Australian Prescriber (1988) Bioavailability and First Past Clearance
Diunggah oleh
1234chocoHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Australian Prescriber (1988) Bioavailability and First Past Clearance
Diunggah oleh
1234chocoHak Cipta:
Format Tersedia
14
Australian Prescriber, Vol. 14, no. 1, 1991. Birkett, D. J. "Bioavailability and first pass clearance", pp. 14-16.
Double-Click icon for Copyright Notice Ausrraliun Prescriber Vol. I4 .Vo. 1 1991
BIOAVAILABILITY AND FIRST PASS CLEARANCE
D. J. Birkett, Professor of Clinical Pharmacology, Flinders University of South Australia, Adelaide
1. Getting the definitions straight As the terms absorption, first pass clearance, bioavailability and bioequivalence are often used loosely, we should first make sure of the definitions. Absorption: is the extent to which intact drug is absorbed from the gut lumen into the portal circulation. T h e factors affecting absorption are summarised in Table 1. First pass clearance: is the extent to which a drug is removed by the liver during its first passage in the portal blood through the liver to the systemic circulation. This is also called first pass metabolism or first pass extraction. Bioavailability: is the fraction of the dose which reaches the systemic circulation as intact drug. It is apparent that bioavailability will depend both o n how well
the drug is absorbed and how much escapes being removed by the liver before reaching the systemic circulation (Fig. 1).
bioavailability= fraction absorbed X (1 - extraction ratio) equation 1
Table I Determinants of drug absorption from the gut
where (1 - extraction ratio) is the fraction of drug escaping extraction by the liver. T h e fact that it is 1 - extraction ratio is important for bioavailability as will be seen below. Bioequivalence: is a clinical definition referring to two formulations of a drug. TWO formulations of the same drug are considered bioequivalent if the extents and rates of absorption of drug from them are so similar that there is likely to be no clinically important difference between their effects, either therapeutic or adverse. T h e clinical decision as to what would be a clinically important difference will vary from drug to drug. For example, small differences between formulations may be important for drugs such as digoxin which have low therapeutic ratios, or for drugs such as phenytoin which have non-linear kinetics. A larger difference may be tolerated for drugs such as amoxycillin which have high therapeutic ratios.
--
A. Dissolution physico-chemical properties of drug crystal size and form excipients special dosage forms (sustained release, enteric coated) pH (stomach and small intestine)
Fig. 1
Factors affecting bioavailability. In this example, 80 mg of the original 100 mg dose are absorbed intact into the portal circulation (fraction absorbed is 0.8). The hepatic extraction ratio is 0.75, so that 60 mg are extracted in the first pass through the liver and 20 mg escape extraction. The bioavailability (see equation 1) is fraction absorbed X (1 - extraction ratio) which is 0.8 X ( I - 0.75) = 0.2 (20%). jut lumen Portal circulation Liver Systematic circulation
B.
Gastric emptying rate stability of drug at acid pH solution or solid dosage forms (liquids and small particles empty more quickly) affected by: food; antacids; drugs (opiates, anticholinergics, metoclopramide); disease (autonomic neuropathy)
C. Intestinal motility dissolution of slowly soluble drugs (digoxin, sustained release formulations) chemical degradation or metabolism by rnicroflora affected by: drugs (opiates, anticholinergics, rnetoclopramide); disease states (gastroenteritis)
3rug in gut
Drug absorbed intact
Drug both absorbed intact and escaping first pass metabolism
D. Drug interactions in the gut lumen complexation (tetracyclines with divalent metal ions) adsorption (anion exchange resins) food interactions (many antibiotics) E. Passage through the gut wall physico-chemical characteristics of the drug (quaternary ammonium compounds) metabolism by enzymes in the intestinal endothelium
