ARB Delays Microalbuminuria in Diabetes
Diunggah oleh
César EscalanteDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
ARB Delays Microalbuminuria in Diabetes
Diunggah oleh
César EscalanteHak Cipta:
Format Tersedia
T R A N S L A T I N G
R E S E A R C H
T O
P R A C T I C E
Angiotensin Receptor Blocker to Prevent Microalbuminuria?
Reviewed by John R. White, Jr. STUDY Haller H, Ito S, Izzo JL Jr, Januszewicz A, Katayama S, Menne J, Mimran A, Rabelink TJ, Ritz E, Ruilope LM, Rump LC, Viberti G, for the ROADMAP Trial Investigators: Olmesartan for delay or prevention of microalbuminuria in type 2 diabetes. N Engl J Med 364:907917, 2011 SUMMARY Objective. Microalbuminuria is a predictor of cardiovascular disease (CVD), as well as diabetes-related nephropathy. This study was designed to determine whether the occurrence of microalbuminuria could be prevented or delayed in patients with type 2 diabetes with the angiotensin receptor blocker (ARB) olmesartan. Design and methods. This study was a randomized, multicenter, double-blind, controlled trial of 4,447 patients with type 2 diabetes. The patients were 1875 years of age and had normoalbuminuria at the onset of the trial. They were randomized to receive either placebo or olmesartan, 40 mg daily, for a median of 3.2 years. During the trial, patients were treated to a blood pressure of < 130/90 mmHg using conventional antihypertensive medications (excluding ACE inhibitors, ARBs, or aldosterone blockers except for the ARB olmesartan in the active treatment group). Patients who had used ACE inhibitors or ARBs during the 6-month period leading up to the study were excluded. Blood pressure was measured with an automated device at each follow-up visit. The blood pressure value used was the mean of three measurements taken at 3-minute intervals by an automated device. The primary outcome was the elapsed time until the initial onset of microalbuminuria. Urine was tested by validated measurements of morning spot urine samples. Microalbuminuria was described in this trial as a urinary albumin (mg) to creatinine (g) ratio of > 35 in women or > 25 in men. Any new abnormal albumin-to-creatinine ratio was confirmed by another positive result (out of two tests) within 2 weeks of the initial abnormal finding. Patients with confirmed positive findings were assigned to an open-label arm of the study and were treated with olmesartan, 40 mg daily. Secondary endpoints were 1) a composite of cardiovascular complications, 2) death from cardiovascular causes, and 3) renal events. The median follow-up period in this trial was 3.2 years. The mean A1C level was 7.7%, and the mean duration of diabetes was 6.1 years. Of the patients enrolled in this trial, 67.7% had four cardiovascular risk factors, and > 97% had at least two risk factors in addition to diabetes. Results. Blood pressure: Mean blood pressure during the follow-up period was 128.7/76.2 and 125.7/74.3 mmHg in the placebo and treatment arms, respectively. Approximately 80% of the patients in the treatment arm and 71% of those in the placebo arm achieved a target blood pressure (< 130/90 mmHg) at 48 months. Primary outcome: In the olmesartan group, 178 of 2,160 patients (8.2%) developed microalbuminuria, compared to 210 of 2,139 patients (9.8%) in the placebo group during the double-blind period of the trial. Median time to onset of microalbuminuria was 722 days in the olmesartan group and 576 days in the placebo group. The time to onset of microalbuminuria (the primary endpoint) was increased by 23% in the olmesartan group (hazard ratio [HR] of onset of microalbuminuria 0.77, 95% confidence interval [CI] 0.630.94, P = 0.01). The HR after adjustment for small baseline differences in BMI, systolic blood pressure, and levels of HDL cholesterol and triglycerides was similar at 0.75 (95% CI 0.620.92, P = 0.006). Secondary endpoints: A slightly greater reduction in mean glomerular filtration rate was reported in the olmesartan group (from 85 to 80.1 ml/min/1.73 m 2) versus the placebo group (from 84.7 to 83.7 ml/min/1.73 m 2). This difference was statistically significant (P < 0.001 for betweengroup change from baseline). A doubling of serum creatinine was reported in 23 patients (~ 1%) in each group. End-stage renal disease (ESRD) did not develop in any of the patients in either group. The proportion of patients reaching the composite endpoint of death
20
Volume 30, Number 1, 2012 CLINICAL DIABETES
T R A N S L A T I N G
R E S E A R C H
T O
P R A C T I C E
