Predictor Difficult Intubation BJA
Diunggah oleh
Lovely GaluhDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Predictor Difficult Intubation BJA
Diunggah oleh
Lovely GaluhHak Cipta:
Format Tersedia
British Journal of Medical Practitioners, March 2010, Volume 3, Number 1
BJMP.org
BJMP 2010;3(1):307
Predictors Predictors Predictors Predictors of of of of Difficult Intubation: Study In Kashmiri Population Difficult Intubation: Study In Kashmiri Population Difficult Intubation: Study In Kashmiri Population Difficult Intubation: Study In Kashmiri Population
Arun Kr. Gupta Arun Kr. Gupta Arun Kr. Gupta Arun Kr. Gupta , Mohamad Ommid , Showkat Nengroo , Imtiyaz Naqash and Anjali Mehta , Mohamad Ommid , Showkat Nengroo , Imtiyaz Naqash and Anjali Mehta , Mohamad Ommid , Showkat Nengroo , Imtiyaz Naqash and Anjali Mehta , Mohamad Ommid , Showkat Nengroo , Imtiyaz Naqash and Anjali Mehta
Abstract Abstract Abstract Abstract
Airway assessment is the most important aspect of anaesthetic practice as a difficult intubation may be unanticipated. A prospective study was done to
compare the efficacy of airway parameters to predict difficult intubation. Parameters studied were degree of head extension, thyromental distance, inter
incisor gap, grading of prognathism, obesity and modified mallampati classification. 600 Patients with ASA I& ASA II grade were enrolled in the study. All
patients were preoperatively assessed for airway parameters. Intra-operatively all patients were classified according to Cormack and Lehane laryngoscopic
view. Clinical data of each test was collected, tabulated and analyzed to obtain the sensitivity, specificity, positive predictive value & negative predictive
value. Results obtained showed an incidence of difficult intubation of 3.3 % of patients. Head and neck movements had the highest sensitivity (86.36%);
high arched palate had the highest specificity (99.38%). Head and neck movements strongly correlated for patients with difficult intubation.
KEYWORDS KEYWORDS KEYWORDS KEYWORDS
Intubation, Anaesthesia, Laryngoscopy
Introduction Introduction Introduction Introduction
The fundamental responsibility of an anesthesiologist is to
maintain adequate gas exchange through a patent airway.
Failure to maintain a patent airway for more than a few minutes
results in brain damage or death
1
. Anaesthesia in a patient with
a difficult airway can lead to both direct airway trauma and
morbidity from hypoxia and hypercarbia. Direct airway trauma
occurs because the management of the difficult airway often
involves the application of more physical force to the patients
airway than is normally used. Much of the morbidity
specifically attributable to managing a difficult airway comes
from an interruption of gas exchange (hypoxia and
hypercapnia), which may then cause brain damage and
cardiovascular activation or depression
2
.
Though endotracheal intubation is a routine procedure for all
anesthesiologists, occasions may arise when even an experienced
anesthesiologist might have great difficulty in the technique of
intubation for successful control of the airway. As difficult
intubation occurs infrequently and is not easy to define,
research has been directed at predicting difficult laryngoscopy,
i.e. when is not possible to visualize any portion of the vocal
cords after multiple attempts at conventional laryngoscopy. It is
argued that if difficult laryngoscopy has been predicted and
intubation is essential, skilled assistance and specialist
equipment should be provided. Although the incidence of
difficult or failed tracheal intubation is comparatively low,
unexpected difficulties and poorly managed situations may
result in a life threatening condition or even death
3
.
Difficulty in intubation is usually associated with difficulty in
exposing the glottis by direct laryngoscopy. This involves a
series of manoeuvres, including extending the head, opening the
mouth, displacing and compressing the tongue into the
submandibular space and lifting the mandible forward. The
ease or difficulty in performing each of these manoeuvres can be
assessed by one or more parameters
4
.
