Congestive Heart Failure
Diunggah oleh
E0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
751 tayangan4 halamanCongestive heart failure occurs when there is a malfunction in the pumping action of either the left ventricle, right ventricle or both. This pooling causes pulmonary congestion (fluid build-up in the lungs), reduced cardiac output, increased strain on the heart, reduced stroke volume, increased heart rate, and hypertrophy. Since blood is the oxygen / nutrient supply to the cells, the effects of CHF are systemic.
Deskripsi Asli:
Hak Cipta
© Attribution Non-Commercial (BY-NC)
Format Tersedia
DOC, PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniCongestive heart failure occurs when there is a malfunction in the pumping action of either the left ventricle, right ventricle or both. This pooling causes pulmonary congestion (fluid build-up in the lungs), reduced cardiac output, increased strain on the heart, reduced stroke volume, increased heart rate, and hypertrophy. Since blood is the oxygen / nutrient supply to the cells, the effects of CHF are systemic.
Hak Cipta:
Attribution Non-Commercial (BY-NC)
Format Tersedia
Unduh sebagai DOC, PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
751 tayangan4 halamanCongestive Heart Failure
Diunggah oleh
ECongestive heart failure occurs when there is a malfunction in the pumping action of either the left ventricle, right ventricle or both. This pooling causes pulmonary congestion (fluid build-up in the lungs), reduced cardiac output, increased strain on the heart, reduced stroke volume, increased heart rate, and hypertrophy. Since blood is the oxygen / nutrient supply to the cells, the effects of CHF are systemic.
Hak Cipta:
Attribution Non-Commercial (BY-NC)
Format Tersedia
Unduh sebagai DOC, PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 4
CHF 1
Running Head: CONGESTIVE HEART FAILURE
Congestive Heart Failure
Adrianne Bazo
Montana Tech Nursing Department
NURS 1566 Core Concepts of Adult Nursing
March 14, 2008
CHF 2
Noel Mathis RN, BSN, MSN
Congestive Heart Failure
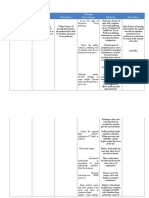
Congestive heart failure occurs when there is a malfunction in the
pumping action of either the left ventricle, right ventricle, or both
which causes blood to pool in the pulmonary arteries and/or veins.
This pooling causes pulmonary congestion (fluid build up in the lungs),
reduced cardiac output, increased strain on the heart, decreased
efficiency of the heart muscle contraction, reduced stroke volume,
increased heart rate, and hypertrophy; leading to increased risk of
cardiac arrest and a decreased blood supply to the rest of the body.
Since blood is the oxygen/nutrient supply to the cells, the effects of
CHF are systemic.
Risk factors for developing CHF are disorders that increase cardiac
workload and disorders that disrupt the pumping ability of the heart.
Examples of such diseases are, CAD, cardiomyopathy, acute
myocardial infarction, disease of the heart valves, fluid volume
overload hypertension, COPD, pulmonary hypertension, and anemia.
My patient had triple bypass surgery six years ago, so the cause of her
CHF is most likely from acute myocardial infarction.
The diagnosis of CHF is primarily made from a composite of patient
history, physical exam, laboratory studies, and radiographs. Lab
CHF 3
studies that indicate CHF are, low serum sodium and Hct from
hemodilution and inadequate oxygen levels in the arteries from poor
pulmonary perfusion. The effects of CHF cause reduced renal funciton
producing elevated blood urea nitrogen and creatinine levels.
The treatment of CHF is directed on decreasing the effects of the
underlying causes. Pharmaceuticals are used to decrease excess fluid
(diuretics), and improve cardiac output (ACE inhibitors, Beta-
adrenergic blockers, inotropics, and nitrates). Nonpharmaceutical
interventions to decrease cardiac workload and increase myocardial
oxygenation include intra-aortic balloon pump, ventricular assist
devices, and biventricular pacing. Also a diet low in sodium is
recommended.
My patient presents with peripheral edema, low SaO2 oxygenation,
rales heard in the lower 2/3 of the posterior lungs, shortness of
breath, low Hct (30.5), high total carbon dioxide, high Lactate
dehydrogenase (778), and high natriuretic peptide (823). Lactate
dehydrogenase and natriuretic peptide are indicators of tissue damage
and degree of heart failure.
