Handout Investigation and Management of Continence Issues in The RACF Setting
Diunggah oleh
asmaaarDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Handout Investigation and Management of Continence Issues in The RACF Setting
Diunggah oleh
asmaaarHak Cipta:
Format Tersedia
Investigation and management of continence issues in the aged care facility setting 1.
Definition: Incontinence is a term that describes any accidental or involuntary loss of urine from the bladder (urinary incontinence) or bowel motion, faeces or wind from the bowel (faecal or bowel incontinence). 2. Types Urinary incontinence Urinary incontinence (or poor bladder control) is a common condition, that is commonly associated with pregnancy, childbirth, menopause or a range of chronic conditions such as asthma, diabetes or arthritis. stress incontinence urge incontinence overflow incontinence, functional incontinence. Faecal incontinence Faecal incontinence is a term used to describe leakage from the bowel due to poor bowel control. Causes of faecal incontinence long term straining medications, e.g. antibiotics, drugs for arthritis and diabetes lifestyle, e.g. heavy lifting leading to weak pelvic floor muscles weak back passage muscles due to having babies, getting older, some types of surgery, or radiation therapy diabetes bowel disease, e.g. Coeliac disease, Crohn's disease nerve disorders resulting from MS and Parkinson's severe diarrhoea, or constipation. Complications: Fall Psychosocial effect Skin breakdown and infection around perineum Risk factors for urinary incontinence pregnancy (both pre- and post-natal women) younger women who have had children menopause obesity urinary tract infections constipation specific types of surgery such as prostatectomy (removal of all or part of the prostate) and hysterectomy (removal of all or part of the uterus and/or ovaries) reduced mobility preventing you from getting to or using the toilet neurological and musculoskeletal conditions such as multiple sclerosis and arthritis
health conditions such as diabetes, stroke, heart conditions, respiratory conditions, and prostate problems, and some medications.
Risk factors for faecal incontinence A risk factor for faecal incontinence is urinary incontinence. Other risk factors are similar to those of urinary incontinence, but also include: chronic diarrhoea, and dementia. Screening/ Assessment History, physical examination, investigation/diagnostic evaluation 1. Urinary questions - polyuria >6times/day - nocturia >twice a night - Urine leakage - Dysuria , retention etc - underlying cause of incontinence > determine type of incontinence. 2. Faecal questions - lost control of bowel movements or leakage - other bowel symptoms > constipation or diarrhoea 3. Pad use - using any pads - how often pads may be soiled/wet > use bowel or bladder chart to determine further information. ~fluid consumption, other factors that may interfere; mobility, dementia. Management 1. Eliminate contributing factors (infection, cough, medication) 2. Physical and behavioural mobility aids, assistance, prompted toileting, physio/pelvic floor exercise, bladder training 3. Diet adequate fibre and fluid intake 4. Skin care 5. Medication? > anticholinergic medication in urge incontinence. Avoid anticholinergic agents in people with dementia because of the risk of cognitive decline and delirium Reference 1. What is Incontinence, 2012, Continence Foundation of Australia, <http://www.continence.org.au/pages/urinary-incontinence.html> 2. Dawson C, n.d, The Diagnosis and Management of Urinary Incontinence. 3. NPS Medicine Wise, 2013, Managing Incontinence in Aged Care, <http://agedcare.nps.org.au/clinical_info/feature_topics/topics/managing_urinary_incontinence>
