Really WorkDokumen16 halamanIrritablebowelsyndrome: What Treatments Really WorkTeodora RaindropBelum ada peringkat
- CretDokumen63 halamanCretMtpa MashoorBelum ada peringkat
- Covid-19 Info DriveDokumen61 halamanCovid-19 Info DriveMac MacapilBelum ada peringkat
- Joint Mobilization EnhancesDokumen12 halamanJoint Mobilization EnhancesDavid BrunoBelum ada peringkat
- Clinical For PracticalDokumen72 halamanClinical For PracticalYogendra SinghBelum ada peringkat
- Introduction and Basic Principles: Dr. K. S. Abbasi Department of Food Tech/Human NutritionDokumen8 halamanIntroduction and Basic Principles: Dr. K. S. Abbasi Department of Food Tech/Human Nutritionnouman ashrafBelum ada peringkat
- Rectal Cancer,: Clinical Practice Guidelines in OncologyDokumen28 halamanRectal Cancer,: Clinical Practice Guidelines in OncologyRaíla SoaresBelum ada peringkat
- Biological Control 178 (2023) 105145 M. Yousefvand Et AlDokumen5 halamanBiological Control 178 (2023) 105145 M. Yousefvand Et AlGenaina CristofoliBelum ada peringkat
- How Can Women Make The RulesDokumen0 halamanHow Can Women Make The Ruleshme_s100% (2)
- Nursing Care Plan #1 Assessment Explanation of The Problem Goal/Objective Intervention Rational EvaluationDokumen10 halamanNursing Care Plan #1 Assessment Explanation of The Problem Goal/Objective Intervention Rational EvaluationmalindaBelum ada peringkat
- Census August 8 - August 9, 2020Dokumen6 halamanCensus August 8 - August 9, 2020Patrick JohnBelum ada peringkat
- Diane Pills Drug StudyDokumen4 halamanDiane Pills Drug StudyDawn EncarnacionBelum ada peringkat
- Abraham Lincoln and John F. Kennedy: Evidence of Reincarnation Through Coincidence and Synchronicity by Kevin WilliamsDokumen53 halamanAbraham Lincoln and John F. Kennedy: Evidence of Reincarnation Through Coincidence and Synchronicity by Kevin WilliamsKevin Williams50% (2)