Status Epilepticus1
Diunggah oleh
doktoreluHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Status Epilepticus1
Diunggah oleh
doktoreluHak Cipta:
Format Tersedia
Summary Status epilepticus (SE) is a major neurological emergency [1,2,3], potentially life-threatening that requires immediate and vigorous
treatment [1,2,3] to stop the ongoing seizures, purpose to prevent severe neuronal injuries, associated complications or even death [3,4]. This study was designed to evaluate the incidence of SE in the neurological intensive care unit, the basic etiology favored the development of SE, the management in stopping the seizures and recurrence prevention. In the study was performed a retrospective analysis of the medical records of the Emergency Hospital over a period of 3 years (01.01.2008-01.10.2011) that included evaluation of 220 patients hospitalized with SE. The mean age of patients was 53.52.6 years with the highest percentage among males (54.1%). The most common cause of SE was appreciated to be of toxico-dysmetabolic genesis (47.27%).According to the morphology of seizures the highest incidence returns to SE generalized convulsive (SECG) type (85%). In the study group was found that every patient has more than one probable cause of SE development of which alcohol abuse was in 41.1%, on the second being placed history of stroke (16.81%). To elderly patients acute and chronic
cerebrovascular pathology together form more than 50% of cases. Clinical outcome during the period immediately after finalization was characterized by a polymorphism of neurological and systemic symptoms that appreciate entirely the clinical picture and severity of the process. The management was performed according to international and institutional protocols, which was primary directed on rapid finishing of seizures and prevention of recurrence, in parallel with treatment of acute cases. The mortality due to consequences of SE in this group was 16.81%.
Introduction SE constitute a potentially fatal medical emergency, that occurs as a result of primary neurologic disease or secondary to critical illness[2,3,4] and is manifested by continuous seizure activity >30min. or 2 sequential seizures during this period without full recovery of consciousness [3,6], being associated with a high rate of morbidity and mortality[4,5]. SE accounts for 3.5% of admissions to emergency departments in the developed nations and for 11% in developing country[3,4].The average incidence of SE is 20/100.000 for industrialized countries [1,5]. SE affects males and females equally, the major causes in adults are: cerebrovascular diseases (23-25%), trauma (4.6%), ethanol/drug -related (12.2%) tumors (4.3%), CNS infections (1.8%) [2,4,6]. Approximately 25% of SE occurs in patients with epilepsy and more than 15% of patients with epilepsy experience at least one episode of SE[1,3]. Complications of SE include: epilepsy (20-40%), encephalopathy (6-15%) and focal neurological deficits (9-11%) [1,4,5]. SE mortality rates are 15-20%[4,6]. Death usually occurs as a consequence of brain injury underlying the development of SE and no more than 2% of patients die directly from it [1,5]. Fortunately, SE responds to relatively simple treatment, but when simple interventions fail, refractory SE requires more aggressive measures to prevent complications [3,5]. Purpose of the study: analysis of SE incidence, etiology, the management features and mortality rates. Materials and Methods: This study was based on retrospective analysis of medical records from the Stroke / Intensive Care Unit and Neurology departments over a period of 3 years (01.01.2008-01.01.2011). All medical records were standardized according to: general data, medical history/ pathological history, etiology, type of SE, methods of diagnosis, management of SE.
Results: During the period 01.01.2008-01.01.2011 in Neurological Clinic of Emergency Hospital, 220 patients were admitted with the diagnosis of SE, patient age ranged from 15-88 years, mean age 53.5years 2.6. Structure of the patients according to age is presented in Table 1. Table 1. Structure of the patients according to age (%) <20 8 3,63 21-40 50 22,72 Age (years) 41-60 61-80 101 57 45,90 25,90 >80 4 1,81 Total 220 100
Total %
The distribution by sex was: females -101p (45.9% 3.2) respectively males 119p (54.1% 3.3). Structure of the SE etiology is represented in Table 2. Tabel 2. Structure of the SE etiology (%) Etiologic factor Idiopathic epilepsy Secondary vascular epilepsy posttraumatic Secondary epilepsy with unspecified etiology Encephalopathy toxicodysmetabolic Anoxic encephalopathy (CO intoxication) Stroke ischemic hemorrhagic Secondary purulent meningoencephalitis Cerebral arterio-venous malformation Expansive process Brain metastases Fluid and electrolyte disorders Number of cases 11 41 24 8 93 1 22 9 2 2 2 1 2 % 5,9 18,63 10,90 3,63 42,27 0,45 10 4,09 0.9 0,9 0,9 0,45 0,9 eP 1,58 2,62 2,1 1,26 3,52 0,44 2 1,31 0,63 0,63 0,63 0,44 0,63
The polymorphism of SE according to seizures morphology is represented in Figure1.
