4
Diunggah oleh
Mike FandriHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
4
Diunggah oleh
Mike FandriHak Cipta:
Format Tersedia
202 CHAPTER 18/Neonatal Hyperoiiirubinemia Neonatal Fiypcrbilirubinemia 203 ever, an increase in minor motor abnormalities of unclear signiWance was
detected in those with serum bilirubin levels over 20 m1;idL. Hyperbiliru binemia in term infants has been associated with abnormalities in brain-stem audiomeiric-evoked responses (B.4ER), cry characteristics, and neurobehavioral measures. However, these changes disappear when bilirubin levels fall and there are no measurable long-term sequelae. Kernicterus has been reported in jaundiced healthy, full-term, breastfed infants. All predictive values for bilirubin toxicity are based on heel stick values. G. Bilirubin toxicity and the low-birth-weight infant. Initial early studies of babies of 1250 to 2500 g and 28 to 36 weeks' gestational age showed no relationship between neurologic damage and bilirubin levels over 18 to 20 mgldL. Later studies, however, began to report "kernicterus at autopsy or neurodevelopmental abnormalities at follow-up in premature infants under 1250 g who had bslv _ . : ' U i ' . i levels previously thought to be safe (e.g., under 10 to 20 mg/dL). ,=recause kern:cterus in preterm infants is now considered uncommon, hind sight suggests that this so-called "low bilirubin kernicte_ - us" was largely due to factors other than bilirubin alone. For example, unrecognized intracranial hemorrhage, inadvertent exposure to drugs that displace bilirubin from albu min, or the use of solutions (e.g., benzyl alcohol) that can alter the blood-brain barrier may have accounted for developmental handicaps or kernicterus in infants with low levels of serum bilirubin. In addition, premature infants are more likely to sutler from anoxia, hypercarbia, and sepsis, whi,:.`. also open the blood-brain barrier and lead to enhanced bilirubin deposition in neural tissue. Finally, the pathologic changes seen in postmortem preterm infant brains has been more consistent with nonspecific damage than with true kerructerus. Thus, bilirubin toxicity in lowbirth-weight infants may not be a function of bilirubin levels per se bill of their overall clinical status. VI. Management of unconjuyated hyperbilirubinemia. Given the uncertainty of determinirrg what levels of bilirubin are toxic, these are general clinical guidelines only and should be modified in any sick infant :vith acidosis, hypercapnia, hypoxemia, asphyxia, sepsis, hypoalhurninemia (<2.5 mg/dL), or signs of biliru bin encephalopathy. A. General principles. Management of unconjugated hyperbilirubinemia is clearly tied to the etioloec. Early identification of known causes of nonphysio logic hyperbilirubinemia (see III. B- C- and D) should prompt close observation for development of jaunc:oe, appropriate laboratory investigation, and timelc intervention. Any medication (see Table 18.1) or clinical factor that may inter fere with bilirubin metabolism, bilirubin binding to albumin, or the integrity of the blood-brain barrier should be discoatinued or corrected. Infants who are receiving inadequate feedings, or who have decreased urine and stool output, need increased feedings both in :o!ume and iii calories to reduce the entero hepatic circulation of bilin~bin. Inf.^.nts with hypothyroidism need adequate re placement of thyroid hormone. If levels of bilirubin are so high that the infant is at risk for kernicter us, bilirubin may be removed mechanically by eachang" transfusion, its excretion increased by alternative pathways using photothcr apy, or its normal metabolism increased by drugs such as phenobarbital. B. Infants with hemc'.ytic disease 1. in Rh disease we start intensive phototherapy immediately An eschan ,;w transfusion is performed if the hilirubin level c; predicted to each 20 (see Fig. 18.5, A and B). 2. In ABO hemolytic disease we start phototl:erapy if the bilirubin IrwI w ceeds l U mg!dL at 12 hours, 12 mg/dL at 18 hours, 14 mg!dL at Z 1 hm l
.
or 15 mgldL at any time. If the bilirubin reaches 20 ma/dL, an ex(li:w w transfusion is done. 3. [n hernolytic disease of other causes we treat as if it were Rh disr:r:.w bles 18.3. 18.4, 18.5). C. Healthy term infants (Fig. 18.2). The American Academy of Pediatrics (AAP) has published a set of practice parameters for the treatment of unronju a=ataA hvnrrW!:-mhinemia in healthv, full-term neonates.
