A Novel Technique For Attaining Maxillomandibular
Diunggah oleh
Si PuputJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
A Novel Technique For Attaining Maxillomandibular
Diunggah oleh
Si PuputHak Cipta:
Format Tersedia
7
A Novel Technique for Attaining Maxillomandibular Fixation in the Edentulous Mandible Fracture
Christopher Knotts, M.D. 1 Meredith Workman, M.D. 1 Kamal Sawan, M.D. 1 Christian El Amm, M.D. 1
1 Division of Plastic Surgery, University of Oklahoma Health Sciences
Center, Oklahoma City, Oklahoma Craniomaxillofac Trauma Reconstruction 2012;5:7 10
Address for correspondence and reprint requests Christopher Knotts, M.D., Division of Plastic Surgery, University of Oklahoma Health Sciences Center, 920 S.L. Young Blvd. Williams Pavillion #2210, P.O. Box 26901, Oklahoma City, OK 73104 (e-mail: christopher-knotts@ouhsc.edu).
Abstract
Keywords
MMF maxillomandibular xation mandible fracture edentulous spanning
Edentulous mandible fractures present a unique and challenging surgical problem, particularly because of lack of occlusive dental surfaces to capitalize upon maxillomandibular xation (MMF). We present a novel technique to achieve MMF using rigid plates spanning the oral cavity to xate the maxilla to the mandible. The process is rapid and allows stability using the established principles of rigidity, external xation, and osteosynthesis. This technique allows for a faster MMF than with a Gunning splint and allows for easier oral hygiene. An illustrative case and pre- and postoperative imaging are provided.
The edentulous mandible fracture presents a challenging and controversial clinical scenario for a multitude of reasons, the most obvious of which is the lack of occlusive dental surfaces to capitalize upon for manual fracture reduction and maxillomandibular xation (MMF). Further complicating the situation is an often severely atrophic mandible with poor vascularity. The rate of fracture nonunion is inversely proportional to the thickness of the atrophic segment.1 Rigid xation of these dif cult fractures can result in palpable plates and sometimes painful tting of dentures down the road. All of these problems are encountered in the setting of a frequently aged patient, with multiple comorbid conditions and higher anesthetic risks. Historically, these fractures were treated conservatively, but success with open reduction and internal xation of mandible fractures in general has led to a more aggressive approach with the edentulous mandible.2,3 Various open treatment strategies have been described, with no consensus regarding the best therapy.4 This is confounded by certain treatment modalities, namely external xation, having an increased rate of complications, though these modalities are often reserved for more severe injuries.5 Treatment of edentulous mandible fractures with plates beneath the periosteum, above the periosteum, and even atop the mucosal
surfaces have all been described.1,6 The treatment plan must be individualized depending on bone stock available, degree of comminution, availability of dentures, medical comorbidities including smoking, and patient preferences.7 Although the use of MMF is often cited in the literature, it is also controversial.8,9 Many novel ways of achieving xation have been described, including the traditional methods of arch bars or circumdental wires, Gunning splints, bone anchors, embrasure wires, orthodontic dental brackets, and cortical bone screws, among others.1013 We present a novel way of achieving MMF using rigid plates, xed to both the mandible and maxilla with screws, thus spanning the oral cavity.
Case Report
A 55-year-old woman presented to the trauma bay by helicopter from the scene of a single-vehicle rollover crash. Facial computed tomography scans showed a bilateral Lefort 2 fracture, a left mandibular body fracture measuring 17.5 mm in height, and a right subcondylar fracture (Fig. 1). The patients dentures were irreparably damaged in the accident, with most of the pieces missing entirely. She presented with a low albumin, multiple extremity orthopedic
received August 18, 2011 accepted after revision September 20, 2011 published online January 30, 2012
Copyright 2012 by Thieme Medical Publishers, Inc., 333 Seventh Avenue, New York, NY 10001, USA. Tel: +1(212) 584-4662.
DOI http://dx.doi.org/ 10.1055/s-0031-1300962. ISSN 1943-3875.
