Otitis Media
Diunggah oleh
apocruJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Otitis Media
Diunggah oleh
apocruHak Cipta:
Format Tersedia
Page 1 of 4
105 Otitis Media
ETIOLOGY
Otitis media (OM) is a suppurative infection of the middle ear cavity. Bacteria gain access to the middle ear when the normal patency of the eustachian tube is blocked by upper airway infection or hypertrophied adenoids. Air trapped in the middle ear is resorbed, creating negative pressure in this cavity and facilitating reflux of nasopharyngeal bacteria. Obstructed flow of secretions from the middle ear to the pharynx combined with bacterial reflux leads to infected middle ear effusion. Integration link: Middle ear Anatomy Taken from Netter's Clinical Anatomy 2E Both bacteria and viruses can cause OM. The common bacterial pathogens are Streptococcus pneumoniae, nontypable Haemophilus influenzae, Moraxella catarrhalis, and, less frequently, group A streptococcus. S. pneumoniae that is relatively resistant to penicillin (minimal inhibitory concentration 0.1 to 1 g/mL) or highly resistant to penicillin (minimal inhibitory concentration 2 g/mL) is isolated with increasing frequency from young children, particularly those who attend day care or have received antibiotics recently. Viruses, including rhinoviruses, influenza, and respiratory syncytial virus, are recovered alone or as copathogens in 20% to 25% of patients.
EPIDEMIOLOGY
Diseases of the middle ear account for approximately one third of office visits to pediatricians. The peak incidence of acute OM is between 6 to 15 months of life. By the first birthday, 62% of children experience at least one episode. Few first episodes occur after 18 months of age. OM is more common in boys and in patients of lower socioeconomic status. There is increased incidence of OM in Native Americans and Alaskan Natives and in certain high-risk populations, such as children with human immunodeficiency virus (HIV), cleft palate, and trisomy 21. In most of the United States, OM is a seasonal disease with a distinct peak in January and February, which corresponds to the rhinovirus, respiratory syncytial virus, and influenza seasons. It is less common from July to September. The major risk factors for acute OM are young age, bottle-feeding as opposed to breastfeeding, drinking a bottle in bed, parental history of ear infection, presence of a sibling in the home (especially a sibling with a history of ear infection), sharing a room with a sibling, passive exposure to tobacco smoke, and increased exposure to infectious agents (day care). As defined by the presence of six or more acute OM episodes in the first 6 years of life, at least 12% of children in the general population have recurrent OM and would be considered otitis-prone. Craniofacial anomalies and immunodeficiencies often are associated with recurrent OM; most children with recurrent acute OM are otherwise healthy.
CLINICAL MANIFESTATIONS
In infants, the most frequent symptoms of acute OM are nonspecific and include fever, irritability, and poor feeding. In older children and adolescents, acute OM usually is associated with fever and otalgia (acute ear pain). Acute OM also may present with otorrhea (ear drainage) after spontaneous rupture of the tympanic membrane. Signs of a common cold, which predisposes to acute OM, are often present (see Chapter 102). A bulging tympanic membrane, air fluid level, or visualization of purulent material by otoscopy are reliable signs of infection (Table 105-1).
LABORATORY AND IMAGING STUDIES
page 390 page 391
file://C:\Users\Xiang Yan\AppData\Local\Temp\~hh875C.htm
3/5/2013
Page 2 of 4
Table 105-1. Definition of Acute Otitis Media (AOM) A diagnosis of AOM requires History of acute onset of signs and symptoms Presence of middle ear effusion Signs and symptoms of middle ear inflammation The definition of AOM includes all of the following: Recent, usually abrupt, onset of signs and symptoms of middle ear inflammation and middle ear effusion The presence of middle ear effusion that is indicated by any of the following: Bulging of the tympanic membrane Limited or absent mobility of the tympanic membrane Air-fluid level behind the tympanic membrane Otorrhea Signs or symptoms of middle ear inflammation as indicated by either Distinct erythema of the tympanic membrane or Distinct otalgia (discomfort clearly referable to the ear that results in interference with or precludes normal activity or sleep) Routine laboratory studies, including complete blood count and erythrocyte sedimentation rate, are not useful in the evaluation of OM. Tympanometry provides objective acoustic measurements of the tympanic membrane-middle ear system by reflection or absorption of sound energy from the external ear duct as pressure in the duct is varied. Measurements of the resulting tympanogram correlate well with the presence or absence of middle ear effusion. Instruments using acoustic reflectometry are available for office and home use. Use of reflectometry as a screening test for acute OM should be followed by examination with pneumatic otoscopy when abnormal reflectometry is identified. Bacteria recovered from the nasopharynx do not correlate with bacteria isolated by tympanocentesis. Tympanocentesis and middle ear exudate culture are not always necessary, but they are required for accurate identification of bacterial pathogens and may be useful in neonates, immunocompromised patients, and patients not responding to therapy.