Extension of the head at the atlanto-occipital joint can be
assessed by simply looking at the movements of the head,
measuring the sternomental distance, or by using devices to
measure the angle
5
. Mouth opening can be assessed by
measuring the distance between upper and lower incisors with
the mouth fully open. The ease of lifting the mandible can be
assessed by comparing the relative position of the lower incisors
in comparison with the upper incisors after forward protrusion
of the mandible
6
. The measurement of the mento-hyoid
distance and thyromental distance provide a rough estimate of
the submandibular space
7
. The ability of the patient to move
the lower incisor in front of the upper incisor tells us about jaw
movement. The classification provided by Mallampati et al
8
and
later modified by Samsoon and Young
9
helps to assess the size
of tongue relative to the oropharynx. Abnormalities in one or
more of these parameters may help predict difficulty in direct
laryngoscopy
1
.
Initial studies attempted to compare individual parameters to
predict difficult intubation with mixed results
8,9
. Later studies
have attempted to create a scoring system
3,10
or a complex
mathematical model
11,12
. This study is an attempt to verify
which of these factors are significantly associated with difficult
exposure of glottis and to rank them according to the strength
of association.
Materials & methods Materials & methods Materials & methods Materials & methods
The study was conducted after obtaining institutional review
board approval. Six hundred ASA I & II adult patients,
scheduled for various elective procedures under general
anesthesia, were included in the study after obtaining informed
consent. Patients with gross abnormalities of the airway were
excluded from the study. All patients were assessed the evening
before surgery by a single observer. The details of airway
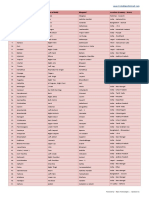
assessment are given in Table I.
R
e
R
e
R
e
R
e
s
e
a
r
c
h
s
e
a
r
c
h
s
e
a
r
c
h
s
e
a
r
c
h
A
r
t
i
c
l
e
A
r
t
i
c
l
e
A
r
t
i
c
l
e
A
r
t
i
c
l
e
British Journal of Medical Practitioners, March 2010, Volume 3, Number 1
BJMP.org
Table I: Method of assessment of various airway parameters Table I: Method of assessment of various airway parameters Table I: Method of assessment of various airway parameters Table I: Method of assessment of various airway parameters
(predictors) (predictors) (predictors) (predictors)
Airway Paramet Airway Paramet Airway Paramet Airway Parameter er er er Method of assessment Method of assessment Method of assessment Method of assessment
Modified
Mallampati Scoring
Class I: Faucial pillars, soft palate and uvula
visible.
Class II: Soft palate and base of uvula seen
Class III: Only soft palate visible.
Class IV: Soft palate not seen
Class I & II : Easy Intubation
Class III & IV: Difficult Intubation
Obesity Obese BMI ( 25)
Non Obese BMI (< 25)
Inter Incisor Gap Distance between the incisors with mouth fully
open(cms)
Thyromental
distance
Distance between the tip of thyroid cartilage and
tip of chin, with fully extended(cms)
Degree of Head
Extension
Grade I 90
Grade II = 80
-90
Grade III < 80
Grading of
Prognathism
Class A: - Lower incisor protruded anterior to
the upper incisor.
Class B: - Lower incisor brought edge to edge
with upper incisor but not anterior to them.
Class C: - Lower incisors could be brought edge
to edge.
In addition the patients were examined for the following.
High arched palate.
Protruding maximally incisor (Buck teeth)
Wide & short Neck
Direct laryngoscopy with Macintosh blade was performed by an
anaesthetist who was blinded to preoperative assessment.
Glottic exposure was graded as per Cormack-Lehane
classification
13
(Fig 1).
Figure 1: Cormack Figure 1: Cormack Figure 1: Cormack Figure 1: Cormack- -- -Lehane grading of glottic exposure on direct Lehane grading of glottic exposure on direct Lehane grading of glottic exposure on direct Lehane grading of glottic exposure on direct
laryngoscopy laryngoscopy laryngoscopy laryngoscopy
Grade 1: most of the glottis visible; Grade 2: only the posterior
extremity of the glottis and the epiglottis visible; Grade 3: no part of the
glottis visible, only the epiglottis seen; Grade 4: not even the epiglottis
seen. Grades 1 and 2 were considered as easy and grades 3 and 4 as
difficult.
Results Results Results Results
Glottic exposure on direct laryngoscopy was difficult in 20
(3.3%) patients. The frequency of patients in various categories
of predictor variables is given in Table-II.
