Complications of Local and General Anesthesia
Diunggah oleh
Tarquin TomadaHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Complications of Local and General Anesthesia
Diunggah oleh
Tarquin TomadaHak Cipta:
Format Tersedia
Week Two: Complications of local and general anesthesia
1. Anaphylaxis- occurs to any anesthetic agent and in all types of anesthesia. The severity of the reaction may vary but features may include rash, urticaria, bronchospasm, hypotension, angioedema, and vomiting. It needs to be carefully looked for in the preoperative assessment and previous general anesthetic charts may help. 2. Aspiration pneumonitis- A reduced level of consciousness can lead to an unprotected airway. If the patient vomits they can aspirate the vomitus contents into their lungs. This can set up lung inflammation with infection. The risk of aspiration pneumonitis and aspiration pneumonia is reduced by fasting for several hours prior to the procedure and cricoid cartilage pressure during induction of anesthesia. However, the evidence for the use of cricoid pressure is not clearly documented and further investigation is required. 3. Peripheral nerve damage- occurs with all the types of anesthesia and results from nerve compression. The most common cause is exaggerated positioning for prolonged periods of time. Both the anesthetist and the surgeons should be aware of this potential complication and patients should be moved on a regular basis if possible. The severity varies and recovery may be prolonged. The most common nerves affected are the ulnar nerve and the common peroneal nerve. More rarely, the brachial plexus may be affected. 4. Damage to teeth- Damage to teeth is actually the most common cause of claims made against anesthetists. The tooth most commonly affected is the upper left incisor. 5. Embolism- rare during an anesthetic but is potentially fatal. Air embolism occurs more commonly during neurosurgical procedures or pelvic operations. Prophylaxis of thromboembolism is common and begins preoperatively with thromboembolic deterrents (TEDS) and low molecular weight heparin (LMWH). 6. Total spinal block- occurs with the injection of large amounts of anesthetic agents into the spinal cord. It is detected by a high sensory level and rapid muscle paralysis. The block moves up the spinal cord so that respiratory embarrassment may occur, as can unconsciousness. In these situations the patient needs prompt assessment and may need to be intubated and ventilated until the spinal block wears off. 7. Hypotension- up to half of patients receiving spinal anesthesia will develop transient hypotension as sympathetic nerves are blocked. This usually responds to prompt fluid replacement, usually starting with crystalloids followed by colloids. Occasionally hypotension can be severe and may require vasopressors along with fluids.
Anda mungkin juga menyukai
- Vocabulary BankDokumen2 halamanVocabulary BankTarquin TomadaBelum ada peringkat
- DMV 2016Dokumen116 halamanDMV 2016రణధీర్ గౌడ్Belum ada peringkat
- Herbal Medications (DOH)Dokumen2 halamanHerbal Medications (DOH)Tarquin TomadaBelum ada peringkat
- Pain Management Nursing RoleDokumen13 halamanPain Management Nursing Rolebacky_pzBelum ada peringkat
- IMCI Chart Booklet PDFDokumen80 halamanIMCI Chart Booklet PDFmikay100% (1)
- Fluid Balance ChartDokumen1 halamanFluid Balance ChartTarquin TomadaBelum ada peringkat
- Transient Tachypnea of The NewbornDokumen6 halamanTransient Tachypnea of The NewbornTarquin TomadaBelum ada peringkat
- Acls Aha 2010Dokumen67 halamanAcls Aha 2010heraaaaBelum ada peringkat
- Types of Therapy: Type of Therapy Objectives Materials Mechanics of TherapyDokumen3 halamanTypes of Therapy: Type of Therapy Objectives Materials Mechanics of TherapyTarquin TomadaBelum ada peringkat
- Health IssuesDokumen13 halamanHealth IssuesTarquin TomadaBelum ada peringkat
- Drug StudyDokumen3 halamanDrug StudyTarquin Tomada100% (2)
- Drug StudyDokumen4 halamanDrug StudyTarquin TomadaBelum ada peringkat
- Mindanao Sanitarium and Hospital College: School of NursingDokumen2 halamanMindanao Sanitarium and Hospital College: School of NursingTarquin TomadaBelum ada peringkat
- Death and DyingDokumen4 halamanDeath and DyingTarquin TomadaBelum ada peringkat
- Drug Study - PanitumumabDokumen2 halamanDrug Study - PanitumumabTarquin TomadaBelum ada peringkat
- Caring AidsDokumen9 halamanCaring AidsTarquin TomadaBelum ada peringkat
- Diversity and IndividualityDokumen2 halamanDiversity and IndividualityTarquin TomadaBelum ada peringkat
- Role and Responsibility of Director of NursingDokumen1 halamanRole and Responsibility of Director of NursingTarquin TomadaBelum ada peringkat