from cardiovascular causes or cardiac complications was similar in the two groups: 4.3% in the olmesartan group and 4.2% in the placebo group. Mortality rates from any cause were 1.2% (26 deaths) in the olmesartan group and 0.7% (15 deaths) in the placebo group (P = 0.10). However, the number of deaths from cardiovascular causes alone was statistically significantly higher in the olmesartan group than in the placebo group (15 vs. 3 deaths in the olmesartan and placebo groups, respectively; P = 0.01). These deaths were primarily the result of higher rates of myocardial infarction (MI; 5 vs. 0) and sudden cardiac death (7 vs. 1) in the olmesartan group compared to the placebo group. Adverse events: Overall, the number of adverse events was similar in the two groups. Serious events were reported in 15.2% of the placebo group and in 15% of the olmesartan group. A statistically significant difference was reported in drugrelated adverse events (11.4% in the olmesartan group vs. 7.5% in the placebo group, P < 0.001). These differences were primarily caused by much higher rates of hypotension (58 vs. 6, P < 0.001) and dizziness (103 vs. 61, P = 0.001) in the olmesartan group compared to the placebo group. The number of withdrawals from the study because of symptomatic hypotension was greater in the olmesartan group (n = 10) than in the placebo group (n = 1). Conclusion. The researchers concluded that this trial suggests that olmesartan increases the time to onset of microalbuminuria in patients with type 2 diabetes, even under conditions of excellent blood pressure control. COMMENTARY The question being evaluated in this study is important. Should we preemptively treat patients with type
2 diabetes with an ARB to delay the appearance of microalbuminuria? The obvious implication is that, if we can delay the initial appearance of microalbuminuria, then perhaps we can delay or circumvent the progression to ESRD. Taking this logic a step further, perhaps this type of pharmacological modality might also be associated with an improvement in cardiovascular outcome. This second step, although seemingly logical, is based on the potentially flawed assumption that if we treat one of the markers of CVD (microalbuminuria), the complication itself will be assuaged. Thus far in other studies, it has been quite difficult to tease out the impact of blood pressure reduction from the impact of microalbuminuria reduction from the impact of other pleiotropic effects of renin/angiotensin modulation on CVD. However, the HOPE (Heart Outcomes Prevention Evaluation) study and its Micro-HOPE substudy did demonstrate that the ACE inhibitor ramipril was associated with a reduction in CVD outcomes MI, stroke, and death in patients with diabetes.1 Diabetes-related nephropathy occurs in 2040% of patients with diabetes and is the leading cause of ESRD.2 Persistent microalbuminuria has been shown to be a marker for the development of nephropathy in patients with type 2 disease. Additionally, microalbuminuria is well established as a marker for CVD risk.3 It is clear that inhibition of the renin-angiotensin system (RAS) is useful in slowing down the progression of nephropathy in patients with demonstrable microalbuminuria. If fact, the American Diabetes Association (ADA) is clear in recommending the use of RAS inhibition (with converting enzyme inhibitors or ARBs) in non-preg-
nant type 2 diabetic patients with microalbuminuria.2 The BENEDICT study4 reported that the use of the ACE inhibitor trandolapril in hypertensive, normoalbuminuric patients with type 2 diabetes was associated with a reduction in the development of diabetic nephropathy. The study also demonstrated that this effect was not enhanced by the addition of a nondihydropyridine calcium channel antagonist. It has been demonstrated that ARBs can reduce the rate of progression from microalbuminuria to macroalbuminuria and to ESRD in patients with type 2 diabetes,57 hence the ADA recommendations mentioned above. However, one ARB, candesartan, was not shown to have a protective effect against the initial development of microalbuminuria in normotensive normoalbuminuric patients with type 2 diabetes.8 Although this study did demonstrate that the use of the ARB olmesartan was associated with delay in the onset of microalbuminuria in patients with type 2 diabetes, the effect was modest (mean difference was < 5 months). Additionally, the statistically significant number of deaths from cardiovascular causes in the olmesartan arm, although possibly due to chance, is reason for concern. At this juncture, it would be premature to recommend an ARB for prevention of microalbuminuria in normotensive patients with type 2 diabetes. The most prudent and beneficial course is to attend to patients glycemic and blood pressure control while continuing annual screening for microalbuminuria and treating microalbuminuria if it develops with an ACE inhibitor or an ARB.