Drug extracted first pass
.4 usrrulian Prescriber Vol. I 4 .Vo. 1 1991
2. How is bioavailability measured?
Absolute bioavailability is measured against an intravenous reference dose (the bioavailability of an intravenous dose is 100% by definition). The usual method is to give a group of volunteers intravenous and oral doses of the drug on separate occasions. T h e areas under the plasma drug concentration versus time curves (AUC) after the two doses, are used to calculate the bioavailability of the oral formulation by simple proportion. For example, if the same intravenous and oral doses are given and the oral AUC is 50% of the intravenous AUC, the bioavailability of the oral formulation is 50%. T h e fact that the bioavailability is only 50% might be due to incomplete absorption, first pass clearance or a combination of these. Other methods which are used less frequently include comparing the urinary recoveries of drug or metabolite after intravenous and oral doses, or measuring the steady state plasma drug concentrations during intravenous and oral dosing. The bioavailability of one oral formulation is often assessed against a second oral (reference) formulation. This is referred to as measuring relative bioavailability, and is commonly done for new generic products where the reference formulation is the innovator's brand or the market leader formulation (brand) for that drug. It is called relative bioavailability as drug from both products could be subject to first pass clearance and this would not be detected. This type of study provides a measure of the relative performance of two formulations in getting drug absorbed.
3. What determines first pass clearance?
Thus for these drugs, hepatic enzyme activity is the major determinant of first pass metabolism and oral bioavailability, whereas hepatic blood flow is the major determinant of systemic clearance.
4. Why is first pass clearance important?
(i) Variability in drug response. As seen from Table 2, even small changes in the extraction of drugs such as verapamil can cause large changes in bioavailability. T h u s the plasma concentrations of such drugs after oral administration are more variable, both within and between individuals, than the plasma concentrations of drugs with close to complete bioavailability. (ii) Relationship between oral and intravenous doses. In example B in Table 2, only 10% of the oral dose reaches the systemic circulation as against, by definition, 100% of an intravenous dose. If there are no other complicating factors, the oral dose will therefore have to be 10 times the i n t r a v e n o u s d o s e to a c h i e v e s i m i l a r plasma concentrations and effects by the two routes of administration. For drugs with complete bioavailability, oral and intravenous doses are similar. (iii) Alternative routes of administration. Some drugs are so highly extracted by the liver that their oral bioavailability is negligible. Glyceryl trinitrate and ergotamine ark examples, both having first pass clearances of 99% or more and therefore oral bioavailabilities of less than 1% of the dose. Glyceryl trinitrate is administered by the sublingual route because the venous drainage from the mouth goes directly to the systemic circulation and first pass clearance by the liver is avoided. Percutaneous or transdermal administration of glyceryl trinitrate achieves the same result and also provides a slow, sustained delivery of drug. Part of the rectal circulation is systemic rather than portal, so rectal administration reduces first pass clearance. However, absorption of drugs from the rectum is often erratic and incomplete. Administration by inhalation can also be used for systemic
Let us now concentrate on first pass clearance and, for the moment, assume that all the drug is absorbed intact from the gut lumen into the portal circulation. T h e bioavailability then depends only on the fraction escaping first pass hepatic extraction as the fraction absorbed is 1.0 (see equation 1). Then,
bioavaiiabiiity = (1
- hepatic extraction ratio)
equation 2
The determinants of hepatic extraction ratio were considered in detail in the previous article (How drugs are cleared by the liver. Aust Prescr 1990;13:88-9). Let us take the same two limiting cases as previously, and look at the effects on bioavailability of increasing or decreasing the hepatic extraction ratio by changing the activity of the liver drug metabolising enzymes. Table 2 summarises these effects.
Table 2 Effects of increase or decrease in hepatic drug metabolising enzyme activity on bioavailability
Hepatic enzyme activity
% extracted first pass
Low hepatic extracrion ratio drugs In the case of drugs such as theophylline which are poorly extracted by the liver, nearly all the dose gets through the liver first pass and bioavailability is essentially complete as long as they are well absorbed from the gut. Even doubling or halving the minor proportion extracted by the liver does not make any significant difference to bioavailability (see Table 2). High hepatic extraction ratio drugs For drugs such asverapamil which are efficiently extracted by the liver, most of the dose is extracted on the first pass through the liver so that only a minor proportion reaches the systemic circulation intact (Table 2). Inducing or inhibiting the metabolising enzymes has only a small effect on hepatic extraction ratio, and thus on systemic clearance (see previous article Aust Prescr 1990;13:88-9), but has a major effect on the proportion escapinRextractiG (which is 1 .- extraction ratio), and thus has a-major effect on b i o a ~ a i l a b i l i(Table t~ 2).