SE
, .
.- --
~
ii
I N
>
I B
I N
: : :
WIN '
A
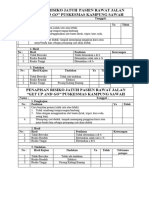
FIG. 78.5_ H,rth dace
_;ij
S~rum I,i:,i ~~I~in IwuI~ plmttcd a;;ainst ayc in tcrm infants (A) and prma;r tut'e inf:rirt~ (li) ~mtli ~wnliwl,l:wt~usi;.
Hour or6irth
St rum bilirubin (mg/dl) in term infants (Continuw:. J
r, v-~ lcfs (see IIID1 mcasurement.~ and thu hour-,Iwwlo iwwliiil .wa m vdce ,ttv infants at risk /or-;i;;ni(icant hyxrlvln w I'll 14 -1111, 1 I,-I. :mc not ruutinel V strccned on our III';IILII\' 0-In, 11 f:mn , 11111, (wrur; in tile first 2 dacs of lilc oi other risk (,I, I
p - . ~w \I,, i ~,f wnr Lor!r: inf~a^W at ,( -Sent home Iw'?-7 to 48 huw . w( il1.v, nwc fcm ,nt< ,hwul<1 tile Informed about neonatal jaundic, III lot n~ ., lv.v ,4Iww t Ivr h~;;; ital. Arrangements s.Juld be made for follow tit) tit t m 2 d;+y.- This is especially true if the infant isIS under 38 week-. oyxkAb17V) -F1ne C~nt1d I s 6tLaa"~'rZ2Clivv q I p~- ~~ (AV, ~ ftst,c tcutvrc For 14q~cfhillruY5tnwliu _ . , ( ' H _ a P T E : R 1i%N,:-?ratal Hy'perbilirubinemia
3. EJe '.'.ow obstruction (biliary atresia, extra hepatic or intrahepatic). The ex .-:..-z A t a : : . . , ~ a may be isolated or assc:iated with >! :dochal cyst, tris- - my 13 or 18, or polysplenia.The , intrahepari w. :+~sociated with t:-,e Alagiiie syndrome, intrahepatic atresi:+ u.:-in --ma (.kagenaes syndrome, nonsymdromic paucity of intrahepatic h:',- - d_:caprosutnie acidemia, choledochal cyst, bile duct stenosis, mptur,~ of hi'-- duct, lymph node enlargement, hemangiomas, tumors, pancreatic c_:st. in~pissated bile syndrome, and cystic fibrosis). 4. In the newborn intensive care unit, the most common causes of elevated CB, in decreasing order of f equency, are parenteral nutrition, idi -Pal hic hepatitis, biliary atresia, alpha-l-antitryTsin deiiciency, intrauterine infection, choledochal cyst, galaetosemia, and incre2sed bi)irubin I -, ad from hemolytic disc-se 13- Diagnostic tests and man-nPment 1. Evaluate for hepatomeeal, s; l~rorre;al_v. petechiae, chorioretinitis, and microcephaly 2. Evaluate liver damac.z a-. 4 ....n:ii;n by measurement of serum glutamic oxaloacetic transaminas- ~'SGOT) level, serum glutamic pyruvic transaminase (SGPT) lewl, alf.:+'.in? ph-phatase level, prothrombin time !PT), partial thrombopla:nn ti; - ,,e (F"I"f),and serum albumin level. 3_ Stop parenteral nutri'inn va ith amino acids. If this is the cause, the liver dysfunction will u;uaiiv resolve. 4. Test for bacterial. viral. and intrauterine infections i,ee Chap. 23)S. Serum analvsis for alpha-lantitrypsin deficiencv. 6_ Serum and urine amino acids determinations ( s e e Chap 29 1. 