CLINICAL DIABETES Volume 30, Number 1, 2012
21
T R A N S L A T I N G
R E S E A R C H
T O
P R A C T I C E
REFERENCES
1 Heart Outcomes Prevention Evaluation Study Investigators: Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. Lancet 355:253259, 2000 2 American Diabetes Association: Standards of medical care in diabetes2011. Diabetes Care 34 (Suppl. 1):S11S61, 2011 3 Garg JP, Bakris GL: Microalbuminuria: marker of vascular dysfunction, risk factor for cardiovascular disease. Vasc Med 7:3543, 2002
disease in type 2 diabetes: the BENEDICT study. J Am Soc Nephrol 17:S90S97, 2006
5 Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA, Lewis JB, Ritz E, Atkins RC, Rohde R, Raz I; Collaborative Study Group: Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med 345:851860, 2001 6 Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, Remuzzi G, Snapinn SM, Zhang Z, Shahinfar; SRENAAL Study Investigators: Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 345:861869, 2001 7 Parving HH, Lehnert H, BrchnerMortensen J, Gomis R, Andersen S, Arner P; Irbesartan in Patients with Type 2 Diabetes
and Microalbuminuria Study Group: The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med 345:870878, 2001
8 Bilous R, Chaturvedi N, Sjlie AK, Fuller J, Klein R, Orchard T, Porta M, Parving HH: Effect of candesartan on microalbuminuria and albumin excretion rate in diabetes: three randomized trials. Ann Intern Med 151:1114, 2009
Remuzzi G, Macia M, Ruggenenti P: Prevention and treatment of diabetic renal
John R. White, Jr., PA, PharmD, is the interim chairman and a professor of pharmacotherapy at Washington State University in Spokane. He is a deputy editor of Clinical Diabetes.
22
Volume 30, Number 1, 2012 CLINICAL DIABETES
Anda mungkin juga menyukai
- X. Tillin 2011 DT2Dokumen6 halamanX. Tillin 2011 DT2Juan Carlos FloresBelum ada peringkat
- Blood Pressure Management in Patients With Diabetes: Clinical Trial Evidence For BP ControlDokumen8 halamanBlood Pressure Management in Patients With Diabetes: Clinical Trial Evidence For BP ControlNovita WulandariBelum ada peringkat
- Empagliflozin in Prevention of Cardiovascular Disease Among Patients With Diabetes Mellitus Type 2Dokumen4 halamanEmpagliflozin in Prevention of Cardiovascular Disease Among Patients With Diabetes Mellitus Type 2tb9Belum ada peringkat
- Jurnal 1Dokumen17 halamanJurnal 1convenienceBelum ada peringkat
- DM Nefro3Dokumen10 halamanDM Nefro3Teddy Alexander MorinBelum ada peringkat
- 593 Full PDFDokumen11 halaman593 Full PDFsalman672003Belum ada peringkat
- Management of Diabetes Mellitus in Patients With Chronic Kidney DiseaseDokumen9 halamanManagement of Diabetes Mellitus in Patients With Chronic Kidney DiseasezakyBelum ada peringkat
- UKPDS 39 compares atenolol and captoprilDokumen8 halamanUKPDS 39 compares atenolol and captoprilLaila MayangsariBelum ada peringkat
- MatsutaniDokumen12 halamanMatsutanigarry.soloanBelum ada peringkat
- Prevalence of Microalbuminuria Among Sudanese Type 2 Diabetic Patients at Elmusbah Center at Ombadda - OmdurmanDokumen5 halamanPrevalence of Microalbuminuria Among Sudanese Type 2 Diabetic Patients at Elmusbah Center at Ombadda - OmdurmanIOSR Journal of PharmacyBelum ada peringkat