Bioavailability (% escaping first pass extraction)
A. Low extraction ratio drug Normal Doubled (induced) Halved (inhibited)
2 4 1
98
96 99
B. High extraction ratio drug Normal 90 10 Doubled (induced) 95 5 Halved (inhibited) 83 17 All the dose is assumed to be absorbed intact from the gut lumen. The low extraction ratio example is characteristic of theophylline which has an intrinsic clearance (see previous article Aust Prescr 1990;13:88-9) of about 15 mL/min. The high extraction ratio example is characteristic of verapamil which has an intrinsic clearance of about 15 000 mL/min. Liver blood flow is normally around 1500 mL/min.
16
Ausrruliun Prescriber Val. 14 No. 1 1991
delivery without first pass clearance of some drugs (e.g. ergotamine). When drugs are used by inhalation for local effects on the lung, extensive first pass clearance can be a protective mechanism against systemic effects of the drug which is swallowed (often as much as 90% of the inhaled dose) rather than passing to the lungs. Examples are the beta-2 receptor agonist salbutamol and the inhaled corticosteroid beclomethasone. (iv) Drug interactions. As seen in Table 2, induction or inhibition of drug rnetabolising enzymes in the liver by other drugs or environmental agents such as cigarette smoke can cause large changes in the bioavailability of high, but not low, clearancedrugs. An example of this effect is shown in Fig. 2.
(v) Liver disease. In chronic liver disease, a substantial part of the portal circulation does not perfuse functional liver cells due to the presence of intrahepatic functional shunts or extrahepatic anatomic shunts. If 50% of the portal blood does not perfuse functioning liver cells, then 50% of first pass clearance will be avoided and bioavailability increased markedly. In example B in Table 2, bioavailability and effective dose would be increased from 10% to 55% (i.e. 5.5-fold) in this situation. Thus, high hepatic extraction drugs given to patients with liver disease are particularly liable to overdosing and causing a n increased incidence of adverse effects.
Fig. 2
Effect on felodipine bioavailability due to a drug interaction with anticonvulsants. tihealthy control subjects; 0 4 epileptic patients on liver enzyme inducing anticonvulsants. The relative oral bioavailability in epileptic patients was reduced to 6.6% of that in healthy control subjects. As the usual absolute oral bioavailability of felodipine (compared to an intravenous dose) is about 15%) only about 1% of an oral dose would be absorbed
intact in patients on enzyme inducing anticonvulsants. In this study, 10 out of 12 control subjects, but none of the epileptic patients, experienced vasodilator adverse effects. In 4 of the 10 epileptic patients, felodipine could not be detected in plasma. Adapted with permission from Lancet 1988;2481.
10
12
Time (hr)
Anda mungkin juga menyukai
- Pharmacokinetic & PharmacodynamicDokumen77 halamanPharmacokinetic & Pharmacodynamicdimasscrib100% (1)
- Altered Pharmacokinetics in Liver DiseasesDokumen30 halamanAltered Pharmacokinetics in Liver DiseasesNailaAns100% (1)
- Questions - Answer Bassam QQ 1Dokumen14 halamanQuestions - Answer Bassam QQ 1Bassam SaifBelum ada peringkat
- PharmacokineticsDokumen8 halamanPharmacokineticsPinay YaunBelum ada peringkat
