Dog Model Antiox
Diunggah oleh
Ingrid AtaydeHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Dog Model Antiox
Diunggah oleh
Ingrid AtaydeHak Cipta:
Format Tersedia
JOURNAL OF NEUROCHEMISTRY
| 2012 | 120 | 13
doi: 10.1111/j.1471-4159.2011.07548.x
, ,
*Department of Psychiatry, University Medicine Goettingen, Goettingen, Germany German Research Center for Neurodegenerative Diseases, DZNE Goettingen, Germany German Research Foundation Research Center for Molecular Physiology of the Brain, CMPB, Goettingen, Germany Department of Neurology, University Medicine, Goettingen, Germany MPI for Experimental Medicine, Goettingen, Germany
Read the full article Biliverdin reductase-A: a novel drug target for atorvastatin in a dog pre-clinical model of Alzheimer disease on page 135.
Alzheimers disease is the most common type of dementia in old-age. An increasing number of studies has shown that elevated serum cholesterol levels might increase the risk of Alzheimers disease (Notkola et al. 1998; Kivipelto et al. 2001). Statins lower cholesterol levels by inhibiting HMGCoA-reductase, the key enzyme of cellular cholesterol synthesis. The application of statins in animal models of Alzheimers disease resulted in reduced production of the neurotoxic peptide amyloid-beta and a benetial effect on cognitive parameters (Hartman 2005). This raised the hope that statins might be a promising drug in the treatment of Alzheimers disease. Data from epidemiologic studies and clinical trials remain conicting. Three large epidemiologic cohort studies supported the notion that statins might have a prophylactic effect and reduce the risk to develop Alzheimers disease (Cramer et al. 2008; Sparks et al. 2008; Haag et al. 2009). However, a Cochrane review published in 2009 came to the conclusion that There is good evidence from randomized clinical trials that statins given in late life to individuals at risk of vascular disease have no effect in preventing Alzheimers disease or dementia. Biologically, it seems feasible that statins could prevent dementia because of their role in cholesterol reduction and initial evidence from observational studies was very promising. Indication bias may have been a factor in these studies, however, and the evidence from subsequent randomized clinical trials has been negative (McGuinness et al. 2009). No benet could be deduced from previous clinical trials with statins in Alzheimers disease patients, according to a second Cochrane report from 2009. In the randomized,
controlled, double-blind and multicenter trial LEADe, atorvastatin was evaluated as a treatment for mild to moderate Alzheimer disease in 640 patients. Treatment was well tolerated but did not result in improved cognition or global function. Likewise, in a randomized, controlled, double-blind study of Alzheimer patients treated with 80 mg simvastatin daily for 26 weeks, a small benet in the mini mental state examination (MMSE) test was observed in the simvastatin group, however no effect could be shown in the ADAS-Cog scale (Simons et al. 2002). Consistent with this, in a recently published report by Sano et al. (2011) no benet of 40 mg Simvastatin was detected regarding cognition, global function or behavior in a randomized, double-blind and placebocontrolled trial in 406 patients with mild to moderate Alzheimers disease. So far, no primary prevention trials have been initiated with statins. Current strategies concentrate on earlier interventions such as the stage of mild cognitive impairment based on the understanding that treatment in the stage of mild to moderate Alzheimers disease might be far too late in the disease process. An ongoing, double-blind, placebocontrolled and multicenter trial with simvastatin is currently
Received October 12, 2011; accepted October 18, 2011. Address correspondence and reprint requests to Anja Schneider, MD, Memory Clinic, Department of Psychiatry and Psychotherapy, University Medicine Goettingen, Von-Siebold-Str. 5, 37075 Goettingen, Germany. E-mail: aschnei8@gwdg.de Abbreviations used: APP, amyloid precursor protein; HO-1/BVR-A, heme oxygenase-1/biliverdin reductase-A.