The association between different variables and difficulty in
intubation was evaluated using the chi-square test for qualitative
data and the students test for quantitative data and p<0.05 was
regarded as significant. The clinical data of each test was used to
obtain the sensitivity, specificity and positive and negative
predictive values. Results are shown in Table III.
Table II: The frequency analysis of predictor parameters Table II: The frequency analysis of predictor parameters Table II: The frequency analysis of predictor parameters Table II: The frequency analysis of predictor parameters
Airway Parameter Airway Parameter Airway Parameter Airway Parameter Group Group Group Group Frequency (%) Frequency (%) Frequency (%) Frequency (%)
Modified Mallampati
Scoring
Class 1&2
Class 3&4
96%
4%
Obesity Obese BMI ( 25)
Non Obese BMI (< 25)
28.7%
71.3%
Inter Incisor Gap Class I : >4cm
Class II: <4cm
93.5%
6.5%
Thyromental distance Class I: 6cm.
Class II: 6cm.
94.6%
5.4%
Head & Neck
Movements
Difficult {class II & III
(90)}
Easy {class I(>90)}
16%
84%
Grading of
Prognathism
Difficult (class III)
Easy (class I + II)
96.1%
3.9%
Wide and Short neck Normal neck body ratio
1:13
Difficult (Ratio 1:13)
86.9%
13.1%
High arched Palate Yes
No
1.9%
98.1%
Protruding Incisors Yes
No
4.2%
95.8%
Table III: Comparative analysis of various physical factors and Table III: Comparative analysis of various physical factors and Table III: Comparative analysis of various physical factors and Table III: Comparative analysis of various physical factors and
scoring systems scoring systems scoring systems scoring systems
Physical factors and various Physical factors and various Physical factors and various Physical factors and various
Scoring Systems Scoring Systems Scoring Systems Scoring Systems
Sensitivity Sensitivity Sensitivity Sensitivity
( % ) ( % ) ( % ) ( % )
Specificity Specificity Specificity Specificity
( % ) ( % ) ( % ) ( % )
PPV PPV PPV PPV
( % ) ( % ) ( % ) ( % )
NPV NPV NPV NPV
( % ) ( % ) ( % ) ( % )
Obesity 81.8 72.76 6.34 99.43
Inter incisor gap 18.8 94.14 6.6 98.1
Thyromental distance 72.7 96.5 32.0 99.4
Head and Neck movement 86.36 86.0 34.6 99.7
Prognathism 4.5 96.3 2.7 97.9
Wide and Short neck 45.5 87.9 7.8 98.6
High arched palate 40.1 99.38 60.0 98.67
Protruding incisor 4.6 95.9 2.5 97.79
Mallampati scoring system 77.3 98.2 48.57 99.5
Cormack and Lehanes scoring
system
100 99.7 88 100
Discussion Discussion Discussion Discussion
Difficulty in endotracheal intubation constitutes an important
cause of morbidity and mortality, especially when it is not
anticipated preoperatively. This unexpected difficulty in
intubation is the result of a lack of accurate predictive tests and
inadequate preoperative assessment of the airway. Risk factors if
identified at the preoperative visit help to alert the anaesthetist
so that alternative methods of securing the airway can be used
or additional expertise sought before hand.
Direct laryngoscopy is the gold standard for tracheal intubation.
There is no single definition of difficult intubation but the ASA
defines it as occurring when tracheal intubation requires
multiple attempts, in the presence or absence of tracheal
pathology. Difficult glottic view on direct laryngoscopy is the
most common cause of difficult intubation. The incidence of
difficult intubation in this study is similar to that found in
others.
British Journal of Medical Practitioners, March 2010, Volume 3, Number 1
BJMP.org
As for as the predictors are concerned, different parameters for
the prediction of difficult airways have been studied. Restriction
of head and neck movement and decreased mandibular space
have been identified as important predictors in other studies.
Mallampati classification has been reported to be a good
predictor by many but found to be of limited value by others
14
.
Interincisor gap, forward movement of jaw and thyromental
distance have produced variable results in predicting difficult
airways in previous studies
7,15
. Even though thyromental
distance is a measure of mandibular space, it is influenced by
degree of head extension.