CHF 4
Anda mungkin juga menyukai
- Congestive Heart Failure-ABDokumen3 halamanCongestive Heart Failure-ABEBelum ada peringkat
- ICCI PatofisiologíaDokumen10 halamanICCI PatofisiologíaAndrea Roman chavezBelum ada peringkat
- Heart FailureDokumen9 halamanHeart Failuregmqkxq6wshBelum ada peringkat
- Lec 3 Heart FailureDokumen25 halamanLec 3 Heart FailureDelete AccountBelum ada peringkat
- Nursing Management of Patient With CCFDokumen34 halamanNursing Management of Patient With CCFJayarani Ashok100% (1)
- Ehv 741Dokumen13 halamanEhv 741ErdaBelum ada peringkat
- Insuficiencia Cardiaca Congestiva IzquierdaDokumen10 halamanInsuficiencia Cardiaca Congestiva IzquierdaCindy Karina Carbajal MurilloBelum ada peringkat
- Chronic Heart FailureDokumen11 halamanChronic Heart FailurelaydyBelum ada peringkat
- Medicine in Brief: Name the Disease in Haiku, Tanka and ArtDari EverandMedicine in Brief: Name the Disease in Haiku, Tanka and ArtPenilaian: 5 dari 5 bintang5/5 (1)
- Cardiovascular DisordersDokumen38 halamanCardiovascular Disordersmark100% (4)
- Braunwald Lecture Series #2Dokumen33 halamanBraunwald Lecture Series #2usfcards100% (2)
- Case 2 SlosDokumen7 halamanCase 2 SlosNamarBelum ada peringkat
- Nur 111 Session 7 Sas 1Dokumen8 halamanNur 111 Session 7 Sas 1Zzimply Tri Sha UmaliBelum ada peringkat
- Current Strategies For The Prehospital Care of Congestive Heart FailureDokumen8 halamanCurrent Strategies For The Prehospital Care of Congestive Heart FailureAmy Milligan MillerBelum ada peringkat
- Proyecto de Investigación Del Sistema CardiovascularDokumen3 halamanProyecto de Investigación Del Sistema CardiovascularNatalia quirogaBelum ada peringkat
- Heart Failure in ChildrenDokumen44 halamanHeart Failure in ChildrenRisna Ariani100% (2)
- LP CHFDokumen15 halamanLP CHFimunisasi bonyelBelum ada peringkat
- Failure in Infants and Children: HeartDokumen9 halamanFailure in Infants and Children: HeartAzizatul AuliaBelum ada peringkat
- Pharmacology II Sovan Sarkar 186012111012Dokumen14 halamanPharmacology II Sovan Sarkar 186012111012Sovan SarkarBelum ada peringkat
- CHF Blok KardiovaskularDokumen39 halamanCHF Blok KardiovaskularAnonymous Cz5xlxyU9VBelum ada peringkat
- Manage Cardiac EmergenciesDokumen56 halamanManage Cardiac Emergencies21rayhanf100% (1)
- Cardiac Failure: Dr. Abdul Ghani WaseemDokumen33 halamanCardiac Failure: Dr. Abdul Ghani WaseemFarwaBelum ada peringkat
- HF DeaDokumen53 halamanHF DeaSyifa Mahmud Syukran AkbarBelum ada peringkat
- Congestive Heart Failure (CHF) Is The Inability of The Heartto Pump ADokumen3 halamanCongestive Heart Failure (CHF) Is The Inability of The Heartto Pump AAbdulla Abu EidBelum ada peringkat
- Signs and SymptomsDokumen16 halamanSigns and SymptomsRose AnnBelum ada peringkat
- Tugass Paper BryanDokumen10 halamanTugass Paper BryanMauritius BryanBelum ada peringkat
- Hypertension: Hypertension Is One of The Most Common Worldwide Diseases Afflicting Humans. BecauseDokumen8 halamanHypertension: Hypertension Is One of The Most Common Worldwide Diseases Afflicting Humans. BecauseKramojBelum ada peringkat
- Systolic Dysfunction:: Types of Heart FailureDokumen13 halamanSystolic Dysfunction:: Types of Heart FailureElisabeth F. OjhaBelum ada peringkat
- Cardio CHFDokumen18 halamanCardio CHFHajime NakaegawaBelum ada peringkat
- Cardiac FailureDokumen7 halamanCardiac FailureCasuga, Jessica Carmela F.Belum ada peringkat
- In Partial Fulfillment of The Requirements in Medical Ward RotationDokumen5 halamanIn Partial Fulfillment of The Requirements in Medical Ward RotationEiz CabreraBelum ada peringkat