2011 The Authors Journal of Neurochemistry 2011 International Society for Neurochemistry, J. Neurochem. (2012) 120, 13
2 | Review
conducted for individuals suffering from amnestic mild cognitive impairment which is associated with a high risk to develop Alzheimers disease (SIMaMCI, competence network dementia, Germany). In tissue culture experiments and several animal models including mice and guinea pig, it has been shown that reduction of cholesterol results in lower activity of presenilin and beta-secretase, the two enzymes which cleave the amyloid precursor protein (APP) to release the amyloid-beta peptide (Hartman 2005) (for an overview on the pleiotropic actions of statins in Alzheimers disease see Fig. 1). Barone et al. (2012) report in this issue that statins may improve cognition independently from their cholesterol lowering effect by an antioxidant action. Previously, this group has shown that treatment of aged beagles with 80 mg atorvastatin/d over 14.5 months resulted in improved discrimination learning, while amyloid-beta concentrations in the cerebrospinal uid remained unchanged (Buttereld et al. 2011). The authors now identify heme oxygenase-1/ biliverdin reductase-A (HO-1/BVR-A) as a potential cholesterol-independent mediator of this effect. HO-1/BVR-A is a neuronally expressed enzyme which catalizes the reaction of heme to free iron, carbon monoxide and biliverdin. Biliverdin is then converted to the antioxidant bilirubin. The authors show that HO-1/BVR-A protein levels and enzyme activity were up-regulated in the parietal cortex in response to atorvastatin treatment. This was paralleled by reduced oxidative stress indices (4-hydroxy-2-nonenal and 7-ketocholesterol) which might be mediated by the increased activity of HO-1/BVR-A. These ndings might explain the protective effect observed with statins even in the absence of overt hypercholesterinemia in patients (Barone et al. 2012).
Reactive oxygen and nitrogen species are elevated prior to deposition of plaques and tangles and have therefore been widely discussed as potential mediators of neurotoxicity in Alzheimers disease as well as a potential therapeutic target. HO-1/BVR-A is the inducible form of two isoenzymes of heme-oxygenase and up-regulated under oxidative/nitrosative stress conditions and increases the production of the radical scavenger bilirubin. A reduced ability to respond to oxidative stress was described during aging and cortical HO1/BVR-A expression levels decrease during ageing and in the hippocampus of patients with Alzheimers disease or mild cognitive impairment (Abraham and Kappas 2008; Barone et al. 2011). In addition, APP can bind and inhibit HO-1/BVR-A activity (Abraham and Kappas 2008). The authors show that an up-regulation of HO-1/BVR-A protein levels and enzyme activity upon statin treatment is negatively correlated with oxidative stress markers, betasecretase 1 levels and cognitive dysfunction in aged canines. The animal model used in this study, an aged beagle hound, is especially interesting, because it is a natural model of pre-clinical Alzheimers disease and reects the age-related changes and the pathology observed in humans (Barone et al. 2012). The authors did not elucidate the mechanism how statins might regulate HO-1/BVR-A expression. The observed increase in HO-1/BVR-A expression could however be induced by the effects of statin on the transcription factor nuclear factor-like 2 (Lu et al. 2008). Nuclear factor-like 2 has previously been shown to be up-regulated by statins (Hsieh et al. 2008). Besides its antioxidative effect, HO-1/BVR-A might have an impact on other pathophysiological events in Alzheimers disease. Interestingly, HO-1/BVR-A was described to
Microglia acvaon Inammaon Oxidave stress Tau pathology
Stans Aninammatory
Reduced expression of cytokines, MHCII
Anoxidave
iNOS inhibion, reduced NO producon Reducon of free radicals
Reduced tau aggregaon
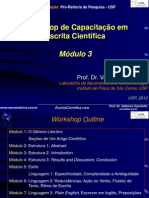
Fig. 1 Pleiotrophic actions of statins in Alzheimers disease. Statins inhibit the production of cholesterol and isoprenoids (farnesyl- and geranygeranylpyrophosphate) (orange box). APP endocytosis and amyloidogenic APP processing are impaired by low plasma membrane cholesterol. Both, b-secretase BACE and c-secretase activity, depend on membrane cholesterol and low cholesterol favors a-secretase cleavage of APP. Statins also counteract several downstream effects of Abeta: inammation, oxidative stress and tau pathology, partially by inhibition of protein isoprenylation which regulates activity of small GTPase rho, rac and ras.