- Screening and Diagnosis: of DiabeticDokumen3 halamanScreening and Diagnosis: of DiabeticFanyshaa VeshaapuetriBelum ada peringkat
- Association of Blood Pressure Control and Metabolic Syndrome With Cardiovascular Risk in Elderly Japanese: JATOS StudyDokumen7 halamanAssociation of Blood Pressure Control and Metabolic Syndrome With Cardiovascular Risk in Elderly Japanese: JATOS StudyRobertoBelum ada peringkat
- Diabetic Nephropathy: Landmark Clinical TrialsDokumen45 halamanDiabetic Nephropathy: Landmark Clinical TrialsTRP TSYOBelum ada peringkat
- Patient Information Handout: Am Fam PhysicianDokumen5 halamanPatient Information Handout: Am Fam PhysicianJacky Lou Tabamo LumacadBelum ada peringkat
- 2018-10-31 Final Research Paper MPI CAD Vs HBA1CDokumen12 halaman2018-10-31 Final Research Paper MPI CAD Vs HBA1Cbilly medinaBelum ada peringkat
- AURORA: Is There A Role For Statin Therapy in Dialysis Patients?Dokumen4 halamanAURORA: Is There A Role For Statin Therapy in Dialysis Patients?Ravan WidiBelum ada peringkat
- Do Angiotensin Converting Enzyme Inhibitors or Angiotensin Receptor Blockers Prevent Diabetes Mellitus? A Meta-AnalysisDokumen9 halamanDo Angiotensin Converting Enzyme Inhibitors or Angiotensin Receptor Blockers Prevent Diabetes Mellitus? A Meta-AnalysisURSULA LAZOBelum ada peringkat
- The Pathological Effects of Hyperglycaemia On The Cardiovascular (CV) System and BrainDokumen5 halamanThe Pathological Effects of Hyperglycaemia On The Cardiovascular (CV) System and BrainRyzka Izza MayFanyBelum ada peringkat
- DM To CKDDokumen12 halamanDM To CKDMuhamad Ansori BastianBelum ada peringkat
- DR. Butar Butar - Diabetic Kidney Disease How To Regress (PIT MAKASAR, 23-26 Nov 06)Dokumen42 halamanDR. Butar Butar - Diabetic Kidney Disease How To Regress (PIT MAKASAR, 23-26 Nov 06)Didi RaufBelum ada peringkat
- UKPDS Study Shows Benefits of Lowering Blood Glucose and Blood Pressure in Type 2 DiabetesDokumen5 halamanUKPDS Study Shows Benefits of Lowering Blood Glucose and Blood Pressure in Type 2 DiabetesAgustin MendezBelum ada peringkat
- Hypoglycaemia Documented With Real-Time Continuous Glucose Sensing in A Case of Dead in Bed' SyndromeDokumen106 halamanHypoglycaemia Documented With Real-Time Continuous Glucose Sensing in A Case of Dead in Bed' Syndromemimran1974Belum ada peringkat
- Hypoglycemia: Table 1Dokumen8 halamanHypoglycemia: Table 1erik1585Belum ada peringkat
- Diagnosis and Treatment of Diabetic Nephropathy in Type 1 and Type 2 Diabetes Patients 2155 9929 1000295Dokumen4 halamanDiagnosis and Treatment of Diabetic Nephropathy in Type 1 and Type 2 Diabetes Patients 2155 9929 1000295Hening Tirta KusumawardaniBelum ada peringkat
- Insulin Therapy in The Inpatient and Outpatient SettingDokumen83 halamanInsulin Therapy in The Inpatient and Outpatient SettingFriedman Diabetes Institute100% (1)
- Intensive BloodDokumen2 halamanIntensive BloodHyderBelum ada peringkat
- Optimal Dose of Candesartan For Renoprotection in Type 2 Diabetic Patients With NephropathyDokumen6 halamanOptimal Dose of Candesartan For Renoprotection in Type 2 Diabetic Patients With NephropathyNanaDinaWahyuniBelum ada peringkat