7. Urinalysis for gluco?e and reducing substances (se , Ch:ap_ 29 1 8. If known causes are ruled out, the problem is to diverentiace idinpathic neonatal hepatitis from h i l e duct abnormalities :'.:ch as intrahepatic hiliary atresia or hyp)pi-+sia. choledochal cyst. bile pluct sy:~wrne. extrahepatic biliary atresia, hvpoplasia, or total biliary atresia. a. Abdominal ultrasound should be done to rule out a choledochal c_c'~t or mass. b. We use a hepatobilian scan with technetium 169rn Tcjdiisopropylimin odiaceticfDISfDAI as the next sty to visualize the hiliarv tree. c. Iodine-131-rose hen:-;+l fecal excretion test ma_v be useful if the TcIDISIDA scan is not nvailabla. d- A nasoduodenal tul+e can he pa::.:ed and fluid collecUd in '= unliyuots lot 24 hours _ if there i~ nn hile. with plirn ! ~;""it;+l. 5 mhik! per day for 7 dav'a. and repent the dunurnal fluid e. [('the duod~.:al fluid collections. ;cxn:..rnc! ultrasound no extrahepatic obstruction. the child may be observed with f. If the ultrasound, scan;. or M14 Collections suggel~t ewr:ah~r;:'ic O b struction di,case, the baliv will need sin explrrrwtnrv lap;+r - wto^r.. chn!:mgiogram. and open liver luop.y to enable a definite dia;;v, -i< g. If the dia~ gnosis of extrahepatic obstruction disea.;e cannwt I- rul- d out, the babv must have the studir> mnlined_ hecause sure:^' , 'h, for chnledochal cyst, is curative if dunr earlc and impat++uurt-m_ tomv ha:, better rr:uits if'done , earl
N X!.
,
`!ydrops is :; term :acd to descnt>e ~ena; -+vlizvd w_hcutwuou~ cdema ir. ;he fetus or neonate- I[ i; usu:+llv accompanied Iw and often Im ylrnr<tl and/or pericardial effusions- Hvdrnp; fetalis is discus~~ed t -,cre, he-u< in the p:nst, hernolvtic disease e( Lire newbnrn V% :m tl+c' mnpr cau~e O f f)001 fet.+l ;rnd neonatal hvdrnps. Huww'er. ! xw':ru<c of' thi dorline m Iih ~rn-'ro.~nirnmune condition, are ~nnm the iv-)-r of h_vdrop< in th, United A. Etiology. The pathogenesis of hsdrnps includes anemia, cardiac failure. He creased colloid oncot.ic pressure (hs'poalbuminemia), increased capillary permeability, asphyxia, and placental perfusion abnormalities. There is a general. but not a constant, relationship between the degree of anen+ia. the serum albuNeonat-al Hpperbiiinrhinemia ci5
min level, and the presence of hydrops. There is no correlan,,n between the severity of hydmps and the blood volume of the infank Most hydropic infants have normal blood volume (80 :.:dllcg). 1. Hemato(ogic due to chronic in uwro anemia (10 - k of cases). Isoimmune hemolytic disease (e.g., Rh incompatibility), homozygous alpha thalassemia, homozygous GGPD deficiency, chronic fetomaternal hemorrhage, twin-totwin transfusion, hemorrhage, thrombosis, bone marro+c failure (c}tlor am;a enicol, maternal pawovirus infection), bone marrow ~ ,,placement (Gaucher's disease), leukemia. 2. Cardiovascular due to heart failure r20`%r of cases) (see Chap. 2a). ,- _~ Rhvthm disturbances. Heart 'noci:, supraventricular tachycardia, 2t^11 flutter. b. Majoreardiacdisease.Ily?opla=:i-i ,,t'theart,Epstein'sanomal},truncus arteriosus, myocarditis (rntsackieuia~, endocardial foroeiast.osis, cardiac neoplasm (rhabdomyonna'. cardiac thrombosis, arteriovenous ma', formations, premature clo~uri o; fi ramen ovale, generalized arterial calcification, premature re_:ruccara o; tire iveamen ovale. 3. Renal (5{ of cases). Nephro<v=. ccin thrombosis, renal hypopla; ia, urinarv obstruction. 