DIFFERENTIAL DIAGNOSIS
Examination of the ears is essential for diagnosis and should be part of the physical examination of any child with fever. The hallmark of OM is the presence of effusion in the middle ear cavity (see Table 105-1). The presence of an effusion does not define its nature or potentially infectious etiology, but it does define the need for appropriate diagnosis and therapy. Pneumatic otoscopy, using an attachment to a hermetically sealed otoscope, allows evaluation of ventilation of the middle ear and is a standard for clinical diagnosis. The tympanic membrane of the normal, air-filled middle ear has much greater compliance than if the middle ear is fluid-filled. With acute OM, the tympanic membrane is characterized by hyperemia, or red color rather than the normal pearly gray color, but it can be pink, white, or yellow with a full to bulging position and with poor or absent mobility to negative and positive pressure. The light reflex is lost, and the middle ear structures are obscured and difficult to distinguish. A hole in the tympanic membrane or purulent drainage confirms perforation. Occasionally, bullae are present on the lateral aspect of the tympanic membrane, which characteristically are associated with severe ear pain. The major difficulty is differentiation of acute OM from OM with effusion, which also is referred to as chronic OM. Acute OM is accompanied by signs of acute illness, such as fever, pain, and upper respiratory tract inflammation. OM with effusion is the presence of effusion without any of the other signs and symptoms.
file://C:\Users\Xiang Yan\AppData\Local\Temp\~hh875C.htm
3/5/2013
Page 3 of 4
TREATMENT
Recommendations for treatment are based on certainty of diagnosis and severity of illness. A certain diagnosis can be made if there is rapid onset, signs of middle ear effusion, and signs and symptoms of middle ear inflammation. The recommended first-line therapy for most children with a certain diagnosis of acute OM or those with an uncertain diagnosis but who are younger than 2 years of age or have fever greater than 39 C or otalgia is amoxicillin (80 to 90 mg/kg/day in two divided doses). Children with an uncertain diagnosis who are older than 2 years of age may be observed if appropriate follow-up can be arranged. Failure of initial therapy with amoxicillin at 3 days suggests infection with -lactamase-producing H. influenzae or M. catarrhalis or resistant S. pneumoniae. Recommended next-step treatments include high-dose amoxicillinclavulanate (amoxicillin 80 to 90 mg/kg/day), cefuroxime axetil, cefdinir, or ceftriaxone (50 mg/kg intramuscularly in daily doses for 1 to 3 days). Intramuscular ceftriaxone is especially appropriate for children younger than 3 years of age with vomiting that precludes oral treatment. Tympanocentesis may be required for patients who are difficult to treat or who do not respond to therapy. Acetaminophen and ibuprofen are recommended for fever. Decongestants or antihistamines are not effective.