In study group have been determined the antecedents and comorbidities present in patients, which would be favored the installation of SE, shown in Table 3. Tabel 3. The structure based on antecedents and present comorbidities. Antecedents/Comorbidities Idiopathic epilepsy Trauma Antecedents of stroke Neurosurgical intervention Meningoencephalitis Chronic alcoholism Drug addiction Hepatic cirrhosis Diabetes mellitus Tuberculosis Cerebral arterio-venous malformation Pulmonary adenocarcinoma Expansive intracerebral process Absolute number 11 31 39 5 1 92 2 10 6 5 3 1 2 % 5 14,09 17,72 2,27 0,45 41,81 0,9 4,54 2,72 2,27 1,36 0,45 0,9 eP 1,46 2,31 2,57 1,0 0,44 3,32 0,63 1,4 1,09 1,0 0,77 0,44 0,63
Of all patients diagnosed with idiopathic epilepsy (11p) reduced compliance to treatment was recorded at 5p (45.45% 3.35), canceling treatment because of side-effects without medical advice-3p (27.27% 3.0), change of the preparation-2p (18.18% 2.6) causes that induced SE development. Clinical evolution of SE in the period immediately after completion was characterized by an polymorphism of clinical symptoms which appreciated integral and defined the gravity of the process, so vegetative disorders with systemic involvement were appreciated to the forefront such as deviations in
blood pressure-hypertension/hypotension 89.54% ( 2.06) cases, these symptoms being associated with cardiac rhythm disturbances - arrhythmias/ tachycardias -57, 26% ( 3, 33). Have been present and clinical manifestations generated by the inflammatory process-pneumonia (22.72% 2.82), fever (51.3% 3.36) with the association of pulmonary edema in 16.8% ( 2.51) cases. The severity of the process was determined by metabolic disturbances especially -metabolic acidosis (3.63% 1.26), hyperglycemia (15.9% 2.46), renal failure (8.63% 1.8). Signs of cerebral involvement with different degrees of expressions of the consciousness disturbances were in 100% of cases, the most severe cases being associated with cerebral edema (33.18% 3.17), coma and death. Methods used for establishing the etiology of SE have included: general laboratory analysis and instrumental investigations such as: computerized EEG104p (47.27% 3.36), cerebral CT-139p (63.18% 3.25 ) Angio-CT cerebral3p (1.36% 0.78), chest radiography -86p (39.1% 3.18), lumbar puncture-18p (8.18% 1.84), ultrasonography-62P (28.18% 3.03), transcranial Doppler-19p (8.63% 1.83), EKG - 170p (77.27 2.82%). The management constituted: primary assessment of ABC, the airways was secured with Guedel tube or nasopharyngeal, continuous O2 flow and cardiorespiratory function monitoring, blood pressure. The next step was the establishment of the i/v approach and administration of anticonvulsant preparations. As preparations of first line in resolving SE were used the benzodiazepines (Diazepam 10mg) i/v or rectal tube, followed by intravenous infusion of Phenytoin (Phenydan) 15-20 mg/kg with speed 50mg/min in order to prevent recurrence, in parallel with treatment of the underlying etiology that favored the installation of SE. From all patients, about-55p (25% 2, 91) have been registered repeated recurrent seizures in a period from several hours to
several days after solving SE that were resolved by the administration of sol. Luminal (phenobarbital 15-18 mg/kg i/v infusion rate of 25-60 ml/min). The mortality rate was 37 cases (16.81% 2.5) from which 16p (43.24% 3.3) men and respectively 21p (56.76% 3.33) women. Age of the deceased ranged from 18-82 years, average age 54.05 3.7 years. Discussion: Analyzing the obtained data was appreciated that the highest incidence of SE was in the age group 41-60 years (45.9%), with predominant involvement of male patients (54.1%). Therefore, results that the incident is higher in the elderly population and in males in comparison