Spanning Maxillomandibular Fixation
Knotts et al.
Figure 1 Preoperative 3-D reconstruction of facial bones. Note the left angle fracture and loss of height in right ramus.
Figure 2 Postoperative 3-D reconstruction of facial bones. Note the spanning plates and correction of facial height. The left angle has also been repaired.
injuries, vertebral fractures, spleen injury, mediastinal hematoma, pulmonary contusions, sternal fracture, pelvic fractures, scapula fracture, multiple rib fractures, severe posttraumatic bruising, and edema of the oral gingiva and had a history of smoking. Given her polytrauma status, prolonged respiratory failure, dysphagia, and continued protein-wasting malnutrition, a tracheostomy and percutaneous endoscopic gastric tube were placed prior to fracture repair. Planned MMF did factor in to the decision for feeding tube and tracheostomy placement, though the decision was made in the global setting of preexisting malnutrition, prolonged respiratory failure, dysphagia, and the need for multiple surgical procedures. During fracture repair, each of the patients facial fractures was exposed followed by manual reduction. The left mandible body fracture was plated rst with a miniplate placed subperiostally, trying to capture as many of the comminuted segments as possible but realizing total rigid xation would not be achievable given the multiple bony fragments and the desire to minimize periosteal dissection. This plate was fashioned along Champys line of osteosynthesis. Next, fracture reduction was performed from superior to inferior by plating inferior orbital rims and midface buttresses with miniplates. Once the midface was stabilized, gentle traction was used to reduce the subcondylar fracture and estimate centric occlusion. The appropriate distance between maxilla and mandible was veri ed by measuring the occlusal relationship of the remains of denture fragments. The mandible and maxilla were xed together using 2.0 locking plates placed above the mucosa. These spanning plates were placed in a superoanterior vector to compensate for lack of rigid occlusion behind the left angle fracture (Fig. 2). Routine oral care including chlorhexidine and oral swabs was continued every 6 hours postoperatively. The
Craniomaxillofacial Trauma and Reconstruction Vol. 5 No. 1/2012
patient remained an inpatient and on continuous oxygen saturation monitoring with a screwdriver at the bedside while she was in MMF. The MMF plates were removed at the bedside after 3 weeks, and range of motion exercises began. Three months after surgery, the patient is healed with nontender fracture sites and no temporomandibular joint dysfunction and she is ready to be tted for dentures (Fig. 3).
Discussion
Rigid MMF can be achieved using plates and screws to allow for subcondylar healing and remodeling at appropriate bony height. Given the plates will leave the posterior occlusion un xed behind the angle fracture, certain measures must be taken to prevent torque on the fracture line by the masseter. These measures include placing the plates in a superoanterior vector and also plating the angle fracture along the line of osteosynthesis. This Luhr class III fracture was xed with a miniplate rather than with compression given the degree of comminution and our plan to also use MMF as an adjunct.1 We elected to use locking plates to allow the screw to engage the plate without crushing the xed gingiva beneath. This was done with the aid of a Freer elevator placed between the plate and gingiva. Given the degree of angulation alone, consideration was given to open reduction of the subcondylar fracture.14 However, this fracture was comminuted with intra-articular extension, and this nding, coupled with degree of brittleness found on dissection and reduction of the other facial fractures, led us to the decision to treat the fracture closed with reestablishment of vertical height using MMF.15 The trend toward expanding the indications for open treatment of subcondylar fractures is acknowledged, though repeat randomized and prospective studies have shown comparable
Spanning Maxillomandibular Fixation
Knotts et al.