- Journal Club Preventing Left Ventricular Hypertrophy by ACE Inhibition inDokumen33 halamanJournal Club Preventing Left Ventricular Hypertrophy by ACE Inhibition inTiruvalavan Sokkadu RajanBelum ada peringkat
- Diabetesupdate PDFDokumen7 halamanDiabetesupdate PDFAndhika Jaya SaputraBelum ada peringkat
- AntiDokumen10 halamanAntiSebastián PonceBelum ada peringkat
- Lipid and Inflammatory Biomarkers and Kidney Function Decline in Type 2 DiabetesDokumen5 halamanLipid and Inflammatory Biomarkers and Kidney Function Decline in Type 2 Diabetesannaafia69969Belum ada peringkat
- Hypertension in Diabetes: Treatment Considerations: Review PaperDokumen5 halamanHypertension in Diabetes: Treatment Considerations: Review Paperdivina_grace08Belum ada peringkat
- EMPA REG OUTCOME The Cardiologist S Point 2017 The American Journal of MedDokumen6 halamanEMPA REG OUTCOME The Cardiologist S Point 2017 The American Journal of MedAlina PopaBelum ada peringkat
- Hyperfibrinogenemia Predicts Vascular Risk in DiabetesDokumen6 halamanHyperfibrinogenemia Predicts Vascular Risk in DiabetesHeru MurdiantoBelum ada peringkat
- Atorvastatin in Patients With Type 2 Diabetes Mellitus Undergoing HemodialysisDokumen11 halamanAtorvastatin in Patients With Type 2 Diabetes Mellitus Undergoing HemodialysisJerryEddyaPutraBoerBelum ada peringkat
- Nejmoa 021778Dokumen11 halamanNejmoa 021778aandakuBelum ada peringkat
- Phco 23 15 1564 31963Dokumen9 halamanPhco 23 15 1564 31963كسلان اكتب اسميBelum ada peringkat
- 27 FullDokumen6 halaman27 FullKrishna R KhanalBelum ada peringkat
- Perspective: Management of Hypertension in Patients With Type 2 Diabetes Mellitus: Guidelines Based On Current EvidenceDokumen6 halamanPerspective: Management of Hypertension in Patients With Type 2 Diabetes Mellitus: Guidelines Based On Current EvidencethaihavttBelum ada peringkat
- Examine Nejmoa1305889Dokumen9 halamanExamine Nejmoa1305889Griselda MoraBelum ada peringkat
- DerosaDokumen13 halamanDerosaAmeliana KamaludinBelum ada peringkat
- A Pilot Study On The Effect of Telmisartan & Ramipril On 24 H Blood Pressure Profile & Dipping Pattern in Type 1 Diabetes Patients With NephropathyDokumen6 halamanA Pilot Study On The Effect of Telmisartan & Ramipril On 24 H Blood Pressure Profile & Dipping Pattern in Type 1 Diabetes Patients With Nephropathydini hanifaBelum ada peringkat
- Terjemahan JurnalDokumen13 halamanTerjemahan JurnalIqhe Harsono SyastrowinotoBelum ada peringkat
- Accord StudyDokumen2 halamanAccord StudyCarlos Danilo Noroña CBelum ada peringkat
- UKPDS36Dokumen8 halamanUKPDS36Siskawati SuparminBelum ada peringkat
- tmpFF74 TMPDokumen2 halamantmpFF74 TMPFrontiersBelum ada peringkat
- Blood Pressure Management in Patients With DiabetesDokumen8 halamanBlood Pressure Management in Patients With DiabetesHoài ThươngBelum ada peringkat
- Evaluation of Telmisartan-Amlodipine combo for hypertensionDokumen13 halamanEvaluation of Telmisartan-Amlodipine combo for hypertensionMelanie BirthaharaBelum ada peringkat
- Blood Pressure TTR Predicts Cardiovascular Outcomes in DiabetesDokumen3 halamanBlood Pressure TTR Predicts Cardiovascular Outcomes in DiabetesGiorgi PopiashviliBelum ada peringkat
- 24614-Article Text-88446-1-10-20150819 PDFDokumen4 halaman24614-Article Text-88446-1-10-20150819 PDFNoor OsamaBelum ada peringkat