with females in adult population. Considering the aging of the population in the future SE will become a major problem, increasingly, in the public health and practice. According to the etiology, SE has developed mainly on the background of toxico-dysmetabolic disorders (42.27%), on second place being the secondary epilepsy (31.81%) and only 5.09% of cases assigned to idiopathic epilepsy. Thus, in the study group, SE was present predominantly in patients with secondary generalized epilepsy than in those with idiopathic generalized epilepsy. Pursuant to the type of SE, predominant type was SECG in 85% of cases and just 1.36% is assigned to type SE non-convulsive (SENC). Evaluating patient's history and comorbidities was determined that in the study lot has prevailed on the forefront the alcohol abuse (41.81%) and 16.81% belonging to history of stroke that have been aggravated with SE. As we notice in the Table 2 and 3 for each patient is present more than a cause responsible to the development of SE, which includes both an acute and chronic determinant (to a patient returning to four cases). The management was performed according to international and institutional treatment protocols approved. Therefore treatment is continued simultaneously in several directions and focused on early seizure termination, prevention of recurrent seizures, identification of underlying etiology, and treatment of
secondary complications. The mortality rate constituted 16.81% of cases; the patient's age at diagnosis, etiology of SE, severity of the underlying disease, and duration of SE are the main predictors of increased short-term mortality. Conclusions: 1. SE is a major emergency, potentially fatal which requires prompt recognition according to diagnostic schemes and the use of treatment protocols adopted in neurological intensive care unit to prevent serious neurological complications. 2. The toxico-dysmetabolic etiology constituted primary cause (42.27%) of development of the SE in this study group. References: 1. DeLorenzo RJ, Pellock JM, Towne AR, Boggs JG. Epidemiology of status epilepticus. J Clin Neurophysiol 1995; 12:31625. 2. Edward M. Manno, MD. New Management Strategies in the Treatment of Status Epilepticus. Mayo Clin Proc. 2003;78:508-518 3. Groppa St. Antiepilepticele i tratamentul Epilepsiei. Chiinu, 2006. 176 p. 4. Hussam Seif-Eddeine, David M Treiman. Problems and controversies in status epilepticus: a review and recommendations. Expert Review of Neurotherapeutics 12/2011; 11(12):1747-58. 5. Nathan B. Fountain Status Epilepticus: Risk Factors and Complications. Epilepsia, 41(Suppl. 2):S23-S30, 2000 6. Shorvon S D. The management of status epilepticus. J Neurol Neurosurg Psychiatry 2001. 70II22II27.II27. 7. Susanne Knake, Felix Rosenow, Mathias Vescovi. Incidence of Status Epilepticus in Adults in Germany: A Prospective, Population-Based Study. Epilepsia Volume 42, Issue 6, pages 714718, June 2001
Anda mungkin juga menyukai
- Doppler SymeDokumen12 halamanDoppler SymedoktoreluBelum ada peringkat
- Screening For Carotid Artery Stenosis: U.S. Preventive Services Task Force Recommendation StatementDokumen28 halamanScreening For Carotid Artery Stenosis: U.S. Preventive Services Task Force Recommendation StatementdoktoreluBelum ada peringkat
- Screening For Carotid Artery Stenosis: U.S. Preventive Services Task Force Recommendation StatementDokumen28 halamanScreening For Carotid Artery Stenosis: U.S. Preventive Services Task Force Recommendation StatementdoktoreluBelum ada peringkat
- Articol Statusul EpilepticDokumen8 halamanArticol Statusul EpilepticdoktoreluBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Pharma Module 1 PDFDokumen22 halamanPharma Module 1 PDFSheryhan Tahir BayleBelum ada peringkat
- PharmacologyDokumen9 halamanPharmacologyAishwarya MenonBelum ada peringkat