4. Infection (8ck of cases). SyF~hilm. ru::ella, cytomegalovirus, congenital hepatitis, herpes virus, adenovirus. tc ~opl:-smosis,:eptospirosis,Charas' disease, parvoti'irus (see Chap 2:) 5_ Pulmonary (5`k of cases). Coagcwt._i chylothorax, diaphragmatic hernia, pulmonar - c lymp!:angiectasia, cystic adenomatoid malformations, intrat}uaracic mass. 6. ^::.canta or cord (rare cause). Ciutrang;oma, umbilical vein thrombosis, arter iovenous malformation, cheronic vein thrombosis, true knot in umbilical cord, cord compression, cftoriocarcinoma. 7. Maternal conditions (5`k of case- , ~ Toxemia, diabetes, thyrct,;sitsis. 8. Gastrointestinal (5^ of cases). Al<-cw,nurn peritonitis, in utero volvulus, - at.a 9. Chromosomal (lOk of cases)- Turner s_atrdrome; tr -isomv }:3, 18. '?1; triploidy; aneuploidy. 10- Miscellaneous (20% of cases). ystic hygroma. V'ilrr~; ' turnor, angioma, ier:atema. neuroblastoma, central neraoussastem W1~! nurl(onn.nioc-, anmiotic band syndrome, !-sosorval ~torari di~ ordars. cn ;y=enital mv_ otonic dvstrophy, skeletal abnorrnalii.cs tosu,yenesis irnp,rfercta, acf:-e drugcnesis, hypophospnatasia, thanatophoric dv+arf, artfmogrypr+~i~ i. Nocnan syndrome, acardia, absent ductus vvnosus, - renA venous thrombosis, cystic hyo oma. 11. Unknown (20`7 of cases). 9. Diagnosis. A pregnant woman with polyhydramnios, severe anemia, t,:: emia, or isoimmune disease should undergo ultrasonic examination of the f -Aus. If the fetus is hydropic, a careful search by ultrasound and real-time fetal echocardiography may reveal the cause and may guide fetal treatment. Tile accumulation of pericardial or a_citic fluid may he the first sign oC anpending hydrops in a Rh-sensitized fetus. Investigations should be carried out for the causes of fetal hydrops mentioned in A. The usual inve,ti gation includes the following: 1. Maternal blood type and Coombs' test as well as red cell aniFody titers, compleW blood count and red blood cell indices_ hemoglobin electrop?ooresis, tfemauser --Betke stain of maternal blood for 1e,al red cells, to for svplullis, studies tbr' viral infection and tosopla~tnoai> (~ec Chap_ -ia . -edimontation rate, lupus tests. 2. Fetal echocardiography for cardiac -abnormalities and ultrasound for w,her st.-uctural lesions. 3. Amniocentesis for karyot -ype, metabolic studies, fetoprot.ein, cultur<., and poymerase chain reaction tPCN1 for virai infections and restric;mn endonucleases as indicated.
216 CH.W'TEK I8 Neor.:atal Hyperbilirubinemia
4. Fetal blood sampling (PUBS) (see Chap. 1). ICarzwt_.a?. complete blood count (CBC), S. Neonatal. Following delivery, many of the same studies may be carried out on the infant. A
hemoglobin electrophoresis, culture" and YCR. DNA studies, albumin.
C. Management
complete blood count, bl--d typing, and Coombs' te-; ultrasound studies of the head, heart, and abdomen; and a search for the causes listed in XLA should be done. Examination of pleural and/or ascitic fluid, liver function tests, urinalysis, viral titers, chromosomes, placental examination, arid X rays may be indicated. If the infant is still born or dies, a detailed autopsy should be done.