There have been attempts to create various scores in the past.
Many of them could not be reproduced by others or were
shown to be of limited practical value. Complicated
mathematical models based on clinical and/or radiological
parameters have been proposed in the past
16
, but these are
difficult to understand and follow in clinical settings. Many of
these studies consider all the parameters to be of equal
importance.
Instead of trying to find ideal predictor(s), scores or models,
we simply arranged them in an order based on the strength of
association with difficult intubation. Restricted extension of
head, decreased thyromental distance and poor Mallampati class
are significantly associated with difficult intubation.
In other words patients with decreased head extension are at
much higher risk of having a difficult intubation compared to
those with abnormalities in other parameters. The type of
equipment needed can be chosen according to the parameter
which is abnormal. For example in a patient with decreased
mandibular space, it may be prudent to choose devices which
do not involve displacement of the tongue like the Bullard
laryngoscope or Fiber-optic laryngoscope. Similarly in patients
with decreased head extension devices like the McCoy
Larngoscope are likely to be more successful.
Conclusion Conclusion Conclusion Conclusion
This prospective study assessed the efficacy of various
parameters of airway assessment as predictors of difficult
intubation. We have find that head and neck movements, high
arched palate, thyromental distance & Modified Malampatti
classification are the best predictors of difficult intubation.
Competing Interests Competing Interests Competing Interests Competing Interests
None Declared
Author Details Author Details Author Details Author Details
ARUN KUMAR GUPTA, Dept. Of Anaesthesiology, Rural Medical College,
Loni, India, MOHAMED OMMID, Dept. Of Anaesthesiology, SKIMS, Soura,
J&K, India, SHOWKAT NENGROO, Dept. Of Anaesthesiology, SKIMS,
Soura, J&K, India, IMTIYAZ NAQASH, Dept. Of Anaesthesiology, SKIMS,
Soura, J&K, India, ANJALI MEHTA, Dept. Of Anaesthesiology, GMC Jammu,
J&K, India.
CORRESSPONDENCE: ARUN KUMAR GUPTA, Assistant Professor Dept. of
Anaesthesiology & Critical Care Rural Medical College, Loni Maharashtra, India,
413736
Email: guptaarun71@yahoo.com
REFERENCES REFERENCES REFERENCES REFERENCES
1. Rose DK, Cohen MM. The airway: problems and predictions in
18,500 patients. Can J Anaesth 1994; 41:372-83.
2. Benumof JL: Management of the difficult airway: With special
emphasis on awake tracheal intubation. Anesthesiology 1991; 75: 1087-
1110
3. Wilson ME, Spiegelhalter D, Robertson JA, Lesser P. Predicting
difficult intubation. Br J Anaesth 1988; 61(2):211-6.
4. A.Vasudevan, A.S.Badhe. Predictors of difficult intubation a simple
approach. The Internet Journal of Anesthesiology 2009; 20(2)
5. Tse JC, Rimm EB, Hussain A. Predicting difficult endotracheal
intubation in surgical patients scheduled for general anesthesia: a
prospective blind study. Anesth Analg 1995; 81(2):254-8.
6. Savva D. Prediction of difficult tracheal intubation. Br J
Anaesth 1994; 73(2):149-53.
7. Butler PJ, Dhara SS. Prediction of difficult laryngoscopy: an
assessment of the thyromental distance and Mallampati predictive
tests. Anaesth Intensive Care 1992; 20(2):139-42.
8. Mallampati SR, Gatt SP, Gugino LD, Desai SP, Waraksa B,
Freiberger D, et al. A clinical sign to predict difficult tracheal
intubation: a prospective study. Can Anaesth Soc J 1985; 32(4):429-34.
9. Samsoon GL, Young JR. Difficult tracheal intubation: a retrospective
study. Anaesthesia 1987; 42(5):487-90.
10. Nath G, Sekar M. Predicting difficult intubation--a comprehensive
scoring system. Anaesth Intensive Care 1997; 25(5):482-6.
11. Charters P. Analysis of mathematical model for osseous factors in
difficult intubation. Can J Anaesth 1994; 41(7):594-602.