B A sec ret C ase E APP
A b e t a
A bA eb t e at
a
A bA eb t e at a
Acetyl-CoA HMG-CoA Mevalonate Isopentyl-PP Ras/Rho/Rac
Oligomers
Stans
APP -secretase
Farnesyl-PP Squalen Geranylgeranyl-PP
Membrane cholesterol Stans
Cholesterol
Inhibion of Abeta producon:
Reducon of BACE/ -secretase acvity Reducon of APP endocytosis and processing
2011 The Authors Journal of Neurochemistry 2011 International Society for Neurochemistry, J. Neurochem. (2012) 120, 13
Review | 3
facilitate microglial clearance of amyloid-beta and to downregulate tau expression in a cell model (Abraham and Kappas 2008). HO-1/BVR-A expression also enhances resistance against nitrosative stress and Selley et al. reported reduced protein tyrosine nitration in APP mice treated with simvastatin (Selley 2005). Whether HO-1/BVR-A plays a crucial role in mediating antioxidant effects during aging and in Alzheimers disease remains to be established further in transgenic and knockout animal models. If this appears to be the case the regulation of HO-1/BVR-A levels can be added to the list of potentially benecial actions of statins in aging and neurodegeneration.
Conict of interest
The authors state no conict of interest.
References
Abraham N. G. and Kappas A. (2008) Pharmacological and clinical aspects of heme oxygenase. Pharmacol. Rev. 60, 79127. Barone E., Di Domenico F., Cenini G., Sultana R., Clini C., Preziosi P., Perluigi M., Mancuso C. and Buttereld D. A. (2011) Biliverdin reductase-a protein levels and activity in the brains of subjects with Alzheimer disease and mild cognitive impairment. Biochim. Biophys. Acta 1812, 480487. Barone E., Mancuso C., Di Domenico F., Sultana R., Murphy M. P., Head E. and Buttereld D. A. (2012) Biliverdin reductase-A: a novel drug target for atorvastatin in a dog pre-clinical model of Alzheimer disease. J. Neurochem 120, 135146. Buttereld D. A., Barone E., Di Domenico F., Cenini G., Sultana R., Murphy M. P., Mancuso C. and Head E. (2011) Atorvastatin treatment in a dog preclinical model of Alzheimer Disease leads to upregulation of heme oxygenase-1 and is associated with reduced oxidative stress in brain. Int. J. Neuropsychopharmacol. Published Online doi: 2010.1017/S1461145711001118. Cramer C., Haan M. N., Galea S., Langa K. M. and Kalbeisch J. D. (2008) Use of statins and incidence of dementia and cognitive
impairment without dementia in a cohort study. Neurology 71, 344350. Haag M. D., Hofman A., Koudstaal P. J., Stricker B. H. and Breteler M. M. (2009) Statins are associated with a reduced risk of Alzheimer disease regardless of lipophilicity. The Rotterdam Study. J. Neurol. Neurosurg. Psychiatry 80, 1317. Hartman T. (2005) Cholesterol and Alzheimers disease: statins, cholesterol depletion in APP processing and Abeta generation. Subcell. Biochem. 