Arthroplasty
Diunggah oleh
Zen Bambang LJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Arthroplasty
Diunggah oleh
Zen Bambang LHak Cipta:
Format Tersedia
Comment
transplants, are just beginning to address their respective responsibilities to protect their people from exploitation and to develop a national self-suciency in organ donation. Leadership and encouragement from transplant professionals would contribute greatly to governments taking eective action to adopt and then to enforce strong laws consistent with the declaration. Participants in the Istanbul meeting have already played major roles in the promulgation of such laws and regulations within the past 2 years in China, Pakistan, and the Philippines. The implications of the declarations denitions, principles, and recommendations are profound. The declaration will reinforce the resolve of governments and international organisations to develop laws and guidelines to bring an end to wrongful practices. The declaration calls for transparent regulatory oversight with international accountabilitythat ensures the safety and wellbeing of donors and recipients alike. Still, more is needed from the transplant and medical communities. The Transplantation Society and the International Society of Nephrology have endorsed the declaration. The steering committee has created task forces to facilitate dissemination of the declaration to national health authorities and to supplement existing professional standards. Recommendations from these task forces ought to include cancelling the professional society membership of individuals who do not adhere to the principles of the declaration. Drug companies and other funding agencies ought to apply the declarations principles when supporting research and other clinical activities. Journals ought not to publish studies from individuals or groups who do not comply with the declaration. The legacy of transplantation is threatened by organ tracking and transplant tourism. The Declaration of Istanbul on Organ Tracking and Transplant Tourism aims to combat these activities and to preserve the nobility
of organ donation. The success of transplantation as a life-saving treatment does not requirenor justify victimising the worlds poor people as the source of organs for the rich. Steering Committee of the Istanbul Summit*
dma@transplantation-soc.org
*Steering Committee: Mario Abbud-Filho, FAMERP and Institute of Urology and Nephrology, Sao Paolo; Mustafa Al-Mousawi, Middle East Society for Organ Transplantation, Kuwait City; Ali Abdulkareem Alobaidli, Kidney Transplant Services, Sheikh Khalifa Medical City, Abu Dhabi; Mona Nasir Al-Rukhaimi, Renal Unit, Dubai Hospital, Dubai; Alireza Bagheri, Tehran University of Medical Sciences; M A Bakr, Urology & Nephrology Centre, Mansoura University, Mansoura; Antoine Barbari, Rak Hariri University Hospital, Beirut; Alexander Capron, University of Southern California, Los Angeles; Jeremy R Chapman, The Transplantation Society and University of Sydney; William Couser, International Society of Nephrology, Seattle; Gabriel Danovitch, David Geen School of Medicine at UCLA; Leonardo D de Castro, University of the Philippines, Quezon City; Francis L Delmonico, The Transplantation Society, Boston; Iraj Fazel, Academy of Medical Sciences, Tehran; Mehmet Haberal, Baskent University and Turkish Transplantation Society, Ankara; Vivekanand Jha, Postgraduate Institute of Medical Education and Research, Chandigarh; Eiji Kobayashi, Jichi Medical University, Tochigi; Norbert Lameire, University Hospital, Ghent; Adeera Levin, University of British Columbia, Vancouver; Mahamane Kalil Maga, University of Bamako; Dominique Martin, Centre for Applied Philosophy and Public Ethics, University of Melbourne; Marwan Masri, Asian Society of Transplantation, Beirut; Saraladevi Naicker, University of the Witwatersrand, Johannesburg; Luc Nol, WHO, Geneva; S Adibul Hasan Rizvi, Sindh Institute of Urology and Transplantation, Karachi; Bernardo Rodriguez-Iturbe, International Society of Nephrology, Maracaibo; Mohamed H Sayegh, Harvard Medical School, Boston; Faissal AM Shaheen, Saudi Council for Organ Transplantation, Jeddah; A G Stephan, Nephrology Division, Rizk Hopsital, Beirut; Annika Tibell, Karolinska Institute, Stockholm; Matthew Kwok-Lung Tong, Princess Margaret Hospital, Hong Kong; and A Vathsala, National University of Singapore. The Istanbul Summit was supported by an unrestricted grant to The Transplantation Society from Astellas Pharmaceuticals. The members of the Steering Committee declare that they have no conict of interest. 1 2 3 World Health Assembly. Development of guiding principles for human organ transplants: WHA40.13. Geneva: World Health Organization, 1987. World Health Assembly. Preventing the purchase and sale of human organs: WHA42.5. Geneva: World Health Organization, 1989. World Health Assembly. Human organ transplantation (adopting the WHO Guiding Principles on Organ Transplantation): WHA44.25. Geneva: World Health Organization, 1991. World Health Assembly. Human organ and tissue transplantation: WHA57.18. May 22, 2004. http://www.who.int/gb/ebwha/pdf_les/WHA57/A57_ R18-en.pdf (accessed June 16, 2008). Shimazono Y. The state of the international organ trade: a provisional picture based on integration of available information. Bull World Health Organ 2007; 85: 95562. Naqvi SAA, Ali B, Mazhar F, Zafar MN, Rizvi SAH. A socioeconomic survey of kidney vendors in Pakistan. Transpl Int 2007; 20: 93439.