Anda mungkin juga menyukai
- Urinary IncontienceDokumen102 halamanUrinary IncontienceHussein AlhaddadBelum ada peringkat
- Pharma-URO-U IncontinenceDokumen27 halamanPharma-URO-U IncontinenceHussein AlhaddadBelum ada peringkat
- Eliminasi Meliputi Informasi / Riwayat Pasien Pemeriksaan - Pola BAB, BAKDokumen7 halamanEliminasi Meliputi Informasi / Riwayat Pasien Pemeriksaan - Pola BAB, BAKNareswari KenitenBelum ada peringkat
- Background: ConstipationDokumen7 halamanBackground: ConstipationErnesErlyanaSuryawijayaBelum ada peringkat
- ConstipationDokumen37 halamanConstipationHero StoreBelum ada peringkat
- Urinary Incontinence Has Sesven TypesDokumen55 halamanUrinary Incontinence Has Sesven TypesDhonat Flash100% (1)
- Urinary Incontinence: 2 PathophysiologyDokumen8 halamanUrinary Incontinence: 2 PathophysiologyZiedTrikiBelum ada peringkat
- Responses To AlterationsDokumen16 halamanResponses To AlterationsFerlyn BotalonBelum ada peringkat
- Chronic Diarrhea in AdultsDokumen2 halamanChronic Diarrhea in AdultsDr. Ammar KhalilBelum ada peringkat
- Ariel Pemicu 5Dokumen37 halamanAriel Pemicu 5yuliBelum ada peringkat
- ConstipationDokumen2 halamanConstipationMaxamed DananBelum ada peringkat
- Incontinentia Urine: HasnawatyDokumen12 halamanIncontinentia Urine: HasnawatyafatspBelum ada peringkat
- Urinary IncontinenceDokumen17 halamanUrinary IncontinenceMohamed Na3eemBelum ada peringkat
- Bowel EliminationDokumen4 halamanBowel EliminationWarner Yague Pacariem Jr.Belum ada peringkat
- The Complete Guide to Chronic Constipation: Symptoms, Risks, Treatments & CuresDari EverandThe Complete Guide to Chronic Constipation: Symptoms, Risks, Treatments & CuresBelum ada peringkat
- ConstipationDokumen16 halamanConstipationOsama ALGabriBelum ada peringkat
- ConstipationDokumen22 halamanConstipationOsama ALGabriBelum ada peringkat
- Fecal Incontinence Means One Is Not Able To Hold Their FecesDokumen2 halamanFecal Incontinence Means One Is Not Able To Hold Their FecesDesBelum ada peringkat
- Key Urological SymptomsDokumen25 halamanKey Urological SymptomsStella Agatha WidjajaBelum ada peringkat
- C&D FinalDokumen31 halamanC&D Finaledilyntayer106Belum ada peringkat
- Urinary Incontinence - DiagnosisDokumen2 halamanUrinary Incontinence - DiagnosisHoney Roselle MorenoBelum ada peringkat
- NCMB 314 - M2-Cu10Dokumen10 halamanNCMB 314 - M2-Cu10Giselle EstoquiaBelum ada peringkat
- Tugas KMB MenerjemahDokumen6 halamanTugas KMB MenerjemahRi ZaBelum ada peringkat
- Illness Symptoms Reasons Solutions Homemade Solutions Ways To Avoid Such Health IssuesDokumen9 halamanIllness Symptoms Reasons Solutions Homemade Solutions Ways To Avoid Such Health IssuessunilviniBelum ada peringkat
- Urinary Incontinence in Individuals With Diabetes MellitusDokumen1 halamanUrinary Incontinence in Individuals With Diabetes MellitusBulan GhafirahBelum ada peringkat
- Understanding ConstipationDokumen10 halamanUnderstanding ConstipationAndy PurnomoBelum ada peringkat
- Constipation 508Dokumen12 halamanConstipation 508Shishir Kumar SinghBelum ada peringkat
- What Is Constipation?: Diarrhea Irritable Bowel SyndromeDokumen51 halamanWhat Is Constipation?: Diarrhea Irritable Bowel SyndromeDiane Kate Tobias MagnoBelum ada peringkat
- Assessment of The Gastrointestinal SystemDokumen4 halamanAssessment of The Gastrointestinal SystemAvery SandsBelum ada peringkat
- كوزرملا حاضو .د .م.أ لباب ةعماج/ بطلا ةيلك 2019 Urinary Incontinence. Involuntary loss of urine in sufficient amount or frequency to constituteDokumen8 halamanكوزرملا حاضو .د .م.أ لباب ةعماج/ بطلا ةيلك 2019 Urinary Incontinence. Involuntary loss of urine in sufficient amount or frequency to constitutewzeer mohammedBelum ada peringkat