38, 365380. Hsieh C. H., Rau C. S., Hsieh M. W., Chen Y. C., Jeng S. F., Lu T. H. and Chen S. S. (2008) Simvastatin-induced heme oxygenase-1 increases apoptosis of Neuro 2A cells in response to glucose deprivation. Toxicol. Sci. 101, 112121. Kivipelto M., Helkala E. L., Hanninen T., Laakso M. P., Hallikainen M., Alhainen K., Soininen H., Tuomilehto J. and Nissinen A. (2001) Midlife vascular risk factors and late-life mild cognitive impairment: A population-based study. Neurology 56, 16831689. Lu Y., Gong P. and Cederbaum A. I. (2008). Pyrazole induced oxidative liver injury independent of CYP2E1/2A5 induction due to Nrf2 deciency. Toxicology 252:916. McGuinness B., Craig D., Bullock R. and Passmore P. (2009) Statins for the prevention of dementia. Cochrane Database Syst. Rev. 2, CD003160. Notkola I. L., Sulkava R., Pekkanen J., Erkinjuntti T., Ehnholm C., Kivinen P., Tuomilehto J. and Nissinen A. (1998) Serum total cholesterol, apolipoprotein E epsilon 4 allele, and Alzheimers disease. Neuroepidemiology 17, 1420. Sano M., Bell K. L., Galasko D., Galvin J. E., Thomas R. G., van Dyck C. H. and Aisen P. S. (2011) A randomized, double-blind, placebocontrolled trial of simvastatin to treat Alzheimer disease. Neurology 77, 556563. Selley M. L. (2005) Simvastatin prevents 1-methyl-4-phenyl-1,2,3,6tetrahydropyridine-induced striatal dopamine depletion and protein tyrosine nitration in mice. Brain Res. 1037, 16. Simons M., Schwarzler F., Lutjohann D., von Bergmann K., Beyreuther K., Dichgans J., Wormstall H., Hartmann T. and Schulz J. B. (2002) Treatment with simvastatin in normocholesterolemic patients with Alzheimers disease: A 26-week randomized, placebo-controlled, double-blind trial. Ann. Neurol. 52, 346350. Sparks D. L., Kryscio R. J., Sabbagh M. N., Connor D. J., Sparks L. M. and Liebsack C. (2008) Reduced risk of incident AD with elective statin use in a clinical trial cohort. Curr. Alzheimer Res. 5, 416421.
2011 The Authors Journal of Neurochemistry 2011 International Society for Neurochemistry, J. Neurochem. (2012) 120, 13
Anda mungkin juga menyukai
- Neurobiology of The Aging DogDokumen12 halamanNeurobiology of The Aging DogIngrid AtaydeBelum ada peringkat
- Introduction To TCVM DX With Tongue & PulseDokumen22 halamanIntroduction To TCVM DX With Tongue & PulseIngrid AtaydeBelum ada peringkat
- CornellsystemDokumen1 halamanCornellsystemapi-253788473Belum ada peringkat
- Cummingsetal k9 As Animal Model of Human Aging and DementiaDokumen10 halamanCummingsetal k9 As Animal Model of Human Aging and DementiaIngrid AtaydeBelum ada peringkat
- Cognitive Dysfunction in DogsfrankDokumen6 halamanCognitive Dysfunction in DogsfrankIngrid AtaydeBelum ada peringkat
- Learn. Mem. 2001 Siwak Aging BeaglesDokumen10 halamanLearn. Mem. 2001 Siwak Aging BeaglesIngrid AtaydeBelum ada peringkat
- Brain Polarization Enhances The Formation and Retention of Motor MemoriesDokumen15 halamanBrain Polarization Enhances The Formation and Retention of Motor MemoriesIngrid AtaydeBelum ada peringkat
- J Neurophysiol-2011-Schambra TDCS LearningDokumen11 halamanJ Neurophysiol-2011-Schambra TDCS LearningIngrid AtaydeBelum ada peringkat
- Intro Comp IntelligenceDokumen14 halamanIntro Comp IntelligenceIngrid AtaydeBelum ada peringkat