- Congestive Heart Failure: Diagnosis, Pathophysiology, Therapy, and Implications For Respiratory CareDokumen10 halamanCongestive Heart Failure: Diagnosis, Pathophysiology, Therapy, and Implications For Respiratory CareIntan PurnamasariBelum ada peringkat
- Congestive Cardiac Failure Causes, Symptoms & TreatmentDokumen24 halamanCongestive Cardiac Failure Causes, Symptoms & TreatmentFarheen KhanBelum ada peringkat
- Acute Heart FailureDokumen18 halamanAcute Heart FailureGeorge GeorgeBelum ada peringkat
- Congestive Heart FailureDokumen6 halamanCongestive Heart Failureseigelystic100% (1)
- Mitchell 2005Dokumen8 halamanMitchell 2005DianBelum ada peringkat
- Heart Failure and ShockDokumen34 halamanHeart Failure and Shockfrenee aradanasBelum ada peringkat
- Heart FailureDokumen39 halamanHeart FailureMuhammad AsifBelum ada peringkat
- Unit 2 Heart Failure: StructureDokumen29 halamanUnit 2 Heart Failure: StructurebtaleraBelum ada peringkat
- KP 2.5.5.1 Gagal Jantung KronikDokumen39 halamanKP 2.5.5.1 Gagal Jantung Kronikayam kecapBelum ada peringkat
- Heart Failure: Departemen Kardiologi FK USU RSUP. H. Adam Malik MedanDokumen42 halamanHeart Failure: Departemen Kardiologi FK USU RSUP. H. Adam Malik Medanbilli lisanuddinBelum ada peringkat
- Heart Failure IntroductionDokumen12 halamanHeart Failure IntroductionJasper VictoryBelum ada peringkat
- Cardiovascular Dysfunction in ChildrenDokumen15 halamanCardiovascular Dysfunction in ChildrenJhasseryne Orias SanchezBelum ada peringkat
- Neurohormonal Activation in Heart FailureDokumen4 halamanNeurohormonal Activation in Heart Failurekunalprabhu148Belum ada peringkat
- Congestive Heart Failure PDFDokumen11 halamanCongestive Heart Failure PDFpriyanka bhavsarBelum ada peringkat
- HTTPS://WWW - Tvsmotor.com/iqube?utm Source Quora&utm Medium Paid&utm Campaign Quora Postlaunch Pratical ECDokumen21 halamanHTTPS://WWW - Tvsmotor.com/iqube?utm Source Quora&utm Medium Paid&utm Campaign Quora Postlaunch Pratical ECAjithBelum ada peringkat
- Decreased Cardiac OutputDokumen3 halamanDecreased Cardiac OutputCristina L. JaysonBelum ada peringkat
- Acute Biologic CrisisDokumen60 halamanAcute Biologic Crisisraidis100% (4)
- Congestive Heart Failure ReportDokumen6 halamanCongestive Heart Failure ReportSunshine_Bacla_4275100% (1)
- CHFDokumen10 halamanCHFPowpOw SangalangBelum ada peringkat
- CHF PathophysiologyDokumen4 halamanCHF PathophysiologyVirtudazo JessaBelum ada peringkat
- HF Case Analysis: Signs, Symptoms, and TypesDokumen14 halamanHF Case Analysis: Signs, Symptoms, and TypesBrix ValdrizBelum ada peringkat
- Heart Failure in ChildrenDokumen47 halamanHeart Failure in ChildrenDr.P.NatarajanBelum ada peringkat
- Academic Year 2021-2022 2nd Year S-3: Cardiovascular ModuleDokumen66 halamanAcademic Year 2021-2022 2nd Year S-3: Cardiovascular Moduleحسن ميري ناصر حسونBelum ada peringkat
- Congestive Heart Failure: Elias S. (MD+) March 2015 DBUDokumen35 halamanCongestive Heart Failure: Elias S. (MD+) March 2015 DBUkikiBelum ada peringkat
- Hypertension Guide - Causes, Treatment & ManagementDokumen4 halamanHypertension Guide - Causes, Treatment & ManagementMarisol AaronsBelum ada peringkat
- Heart Failure Nursing Care Management - A Study GuideDokumen16 halamanHeart Failure Nursing Care Management - A Study GuideJOSHUA DICHOSOBelum ada peringkat
- Pyelonephritis 1 Running Head: PYELONEPHRITISDokumen4 halamanPyelonephritis 1 Running Head: PYELONEPHRITISEBelum ada peringkat