- Fecal IncontinenceDokumen5 halamanFecal IncontinenceDaniel Galindo SotomayorBelum ada peringkat
- Gouty ArthritisDokumen5 halamanGouty ArthritisLorebell100% (3)
- Geriatric Urinary Incontinence & UTI CaseDokumen9 halamanGeriatric Urinary Incontinence & UTI CaseStarr NewmanBelum ada peringkat
- Overview of Urinary Incontinence (UI) in The Long Term Care FacilityDokumen81 halamanOverview of Urinary Incontinence (UI) in The Long Term Care Facilityالغزال الذهبيBelum ada peringkat
- Caused Abdominal DistensionDokumen20 halamanCaused Abdominal Distensionstella pangestikaBelum ada peringkat
- Anatomy and Physiology of The BowelDokumen10 halamanAnatomy and Physiology of The BowelholzzBelum ada peringkat
- 01Dokumen12 halaman01whackjack_696977Belum ada peringkat
- FecalincontinanceDokumen17 halamanFecalincontinancerabiullah.edu987Belum ada peringkat
- Case Study For Chronic Renal FailureDokumen6 halamanCase Study For Chronic Renal FailureGabbii CincoBelum ada peringkat
- Diverticulosis, A Simple Guide to the Condition, Treatment and Related DiseasesDari EverandDiverticulosis, A Simple Guide to the Condition, Treatment and Related DiseasesPenilaian: 1 dari 5 bintang1/5 (1)
- Neurogenic BowlDokumen21 halamanNeurogenic BowlFaridatul IsniyahBelum ada peringkat
- Constipation: How To Treat Constipation: How To Prevent Constipation: Along With Nutrition, Diet, And Exercise For ConstipationDari EverandConstipation: How To Treat Constipation: How To Prevent Constipation: Along With Nutrition, Diet, And Exercise For ConstipationBelum ada peringkat
- Dysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsDari EverandDysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsPenilaian: 5 dari 5 bintang5/5 (1)
- 1 DeferactionDokumen9 halaman1 Deferactiondesign bahana bahana proBelum ada peringkat
- Postpartum HemorrhageDokumen25 halamanPostpartum Hemorrhagejam100% (1)
- CKD CaseDokumen2 halamanCKD CasePatricia Kaye Tayag CastroBelum ada peringkat
- Chronic DiarrhoeaDokumen9 halamanChronic DiarrhoeaDennis CobbBelum ada peringkat
- Cu Task 11 Urinary ProblemsDokumen5 halamanCu Task 11 Urinary ProblemsSamsung Note 9Belum ada peringkat
- Constipation (Sembelit)Dokumen8 halamanConstipation (Sembelit)Eki MegaraniBelum ada peringkat
- Constipation: Ekaterine Labadze MDDokumen24 halamanConstipation: Ekaterine Labadze MDsushant jainBelum ada peringkat
- Quiz of Urinary IncontinenceDokumen4 halamanQuiz of Urinary IncontinenceTiffanny Ocktivianie TobingBelum ada peringkat
- NCM 116 NB - Care of Clients With Problem in Nutrition and Gi, Metabolism and Endocrine, PerceptionDokumen4 halamanNCM 116 NB - Care of Clients With Problem in Nutrition and Gi, Metabolism and Endocrine, PerceptionSureen RegularBelum ada peringkat
- Constipation: Group 5Dokumen9 halamanConstipation: Group 5Iremide OlayemiBelum ada peringkat
- Urinary IncontinenceDokumen12 halamanUrinary IncontinenceAmrit Preet KaurBelum ada peringkat
- ConstipationDokumen12 halamanConstipationfrechel kimBelum ada peringkat
- Constipation in The Elderly - American Family PhysicianDokumen9 halamanConstipation in The Elderly - American Family PhysicianMudassar SattarBelum ada peringkat
- Inkontinensia UrinDokumen2 halamanInkontinensia UrinYoh Spy 朝倉Belum ada peringkat
- About Urinary IncontinenceDokumen6 halamanAbout Urinary IncontinenceRitesh SinghBelum ada peringkat
- Polycystic Kidneys, A Simple Guide To The Condition, Treatment And Related DiseasesDari EverandPolycystic Kidneys, A Simple Guide To The Condition, Treatment And Related DiseasesBelum ada peringkat