- Myocardial Infarction in Diabetic Vs Non-Diabetic SubjectsDokumen10 halamanMyocardial Infarction in Diabetic Vs Non-Diabetic SubjectsAji Prima PutraBelum ada peringkat
- Polypharmacy in The Aging Patient A Review of Glycemic Control in Older Adults With Type 2 DiabetesDokumen12 halamanPolypharmacy in The Aging Patient A Review of Glycemic Control in Older Adults With Type 2 Diabetesapi-311409998Belum ada peringkat
- ADA - UKPD StudyDokumen5 halamanADA - UKPD StudyMagdalena MercyanaBelum ada peringkat
- Managing Diabetes ComplicationsDokumen35 halamanManaging Diabetes ComplicationsironBelum ada peringkat
- EMPA-REG OUTCOME: The Endocrinologist 'S Point of View: Clinical Research StudyDokumen6 halamanEMPA-REG OUTCOME: The Endocrinologist 'S Point of View: Clinical Research StudyAlina PopaBelum ada peringkat
- Hypoglycemia - 2014 Morales N DoronDokumen8 halamanHypoglycemia - 2014 Morales N DoronDian Eka RamadhaniBelum ada peringkat
- PP Lancet 1998 Ukpds33Dokumen17 halamanPP Lancet 1998 Ukpds33HelloBelum ada peringkat
- Ni Hmsdasads 34581Dokumen11 halamanNi Hmsdasads 34581Joe AjaBelum ada peringkat
- Liraglutide and Cardiovascular Outcomes in Type 2 DiabetesDokumen17 halamanLiraglutide and Cardiovascular Outcomes in Type 2 DiabetesCésar EscalanteBelum ada peringkat
- The Physiology of Endocrine Systems With AgeingDokumen24 halamanThe Physiology of Endocrine Systems With AgeingCésar EscalanteBelum ada peringkat
- Five Elements Tai Chi Chuan Theory In-DepthDokumen10 halamanFive Elements Tai Chi Chuan Theory In-DepthCésar EscalanteBelum ada peringkat
- Model Systems in SDHx-related Pheochromocytoma/paragangliomaDokumen25 halamanModel Systems in SDHx-related Pheochromocytoma/paragangliomaCésar EscalanteBelum ada peringkat
- COVID-19 and The Endocrine System Exploring The Unexplored PDFDokumen5 halamanCOVID-19 and The Endocrine System Exploring The Unexplored PDFDiego CoronelBelum ada peringkat
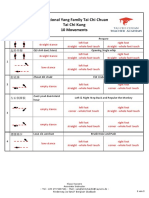
- Traditional Yang Family Tai Chi Chuan Senior Form 26 MovementsDokumen5 halamanTraditional Yang Family Tai Chi Chuan Senior Form 26 MovementsCésar EscalanteBelum ada peringkat
- Steps: Liraglutide (Saxenda) For Weight LossDokumen2 halamanSteps: Liraglutide (Saxenda) For Weight LossCésar EscalanteBelum ada peringkat
- Treatment of Peripheral Precocious Puberty in McCune-Albright SyndromeDokumen12 halamanTreatment of Peripheral Precocious Puberty in McCune-Albright SyndromeCésar EscalanteBelum ada peringkat
- 2020 Article 1793Dokumen13 halaman2020 Article 1793César EscalanteBelum ada peringkat
- Traditional Yang Family Tai Chi Chuan Tai Chi Kung 10 MovementsDokumen3 halamanTraditional Yang Family Tai Chi Chuan Tai Chi Kung 10 MovementsCésar EscalanteBelum ada peringkat
- Latent Adrenal Insufficiency: From Concept To DiagnosisDokumen12 halamanLatent Adrenal Insufficiency: From Concept To DiagnosisCésar EscalanteBelum ada peringkat
- The Effects Induced by Spinal Manipulative Therapy On The Immune and Endocrine SystemDokumen12 halamanThe Effects Induced by Spinal Manipulative Therapy On The Immune and Endocrine SystemCésar EscalanteBelum ada peringkat