- Drugs and Doping in SportDokumen39 halamanDrugs and Doping in SportAbhijit Sharma100% (1)
- Drug Interaction Can Be Defined As TheDokumen34 halamanDrug Interaction Can Be Defined As TheIstianah Es100% (1)
- Absorption of DrugsDokumen41 halamanAbsorption of DrugsSibtain100% (2)
- Preoperative AssessmentDokumen9 halamanPreoperative Assessment1234chocoBelum ada peringkat
- Bioavailability and First Pass MetabolismDokumen37 halamanBioavailability and First Pass MetabolismFitrye Yhana Rayyi KurniawanBelum ada peringkat
- Hydrophilic-Lipophilic BalanceDokumen56 halamanHydrophilic-Lipophilic Balancealanmarr100% (1)
- Katzung Chapter 3Dokumen2 halamanKatzung Chapter 3geldevera100% (1)
- نم هدمتعم و هعجارم اهنل اهب قوثوم لخادلاب تامولعملا Certified fromDokumen20 halamanنم هدمتعم و هعجارم اهنل اهب قوثوم لخادلاب تامولعملا Certified fromMedhat EyadaBelum ada peringkat
- Final PharmacologyDokumen284 halamanFinal PharmacologytrialqwBelum ada peringkat
- Pharmacology in Drug Discovery: Understanding Drug ResponseDari EverandPharmacology in Drug Discovery: Understanding Drug ResponseBelum ada peringkat
- Biopharmaceutics - BrahmankarDokumen414 halamanBiopharmaceutics - Brahmankarmatin586% (57)
- Principles of Pharmacology Chapter 1Dokumen37 halamanPrinciples of Pharmacology Chapter 1Muhammad ZakriaBelum ada peringkat
- BiopharmaceuticsDokumen52 halamanBiopharmaceuticsDharma ShantiniBelum ada peringkat
- Dosage and Solutions - FinalDokumen27 halamanDosage and Solutions - Finalramoli1988100% (1)
- Clinical PharmacologDokumen81 halamanClinical PharmacologSHILOTABelum ada peringkat
- Drug Metabolism in DiseasesDari EverandDrug Metabolism in DiseasesWen XieBelum ada peringkat
- Handbook of Drug Interaction and the Mechanism of InteractionDari EverandHandbook of Drug Interaction and the Mechanism of InteractionPenilaian: 1 dari 5 bintang1/5 (1)
- Pharmacology: Pharmacokinetic & Dose: Ana Khusnul Faizah Farmasi FK Uht 2018Dokumen27 halamanPharmacology: Pharmacokinetic & Dose: Ana Khusnul Faizah Farmasi FK Uht 2018Aulia rahmawatiBelum ada peringkat
- Abdullahi V Pfizer PaperDokumen2 halamanAbdullahi V Pfizer PaperTeam2KissBelum ada peringkat
- List of Indus of Pithampur ExcelDokumen32 halamanList of Indus of Pithampur ExcelWHATSAPP VIRAL & FUNNY COMEDY MAST WALE VIDEOS100% (1)
- Metabolism, Pharmacokinetics and Toxicity of Functional GroupsDokumen545 halamanMetabolism, Pharmacokinetics and Toxicity of Functional GroupsDenisa Nițu100% (1)
- Language of PreventionDokumen9 halamanLanguage of Prevention1234chocoBelum ada peringkat
- Bioavailability and First Pass ClearanceDokumen3 halamanBioavailability and First Pass ClearanceMergu Bala RajuBelum ada peringkat
- First Pass MetabolismDokumen8 halamanFirst Pass MetabolismMuhammad bilalBelum ada peringkat
- PharmacologyDokumen48 halamanPharmacologyRere Oslec100% (1)
- Assignment On Pharmacokinetic Drug Interaction: Teerthanker Mahaveer UniversityDokumen8 halamanAssignment On Pharmacokinetic Drug Interaction: Teerthanker Mahaveer Universityt24008882Belum ada peringkat
- M.Pharm (PH - Ceutics) : Presented byDokumen28 halamanM.Pharm (PH - Ceutics) : Presented byDipankar DasBelum ada peringkat
- Ayine Chap 4Dokumen59 halamanAyine Chap 4Abdi JifarBelum ada peringkat
- Assignment PharmaDokumen10 halamanAssignment Pharmac2bmqsfkp7Belum ada peringkat