- Hospital ICU Organization and TypesDokumen82 halamanHospital ICU Organization and TypesPaul Shan GoBelum ada peringkat
- TCM Cases - PainDokumen671 halamanTCM Cases - PainGeander G. Bacheti100% (5)
- Recurrent Gingival Cyst of Adult: A Rare Case Report With Review of LiteratureDokumen5 halamanRecurrent Gingival Cyst of Adult: A Rare Case Report With Review of Literaturesayantan karmakarBelum ada peringkat
- CPG 2013 - Prevention and Treatment of Venous ThromboembolismDokumen170 halamanCPG 2013 - Prevention and Treatment of Venous ThromboembolismMia Mus100% (1)
- Check Your English Vocabulary For MedicineDokumen59 halamanCheck Your English Vocabulary For MedicineCentru RefillBelum ada peringkat
- Dental CementsDokumen208 halamanDental CementsAkriti Goel33% (3)
- Clinical Hypnosis in The Treatment of P... Flashes - A Randomized Controlled TrialDokumen17 halamanClinical Hypnosis in The Treatment of P... Flashes - A Randomized Controlled TrialRIJANTOBelum ada peringkat
- Enriched Air Diver Knowledge ReviewDokumen2 halamanEnriched Air Diver Knowledge Reviewgabriele belmonte100% (1)
- Thyroidectomy Nursing CareDokumen73 halamanThyroidectomy Nursing CareZNEROL100% (1)
- Comparison of Roth Appliance and Standard Edgewise Appliance Treatment ResultsDokumen9 halamanComparison of Roth Appliance and Standard Edgewise Appliance Treatment ResultsseboistttBelum ada peringkat
- Patar Elementary School Fourth Periodic Test in Mapeh 6Dokumen8 halamanPatar Elementary School Fourth Periodic Test in Mapeh 6Mark Angel MorenoBelum ada peringkat
- Functional Dyspepsia: Recent Advances in Pathophysiology: Update ArticleDokumen5 halamanFunctional Dyspepsia: Recent Advances in Pathophysiology: Update ArticleDen BollongBelum ada peringkat
- Antioxidant and Antimicrobial Activities of Pink Guava Leaves and SeedsDokumen10 halamanAntioxidant and Antimicrobial Activities of Pink Guava Leaves and SeedsRobbyBelum ada peringkat
- 9 Hair CleanseDokumen11 halaman9 Hair CleanseSeetha ChimakurthiBelum ada peringkat
- Wound Management ProcedureDokumen51 halamanWound Management ProcedureSisca Dwi AgustinaBelum ada peringkat
- Headache History Checklist For PhysiciansDokumen3 halamanHeadache History Checklist For PhysiciansFarazBelum ada peringkat
- NIC Network HospitalsDokumen172 halamanNIC Network HospitalsParas JainBelum ada peringkat
- Pediatric Caseheet PDFDokumen23 halamanPediatric Caseheet PDFAparna DeviBelum ada peringkat
- Review Article On History of LM Potency - Tracing Its Roots in The PastDokumen6 halamanReview Article On History of LM Potency - Tracing Its Roots in The PastRenu BalaBelum ada peringkat
- Nutrition Quiz: Build a Healthy DietDokumen17 halamanNutrition Quiz: Build a Healthy DietJan Angelo OcadoBelum ada peringkat
- HHDBI7 W FX Xe 35 R DNJHN 6 Xsadtz 5 PQ9 ZSNI6 SXZXWDokumen26 halamanHHDBI7 W FX Xe 35 R DNJHN 6 Xsadtz 5 PQ9 ZSNI6 SXZXWleartaBelum ada peringkat
- Acute Lymphoblastic LeukaemiaDokumen3 halamanAcute Lymphoblastic LeukaemiamelpaniBelum ada peringkat
- 10 0000@Www Quintpub Com@ejed@18638Dokumen23 halaman10 0000@Www Quintpub Com@ejed@18638Víctor Rodríguez67% (3)
- Activity Intolerance Care Plan For CFDokumen8 halamanActivity Intolerance Care Plan For CFapi-314197645Belum ada peringkat
- Neonatal Developemental MilestonesDokumen4 halamanNeonatal Developemental MilestonesSubha DeepBelum ada peringkat
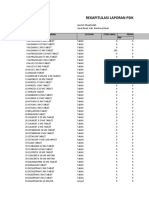
- Rekapitulasi Laporan Psikotropika Bandung BaratDokumen8 halamanRekapitulasi Laporan Psikotropika Bandung BaratFajarRachmadiBelum ada peringkat
- 129 Accommodative EsotropiaDokumen6 halaman129 Accommodative EsotropiakarenafiafiBelum ada peringkat
- Guidance For Installation and Testing AcceptanceDokumen32 halamanGuidance For Installation and Testing AcceptanceMun WaiBelum ada peringkat