Figure 3 Postoperative panoramic view after removal of spanning plates. Note evidence of bony union at left angle.
clinical results in both open and closed management of subcondylar fractures.14,16 The issue remains controversial and each patient must be approached individually. Our management strategy achieved an acceptable result with imaging-proven establishment of vertical height and no limitation of function. This technique is not suggested to be an absolute alternative to Gunning splints for closed management of subcondylar fractures, though it does have several advantages. The xation takes 5 to 10 minutes and is certainly quicker than open reduction of a subcondylar fracture, diminishing anesthetic time and operating time costs while also avoiding facial scarring. Hardware costs are higher with spanning MMF plates as two 4-hole plates and eight screws runs on the order of $950 and four rapid MMF screws would cost around $225 at our institution. Arch bars and wires would be even less expensive but take longer to apply. Given reduced operating time, we still believe spanning xation to be less expensive than open reduction. Oral care is simpli ed and visualization improved compared with burdensome splints or even arch bars. The preoperative preparation time of making impressions and splints is also avoided, though the potential role of a dental specialist should not be understated. In this case, the dentures were largely unrecoverable and the remains were sparse and in fragments. This coupled with contused and swollen gingiva did not allow repair of dentures and use as Gunning splints. However, consideration should be given to early involvement of dental specialists, especially in the setting of a partially edentulous patient, to allow precise placement of implants for functional long-term occlusion.17 There is a narrow subset of patients who will bene t from this novel approach, typically patients with another means of controlled airway who are edentulous and require rapid, short-term MMF, where Gunning splints are not an option. Although this approach is not used often given the narrow indications, it is certainly a useful tool to have in the armamentarium of a craniofacial surgeon. The spanning plates essentially function as an intraoral external xator and allow for absolute rigidity in the setting where dentures are not available and as an alternative to Gunning splints.
References
1 Luhr HG, Reidick T, Merten HA. Results of treatment of fractures of
3 4
10 11
12
13
14
the atrophic edentulous mandible by compression plating: a retrospective evaluation of 84 consecutive cases. J Oral Maxillofac Surg 1996;54;250254 Madsen MJ, Haug RH, Christensen BS, Aldridge E. Management of atrophic mandible fractures. Oral Maxillofac Surg Clin North Am 2009;21;175183, v Ellis E III, Price C. Treatment protocol for fractures of the atrophic mandible. J Oral Maxillofac Surg 2008;66;421435 Nasser M, Fedorowicz Z, Ebadifar A. Management of the fractured edentulous atrophic mandible. Cochrane Database Syst Rev 2007 (1):CD006087 Ellis E III, Muniz O, Anand K. Treatment considerations for comminuted mandibular fractures. J Oral Maxillofac Surg 2003;61;861 870 Wood GA, Campbell DF, Greene LE. Transmucosal xation of the fractured edentuous mandible. Int J Oral Maxillofac Surg 2011;40 (5):549552 Furr AM, Schweinfurth JM, May WL. Factors associated with longterm complications after repair of mandibular fractures. Laryngoscope 2006;116;427430 Bell RB, Wilson DM. Is the use of arch bars or interdental wire xation necessary for successful outcomes in the open reduction and internal xation of mandibular angle fractures? J Oral Maxillofac Surg 2008;66;21162122 Gear AJ, Apasova E, Schmitz JP, Schubert W. Treatment modalities for mandibular angle fractures. J Oral Maxillofac Surg 2005;63; 655663 Rinehart GC. Mandibulomaxillary xation with bone anchors and quick-release ligatures. J Craniofac Surg 1998;9;215221 Engelstad ME, Kelly P. Embrasure wires for intraoperative maxillomandibular xation are rapid and effective. J Oral Maxillofac Surg 2011;69;120124 Laurentjoye M, Majoufre-Lefebvre C, Siberchicot F, Ricard AS. Result of maxillomandibular xation using intraoral cortical bone screws for condylar fractures of the mandible. J Oral Maxillofac Surg 2009;67;767770 Utley DS, Utley JD, Koch RJ, Goode RL. Direct bonded orthodontic brackets for maxillomandibular xation. Laryngoscope 1998;108; 13381345 Schneider M, Erasmus F, Gerlach KL, et al. Open reduction and internal xation versus closed treatment and mandibulomaxillary xation of fractures of the mandibular condylar process: a randomized, prospective, multicenter study with special evaluation of fracture level. J Oral Maxillofac Surg 2008; 66;25372544
Craniomaxillofacial Trauma and Reconstruction
Vol. 5
No. 1/2012
10
Spanning Maxillomandibular Fixation
Knotts et al.