- Ceutics CAT 2Dokumen9 halamanCeutics CAT 2Ria KitlerBelum ada peringkat
- Bioavailability: Clinical Research TrialsDokumen2 halamanBioavailability: Clinical Research TrialsRohan SawantBelum ada peringkat
- Makalah KBM Kel 3Dokumen32 halamanMakalah KBM Kel 3Novia RozadiBelum ada peringkat
- 3 - Pharmakcokinetics & Pharmacodynamics: Apparent VolumeDokumen10 halaman3 - Pharmakcokinetics & Pharmacodynamics: Apparent VolumexCadisRaiBelum ada peringkat
- Drug InteractionsDokumen43 halamanDrug InteractionsNinaBelum ada peringkat
- Pharmaco KineticsDokumen10 halamanPharmaco KineticsVithyaah ParameswaranBelum ada peringkat
- 03 - Principles of PharmacokineticsDokumen25 halaman03 - Principles of PharmacokineticsSimonBelum ada peringkat
- Basic Pharmacological Principles - WSAVA2011 - VINDokumen13 halamanBasic Pharmacological Principles - WSAVA2011 - VINMystry MailBelum ada peringkat
- General Pharmacology NotesDokumen76 halamanGeneral Pharmacology NotesXara Barretto Magadia100% (1)
- Trepanier2013 Applying Pharmacokinetics To Veterinary Clinical PracticeDokumen14 halamanTrepanier2013 Applying Pharmacokinetics To Veterinary Clinical PracticeSarahBelum ada peringkat
- Bioavailability - A Pharmaceutical ReviewDokumen17 halamanBioavailability - A Pharmaceutical Reviewraju155940550% (2)
- Pharmacokinetic and Pharmacodynamic2021Dokumen12 halamanPharmacokinetic and Pharmacodynamic2021STEFANIA AYA DIAZBelum ada peringkat
- Absorption WindowsDokumen9 halamanAbsorption WindowsFilip IlievskiBelum ada peringkat
- Select The Single Best Answer: A. BioavailabilityDokumen14 halamanSelect The Single Best Answer: A. BioavailabilityleahbayBelum ada peringkat
- A Dictionary of Terms Used in Drug MetabolismDokumen7 halamanA Dictionary of Terms Used in Drug MetabolismOksana KamenetskaBelum ada peringkat
- Research ArticleDokumen12 halamanResearch ArticleMary VegaBelum ada peringkat
- PDQ PharmaDokumen17 halamanPDQ PharmaRui PenedaBelum ada peringkat
- Facttors Affecting Drug MetabolismDokumen3 halamanFacttors Affecting Drug MetabolismAnanyaBelum ada peringkat
- Bio Case StudyDokumen20 halamanBio Case StudyMd. Nure Alamin SiddikBelum ada peringkat
- Biopharmaceutics KU (Maam Shaista)Dokumen13 halamanBiopharmaceutics KU (Maam Shaista)areebaBelum ada peringkat
- Farmacologia y Farmacocinetica NeonatalDokumen8 halamanFarmacologia y Farmacocinetica NeonatalRafael Flores PintoBelum ada peringkat
- Drug - Drug Int2Dokumen35 halamanDrug - Drug Int2alishba100% (2)
- College of Pharmacy Biopharmaceutics and Pharmacokinetics Assignment No. 1Dokumen6 halamanCollege of Pharmacy Biopharmaceutics and Pharmacokinetics Assignment No. 1ERIKA JADE TORRESBelum ada peringkat
- Pha 201 Lecture NoteDokumen10 halamanPha 201 Lecture NoteDebby14Belum ada peringkat
- Food Effects On Drug Bioavailability: Implications For New and Generic Drug DevelopmentDokumen19 halamanFood Effects On Drug Bioavailability: Implications For New and Generic Drug DevelopmentFanny MoralesBelum ada peringkat
- Pharmacology: Core Curriculum in NephrologyDokumen11 halamanPharmacology: Core Curriculum in NephrologyYuppie RajBelum ada peringkat
- Chapter 2Dokumen13 halamanChapter 2simbaiBelum ada peringkat
- Biopharmaceutics by John G. WagnerDokumen29 halamanBiopharmaceutics by John G. WagnerNick GanteBelum ada peringkat