- Guidelines For The Management of Glucocorticoids During The Peri OperativeDokumen10 halamanGuidelines For The Management of Glucocorticoids During The Peri OperativeCésar EscalanteBelum ada peringkat
- Traditional Yang Family Tai Chi Chuan Essential Form 22 MovementDokumen5 halamanTraditional Yang Family Tai Chi Chuan Essential Form 22 MovementCésar EscalanteBelum ada peringkat
- Diagnosis and Management of Adrenal InsufficiencyDokumen29 halamanDiagnosis and Management of Adrenal InsufficiencyCésar EscalanteBelum ada peringkat
- iPSC Technology-Based Regenerative Therapy For DiabetesDokumen10 halamaniPSC Technology-Based Regenerative Therapy For DiabetesCésar EscalanteBelum ada peringkat
- Hypertension and AcromegalyDokumen26 halamanHypertension and AcromegalyCésar EscalanteBelum ada peringkat
- HHS Public AccessDokumen35 halamanHHS Public AccessBudi PutraBelum ada peringkat
- The Tailgate Study: Differing Metabolic Effects of A Bout of Excessive Eating and DrinkingDokumen36 halamanThe Tailgate Study: Differing Metabolic Effects of A Bout of Excessive Eating and DrinkingCésar EscalanteBelum ada peringkat
- A Consensus Statement On Acromegaly Therapeutic OutcomesDokumen10 halamanA Consensus Statement On Acromegaly Therapeutic OutcomesCésar EscalanteBelum ada peringkat
- Hypothalamic Amenorrhea and The Long-Term Health ConsequencesDokumen12 halamanHypothalamic Amenorrhea and The Long-Term Health ConsequencesCésar EscalanteBelum ada peringkat
- AmenorrheaDokumen11 halamanAmenorrheaisaBelum ada peringkat
- Polycystic Ovary SyndromeDokumen17 halamanPolycystic Ovary SyndromeCésar EscalanteBelum ada peringkat
- Drugs That May Worsen Myasthenia GravisDokumen1 halamanDrugs That May Worsen Myasthenia GravisyulianitadewiBelum ada peringkat
- 2 PDFDokumen6 halaman2 PDFCésar EscalanteBelum ada peringkat
- Traditional Chinese Medicine Combined With Conventional Therapy For Female Kidney Stone: A Protocol For Systematic Review.Dokumen5 halamanTraditional Chinese Medicine Combined With Conventional Therapy For Female Kidney Stone: A Protocol For Systematic Review.César EscalanteBelum ada peringkat
- 2 PDFDokumen6 halaman2 PDFCésar EscalanteBelum ada peringkat
- Correspondence on COVID-19 cytokine storm syndromes and immunosuppressionDokumen2 halamanCorrespondence on COVID-19 cytokine storm syndromes and immunosuppressionCésar EscalanteBelum ada peringkat
- Correspondence on COVID-19 cytokine storm syndromes and immunosuppressionDokumen2 halamanCorrespondence on COVID-19 cytokine storm syndromes and immunosuppressionCésar EscalanteBelum ada peringkat
- The Effect of High-Dose Vitamin C On Biochemical Markers of Myocardial Injury in Coronary Artery Bypass SurgeryDokumen8 halamanThe Effect of High-Dose Vitamin C On Biochemical Markers of Myocardial Injury in Coronary Artery Bypass SurgeryCésar EscalanteBelum ada peringkat
- Rohit Patil Black BookDokumen19 halamanRohit Patil Black BookNaresh KhutikarBelum ada peringkat
- Sentinel 2 Products Specification DocumentDokumen510 halamanSentinel 2 Products Specification DocumentSherly BhengeBelum ada peringkat
- April 26, 2019 Strathmore TimesDokumen16 halamanApril 26, 2019 Strathmore TimesStrathmore Times100% (1)
- Insider Threat ManagementDokumen48 halamanInsider Threat ManagementPatricia LehmanBelum ada peringkat