- Ferrara 2017Dokumen5 halamanFerrara 2017nurharyanti darmaningtyasBelum ada peringkat
- Incontinencia Urinaria Fisiopatologia The Clinics PDFDokumen12 halamanIncontinencia Urinaria Fisiopatologia The Clinics PDFOmar Teran LinaresBelum ada peringkat
- Festival of Wreaths Will Kick Off Holiday Season: Glenridge Hosts Bestselling Author and Columnist at Book FestivalDokumen16 halamanFestival of Wreaths Will Kick Off Holiday Season: Glenridge Hosts Bestselling Author and Columnist at Book Festivalgray4801Belum ada peringkat
- Vaginal FistulaDokumen3 halamanVaginal FistulaDaryl TarucBelum ada peringkat
- Xylocaine Jelly Cil enDokumen4 halamanXylocaine Jelly Cil enRavi KumarBelum ada peringkat
- Flash On: English For NursingDokumen16 halamanFlash On: English For NursingNarcisaBelum ada peringkat
- Maternal ExamsDokumen37 halamanMaternal ExamsMarianne Baquilala100% (2)
- BISA Presentasi IUGA BaliDokumen2 halamanBISA Presentasi IUGA BaliBudi Iman SantosoBelum ada peringkat
- Geriatric CareDokumen24 halamanGeriatric CareDr. Jayesh Patidar0% (1)
- Cystocele & RectoceleDokumen22 halamanCystocele & RectocelefincyjosephcmcBelum ada peringkat
- Neurological DisordersDokumen117 halamanNeurological DisordersMohammed JawadBelum ada peringkat
- Urological History TakingDokumen6 halamanUrological History TakingayuniBelum ada peringkat
- Rehabilitation Concepts For Chronic and Disabling Health ProblemsDokumen59 halamanRehabilitation Concepts For Chronic and Disabling Health ProblemsBammary88909Belum ada peringkat
- Gordons Functional PatternDokumen3 halamanGordons Functional PatternGee Villa100% (5)
- NLE - Practice TestsDokumen25 halamanNLE - Practice TestsBen0% (1)
- Martinez Et Al V Mentor Worldwide LLC Et AlDokumen56 halamanMartinez Et Al V Mentor Worldwide LLC Et AlKenneth SandersBelum ada peringkat
- Functional Health PatternsDokumen6 halamanFunctional Health PatternsBrianne SheldonBelum ada peringkat
- Benign Prostatic HyperplasiaDokumen55 halamanBenign Prostatic HyperplasiaJeffrey DyerBelum ada peringkat
- Nursing ExamDokumen117 halamanNursing ExamticticBelum ada peringkat
- Evidence-Based Guidelines For Best Practice in Urological Health Care: Catherisation Indwelling Catheters in Adults (Urethral and Suprapubic)Dokumen114 halamanEvidence-Based Guidelines For Best Practice in Urological Health Care: Catherisation Indwelling Catheters in Adults (Urethral and Suprapubic)cateterdoblejota100% (2)
- Elimination Needs 04Dokumen52 halamanElimination Needs 04Kishore RathoreBelum ada peringkat
- BMJ 22-09Dokumen15 halamanBMJ 22-09Kiran ShahBelum ada peringkat
- 1 - Physical AssessmentDokumen63 halaman1 - Physical AssessmentMohamed OmarBelum ada peringkat
- A Nurse-Driven Process For TimelyDokumen7 halamanA Nurse-Driven Process For TimelyWardah Fauziah El SofwanBelum ada peringkat
- 8 Steps To A Healthy PregnancyDokumen4 halaman8 Steps To A Healthy Pregnancybeverly-cope-6067Belum ada peringkat
- Evidence Based PostpartumDokumen75 halamanEvidence Based PostpartumAnnisatus SholehahBelum ada peringkat
- The Illustrious Jade Egg EbookDokumen63 halamanThe Illustrious Jade Egg EbookAndre Silva100% (3)
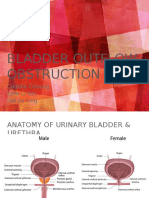
- BLadder Outlet ObstructionDokumen28 halamanBLadder Outlet ObstructionCodillia Cheong100% (1)
- Jurnal RevyDokumen6 halamanJurnal Revyobgin januari19Belum ada peringkat
- A Case Study of Urinary Incontinence Treated With AcupunctureDokumen5 halamanA Case Study of Urinary Incontinence Treated With AcupunctureHerald Scholarly Open AccessBelum ada peringkat
- Fundamental Nursing PracticeDokumen23 halamanFundamental Nursing PracticeChristine MagbataBelum ada peringkat