12. Arne J, Descoins P, Fusciardi J, Ingrand P, Ferrier B, Boudigues D,
et al. Preoperative assessment for difficult intubation in general and
ENT surgery: predictive value of a clinical multivariate risk index. Br J
Anaesth 1998; 80(2):140-6.
13. Cormack RS, Lehane J. Difficult tracheal intubation in
obstetrics. Anaesthesia 1984; 39(11):1105-11.
14. Lee A, Fan LT, Gin T, Karmakar MK, Ngan Kee WD. A
systematic review (meta-analysis) of the accuracy of the Mallampati tests
to predict the difficult airway. Anesth Analg 2006; 102(6):1867-78.
15. Bilgin H, Ozyurt G. Screening tests for predicting difficult
intubation. A clinical assessment in Turkish patients.Anaesth Intensive
Care 1998; 26(4):382-6.
16. Naguib M, Malabarey T, AlSatli RA, Al Damegh S, Samarkandi
AH. Predictive models for difficult laryngoscopy and intubation. A
clinical, radiologic and three-dimensional computer imaging study. Can
J Anaesth 1999; 46(8):748-59.
Anda mungkin juga menyukai
- IndianJAnaesth572170-2964618 081406Dokumen5 halamanIndianJAnaesth572170-2964618 081406Tanuja DasariBelum ada peringkat
- Predictionof Difficult AirwayDokumen6 halamanPredictionof Difficult AirwayjemyBelum ada peringkat
- Proceedings of Singapore Healthcare 2016 Wong 19 26Dokumen8 halamanProceedings of Singapore Healthcare 2016 Wong 19 26Aristiyan LuthfiBelum ada peringkat
- Difficult Airway Management in The Intensive Care UnitDokumen10 halamanDifficult Airway Management in The Intensive Care UnitcedivadeniaBelum ada peringkat
- Ulbt X Mallampati Preditor de VadDokumen6 halamanUlbt X Mallampati Preditor de VadAndre RibeiroBelum ada peringkat
- Mallampati ScoreDokumen6 halamanMallampati ScoreJudy DlRopzBelum ada peringkat
- A Retrospective Study of Success, Failure, and Time Needed To Perform Awake IntubationDokumen10 halamanA Retrospective Study of Success, Failure, and Time Needed To Perform Awake IntubationAinun RamadaniBelum ada peringkat
- Anaesthesia - 2014 - Hui - Sublingual Ultrasound As An Assessment Method For Predicting Difficult Intubation A Pilot StudyDokumen6 halamanAnaesthesia - 2014 - Hui - Sublingual Ultrasound As An Assessment Method For Predicting Difficult Intubation A Pilot StudyIndhu SubbuBelum ada peringkat
- Predictores de Intubacion DificilDokumen12 halamanPredictores de Intubacion DificilNoema AmorochoBelum ada peringkat
- Airway Management in The Obese Patient: William A. LoderDokumen6 halamanAirway Management in The Obese Patient: William A. LoderTapas Kumar SahooBelum ada peringkat
- 2011 - Preoperative Endoscopic Airway Examination (PEAE) Provides Superior Airway Information and May Reduce The Use of Unnecessary Awake Ion - MylenaDokumen6 halaman2011 - Preoperative Endoscopic Airway Examination (PEAE) Provides Superior Airway Information and May Reduce The Use of Unnecessary Awake Ion - MylenaMirella Andraous100% (1)
- Airway Management For Induction of General Anesthesia - UpToDate - Be4225b0Dokumen31 halamanAirway Management For Induction of General Anesthesia - UpToDate - Be4225b0Nitin TrivediBelum ada peringkat
- Journal Homepage: - : Manuscript HistoryDokumen12 halamanJournal Homepage: - : Manuscript HistoryIJAR JOURNALBelum ada peringkat
- Emergency Tracheal Intubation Immediately Following Traumatic Injury An Eastern Association For The Surgery of Trauma Practice ManagementDokumen11 halamanEmergency Tracheal Intubation Immediately Following Traumatic Injury An Eastern Association For The Surgery of Trauma Practice ManagementMadalina TalpauBelum ada peringkat