1. A hydrapic fetus is at great risk for intrauterine death. A decision must be made about intray+A,~ine treatment if possible, for examp!e, fetal transfu sion in iso~^-::.iune hemolytic anemia (see Chap. 11 or maternal digitalis therap; ior supraventricwlar tachycardia (see Chap. 25). L` fetal treatment is not possible, the fWus must be evaluated for the relative possi4:!;y of intrauterine death versus the risks r'< premature delivery. If premature delivery is planned, pulmonary maturity should be rnducPd with steroids if it is not present (see Chap. 24). Intrauterine par< centesis or thoracenG:sis just prior to delivery ^nay facilitate subsequent newbom resuscitation. 2. Resuscitation of the hydropic infant is complex and requires advance preparation whenever feasible. Intubation can be extremely difflicult with massive edema of the head, neck, and oropharynx and should be done by a skilled operator immediately after birth. (A fiberoptic scope may facilitate placement of the endotrscheal tube.) A second individual should providc rapid relief of hydrostatic pressure on the diaphragm and lungs by parace.^.tesis and/or thoracentesis with an 18- to 20-gauge an,^i,-. atheter at tached to a - three-way stopcock and !zyringe. After entry into the chest or abdominal cavity, the needle is withdrawn so that the plastic catheter can remain without fear of laceration. Cardiocentesis may also be required if there is electromechanical owsociation due to cardiac tamponade. 3. Ventilator management can be complicated by pulmonary hyNuplasia, barotrauma, pulmonary edema, or reaccumulation of ascites and/or pleural fluid. If repeated thoracenteses cannot control hydrothoray, chest tube drainage"may be indicated-
Judicious use of diuretics (e.g-, furosemide) is often helpful in ruuuci; h putmonay edema. Arterial access is needed to rnonitor blond gases and acid-base balance. 4- Because hydropic infants have enormous quantitios of extravascutar salt and water, fluid intake is based on an e.,timate of the infant's "drv weight" (e.g., 80th percentile for gestationdl ae;c'. Free water salt are kept at a minimum (e.g., 40 ro 60 ml-.,'kg per da~ as dextrose water) until edema is . 'solved. Nlonitoring the electrolyte composition of serum, urine, ascites fluid, and/or pleural fluid, and careful measurement of intake, output, and weight are essential for guiding therapy. tiormoglycemia is achieved by providing glucose at a rate of 4 to 8 mg k ; per minute. Unless cardio vascular ana'3r renal function are compromised, edema will "ventually resolve and salt and water intake can then be normalized. S. If tae hematocrit is under 30%, a partial exchan 1 ge transfusion with i;Q to 30 ml/kg packed red blood cells (hern.aocrit 70% ) sh-31d be performed to raise the hematocrit and increase oxygen carrying capacity. If the problem i; Rv i--oimmuni2ation, the blood should be type O Rh-negative. We often use O-negative cells and Aii serum prepared before delivery and crossmatched against the other. An isovolumetric exchange (simultaneous removal of blood from the umbilical artery while blood is transfused in the umbilical vein at 2 to 4 mL.fkg per minute) may be better tolerated in infants with compromised cardiovascular systems. 6. Inotropic support (e.g., dopamine) may W iequired to improve cardiac output. Central venous and arterial lines are needed for monitoring pres sures_ Most hvdrooic infants are normovnlemic, but manipulation of the
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- KRITIKDokumen1 halamanKRITIKMike FandriBelum ada peringkat
- Get Up and Go Rawat JalanDokumen2 halamanGet Up and Go Rawat JalanMike FandriBelum ada peringkat
- Lamp IranDokumen1 halamanLamp IranMike FandriBelum ada peringkat
- Cover KELOMPOK 1 StuntingDokumen1 halamanCover KELOMPOK 1 StuntingMike FandriBelum ada peringkat
- The Mandala of HealthDokumen3 halamanThe Mandala of HealthMike FandriBelum ada peringkat
- Analisa Bivariat: Imunisasi Dasar Status Gizi CrosstabulationDokumen19 halamanAnalisa Bivariat: Imunisasi Dasar Status Gizi CrosstabulationMike FandriBelum ada peringkat
- 7Dokumen6 halaman7Mike FandriBelum ada peringkat
- FileDokumen2 halamanFileMike FandriBelum ada peringkat