- Animal Models For AD ResDokumen8 halamanAnimal Models For AD ResIngrid AtaydeBelum ada peringkat
- Fecteau e Al Tdcs Decison RiskDokumen7 halamanFecteau e Al Tdcs Decison RiskIngrid AtaydeBelum ada peringkat
- J Neurophysiol-2009-Galea-Formation Retention Motor MemoDokumen9 halamanJ Neurophysiol-2009-Galea-Formation Retention Motor MemoIngrid AtaydeBelum ada peringkat
- Facteu at Al Decision Risk NovDokumen6 halamanFacteu at Al Decision Risk NovIngrid AtaydeBelum ada peringkat
- 2010 The Canine Cognitive Dysfunction Rating Scale CCDRDokumen6 halaman2010 The Canine Cognitive Dysfunction Rating Scale CCDRIngrid AtaydeBelum ada peringkat
- J Neurophysiol 2010 Tecchio 1134 40Dokumen8 halamanJ Neurophysiol 2010 Tecchio 1134 40Ingrid AtaydeBelum ada peringkat
- Planning AbilityDokumen7 halamanPlanning AbilityIngrid AtaydeBelum ada peringkat
- Tdcs Healthy SubjDokumen10 halamanTdcs Healthy SubjIngrid AtaydeBelum ada peringkat
- W.K. Kellogg Foundation Logic Model Development GuideDokumen72 halamanW.K. Kellogg Foundation Logic Model Development GuideSiddharth SrivastavaBelum ada peringkat
- As Cinco Forças e Supply ChainTrab - TGADokumen11 halamanAs Cinco Forças e Supply ChainTrab - TGAIngrid AtaydeBelum ada peringkat
- Global Financial Management: Debt Policy, Capital Structure, and Capital BudgetingDokumen40 halamanGlobal Financial Management: Debt Policy, Capital Structure, and Capital BudgetingahmedmtBelum ada peringkat
- Scorecard WhitepaperDokumen12 halamanScorecard WhitepaperIngrid AtaydeBelum ada peringkat
- Plain English HandbookDokumen83 halamanPlain English HandbookJessa Mae MuñozBelum ada peringkat
- Spirit RepDokumen4 halamanSpirit Repapi-27237371Belum ada peringkat
- Workshops Escrita Modulos 3 4Dokumen72 halamanWorkshops Escrita Modulos 3 4Ingrid AtaydeBelum ada peringkat
- EXCERPT FROM CHAPTER 8: The Cat: Its Behavior, Nutrition and Health, Linda P. Case, Iowa State Press (2003)Dokumen8 halamanEXCERPT FROM CHAPTER 8: The Cat: Its Behavior, Nutrition and Health, Linda P. Case, Iowa State Press (2003)Ingrid AtaydeBelum ada peringkat
- Plain English HandbookDokumen83 halamanPlain English HandbookJessa Mae MuñozBelum ada peringkat
- Developing Financial ProjectionsDokumen14 halamanDeveloping Financial ProjectionsIngrid AtaydeBelum ada peringkat
- Workshops Escrita Modulos 7 8Dokumen58 halamanWorkshops Escrita Modulos 7 8Alexandre Magno Batista MachadoBelum ada peringkat
- The Link New Zealand StoryDokumen16 halamanThe Link New Zealand StoryIngrid AtaydeBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- ST. LUKE'S MEDICAL CENTER EMPLOYEE'S FOUNDATION AFW v. NLRCDokumen3 halamanST. LUKE'S MEDICAL CENTER EMPLOYEE'S FOUNDATION AFW v. NLRCjodelle11Belum ada peringkat
- CPHQ Text BookDokumen20 halamanCPHQ Text BookCphq Cphq Ali100% (2)
- 8-Critical Appraisal of An ArticleDokumen20 halaman8-Critical Appraisal of An ArticleMohmmed Abu MahadyBelum ada peringkat
- Exp 4 Centrifugal CompressorDokumen11 halamanExp 4 Centrifugal CompressorFaris HamirBelum ada peringkat