condylar neck fractures: a prospective, randomized clinical study. J Oral Maxillofac Surg 2010;68;12381241 17 Baker SB, Goldstein JA, Seiboth L, Weinzweig J. Posttraumatic maxillomandibular reconstruction: a treatment algorithm for the partially edentulous patient. J Craniofac Surg 2010;21; 217221
15 Zachariades N, Mezitis M, Mourouzis C, Papadakis D, Spanou A.
Fractures of the mandibular condyle: a review of 466 cases. Literature review, re ections on treatment and proposals. J Craniomaxillofac Surg 2006;34;421432 16 Danda AK, Muthusekhar MR, Narayanan V, Baig MF, Siddareddi A. Open versus closed treatment of unilateral subcondylar and
Craniomaxillofacial Trauma and Reconstruction
Vol. 5
No. 1/2012
Anda mungkin juga menyukai
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- INFOCUS MANUAL CATARACT SCREENINGF Primary-Eye-Care-Manual-Summary1Dokumen21 halamanINFOCUS MANUAL CATARACT SCREENINGF Primary-Eye-Care-Manual-Summary1Si PuputBelum ada peringkat
- Risk factors of diabetic retinopathy and vision threatening diabetic retinopathy and vision threatening diabetic retinopaty based on diabetic retinopathy screening program in greater bandung, west java.astriDokumen14 halamanRisk factors of diabetic retinopathy and vision threatening diabetic retinopathy and vision threatening diabetic retinopaty based on diabetic retinopathy screening program in greater bandung, west java.astriSi PuputBelum ada peringkat
- Eye Health in The Commonwealth - Progress Report 2018 To 2020Dokumen30 halamanEye Health in The Commonwealth - Progress Report 2018 To 2020Si PuputBelum ada peringkat
- Current Management of Vitreous Hemorrhage Due To Proliferative Diabetic RetinopathyDokumen11 halamanCurrent Management of Vitreous Hemorrhage Due To Proliferative Diabetic RetinopathySi PuputBelum ada peringkat
- Towards Universal Eye Health Western PacificDokumen28 halamanTowards Universal Eye Health Western PacificSi PuputBelum ada peringkat
- Normal Postnatal Ocular DevelopmentDokumen23 halamanNormal Postnatal Ocular DevelopmentSi PuputBelum ada peringkat
- Duty Report 18 Januari 2020Dokumen13 halamanDuty Report 18 Januari 2020Si PuputBelum ada peringkat
- Rapid Sequence InductionDokumen2 halamanRapid Sequence InductionSi PuputBelum ada peringkat
- New Doc 2018-05-04Dokumen2 halamanNew Doc 2018-05-04Si PuputBelum ada peringkat
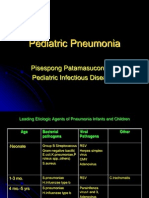
- Pediatric Pneumonia: Pisespong Patamasucon, M.D Pediatric Infectious DiseasesDokumen39 halamanPediatric Pneumonia: Pisespong Patamasucon, M.D Pediatric Infectious DiseasesSi PuputBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- US Army First Aid For Soldiers FM 21-11Dokumen243 halamanUS Army First Aid For Soldiers FM 21-11Total Prepper100% (2)
- 224 Closed Manipulation Casting of Distal Radius Fractures Fernandez DL 2005 Hand Clin p307-316 PDFDokumen10 halaman224 Closed Manipulation Casting of Distal Radius Fractures Fernandez DL 2005 Hand Clin p307-316 PDFanindyadputriBelum ada peringkat
- HAAD 100 Top Orthopaedics MCQ and AnswersDokumen18 halamanHAAD 100 Top Orthopaedics MCQ and AnswersAsif Newaz100% (3)