- Drug Study - IbuprofenDokumen2 halamanDrug Study - IbuprofenTarquin Tomada100% (1)
- Outline The Role of The Health Care AssistantDokumen13 halamanOutline The Role of The Health Care AssistantTarquin Tomada67% (3)
- Abdominal ExercisesDokumen2 halamanAbdominal ExercisesTarquin TomadaBelum ada peringkat
- Drug Study - IrinotecanDokumen2 halamanDrug Study - IrinotecanTarquin TomadaBelum ada peringkat
- 14 PrognosisDokumen1 halaman14 PrognosisTarquin TomadaBelum ada peringkat
- Drug Study - HydrocodoneDokumen2 halamanDrug Study - HydrocodoneTarquin Tomada86% (7)
- Drug Study - BevacizumabDokumen2 halamanDrug Study - BevacizumabTarquin TomadaBelum ada peringkat
- Care of The Elder Person: Evidence Based PracticeDokumen11 halamanCare of The Elder Person: Evidence Based PracticeTarquin TomadaBelum ada peringkat
- Drug Study - CetuximabDokumen2 halamanDrug Study - CetuximabTarquin TomadaBelum ada peringkat
- Drug Study - FolfoxDokumen3 halamanDrug Study - FolfoxTarquin TomadaBelum ada peringkat
- Drug Study - AcetaminophenDokumen1 halamanDrug Study - AcetaminophenTarquin TomadaBelum ada peringkat
- Gastrointestinal Tract AnatomyDokumen4 halamanGastrointestinal Tract AnatomyTarquin TomadaBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- VeinViewer® Innovation in VisualizationDokumen7 halamanVeinViewer® Innovation in VisualizationMikheilBelum ada peringkat
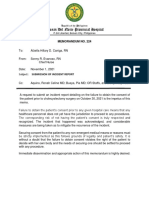
- Agusan Del Norte Provincial Hospital: Memorandum No. 224Dokumen2 halamanAgusan Del Norte Provincial Hospital: Memorandum No. 224Pia Mae BuayaBelum ada peringkat
- 2nd Announcement IHKS Event 2019 v3.1IDRDokumen32 halaman2nd Announcement IHKS Event 2019 v3.1IDRanon_370301325Belum ada peringkat
- Surgery RemediationDokumen14 halamanSurgery RemediationDrbee10Belum ada peringkat
- European COnsensus SDRDokumen19 halamanEuropean COnsensus SDRDiego DppBelum ada peringkat
- BLS ButuanDokumen4 halamanBLS ButuanHarbyBelum ada peringkat
- MAC Vs TIVADokumen2 halamanMAC Vs TIVARicky JalecoBelum ada peringkat
- Laparoscopic Appendectomy StudyDokumen12 halamanLaparoscopic Appendectomy StudypreetshardocBelum ada peringkat
- Toacs by ShireenDokumen244 halamanToacs by ShireenMuhammad Zeeshan100% (1)
- Endocarditis, Pericarditic, Myocarditis: TopicDokumen104 halamanEndocarditis, Pericarditic, Myocarditis: TopicOM VERMABelum ada peringkat
- Colonoscopy ProcedureDokumen2 halamanColonoscopy ProcedureNick Arngel CorporalBelum ada peringkat
- Front of Thigh NotesDokumen8 halamanFront of Thigh NotesMeowBelum ada peringkat
- Evaluasi Usg Dan Tatalaksana Pada Varises Vena Tungkai - DR RamziDokumen31 halamanEvaluasi Usg Dan Tatalaksana Pada Varises Vena Tungkai - DR RamziMohamad ZulfikarBelum ada peringkat
- Liver AbscessDokumen6 halamanLiver AbscessKenneth SunicoBelum ada peringkat
- Literature Review of Cosmetic Procedures in Men Approaches and Techniques Are Gender SpecificDokumen10 halamanLiterature Review of Cosmetic Procedures in Men Approaches and Techniques Are Gender SpecificImanuel Cristianto100% (1)
- ObturatorDokumen15 halamanObturatorFarhan Kabeer100% (1)
- Fundamentals of Pediatric Central Venous AccessDokumen38 halamanFundamentals of Pediatric Central Venous AccesssirrfsBelum ada peringkat
- JV Electrophysiology of HeartDokumen19 halamanJV Electrophysiology of HeartRiya GuptaBelum ada peringkat
- JurnalDokumen5 halamanJurnalJamila JuwitaBelum ada peringkat
- Pre and Post-Operative Care of Patient For Mastectomy: Prepared By: Gianne T. Gregorio RNDokumen13 halamanPre and Post-Operative Care of Patient For Mastectomy: Prepared By: Gianne T. Gregorio RNmalathiBelum ada peringkat
- Cardiopulmonary BypassDokumen42 halamanCardiopulmonary BypassСергей МатюшинBelum ada peringkat
- 9789386478122Dokumen15 halaman9789386478122ruacondungmanhBelum ada peringkat
- Star PackageDokumen24 halamanStar PackagePrsdeepBelum ada peringkat
- Intubasi SulitDokumen26 halamanIntubasi SulitfrostedsurgeonBelum ada peringkat
- Luka Bakar Poster PDFDokumen1 halamanLuka Bakar Poster PDFnurisumirizqiBelum ada peringkat
- Week 1 - Lecture NotesDokumen2 halamanWeek 1 - Lecture NotesAliceBelum ada peringkat
- Biomechanical Effects of Double or Wide Implants For Single Molar Replacement in The Posterior Mandibular RegionDokumen4 halamanBiomechanical Effects of Double or Wide Implants For Single Molar Replacement in The Posterior Mandibular RegiondwinugrohojuandaBelum ada peringkat
- Pterygium Ambreen ppt1Dokumen87 halamanPterygium Ambreen ppt1Syeda F AmbreenBelum ada peringkat
- Phakic Intraocular Lens Implantation Patient Leaflet April2017Dokumen11 halamanPhakic Intraocular Lens Implantation Patient Leaflet April2017Lilianty FauziBelum ada peringkat
- History of CRCDokumen26 halamanHistory of CRCFlaviu Ionuț FaurBelum ada peringkat