- Review Article Dose-Dependent Pharmacokinetics: Experimental Observations and Theoretical ConsiderationsDokumen31 halamanReview Article Dose-Dependent Pharmacokinetics: Experimental Observations and Theoretical Considerationsירדן לויןBelum ada peringkat
- OkokosDokumen3 halamanOkokoskaulauBelum ada peringkat
- Pharmacokinetic: Herni SupraptiDokumen76 halamanPharmacokinetic: Herni SupraptiveniBelum ada peringkat
- Pharmacology- The Molecular Dance: Understanding Drug Interactions: Harmony and Chaos: The Symphony of Drug InteractionsDari EverandPharmacology- The Molecular Dance: Understanding Drug Interactions: Harmony and Chaos: The Symphony of Drug InteractionsBelum ada peringkat
- Presystemic Drug Elimination: Butterworths International Medical Reviews: Clinical Pharmacology and TherapeuticsDari EverandPresystemic Drug Elimination: Butterworths International Medical Reviews: Clinical Pharmacology and TherapeuticsCharles F. GeorgePenilaian: 1 dari 5 bintang1/5 (1)
- Translational ADMET for Drug Therapy: Principles, Methods, and Pharmaceutical ApplicationsDari EverandTranslational ADMET for Drug Therapy: Principles, Methods, and Pharmaceutical ApplicationsPenilaian: 1 dari 5 bintang1/5 (1)
- Fairy Tail - Main ThemeDokumen3 halamanFairy Tail - Main Theme1234chocoBelum ada peringkat
- Mbs Quick Guide: JULY 2020Dokumen2 halamanMbs Quick Guide: JULY 20201234chocoBelum ada peringkat
- Code Geass - StoriesDokumen5 halamanCode Geass - Stories1234chocoBelum ada peringkat
- Blue BirdDokumen7 halamanBlue Bird1234chocoBelum ada peringkat
- Doctor Talk: Communication Practice Role PlaysDokumen6 halamanDoctor Talk: Communication Practice Role Plays1234chocoBelum ada peringkat
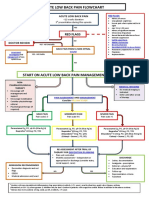
- Acute Low Back Pain Flowchart January 2017Dokumen1 halamanAcute Low Back Pain Flowchart January 20171234chocoBelum ada peringkat
- Topical Steroids (Sep 19) PDFDokumen7 halamanTopical Steroids (Sep 19) PDF1234chocoBelum ada peringkat
- Blue Card Declaration PDFDokumen1 halamanBlue Card Declaration PDF1234chocoBelum ada peringkat
- PBM Module1 MTP Template 0Dokumen2 halamanPBM Module1 MTP Template 01234chocoBelum ada peringkat
- Taking A Social and Cultural HistoryDokumen3 halamanTaking A Social and Cultural History1234chocoBelum ada peringkat
- Managing Mental Illness in Patients From CALD Backgrounds: PsychiatryDokumen5 halamanManaging Mental Illness in Patients From CALD Backgrounds: Psychiatry1234chocoBelum ada peringkat
- A Conceptual Framework For HealthDokumen1 halamanA Conceptual Framework For Health1234chocoBelum ada peringkat
- Acute Post-Op Pain ManagementDokumen4 halamanAcute Post-Op Pain Management1234chocoBelum ada peringkat
- Barrett's Esophagus: Identifying The Squamocolumnar (SC) and Gastroesophageal (GE) Junctions EndoscopicallyDokumen10 halamanBarrett's Esophagus: Identifying The Squamocolumnar (SC) and Gastroesophageal (GE) Junctions Endoscopically1234chocoBelum ada peringkat
- Prenatal Screening Test (AUS) PDFDokumen24 halamanPrenatal Screening Test (AUS) PDFshirley_ling_15Belum ada peringkat
- 1 PBDokumen3 halaman1 PBHaola andaniBelum ada peringkat
- Colchicine - General DataDokumen3 halamanColchicine - General DataCatalina BanuBelum ada peringkat