- Enzymes in Grain ProcessingDokumen1 halamanEnzymes in Grain ProcessingAttila-Levente FogarasiBelum ada peringkat
- Punjab National BankDokumen4 halamanPunjab National BankShubham RajBelum ada peringkat
- Health Insurance BookDokumen3 halamanHealth Insurance BookHarish SihareBelum ada peringkat
- Thank You For Being A Liberty Mutual Renters Customer Since 2014!Dokumen29 halamanThank You For Being A Liberty Mutual Renters Customer Since 2014!RewaBelum ada peringkat
- 6 Instrumentation PDFDokumen144 halaman6 Instrumentation PDFWanderley MandruzatoBelum ada peringkat
- Leonard Peikoff-Introduction To LogicDokumen20 halamanLeonard Peikoff-Introduction To Logicbursa07Belum ada peringkat
- Outback MenuDokumen2 halamanOutback MenuzeeBelum ada peringkat
- Sebuguero V NLRC Case Digest PDFDokumen2 halamanSebuguero V NLRC Case Digest PDFYodh Jamin Ong0% (1)
- MUMMY'S KITCHEN NEW FinalDokumen44 halamanMUMMY'S KITCHEN NEW Finalanon_602671575100% (4)
- Yuasa NPL Range: VRLA BatteriesDokumen2 halamanYuasa NPL Range: VRLA BatteriesVuro BegaBelum ada peringkat
- FBS Q1 WK1Dokumen4 halamanFBS Q1 WK1Nicole Eve Pelaez-AbarrientosBelum ada peringkat
- Dingenen 2017Dokumen14 halamanDingenen 2017pedro.coleffBelum ada peringkat
- Scooty PepDokumen1 halamanScooty PepYASHBelum ada peringkat
- Plant Based Plan White PaperDokumen24 halamanPlant Based Plan White PaperSara AdemovicBelum ada peringkat
- Dental Caries PrevelenceDokumen11 halamanDental Caries PrevelenceSonal KaleBelum ada peringkat
- Full Download Book Microbiome Immunity Digestive Health and Nutrition Epidemiology Pathophysiology Prevention and Treatment PDFDokumen41 halamanFull Download Book Microbiome Immunity Digestive Health and Nutrition Epidemiology Pathophysiology Prevention and Treatment PDFmildred.walker324100% (15)
- Lesson 5: Prejudice and StereotypesDokumen31 halamanLesson 5: Prejudice and StereotypesZeynep SulaimankulovaBelum ada peringkat
- NABARD Grade A 2020 Phase 2 ESI ARDDokumen6 halamanNABARD Grade A 2020 Phase 2 ESI ARDrohit bhosadBelum ada peringkat
- Single Conductor 15KV, Shielded, MV-105Dokumen2 halamanSingle Conductor 15KV, Shielded, MV-105henry hernandezBelum ada peringkat
- Thyroid OphthalmopathyDokumen59 halamanThyroid OphthalmopathyLavanya MadabushiBelum ada peringkat
- Formula Sheet Pre-MidDokumen4 halamanFormula Sheet Pre-MidUzair KhanBelum ada peringkat
- Fitting in and Fighting Back: Stigma Management Strategies Among Homeless KidsDokumen24 halamanFitting in and Fighting Back: Stigma Management Strategies Among Homeless KidsIrisha AnandBelum ada peringkat
- Multicultural Aspects of Communication Disorders - CH 12Dokumen21 halamanMulticultural Aspects of Communication Disorders - CH 12Maitry PatelBelum ada peringkat
- Mechanism of Enzyme ActionDokumen19 halamanMechanism of Enzyme ActionRubi AnnBelum ada peringkat
- 6 Human Diseases That Cause by VirusesDokumen7 halaman6 Human Diseases That Cause by VirusesJefry JapBelum ada peringkat
- Complications of Diabetes MellitusDokumen46 halamanComplications of Diabetes MellitusAbhijith MenonBelum ada peringkat