COMPLICATIONS AND PROGNOSIS
The complications of OM are chronic effusion, hearing loss, cholesteatoma (masslike keratinized epithelial growth), petrositis, intracranial extension (brain abscess, subdural empyema, or venous thrombosis), and mastoiditis. Acute mastoiditis is a suppurative complication of OM with inflammation and potential destruction of the mastoid air spaces. The disease progresses from a periostitis to an osteitis with mastoid abscess formation. Posterior auricular tenderness, swelling, and erythema, in addition to the signs of OM, are present. The pinna is displaced downward and outward. Radiographs or computed tomography scan of the mastoid reveals clouding of the air cells, demineralization, or bone destruction. Treatment includes systemic antibiotics and drainage if the disease has progressed to abscess formation. OM with effusion is the most frequent sequela of acute OM and occurs most frequently in the first 2 years of life. Persistent middle ear effusion may last for many weeks or months in some children but usually resolves by 3 months following infection. Evaluating young children for this condition is part of all well-child examinations.
page 391 page 392
Conductive hearing loss should be assumed to be present with persistent middle ear effusion; the loss is mild to moderate and often is transient or fluctuating. Glue ear is used to describe the presence of a viscous, gluelike effusion that is produced when the chronically inflamed middle ear mucosa produces an excess of mucus that, because of absence of the normal clearance of the middle ear cavity, is retained for prolonged periods. Normal tympanograms after 1 month of treatment obviate the need for further follow-up. In children at developmental risk or with frequent episodes of recurrent acute OM, 3 months of persistent effusion with significant bilateral hearing loss is a reasonable indicator of need for intervention with insertion of pressure equalization tubes.
PREVENTION
Parents should be encouraged to continue exclusive breastfeeding as long as possible and should be cautioned about the risks of bottle-propping and of children taking a bottle to bed. The home should be a smoke-free environment. Children identified at high-risk for recurrent acute OM are candidates for prolonged courses of antimicrobial prophylaxis, which can reduce recurrences significantly. Amoxicillin (20 to 30 mg/kg/day) or sulfisoxazole (50 mg/kg/day) given once daily at bedtime for 3 to 6 months or longer is used for prophylaxis. The conjugate S. pneumoniae vaccine reduces pneumococcal OM caused by vaccine serotypes by 50%, all pneumococcal OM by 33%, and all OM by 6%. Annual immunization against influenza virus may be helpful in
file://C:\Users\Xiang Yan\AppData\Local\Temp\~hh875C.htm
3/5/2013
Page 4 of 4
high-risk children.
file://C:\Users\Xiang Yan\AppData\Local\Temp\~hh875C.htm
3/5/2013
Anda mungkin juga menyukai
- Viral EncephalitisDokumen29 halamanViral Encephalitisruntika100% (1)
- ShockDokumen9 halamanShockapocruBelum ada peringkat
- ILS L4 Transcripts PDFDokumen38 halamanILS L4 Transcripts PDFThuy Lan75% (4)
- Glue Ear, (Otitis Media with Effusion) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandGlue Ear, (Otitis Media with Effusion) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Pharma QuestionsDokumen5 halamanPharma QuestionsLey BeltranBelum ada peringkat