Selective factor Xa inhibition for thromboprophylaxis
Published Online June 25, 2008 DOI:10.1016/S01406736(08)60879-X See Articles page 31
For over 60 years, vitamin K antagonists, such as warfarin, have been the only available oral anticoagulants. Although eective, these drugs are challenging to use. Dose requirements vary among patients and the anticoagulant response is
unpredictable. Consequently, coagulation needs to be monitored and the dose frequently adjusted to ensure that a therapeutic level of anticoagulation is achieved. Such monitoring is inconvenient for patients and costly for health-care systems.
www.thelancet.com Vol 372 July 5, 2008
Comment
The limitations of vitamin K antagonists have prompted the development of new oral anticoagulants that target activated factor X (factor Xa) or thrombin. Rivaroxaban is a new oral direct inhibitor of factor Xa in advanced stages of development. Rivaroxaban has high oral bioavailability, rapid onset of action, and a half life of 59 h;1 furthermore, it produces such a predictable anticoagulant response that no monitoring is required. Building on promising phase II results,2 four large phase III trials, involving more than 12 500 patients, have compared rivaroxaban with enoxaparin for prevention of venous thromboembolism after hip or knee arthroplasty (table).36 In todays Lancet, Ajay Kakkar and colleagues report the results of the RECORD2 trial,4 in which they compared oral unmonitored rivaroxaban, at 10 mg once daily given for 35 days, with subcutaneous enoxaparin, at 40 mg once daily given for 12 days, in 2509 patients undergoing total hip arthroplasty. The primary ecacy outcome, a composite of deep-vein thrombosis, nonfatal pulmonary embolism, and all-cause mortality at 3042 days, occurred in 93% of patients given enoxaparin and 20% of those treated with rivaroxaban (absolute risk reduction 73%, 95% CI 5294%; number needed to treat 14). Compared with enoxaparin, rivaroxaban also signicantly reduced the incidence of symptomatic venous thromboembolism (12% and 02%, respectively; absolute risk reduction 1%; number needed to treat 100). Unlike most other thromboprophylaxis trials, the primary safety outcome of major bleeding in the RECORD2 trial excluded surgical-site bleeding unless it led to reoperation or death. As a result, the incidence of major bleeding was low (<01% in both groups); however, rates of non-major bleeding, which included surgical-site bleeding, were similar with enoxaparin and rivaroxaban (55% and 65%, respectively). The RECORD2 results add to the evidence that an extended duration of thromboprophylaxis after total hip arthroplasty is more eective than short-term therapy.7 Although current guidelines recommend extended thromboprophylaxis after total hip arthroplasty,8 such treatment is underused after hospital discharge9 because low-molecular-weight heparin and fondaparinux must be given by subcutaneous injection, whereas vitamin K antagonists need monitoring. With xed oral dosing and no monitoring, rivaroxaban will streamline out-of-hospital thromboprophylaxis. Another barrier to the use of extended prophylaxis is the belief held by many orthopaedic surgeons that most
www.thelancet.com Vol 372 July 5, 2008
cases of deep-vein thrombosis after total hip arthroplasty are asymptomatic and conned to the calf and, therefore, unlikely to lead to pulmonary embolism. RECORD2 challenges this view because the reduction in any deep-vein thrombosis with rivaroxaban was associated with a parallel reduction in symptomatic venous thromboembolism. The unequal treatment durations in RECORD2 tell us little about the relative ecacy of rivaroxaban and enoxaparin. However, RECORD1 showed that 35 days of once daily rivaroxaban was more eective than 35 days of once daily enoxaparin for prevention of venous thromboembolism after total hip arthroplasty, and RECORD3 and RECORD4 showed that 1014 days of once daily rivaroxaban was more eective than 1014 days of once daily or twice daily enoxaparin after knee arthroplasty (table). Importantly, the benets of rivaroxaban over enoxaparin occurred without an increase in bleeding events. With superior ecacy, no compromise in safety, and a convenient once daily regimen, rivaroxaban seems an obvious choice for simplied thromboprophylaxis after hip or knee arthroplasty. What are the unresolved issues? Ximelagatran, an oral thrombin inhibitor, was withdrawn from the market because of potential hepatic toxicity.10 There is no evidence of liver toxicity with the rivaroxaban regimens used in the RECORD trials, but data on exposure in more patients and for longer durations than are currently available are needed to conrm the drugs safety. In RECORD2, the small excess in the number of cardiovascular events after stopping rivaroxaban treatment (ve on drug, none on control) raises concerns about rebound activation of coagulation. Further data are needed to exclude this possibility.