- ExtubationDokumen7 halamanExtubationbalab2311Belum ada peringkat
- Assessment Before Airway PDFDokumen22 halamanAssessment Before Airway PDFAnonymous 9DNZWxbgMZBelum ada peringkat
- Aspiracion EspinalDokumen6 halamanAspiracion EspinalYuriko Castro SanchezBelum ada peringkat
- Anesthetics and Anesthesiology: ClinmedDokumen6 halamanAnesthetics and Anesthesiology: ClinmednadaBelum ada peringkat
- 1 Suhasini SonavdekarDokumen6 halaman1 Suhasini SonavdekarArlia orohBelum ada peringkat
- Oral and Maxillofacial Surgery Clinics of North America Office Based Anesthesia 45 57Dokumen13 halamanOral and Maxillofacial Surgery Clinics of North America Office Based Anesthesia 45 57Max FaxBelum ada peringkat
- Electromyography in Children's Laryngeal Mobility Disorders: A Proposed Grading SystemDokumen6 halamanElectromyography in Children's Laryngeal Mobility Disorders: A Proposed Grading SystemQonita Aizati QomaruddinBelum ada peringkat
- Extubacion British 2010Dokumen4 halamanExtubacion British 2010fciccioliBelum ada peringkat
- Tracheostomy and Intubation Related DysphagiaDokumen25 halamanTracheostomy and Intubation Related DysphagiaVikashBelum ada peringkat
- Management of The Difficult Airway Alternative Airway TechniDokumen31 halamanManagement of The Difficult Airway Alternative Airway TechniChristine NoraBelum ada peringkat
- Anaesthesia - 2016 - Song - Effects of An Alveolar Recruitment Manoeuvre Guided by Lung Ultrasound On Anaesthesia InducedDokumen10 halamanAnaesthesia - 2016 - Song - Effects of An Alveolar Recruitment Manoeuvre Guided by Lung Ultrasound On Anaesthesia InducedAlexandra NemesBelum ada peringkat
- Primary Survey KGD LBM 1Dokumen9 halamanPrimary Survey KGD LBM 1Nur Azizah PermatasariBelum ada peringkat
- Difficult Airway Management During Anesthesia A Review of The Incidence and SolutionsDokumen6 halamanDifficult Airway Management During Anesthesia A Review of The Incidence and SolutionsSudar Pecinta ParawaliBelum ada peringkat
- Predictive Performance of Three Multivariate.24Dokumen7 halamanPredictive Performance of Three Multivariate.24Yves BurckelBelum ada peringkat
- Post in GlycoDokumen4 halamanPost in GlycoSA SHBelum ada peringkat
- Reference: Correspondence Anaesthesia 2014, 69, 281-290Dokumen2 halamanReference: Correspondence Anaesthesia 2014, 69, 281-290Elo Satria SakkaBelum ada peringkat
- Clinical Criteria For Airway Assessment: Correlations With Laryngoscopy and Endotracheal Intubation ConditionsDokumen6 halamanClinical Criteria For Airway Assessment: Correlations With Laryngoscopy and Endotracheal Intubation ConditionscronozerBelum ada peringkat
- Clinical Assessment For The Identification of The Potentially Difficult AirwayDokumen4 halamanClinical Assessment For The Identification of The Potentially Difficult AirwayMuhammad IhsanBelum ada peringkat
- Retracted Article2Dokumen6 halamanRetracted Article2AyuAnatrieraBelum ada peringkat
- Demetriades 2010Dokumen6 halamanDemetriades 2010Sai Rakesh ChavaBelum ada peringkat
- Electrocautery Versus Curette Adenoidectomy: Comparison of Postoperative ResultsDokumen8 halamanElectrocautery Versus Curette Adenoidectomy: Comparison of Postoperative Resultsthanhb1lqdBelum ada peringkat