- Expanded Program On Immunization and Reproductive Health DOH ProgramsDokumen24 halamanExpanded Program On Immunization and Reproductive Health DOH ProgramsPrince Jhessie L. AbellaBelum ada peringkat
- STDDokumen2 halamanSTDapocruBelum ada peringkat
- 12 Otitis MediaDokumen19 halaman12 Otitis MediaCabdiBelum ada peringkat
- Referat Bronkopneumonia JulDokumen18 halamanReferat Bronkopneumonia Juljuliand hidayat100% (1)
- Chronic Suppurative Otitis MediaDokumen14 halamanChronic Suppurative Otitis MediaIkhsan100% (1)
- Otitis Media AcuteDokumen30 halamanOtitis Media AcuteDede Gustina AyuBelum ada peringkat
- Otitis Media3Dokumen6 halamanOtitis Media3Anthony LopezBelum ada peringkat
- Case Presentation - Acute Otits MediaDokumen31 halamanCase Presentation - Acute Otits MediaJean nicole Garibay0% (1)
- Otitis Media OtolaryngologyDokumen45 halamanOtitis Media OtolaryngologyDr.Sherif Bugnah100% (5)
- Deases of Middle EarDokumen43 halamanDeases of Middle EarPrathamesh ParekhBelum ada peringkat
- OtitismediaDokumen5 halamanOtitismediaKrisna Yudi100% (1)
- Jurnal OtitisDokumen35 halamanJurnal OtitisDiah ArumBelum ada peringkat
- Acute Otitis Media - StatPearls (Internet) - Treasure Island (FL) StatPearls Publishing (2023)Dokumen12 halamanAcute Otitis Media - StatPearls (Internet) - Treasure Island (FL) StatPearls Publishing (2023)Kezia KurniaBelum ada peringkat
- Otitis Media KDDokumen13 halamanOtitis Media KDPutri Senna RahayuBelum ada peringkat
- Dr. Asti Widuri Sp. THTDokumen40 halamanDr. Asti Widuri Sp. THTMuhammad Faried FahdaBelum ada peringkat
- Felyanto Puspa Haryani Wirda YunitaDokumen17 halamanFelyanto Puspa Haryani Wirda YunitaSilvia Hari PrastiwiBelum ada peringkat
- Aom PDFDokumen8 halamanAom PDFMei Risanti SiraitBelum ada peringkat
- Otitis Media AkutDokumen7 halamanOtitis Media AkutghostmanzBelum ada peringkat
- Otitis Media AkutDokumen30 halamanOtitis Media Akutindah sariBelum ada peringkat
- Update On Otitis MediaDokumen28 halamanUpdate On Otitis MediakarenafiafiBelum ada peringkat
- Acute Otitis Media (AOM) - 1Dokumen24 halamanAcute Otitis Media (AOM) - 1SabeerBelum ada peringkat
- CPG On AomDokumen9 halamanCPG On AomEllese SayBelum ada peringkat
- Chronic Suppurative Otitis MediaDokumen7 halamanChronic Suppurative Otitis MediavannyanoyBelum ada peringkat
- Atelectasis 1Dokumen17 halamanAtelectasis 1Arief FakhrizalBelum ada peringkat
- 6.otitis MediaDokumen17 halaman6.otitis MediasavasBelum ada peringkat
- Penyebab Otalgia 2010 PDFDokumen11 halamanPenyebab Otalgia 2010 PDFnotpentingBelum ada peringkat
- Penyebab Otalgia 2010Dokumen11 halamanPenyebab Otalgia 2010siska tiaraBelum ada peringkat
- 2010 31 102 Jane M. Gould and Paul S. Matz: Pediatrics in ReviewDokumen17 halaman2010 31 102 Jane M. Gould and Paul S. Matz: Pediatrics in ReviewAndres DynamoMobileBelum ada peringkat
- Diagnosis and Treatment of Otitis MediaDokumen9 halamanDiagnosis and Treatment of Otitis Mediaburbu1490Belum ada peringkat
- Otitis MediaDokumen31 halamanOtitis MediaManish AdhikariBelum ada peringkat
- CH 09Dokumen12 halamanCH 09Daniel DennyBelum ada peringkat
- Acute Otitis MediaDokumen8 halamanAcute Otitis MediaRose JosephBelum ada peringkat
- Chronic Suppurative Otitis MediaDokumen15 halamanChronic Suppurative Otitis MediaEza IndahsariBelum ada peringkat
- Acute Respiratory InfectionDokumen9 halamanAcute Respiratory InfectionStephen FoxBelum ada peringkat
- Upper Respiratory Tract Infections-2009Dokumen103 halamanUpper Respiratory Tract Infections-2009MaህBelum ada peringkat