- AsiaSat 7 at 105Dokumen14 halamanAsiaSat 7 at 105rahman200387Belum ada peringkat
- (23005319 - Acta Mechanica Et Automatica) A Study of The Preload Force in Metal-Elastomer Torsion SpringsDokumen6 halaman(23005319 - Acta Mechanica Et Automatica) A Study of The Preload Force in Metal-Elastomer Torsion Springsstefan.vince536Belum ada peringkat
- Hyper-Threading Technology Architecture and Microarchitecture - SummaryDokumen4 halamanHyper-Threading Technology Architecture and Microarchitecture - SummaryMuhammad UsmanBelum ada peringkat
- 8dd8 P2 Program Food MFG Final PublicDokumen19 halaman8dd8 P2 Program Food MFG Final PublicNemanja RadonjicBelum ada peringkat
- PROF ED 10-ACTIVITY #1 (Chapter 1)Dokumen4 halamanPROF ED 10-ACTIVITY #1 (Chapter 1)Nizelle Arevalo100% (1)
- Liebert PSP: Quick-Start Guide - 500VA/650VA, 230VDokumen2 halamanLiebert PSP: Quick-Start Guide - 500VA/650VA, 230VsinoBelum ada peringkat
- Customer Perceptions of Service: Mcgraw-Hill/IrwinDokumen27 halamanCustomer Perceptions of Service: Mcgraw-Hill/IrwinKoshiha LalBelum ada peringkat
- Mission Ac Saad Test - 01 QP FinalDokumen12 halamanMission Ac Saad Test - 01 QP FinalarunBelum ada peringkat
- LM1011 Global ReverseLogDokumen4 halamanLM1011 Global ReverseLogJustinus HerdianBelum ada peringkat
- Resume of Deliagonzalez34 - 1Dokumen2 halamanResume of Deliagonzalez34 - 1api-24443855Belum ada peringkat
- Energy AnalysisDokumen30 halamanEnergy Analysisca275000Belum ada peringkat
- HenyaDokumen6 halamanHenyaKunnithi Sameunjai100% (1)
- Exercises2 SolutionsDokumen7 halamanExercises2 Solutionspedroagv08Belum ada peringkat
- 2010 - Impact of Open Spaces On Health & WellbeingDokumen24 halaman2010 - Impact of Open Spaces On Health & WellbeingmonsBelum ada peringkat
- ConductorsDokumen4 halamanConductorsJohn Carlo BautistaBelum ada peringkat
- Simply Put - ENT EAR LECTURE NOTESDokumen48 halamanSimply Put - ENT EAR LECTURE NOTESCedric KyekyeBelum ada peringkat
- 621F Ap4405ccgbDokumen8 halaman621F Ap4405ccgbAlwinBelum ada peringkat
- Electronics Project Automatic Bike Controller Using Infrared RaysDokumen16 halamanElectronics Project Automatic Bike Controller Using Infrared RaysragajeevaBelum ada peringkat
- Bank NIFTY Components and WeightageDokumen2 halamanBank NIFTY Components and WeightageUptrend0% (2)
- Pita Cyrel R. Activity 7Dokumen5 halamanPita Cyrel R. Activity 7Lucky Lynn AbreraBelum ada peringkat
- ERP Complete Cycle of ERP From Order To DispatchDokumen316 halamanERP Complete Cycle of ERP From Order To DispatchgynxBelum ada peringkat
- Photographing Shadow and Light by Joey L. - ExcerptDokumen9 halamanPhotographing Shadow and Light by Joey L. - ExcerptCrown Publishing Group75% (4)
- 10 1 1 124 9636 PDFDokumen11 halaman10 1 1 124 9636 PDFBrian FreemanBelum ada peringkat
- Progressive Myoclonic Epilepsies - Practical Neurology 2015. MalekDokumen8 halamanProgressive Myoclonic Epilepsies - Practical Neurology 2015. MalekchintanBelum ada peringkat
- Memo Roll Out Workplace and Monitoring Apps Monitoring Apps 1Dokumen6 halamanMemo Roll Out Workplace and Monitoring Apps Monitoring Apps 1MigaeaBelum ada peringkat
- DECA IMP GuidelinesDokumen6 halamanDECA IMP GuidelinesVuNguyen313Belum ada peringkat