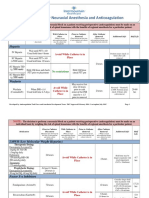
Setting N Enoxaparin dose and treatment duration Rivaroxaban DVT, PE, or death treatment duration Events RECORD13 RECORD24 RECORD35 RECORD46 THA THA TKA TKA 4541 40 mg once daily, 35 days 35 days 37% vs 11% 93% vs 20% 189% vs 96% 101% vs 69% RRR 70% 79% 49% 31% Symptomatic VTE
Events 12% vs 02% 20% vs 07% 12% vs 07%
RRR 80% 66% NS
2509 40 mg once daily, 3139 days 1014 days 2531 3148 40 mg once daily, 1014 days 1014 days 30 mg twice daily, 1014 days 1014 days
Trials compared rivaroxaban (10 mg once daily) with enoxaparin for thromboprophylaxis after hip or knee arthroplasty. N=number of participants. DVT=deep-vein thrombosis. NS=not signicant. PE=pulmonary embolism. VTE=venous thromboembolism. RRR=relative-risk reduction. THA=total hip arthroplasty. TKA=total knee arthroplasty.
Table: Main ecacy outcomes of the RECORD trials
Comment
How does rivaroxaban compare with other new anticoagulants? Extended thromboprophylaxis with once daily unmonitored dabigatran etexilate, an oral direct thrombin inhibitor, was recently shown to be non-inferior to an equal duration of subcutaneous enoxaparin for prevention of venous thromboembolism after total hip arthroplasty,11 prompting approval of dabigatran etexilate for this indication in Europe. However, the ecacy and safety of rivaroxaban and dabigatran etexilate have yet to be compared directly. The major impetus for developing new oral anticoagulants is to replace vitamin K antagonists for long-term indications. Phase III trials comparing rivaroxaban with warfarin for venous-thromboembolism treatment and for prevention of cardioembolic events in patients with atrial brillation are underway. Dabigatran etexilate and apixaban, another oral factor Xa inhibitor, are being investigated for the same indications. The promising results with rivaroxaban and dabigatran etexilate for prevention of venous thromboembolism bring a replacement for warfarin one step closer. *John W Eikelboom, Jerey I Weitz
McMaster University, Hamilton, ON, Canada, L9K 1H8 eikelbj@mcmaster.ca
JWE has received honoraria from companies developing new anticoagulants (AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, GlaxoSmithKline, Pzer, Portola, and Sano-Aventis). JIW was a member of the independent adjudication committee for the RECORD trials and has received honoraria from companies developing new anticoagulants (Bayer, Bristol-Myers Squibb, Boehringer Ingelheim, Daiichi Sankyo, Portola, Sano-Aventis, and Takeda).