- Left-Side CHF PathoDokumen5 halamanLeft-Side CHF PathoEBelum ada peringkat
- Bowel Resection PathoDokumen7 halamanBowel Resection PathoEBelum ada peringkat
- Pneumonia Short PathoDokumen2 halamanPneumonia Short PathoEBelum ada peringkat
- Influenza B PathoDokumen4 halamanInfluenza B PathoEBelum ada peringkat
- Autonomic DysreflexiaDokumen2 halamanAutonomic DysreflexiaEBelum ada peringkat
- Hyperparathyroidism PathoDokumen2 halamanHyperparathyroidism PathoEBelum ada peringkat
- Iron Deficiency Anemia PathoDokumen6 halamanIron Deficiency Anemia PathoEBelum ada peringkat
- Hyponatremic Dehydration PathoDokumen4 halamanHyponatremic Dehydration PathoEBelum ada peringkat
- Chemical Burns PathoDokumen2 halamanChemical Burns PathoEBelum ada peringkat
- Acute Pancreatitis PathoDokumen5 halamanAcute Pancreatitis PathoEBelum ada peringkat
- Pancreatitis Short PathoDokumen2 halamanPancreatitis Short PathoEBelum ada peringkat
- Subluxation c6c7 Short PathoDokumen1 halamanSubluxation c6c7 Short PathoEBelum ada peringkat
- Buspar (Buspirone)Dokumen1 halamanBuspar (Buspirone)EBelum ada peringkat
- Campral (Acamprosate Calcium)Dokumen1 halamanCampral (Acamprosate Calcium)E100% (1)
- Geodon (Ziprasidone)Dokumen2 halamanGeodon (Ziprasidone)EBelum ada peringkat
- Clinical Medications Worksheets: (Why Med Ordered) Contraindications/warnings/interactionsDokumen1 halamanClinical Medications Worksheets: (Why Med Ordered) Contraindications/warnings/interactionsEBelum ada peringkat
- Prozac (Fluoxetine) 40mgDokumen1 halamanProzac (Fluoxetine) 40mgEBelum ada peringkat
- Zosyn (Piperacillin/tazobactram)Dokumen2 halamanZosyn (Piperacillin/tazobactram)E67% (3)
- FiberCon (Polycarbophil)Dokumen1 halamanFiberCon (Polycarbophil)EBelum ada peringkat
- Silvadene (Silver Sulfadiazine)Dokumen1 halamanSilvadene (Silver Sulfadiazine)EBelum ada peringkat
- ZofranDokumen1 halamanZofranKatie McPeek0% (1)
- Darvocet (Propoxyphene Napsylate/Acetaminophen)Dokumen1 halamanDarvocet (Propoxyphene Napsylate/Acetaminophen)EBelum ada peringkat
- Theragran (Multiple Vitamins)Dokumen3 halamanTheragran (Multiple Vitamins)EBelum ada peringkat
- Reglan (Metoclopramide)Dokumen3 halamanReglan (Metoclopramide)E100% (1)
- Lexapro (Escitalopram Oxalate)Dokumen2 halamanLexapro (Escitalopram Oxalate)EBelum ada peringkat
- Florinef (Fludrocortisone)Dokumen3 halamanFlorinef (Fludrocortisone)E100% (1)
- Keppra (Levetiracetam)Dokumen2 halamanKeppra (Levetiracetam)E100% (1)
- DIAGNOSI PENYAKIT VASKULARDokumen73 halamanDIAGNOSI PENYAKIT VASKULARRudy SimamoraBelum ada peringkat
- Scorebuilders Cardiac ReviewDokumen16 halamanScorebuilders Cardiac Reviewboogie33100% (1)
- Cardiovascular System AnatomyDokumen13 halamanCardiovascular System AnatomyDwi Junita SariBelum ada peringkat
- 6th Basic Course of Paediatric EchocardiographyDokumen9 halaman6th Basic Course of Paediatric Echocardiographyajes coolBelum ada peringkat
- Full Download Test Bank For Ecgs Made Easy 5th Edition Aehlert PDF Full ChapterDokumen36 halamanFull Download Test Bank For Ecgs Made Easy 5th Edition Aehlert PDF Full Chapteradrianblackiadxetkrqm100% (14)
- Flash Pulmonary EdemaDokumen11 halamanFlash Pulmonary EdemaEda SopBelum ada peringkat
- Cardiorespiratory Endurance: in This Chapter Student Web ResourcesDokumen9 halamanCardiorespiratory Endurance: in This Chapter Student Web ResourcesFRANCO PANUGALINGBelum ada peringkat
- 3D Printing Applications for Heart Tissue RegenerationDokumen16 halaman3D Printing Applications for Heart Tissue RegenerationSkzAznBelum ada peringkat