- Case Abstract Tibial FractureDokumen20 halamanCase Abstract Tibial FractureKceey CruzBelum ada peringkat
- CGHS Rate ListDokumen29 halamanCGHS Rate ListkkichaBelum ada peringkat
- Objective Questions For NursingDokumen53 halamanObjective Questions For NursingBIBI MOHANAN0% (1)
- Question OrthoDokumen4 halamanQuestion OrthoMohammed AbuzayedBelum ada peringkat
- Biology M10 Musculo-Skeletal SystemDokumen24 halamanBiology M10 Musculo-Skeletal SystemDiana Dealino-Sabandal100% (1)
- Musculoskeletal SystemDokumen22 halamanMusculoskeletal SystemKeyna DizonBelum ada peringkat
- Hip FractureDokumen4 halamanHip FractureJoel Vertt C. Balboa100% (1)
- Chapter 4 Surgery Musculoskeletal System CPT Codes 20000 - 29999Dokumen20 halamanChapter 4 Surgery Musculoskeletal System CPT Codes 20000 - 29999Rashiden MadjalesBelum ada peringkat
- POWEV2434234Dokumen461 halamanPOWEV2434234John M. HemsworthBelum ada peringkat
- Bryant's TractionDokumen2 halamanBryant's TractionGabbii CincoBelum ada peringkat
- 024344Dokumen6 halaman024344Aravind DesaiBelum ada peringkat
- Oet Reading 1 (A&b)Dokumen66 halamanOet Reading 1 (A&b)Richard James San JoseBelum ada peringkat
- Katalog Multiple Casualty Simulation KitDokumen1 halamanKatalog Multiple Casualty Simulation Kitwahyu sulistya affarahBelum ada peringkat
- First AidDokumen25 halamanFirst AidGaurav VermaBelum ada peringkat
- Basic of Manual TherapyDokumen30 halamanBasic of Manual Therapycamy bhagatBelum ada peringkat
- 3 Safety Device and Comfort MeasuresDokumen55 halaman3 Safety Device and Comfort MeasuresKaleb Ashiko100% (1)
- Orthopedic Radiographic in Exoctic Animal PracticeDokumen22 halamanOrthopedic Radiographic in Exoctic Animal PracticeHidaBelum ada peringkat
- n3021 Care Plan Week 2Dokumen7 halamann3021 Care Plan Week 2api-535585535Belum ada peringkat
- Fracture ManagementDokumen21 halamanFracture ManagementPatrickk WandererBelum ada peringkat
- TST D Scope Telescopic Nail EngDokumen28 halamanTST D Scope Telescopic Nail EngnorelBelum ada peringkat
- Sports Injuries: How Are Classified and Managed?Dokumen14 halamanSports Injuries: How Are Classified and Managed?Rachmat BayuBelum ada peringkat
- Helping Your Elbow To Recover After A Radial Head Fracture: Physiotherapy DepartmentDokumen8 halamanHelping Your Elbow To Recover After A Radial Head Fracture: Physiotherapy DepartmentJeongwoo PARKBelum ada peringkat
- Jdhodt 01 00025Dokumen6 halamanJdhodt 01 00025dithaBelum ada peringkat
- Bibliography of Orthopaedic Problems in Developing CountriesDokumen116 halamanBibliography of Orthopaedic Problems in Developing CountriesCristina IlieBelum ada peringkat
- AO Manual of Fracture Management - Internal Fixators, Thieme 2006-TLS (Michael Wagner)Dokumen889 halamanAO Manual of Fracture Management - Internal Fixators, Thieme 2006-TLS (Michael Wagner)Олексій ЮрченкоBelum ada peringkat
- PDF Khatri OdontoidFracturesDokumen65 halamanPDF Khatri OdontoidFracturesAlecsa Ana MariaBelum ada peringkat
- Rhombic 3D Condylar Fracture PlateDokumen8 halamanRhombic 3D Condylar Fracture PlateahujasurajBelum ada peringkat