1 2
10 11
Gross PL, Weitz JI. New anticoagulants for treatment of venous thromboembolism. Arterioscler Thromb Vasc Biol 2008; 28: 38086. Turpie AG. Oral, direct factor Xa inhibitors in development for the prevention and treatment of thromboembolic diseases. Arterioscler Thromb Vasc Biol 2007; 27: 123847. Eriksson BI, Borris LC, Friedman RJ, et al. Oral rivaroxaban compared with subcutaneous enoxaparin for extended thromboprophylaxis after total hip arthroplasty: the RECORD1 trial. 2007. http://abstracts.hematologylibrary. org/cgi/content/abstract/110/11/6?maxtoshow=&HITS=10&hits= 10&RESULTFORMAT=&fulltext=rivaroxaban&searchid=1&FIRSTINDEX= 0&volume=110&issue=11&resourcetype=HWCIT (accessed June 19, 2008). Kakkar AK, Brenner B, Dahl OE, et al, for the RECORD2 investigators. Extended duration rivaroxaban versus short-term enoxaparin for the prevention of venous thromboembolism after total hip arthroplasty: a double-blind, randomised controlled study. Lancet 2008; published online June 25. DOI:10.1016/S0140-6736(08)60880-6. Lassen MR, Turpie AGG, Rosencher N, et al. Rivaroxabanan oral, direct factor Xa inhibitor for thromboprophylaxis after total knee arthoplasty: the RECORD3 trial. 2007. http://abstracts.hematologylibrary.org/cgi/content/ abstract/110/11/308?maxtoshow=&HITS=10&hits=10&RESULTFORMAT= &fulltext=rivaroxaban&searchid=1&FIRSTINDEX=0&volume=110&issue=11 &resourcetype=HWCIT (accessed June 19, 2008). Bayer Healthcare. Prevention of thromboembolism after knee replacement surgery: rivaroxaban one tablet/once-daily superior to twice-daily injectable enoxaparin in preventing venous blood clots after total knee replacement surgery in pivotal phase III trial. May 30, 2008. http://www. investor.bayer.com/no_cache/en/events/live-events/rivaroxaban-data-atefort-2008/ (accessed June 19, 2008). Eikelboom JW, Quinlan DJ, Douketis JD. Extended-duration prophylaxis against venous thromboembolism after total hip or knee replacement: a meta-analysis of the randomised trials. Lancet 2001; 358: 915. Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004; 126 (suppl 3): 338S400S. Warwick D, Friedman RJ, Agnelli G, et al. Insucient duration of venous thromboembolism prophylaxis after total hip or knee replacement when compared with the time course of thromboembolic events: ndings from the Global Orthopaedic Registry. J Bone Joint Surg Br 2007; 89: 799807. Eikelboom JW, Weitz JI. A replacement for warfarin: the search continues. Circulation 2007; 116: 13133. Eriksson BI, Dahl OE, Rosencher N, et al, for the RE-NOVATE Study Group. Dabigatran etexilate versus enoxaparin for prevention of venous thromboembolism after total hip replacement: a randomised, double-blind, non-inferiority trial. Lancet 2007; 370: 94956.
Treatment of depression in patients with cancer
See Articles page 40
In todays Lancet, Vanessa Strong and colleagues report a randomised trial that shows the benet of a nurse-delivered intervention for depression in a mixed group of outpatients with cancer.1 Depression is common in patients with cancer, although it often remains undetected and untreated.2,3 Of late, clinicians have made recommendations to set up routine screening for distress in patients in cancer-treatment centres,4,5 although widespread implementation of these recommendations has lagged.6 Strong and co-workers show that treatment for depression might be cost eective and integrated with cancer care, which highlights the potential value of screening and might lead to wide-scale acceptance of these recommendations.
All patients in Strong and co-workers study met diagnostic criteria for major depressive disorder of at least 1 months duration but for less than 2 years. Depressive disorders were identied initially by screening with a self-report measure of depression, and conrmed by a structured diagnostic interview. All patients received usual care, which consisted of care with a primary-care physician and communication with the primary-care physician and oncologist about the diagnosis of major depressive disorder and, if requested, advice about the choice of antidepressant medication. Those in the test group received a standardised complex psychosocial intervention. This intervention, originally developed for the treatment of depression in primary
www.thelancet.com Vol 372 July 5, 2008