- Allergic Contact DermatitisDokumen16 halamanAllergic Contact DermatitisMike FandriBelum ada peringkat
- 7Dokumen6 halaman7Mike FandriBelum ada peringkat
- FileDokumen2 halamanFileMike FandriBelum ada peringkat
- File 3Dokumen3 halamanFile 3Mike FandriBelum ada peringkat
- DBD Who 2011Dokumen212 halamanDBD Who 2011Mike FandriBelum ada peringkat
- Allergic Contact DermatitisDokumen16 halamanAllergic Contact DermatitisMike FandriBelum ada peringkat
- Allergic Contact DermatitisDokumen16 halamanAllergic Contact DermatitisMike FandriBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- 30947630Dokumen12 halaman30947630carolinapolotorresBelum ada peringkat
- Medical Marijuana PresentationDokumen19 halamanMedical Marijuana Presentationsudheer vamarajuBelum ada peringkat
- Cebu Institute of Technology University N. Bacalso Ave., Cebu City Philippines College of Nursing and Allied Health SciencesDokumen4 halamanCebu Institute of Technology University N. Bacalso Ave., Cebu City Philippines College of Nursing and Allied Health SciencesMikha BorcesBelum ada peringkat
- Nitrous Oxide in Emergency MedicineDokumen4 halamanNitrous Oxide in Emergency MedicinenumaidecatBelum ada peringkat
- International Journal of Surgery Case ReportsDokumen4 halamanInternational Journal of Surgery Case Reportshussein_faourBelum ada peringkat
- Coding TechniquesDokumen16 halamanCoding TechniquesShane BridgesBelum ada peringkat
- Final Past Papers With Common MCQS: MedicineDokumen17 halamanFinal Past Papers With Common MCQS: MedicineKasun PereraBelum ada peringkat
- 6mwt Protocol FinalDokumen7 halaman6mwt Protocol FinalSara Rodríguez SeoaneBelum ada peringkat
- The Mindbody Workbook - Mar 2013Dokumen7 halamanThe Mindbody Workbook - Mar 2013paul lukawski100% (6)
- Employee Enrollment Form - Texas: Allagadda Nageswara RaoDokumen5 halamanEmployee Enrollment Form - Texas: Allagadda Nageswara RaoNageswara Rao AllagaddaBelum ada peringkat
- Comfort Theory Kolcaba EnglishDokumen4 halamanComfort Theory Kolcaba EnglishRahayu SavitriBelum ada peringkat
- Audiology and Speech PathologyDokumen2 halamanAudiology and Speech PathologyErsya MusLih AnshoriBelum ada peringkat
- Stephanie Resume Updated 3-4-19Dokumen1 halamanStephanie Resume Updated 3-4-19StephBelum ada peringkat
- Pulmonary EmbolismDokumen27 halamanPulmonary EmbolismEfren Ezekiel AlbiosBelum ada peringkat
- Tracheostomy Suctioning and HumidificationDokumen5 halamanTracheostomy Suctioning and HumidificationLucila LugoBelum ada peringkat
- Donation After Cardiac Death 3Dokumen18 halamanDonation After Cardiac Death 3api-258141893Belum ada peringkat
- MEdical Surgical REVEWERDokumen86 halamanMEdical Surgical REVEWERennaedBelum ada peringkat
- ObGyn Clerkship Site PowerpointDokumen44 halamanObGyn Clerkship Site PowerpointAnthony ReynardBelum ada peringkat
- DR - Praful Zinzuwadia M.D.,D.ADokumen40 halamanDR - Praful Zinzuwadia M.D.,D.AprafulzinzuwadiaBelum ada peringkat
- Fluid Electrolytes and Acid Base BalanceDokumen108 halamanFluid Electrolytes and Acid Base BalancesayednourBelum ada peringkat
- Infectious Diseases Subspesialty Consult 2nd EdDokumen621 halamanInfectious Diseases Subspesialty Consult 2nd EdgadizaBelum ada peringkat
- HELLO! Magazine Laser Eye Surgery ArticleDokumen1 halamanHELLO! Magazine Laser Eye Surgery ArticleLondon Vision ClinicBelum ada peringkat
- 2016 Pediatric HydrocephalusDokumen15 halaman2016 Pediatric HydrocephalusYudit Arenita100% (1)
- Cefadroxil Journal ABSTRACTDokumen3 halamanCefadroxil Journal ABSTRACTAyu Kusuma NingrumBelum ada peringkat
- Sydney System For The Classification of Chronic GastritisDokumen8 halamanSydney System For The Classification of Chronic GastritisJuniorBelum ada peringkat
- Ivivi Technologies Case Study PDFDokumen2 halamanIvivi Technologies Case Study PDFsapiencecorpBelum ada peringkat
- Vascular EDSDokumen5 halamanVascular EDSMelissa MartinBelum ada peringkat
- Herniated Nucleus Pulposus (HNP)Dokumen4 halamanHerniated Nucleus Pulposus (HNP)Kevin CamilozaBelum ada peringkat
- NURS612 Exam 1 Review-Chen Walta - Week1-3Dokumen15 halamanNURS612 Exam 1 Review-Chen Walta - Week1-3A Marie100% (1)
- Morning Report KhodijahDokumen12 halamanMorning Report KhodijahMaria Jheny FulgensiaBelum ada peringkat