- Vastarel MR From Decades of Clinical Experience inDokumen6 halamanVastarel MR From Decades of Clinical Experience inJonathan Ian ArinsolBelum ada peringkat
- Science 9 Module 1 Quarter 1 The Human Circulatory and Respiratory SystemDokumen23 halamanScience 9 Module 1 Quarter 1 The Human Circulatory and Respiratory SystemMaricel PenaBelum ada peringkat
- Cardiac Conduction System: Origin and Propagation of Electrical ImpulsesDokumen36 halamanCardiac Conduction System: Origin and Propagation of Electrical ImpulsesAtchaya ThillainatarajanBelum ada peringkat
- Introduction to Anatomy and Skin StructureDokumen6 halamanIntroduction to Anatomy and Skin Structurescort cherBelum ada peringkat
- Cardiac CTDokumen7 halamanCardiac CTdaniel7pintiliiBelum ada peringkat
- Cardiac Cycle & Heart Sounds Flashcards - QuizletDokumen11 halamanCardiac Cycle & Heart Sounds Flashcards - QuizletRadijska Postaja KoprivnicaBelum ada peringkat
- Access Vascular FOR Hemodialysis: Dr. Sahal Fatah, SP - BTKVDokumen28 halamanAccess Vascular FOR Hemodialysis: Dr. Sahal Fatah, SP - BTKVAnonymous wVgEAr6Belum ada peringkat
- 2021 AHA ASA Guideline For The Prevention of Stroke in Patients With Stroke and TIA Clinical UpdateDokumen43 halaman2021 AHA ASA Guideline For The Prevention of Stroke in Patients With Stroke and TIA Clinical UpdateKadek Aditya Darma YogaBelum ada peringkat
- Lecture 15 Cardiovascular DiseaseDokumen19 halamanLecture 15 Cardiovascular DiseaseHHGV JGYGUBelum ada peringkat
- Solution Manual For Medical Nutrition Therapy A Case Study Approach 5th EditionDokumen8 halamanSolution Manual For Medical Nutrition Therapy A Case Study Approach 5th EditionMichaelArchermtyg100% (36)
- Clinical Suspicion of Left Ventricular Apical Thrombus - What To Do?: A Case ReportDokumen11 halamanClinical Suspicion of Left Ventricular Apical Thrombus - What To Do?: A Case ReportIJAR JOURNALBelum ada peringkat
- Abdominal Aortic Aneurysm and Atherosclerosis FINALDokumen23 halamanAbdominal Aortic Aneurysm and Atherosclerosis FINALErica P. ManlunasBelum ada peringkat
- Cardiovascular SystemDokumen293 halamanCardiovascular SystemVictor StevenBelum ada peringkat
- Anatomy - Physiology (Chapter 12 - Heart)Dokumen20 halamanAnatomy - Physiology (Chapter 12 - Heart)Avi ZychBelum ada peringkat
- Head and Neck Blood Supply and DrainageDokumen11 halamanHead and Neck Blood Supply and DrainageHisham ChomanyBelum ada peringkat
- Diabetic Macrovascular DiseaseDokumen31 halamanDiabetic Macrovascular DiseaseArina ChifulescuBelum ada peringkat
- Cues Nursing Diagnosis Objectives Nursing Interventions Rationale EvaluationDokumen3 halamanCues Nursing Diagnosis Objectives Nursing Interventions Rationale EvaluationHarvey Lampa SelimBelum ada peringkat
- 2017 ESC Guidelines For The Management of Acute Myocardial Infarction in Patients Presenting With ST Segment ElevationDokumen66 halaman2017 ESC Guidelines For The Management of Acute Myocardial Infarction in Patients Presenting With ST Segment ElevationMoises Torres AlvarezBelum ada peringkat
- Atrial Fibrillation: Racheal James Heart Rhythm Specialist Nurse UHWDokumen37 halamanAtrial Fibrillation: Racheal James Heart Rhythm Specialist Nurse UHWAman ChaudharyBelum ada peringkat
- Manage Cardiac Output in Hyperthyroid PatientDokumen3 halamanManage Cardiac Output in Hyperthyroid PatientPrincess QuirinaBelum ada peringkat
- Practice Exams - CardiovascularDokumen19 halamanPractice Exams - CardiovascularpadialmichelleBelum ada peringkat
- Pex 05 01Dokumen5 halamanPex 05 01Wijoyo KusumoBelum ada peringkat