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- TLDR Anticoag Cheat Sheet v1.1Dokumen3 halamanTLDR Anticoag Cheat Sheet v1.1nitishavenkat100% (9)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Editorial Caravaggio Apixaban en Cáncer y ETVDokumen3 halamanEditorial Caravaggio Apixaban en Cáncer y ETVSANTIAGO FOREROBelum ada peringkat
- Acs 2023 Part 4 Presentation VersionDokumen38 halamanAcs 2023 Part 4 Presentation Versionapi-668470097Belum ada peringkat
- warfarin (Coumadin) - UW Medicine Anticoagulation Services Https Sites - Uw.edu Anticoag Drugs WarfarinDokumen12 halamanwarfarin (Coumadin) - UW Medicine Anticoagulation Services Https Sites - Uw.edu Anticoag Drugs Warfarintl drBelum ada peringkat
- Registrul Produselor Biocide Plasate Pe Piata in Baza Acordarii Certificatelor de Recunoastere MutuaDokumen88 halamanRegistrul Produselor Biocide Plasate Pe Piata in Baza Acordarii Certificatelor de Recunoastere MutuaDaniel IliescuBelum ada peringkat
- Tratamen Ima StrptokinazaDokumen1 halamanTratamen Ima StrptokinazaAriana PascuBelum ada peringkat
- Sdcep Anticoagulants Quick Reference Guide 2nd EditionDokumen5 halamanSdcep Anticoagulants Quick Reference Guide 2nd EditionMeryem LahlouBelum ada peringkat
- DIfferenz TabelleDokumen54 halamanDIfferenz TabellemarkovonduehringBelum ada peringkat
- Role of DOAC in The Management of COVID-19 Patients: Desak Nyoman Desy LestariDokumen32 halamanRole of DOAC in The Management of COVID-19 Patients: Desak Nyoman Desy Lestaridesy lestariBelum ada peringkat
- Dissertation V1 Kopie Für 1,5T PulsDokumen58 halamanDissertation V1 Kopie Für 1,5T PulsmarkovonduehringBelum ada peringkat
- DOAC ChartDokumen3 halamanDOAC ChartRawan ZayedBelum ada peringkat
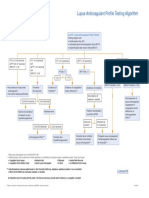
- Lupus Anticoagulant Profile Testing AlgorithmDokumen1 halamanLupus Anticoagulant Profile Testing Algorithmsalamon2tBelum ada peringkat
- Document PDFDokumen4 halamanDocument PDFDebasis SahooBelum ada peringkat
- Anticoagulants Drug TableDokumen1 halamanAnticoagulants Drug TableNicole HoBelum ada peringkat
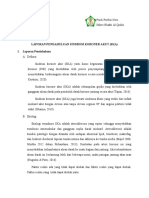
- Laporan Pendahuluan Sindrom Koroner Akut (Ska) I. Laporan PendahuluanDokumen14 halamanLaporan Pendahuluan Sindrom Koroner Akut (Ska) I. Laporan PendahuluanBahiya Az ZahraBelum ada peringkat
- Transition of Anticoagulants 2016: From To ActionDokumen4 halamanTransition of Anticoagulants 2016: From To ActionS_XangaiBelum ada peringkat
- MCQ Bleeding Disorders 2nd Year2021Dokumen6 halamanMCQ Bleeding Disorders 2nd Year2021sherif mamdoohBelum ada peringkat
- NOAC ChartDokumen2 halamanNOAC Chartsgod34Belum ada peringkat
- Obat Sistem HematologiDokumen21 halamanObat Sistem HematologiSuryana AdityaBelum ada peringkat
- Anticoagulants and Antiplatelet AgentsDokumen4 halamanAnticoagulants and Antiplatelet AgentsMark Russel Sean LealBelum ada peringkat
- A Brief Summary of Antiplatelet Agents - Deranged PhysiologyDokumen3 halamanA Brief Summary of Antiplatelet Agents - Deranged Physiologyhnzzn2bymdBelum ada peringkat
- Pretest P4 Khasiat Dan Golongan Obat SlideDokumen4 halamanPretest P4 Khasiat Dan Golongan Obat SlideAFRINA FAJAR EKOWATIBelum ada peringkat
- ASRA - Summary Flash CardsDokumen2 halamanASRA - Summary Flash CardsParvathy R NairBelum ada peringkat
- Principles of Antiplatelet Therapy: DR Htet Htet Htethtet@Imu - Edu.MyDokumen36 halamanPrinciples of Antiplatelet Therapy: DR Htet Htet Htethtet@Imu - Edu.MyAbby Liew100% (1)
- Administration of Coagulation-Altering Therapy in The Patient Presenting For Oral Health and Maxillofacial SurgeryDokumen18 halamanAdministration of Coagulation-Altering Therapy in The Patient Presenting For Oral Health and Maxillofacial SurgeryLaura Giraldo QuinteroBelum ada peringkat
- Anticoagulant and Antiplatelet Medications and Dental Procedures ADADokumen8 halamanAnticoagulant and Antiplatelet Medications and Dental Procedures ADADeeBelum ada peringkat
- 2 Marks QuestionsDokumen6 halaman2 Marks QuestionsAdnanBelum ada peringkat
- Neuraxial ProceduresDokumen2 halamanNeuraxial ProceduresRessy HastoprajaBelum ada peringkat
- Anticoagulation Guidelines For Neuraxial Procedures: Anticoagulants, InjectableDokumen4 halamanAnticoagulation Guidelines For Neuraxial Procedures: Anticoagulants, InjectablepaulaBelum ada peringkat
- Anti Platelet DrugsDokumen3 halamanAnti Platelet DrugsShayan ShayanBelum ada peringkat