- 1.2.1.1 - Overview of Clinical Trials in Canada - Tanya Ramsamy - eDokumen25 halaman1.2.1.1 - Overview of Clinical Trials in Canada - Tanya Ramsamy - ecristofer BellidoBelum ada peringkat
- ReportDokumen21 halamanReportRenz CruzBelum ada peringkat
- Chemistry Is Important in MedicineDokumen6 halamanChemistry Is Important in MedicineKimberly A. S. Smith0% (1)
- Summary Plan Description Book 1 of 2 Plan U3Dokumen20 halamanSummary Plan Description Book 1 of 2 Plan U3Alfred IDunnoBelum ada peringkat
- (Analytical Profiles of Drug Substances 9) Klaus Florey (Eds.) - Academic Press (1981) PDFDokumen614 halaman(Analytical Profiles of Drug Substances 9) Klaus Florey (Eds.) - Academic Press (1981) PDFAstrid Carolina Gutierrez ShimabukuroBelum ada peringkat
- DESIGN, DEVELOPMENT AND IN-VITRO EVALUATION OF METOPROLOL TARTRATE FAST DISSOLVING TABLETS K. Ramesh Reddy, V. Jayasankar Reddy, G. Saisri Harsha, K.AnilDokumen8 halamanDESIGN, DEVELOPMENT AND IN-VITRO EVALUATION OF METOPROLOL TARTRATE FAST DISSOLVING TABLETS K. Ramesh Reddy, V. Jayasankar Reddy, G. Saisri Harsha, K.AniliajpsBelum ada peringkat
- Drug Metabolism & Pharmacokinetics in Drug Discovery: A Primer For Bioanalytical Chemists, Part IDokumen7 halamanDrug Metabolism & Pharmacokinetics in Drug Discovery: A Primer For Bioanalytical Chemists, Part IJoynalIslamKabirBelum ada peringkat
- DsDokumen9 halamanDsVavaxxxRemusaBelum ada peringkat
- Management of Cardiac ArrestDokumen10 halamanManagement of Cardiac ArrestAhmed VelićBelum ada peringkat
- Zidovudineinduced AnaemiaDokumen23 halamanZidovudineinduced AnaemiaSuresh ThanneruBelum ada peringkat
- Pharma Domain 101 - The Industry Lingo (Latest)Dokumen10 halamanPharma Domain 101 - The Industry Lingo (Latest)Ankit AgarwalBelum ada peringkat
- StorageDokumen2 halamanStorageShagorShagorBelum ada peringkat
- Skripsi KustaDokumen61 halamanSkripsi Kustaandre yuindartantoBelum ada peringkat
- Myasthenia GDokumen7 halamanMyasthenia GAcbel RnucoBelum ada peringkat
- Shaylyn Pady ResumeDokumen2 halamanShaylyn Pady Resumeapi-383927437Belum ada peringkat
- Research Journal of Pharmaceutical, Biological and Chemical SciencesDokumen5 halamanResearch Journal of Pharmaceutical, Biological and Chemical SciencesDessy Erlyani Mugita SariBelum ada peringkat
- Protein Binding of Drug: Page - 1 CMR College of Pharmacy, 2013Dokumen18 halamanProtein Binding of Drug: Page - 1 CMR College of Pharmacy, 2013REDDYGAARI ABBAYIBelum ada peringkat
- Introduction To Pharmaceutical Aerosols: D.D Moyo Pharmaceutical Technology 2011Dokumen34 halamanIntroduction To Pharmaceutical Aerosols: D.D Moyo Pharmaceutical Technology 2011valentine mhuteBelum ada peringkat
- Emulsifier For Personal CareDokumen5 halamanEmulsifier For Personal CareWaltoy DinizBelum ada peringkat
- ASSAY METHOD DEVELOPMENT AND VALIDATION FOR THE ESTIMATION OF SOLIFENACIN SUCCINATE IN TABLETS BY UV SPECTROPHOTOMETRY N.J.R. Hepsebah, A. Ashok KumarDokumen6 halamanASSAY METHOD DEVELOPMENT AND VALIDATION FOR THE ESTIMATION OF SOLIFENACIN SUCCINATE IN TABLETS BY UV SPECTROPHOTOMETRY N.J.R. Hepsebah, A. Ashok KumariajpsBelum ada peringkat
- Cosmetic Chemistry VocabularyDokumen2 halamanCosmetic Chemistry Vocabularyapi-266663713Belum ada peringkat
- Encube Corporate PresentationDokumen19 halamanEncube Corporate PresentationAnnu KambleBelum ada peringkat