- Predictors of Difficult Airways in PediatricsDokumen7 halamanPredictors of Difficult Airways in PediatricsPablo Segales BautistaBelum ada peringkat
- The Effect of A Modified Functional Appliance On Obstructive Sleep ApneaDokumen9 halamanThe Effect of A Modified Functional Appliance On Obstructive Sleep ApneaKishore Babu ParvathaneniBelum ada peringkat
- Difficult Airway Management: By: Bereket Habtamu Advisor: Leulayehu AkaluDokumen72 halamanDifficult Airway Management: By: Bereket Habtamu Advisor: Leulayehu AkaluagatakassaBelum ada peringkat
- Airway Management For The Oral Surgery Patient 2018Dokumen20 halamanAirway Management For The Oral Surgery Patient 2018Aldo AguilarBelum ada peringkat
- Emergencias Respiratorias Pediatricas PDFDokumen20 halamanEmergencias Respiratorias Pediatricas PDFMarco Antonio Mendoza OjedaBelum ada peringkat
- Anesthesiology Clinics Volume 32 Issue 2 2014 (Doi 10.1016/j.anclin.2014.02.022) Anderson, Jennifer Klock, P. Allan PDFDokumen17 halamanAnesthesiology Clinics Volume 32 Issue 2 2014 (Doi 10.1016/j.anclin.2014.02.022) Anderson, Jennifer Klock, P. Allan PDFaprinaBelum ada peringkat
- Awake IntubationDokumen35 halamanAwake IntubationEbeneser SitepuBelum ada peringkat
- 269Dokumen4 halaman269Chrasnaya RosaBelum ada peringkat
- Anesthesia NotesDokumen25 halamanAnesthesia NotesReddyBelum ada peringkat
- Need PDFDokumen1 halamanNeed PDFAmirul Ashraf Bin ShukeriBelum ada peringkat
- Imedpub Journals 2018 2018Dokumen6 halamanImedpub Journals 2018 2018jemyBelum ada peringkat
- Airway Emodule - Airway Assessment PDFDokumen6 halamanAirway Emodule - Airway Assessment PDFPreetam PatnalaBelum ada peringkat
- Utilizing Pulmonary Function Parameters To Predict Dysphagia in Individuals With Cervical Spinal Cord InjuriesDokumen9 halamanUtilizing Pulmonary Function Parameters To Predict Dysphagia in Individuals With Cervical Spinal Cord InjuriesElsie Dyana Pretty StephanieBelum ada peringkat
- Article PR 2Dokumen4 halamanArticle PR 2Malak Al SayedBelum ada peringkat
- Jurnal EbmDokumen10 halamanJurnal EbmdeasyBelum ada peringkat
- Clinical Study of Retraction Pockets in Chronic Suppurative Otitis MediaDokumen4 halamanClinical Study of Retraction Pockets in Chronic Suppurative Otitis Mediavivy iskandarBelum ada peringkat
- Best of Best in ENTDokumen34 halamanBest of Best in ENTNagaraj ShettyBelum ada peringkat
- Pulmonary Function TestDokumen7 halamanPulmonary Function TestGhada HusseinBelum ada peringkat
- Academic Emergency Medicine - 2011 - Adhikari - Pilot Study To Determine The Utility of Point of Care Ultrasound in TheDokumen7 halamanAcademic Emergency Medicine - 2011 - Adhikari - Pilot Study To Determine The Utility of Point of Care Ultrasound in TheIndhu SubbuBelum ada peringkat
- Sakle S 2017Dokumen9 halamanSakle S 2017AldyUmasangadjiBelum ada peringkat
- Pediatrics StridorDokumen13 halamanPediatrics StridorEmaBelum ada peringkat
- Anesthesia NotesDokumen25 halamanAnesthesia NotesSaad AbdullahBelum ada peringkat
- Essentials in Lung TransplantationDari EverandEssentials in Lung TransplantationAllan R. GlanvilleBelum ada peringkat
- Normal and Pathological Bronchial Semiology: A Visual ApproachDari EverandNormal and Pathological Bronchial Semiology: A Visual ApproachPierre Philippe BaldeyrouBelum ada peringkat
- Abnormal Uterine Bleeding - Surgical ManagementDokumen14 halamanAbnormal Uterine Bleeding - Surgical ManagementNikhil DevBelum ada peringkat