- Ear InfectionsDokumen16 halamanEar Infectionsjoal510Belum ada peringkat
- Chronic Otitis MediaDokumen4 halamanChronic Otitis MediaOvyanda Eka MItraBelum ada peringkat
- Otitis MediaDokumen7 halamanOtitis MediaNorminaKiramAkmadBelum ada peringkat
- URTIpedia ADabbaghDokumen68 halamanURTIpedia ADabbaghMuhammad AbdurrahmanBelum ada peringkat
- Case Report OMEDokumen8 halamanCase Report OMEYosephine ninaBelum ada peringkat
- Otitis MediaDokumen18 halamanOtitis MediaShesilia AgnestiBelum ada peringkat
- Otitis Media Diagnosis and TreatmentDokumen19 halamanOtitis Media Diagnosis and TreatmentreyhanrrBelum ada peringkat
- 18mo With CongestionDokumen7 halaman18mo With CongestiondakewtwontonBelum ada peringkat
- Otītis MediaDokumen12 halamanOtītis MediaABUBEKER BESHIRBelum ada peringkat
- Nursing Management of Children With Respiratory System DysfunctionsDokumen27 halamanNursing Management of Children With Respiratory System DysfunctionsDody ZainBelum ada peringkat
- Journal Reading: Presented By: Ratna WindyaningrumDokumen46 halamanJournal Reading: Presented By: Ratna WindyaningrumRatna WindyaningrumBelum ada peringkat
- Chronic Suppurative Otitis MediaDokumen16 halamanChronic Suppurative Otitis MediaEmil P. MuhammadBelum ada peringkat
- Acute Otitis Media in Young Children - Diagnosis and MGT PDFDokumen9 halamanAcute Otitis Media in Young Children - Diagnosis and MGT PDFdanny17phBelum ada peringkat
- ABTRACTDokumen1 halamanABTRACTPrajin SaranBelum ada peringkat
- Otitis Media NCBIDokumen10 halamanOtitis Media NCBISYAFIRA LAILA NURULITABelum ada peringkat
- Otitis MediaDokumen43 halamanOtitis MediaJamie AgbannawagBelum ada peringkat
- Otitis Media Clinical PresentationDokumen14 halamanOtitis Media Clinical PresentationIvan PathfinderBelum ada peringkat
- BPJ PDFDokumen5 halamanBPJ PDFriyanBelum ada peringkat
- Hutz2018 Article NeurologicalComplicationsOfAcuDokumen7 halamanHutz2018 Article NeurologicalComplicationsOfAcuAchmad YunusBelum ada peringkat
- Upper Respiratory Tract InfectionsDokumen20 halamanUpper Respiratory Tract Infectionsshamma shahulhameedBelum ada peringkat
- Chronic Suppurative Otitis MediaDokumen4 halamanChronic Suppurative Otitis MediarchristoverBelum ada peringkat
- Otitis MediaDokumen1 halamanOtitis MediaThan Ramile Dela CruzBelum ada peringkat
- Otitis Media With Effusion: Case ReportDokumen8 halamanOtitis Media With Effusion: Case ReportMas KaryonBelum ada peringkat
- Ear Infection Essentials Understanding, Treating, and PreventingDari EverandEar Infection Essentials Understanding, Treating, and PreventingBelum ada peringkat
- Acute Otitis Media: Causes, Treatment, and PreventionDari EverandAcute Otitis Media: Causes, Treatment, and PreventionBelum ada peringkat
- Acute PancreatitisDokumen48 halamanAcute PancreatitisapocruBelum ada peringkat
- Application FormDokumen1 halamanApplication FormapocruBelum ada peringkat
- Abortionsource 100605123737 Phpapp01Dokumen38 halamanAbortionsource 100605123737 Phpapp01Erina Erichan OtoBelum ada peringkat
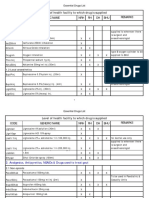
- March 2013 April 2013 : Feb 2013 Apr 2013 Mar 2013 May 2013Dokumen1 halamanMarch 2013 April 2013 : Feb 2013 Apr 2013 Mar 2013 May 2013apocruBelum ada peringkat
- March 2013 : Sun Mon Tue Wed Thu Fri SatDokumen4 halamanMarch 2013 : Sun Mon Tue Wed Thu Fri SatapocruBelum ada peringkat
- The Four-Color Problem: Concept and Solution: Steven G. KrantzDokumen37 halamanThe Four-Color Problem: Concept and Solution: Steven G. KrantzapocruBelum ada peringkat