- 2004 - Quality of Life in Romania I MargineanDokumen206 halaman2004 - Quality of Life in Romania I Margineandale_titiBelum ada peringkat
- Journal of Environmental Management: Ajay Singh TDokumen7 halamanJournal of Environmental Management: Ajay Singh TNestor Garay CahuanaBelum ada peringkat
- 10 de Thi Tieng Anh Hướng Dẫn Giải Chi TiếtDokumen145 halaman10 de Thi Tieng Anh Hướng Dẫn Giải Chi TiếtVuong DiepBelum ada peringkat
- Who Has Allergies & Why: Allergies, Also Known As Allergic Diseases, Are A Number of Conditions Caused byDokumen6 halamanWho Has Allergies & Why: Allergies, Also Known As Allergic Diseases, Are A Number of Conditions Caused byJun Dl CrzBelum ada peringkat
- Compressed Air Pressure Drop DiagramDokumen4 halamanCompressed Air Pressure Drop DiagramycemalBelum ada peringkat
- Final Tana Beles - pdf2222Dokumen72 halamanFinal Tana Beles - pdf2222Tiruneh Yeneneh100% (1)
- First Periodical Exam Math 8Dokumen2 halamanFirst Periodical Exam Math 8Joanne88% (8)
- Testo-Flue Gas in Industry 3-27-2008Dokumen149 halamanTesto-Flue Gas in Industry 3-27-2008leruaitesBelum ada peringkat
- Unit 21Dokumen22 halamanUnit 21Yuni IndahBelum ada peringkat
- N100 Rle Back MassageDokumen24 halamanN100 Rle Back MassagerlinaoBelum ada peringkat
- Peethas ListDokumen1 halamanPeethas ListChetan PrajapatiBelum ada peringkat
- Full Site PDFDokumen23 halamanFull Site PDFpursuwBelum ada peringkat
- 365-M - City Bus Route & Timings, Bangalore (BMTC) Map, First & Last BusDokumen10 halaman365-M - City Bus Route & Timings, Bangalore (BMTC) Map, First & Last BusER Aditya DasBelum ada peringkat
- bNSG9000 Datasheet 2Dokumen3 halamanbNSG9000 Datasheet 2RobertBelum ada peringkat
- 9500 MPR Wireless TransmissionDokumen46 halaman9500 MPR Wireless TransmissionMahdi AhmadiBelum ada peringkat
- CN 235 Aircraft DefinitionDokumen22 halamanCN 235 Aircraft DefinitionMoch Dedy100% (4)
- Danas Si Moja I BozijaDokumen1 halamanDanas Si Moja I BozijaMoj DikoBelum ada peringkat
- IKEA - Huntsman Positive List - 27 May 2016 - EN - FINAL - v1Dokumen30 halamanIKEA - Huntsman Positive List - 27 May 2016 - EN - FINAL - v1Flávia DutraBelum ada peringkat
- CatalogDokumen52 halamanCatalogtalabiraBelum ada peringkat
- Vertical HabitatDokumen6 halamanVertical HabitatAbdul SakurBelum ada peringkat
- ABS Rules For Cable SizingDokumen2 halamanABS Rules For Cable SizingMohammed JassimBelum ada peringkat
- Factory Program Library List v1.0Dokumen9 halamanFactory Program Library List v1.0Ronaldo DamattaBelum ada peringkat
- Worksheet 3 (Partial Pressures)Dokumen2 halamanWorksheet 3 (Partial Pressures)Jose Ruben SortoBelum ada peringkat
- KIN-CN-STU-NW-0001 Puerto Real Towing Study of Kincardine 04Dokumen44 halamanKIN-CN-STU-NW-0001 Puerto Real Towing Study of Kincardine 04RUBEN BARTOLOME GARCIA100% (1)
- Scan&SolveDokumen24 halamanScan&SolveAtul ChauhanBelum ada peringkat
- TCNHS - Diagnostic-test-G8-cookery 7&8Dokumen2 halamanTCNHS - Diagnostic-test-G8-cookery 7&8Elna Grace Dicon-Ybañez100% (4)
- ASD Fan CalculatorsDokumen14 halamanASD Fan CalculatorslubricacionBelum ada peringkat
- Latihan Soal Report TextDokumen28 halamanLatihan Soal Report TextHidayatul HikmahBelum ada peringkat
- Kelvin Hughes LTD: Technical Advice SheetDokumen7 halamanKelvin Hughes LTD: Technical Advice SheetVladymirBelum ada peringkat