- Cost Break Down For Kaluthra Kalu, Mahrgama Nine Puppies and DeltaDokumen10 halamanCost Break Down For Kaluthra Kalu, Mahrgama Nine Puppies and DeltaAdopt a Dog in Sri LankaBelum ada peringkat
- Jama Shenoy 2019 RV 180010Dokumen12 halamanJama Shenoy 2019 RV 180010GustavoCalderinBelum ada peringkat
- 1446798272-Tanzania Road Distance ChartDokumen86 halaman1446798272-Tanzania Road Distance ChartSTEVEN TULABelum ada peringkat
- Isolation of Virus in Cell Culture, Embryonated: Eggs and Laboratory AnimalsDokumen70 halamanIsolation of Virus in Cell Culture, Embryonated: Eggs and Laboratory AnimalsSandeep PokhrelBelum ada peringkat
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDokumen1 halamanCertificate For COVID-19 Vaccination: Beneficiary DetailsDDHS KANCHEEPURAMBelum ada peringkat
- Immunization Verification (CW 107) enDokumen3 halamanImmunization Verification (CW 107) enGoldy MaezBelum ada peringkat
- HepadnaviridaeDokumen15 halamanHepadnaviridaeNaty SantamariaBelum ada peringkat
- KFDDokumen6 halamanKFDsubhash nayakBelum ada peringkat
- Talon PDFDokumen1 halamanTalon PDFJern HullBelum ada peringkat
- Star Smiley 2007Dokumen343 halamanStar Smiley 2007David Ajibade100% (1)
- Factors Affecting Compliance of Childhood Routine Immunization and Dropout RateDokumen4 halamanFactors Affecting Compliance of Childhood Routine Immunization and Dropout RateInternational Journal of Innovative Science and Research Technology100% (1)
- Procedure For Assessing The Acceptability, in Principle, of Vaccines (Page 315)Dokumen398 halamanProcedure For Assessing The Acceptability, in Principle, of Vaccines (Page 315)Abdelkarim BelkebirBelum ada peringkat
- Confused Drug NamesDokumen9 halamanConfused Drug Nameszoemilanista12Belum ada peringkat
- Avian Encephalomyelitis (AE)Dokumen22 halamanAvian Encephalomyelitis (AE)Dr.Kedar Karki ,M.V.Sc.Preventive Vet.Medicine CLSU Philippines100% (1)
- Code Generic Name NRH RH DH BHU Remarks Level of Health Facility To Which Drug Is SuppliedDokumen42 halamanCode Generic Name NRH RH DH BHU Remarks Level of Health Facility To Which Drug Is SuppliedTob JurBelum ada peringkat
- H1N1 Swine FluDokumen17 halamanH1N1 Swine Flurhtsghmagkfsy100% (5)
- CBDMT - Market and Business Intelligence - Pharmaceutical IndustryDokumen1 halamanCBDMT - Market and Business Intelligence - Pharmaceutical IndustrycbdmtBelum ada peringkat
- Isaenit Cerrud SPIN Phrasal VerbsDokumen6 halamanIsaenit Cerrud SPIN Phrasal VerbsisaenitBelum ada peringkat
- Communicable Diseases Causes, Control and Prevention Among Pre-School Age ChildrenDokumen4 halamanCommunicable Diseases Causes, Control and Prevention Among Pre-School Age ChildrenVinayagam VenkatesanBelum ada peringkat
- Babesia MicrotiDokumen9 halamanBabesia MicrotiFrancene Ac-DaBelum ada peringkat
- Biliary AtresiaDokumen9 halamanBiliary AtresiaPrabhakar KumarBelum ada peringkat
- Search Results For: Dengue: FeverDokumen18 halamanSearch Results For: Dengue: FeverlakshmibavaBelum ada peringkat
- Resistance of The Body To Infection: Ii. Immunity and AllergyDokumen25 halamanResistance of The Body To Infection: Ii. Immunity and AllergyVergel John ErciaBelum ada peringkat
- Health Assessment Phemap 2009Dokumen67 halamanHealth Assessment Phemap 2009SergeGaudielBelum ada peringkat
- Biodiversity: Protista MoneraDokumen11 halamanBiodiversity: Protista MoneraridwanBelum ada peringkat