Immunization Schedule Updates and Vaccine Options
Diunggah oleh
Abu Furqan FakhrurraziDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Immunization Schedule Updates and Vaccine Options
Diunggah oleh
Abu Furqan FakhrurraziHak Cipta:
Format Tersedia
1
Immunizations
David Kramer, M.D.
2
Changes in the 1997 Immunization Schedule
# Incorporation of inactivated polio vaccination (IPV)
# Use of DTaP
# Combination vaccines: DTaP/Hib conjugate, HBV/Hib
# Initiation of HBV at any age
# Second MMR is given at 4-6 yrs
# Adolescent visit vaccinations are recommended
3
Polio: Background
# Inapparent infection: paralytic disease 1:100-1000
# Case fatality rate in paralytic polio is 2-10%.
# Goal of global eradication by year 2000
Last wild-type case occurred in the Americas in 1991; last imported case
was detected in 1993
Western hemisphere has been free of indigenous polio virus since 1994
# Vaccine associated paralytic polio (VAPP) is the only indigenous form of
disease in the US since 1979; 8-9 cases per year are detected.
4
Advantages and Disadvantages of the Three
Poliovirus Vaccination Options
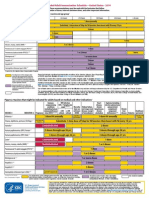
Attribute OPV* IPV IPV-OPV in Sequence
Occurrence of VAPP 8-9 cases/yr None 2-5 cases/yr
Other serious adverse events None known None known None known
Systemic immunity High High High
Immunity of GI mucosa High Low High
Secondary transmission of Yes No Some
vaccine virus
Extra injections or visits No Yes Yes
needed
Compliance with immunization High Possibly reduced Possibly reduced
schedule
Current cost Low Higher Intermediate
5
Options For Providing Poliovirus Vaccine
1. Sequential use of IPV and OPV (preferred by ACIP)
Estimated 95% reduction in vaccine associated paralytic polio (VAPP)
amongst recipients
Predicted reduction in VAPP amongst household and community
contracts
Continued use of OPV induces intestinal immunity and resistance to
transmission of wild type virus if reintroduced
Fewer injections in the second year of life
2. IPV Only (IPOL, Poliovax)
Immunocompromised persons or recipients of immunosuppressive
chemotherapy and their household contacts
Children for whom adult household members are inadequately immu-
nized against polio.
3. OPV Only
Preference to minimize number of injections
Initiation of vaccination regimen after 6 months of age
Children for whom accelerated protection is required if OPV not
contraindicated
Contraindicated for primary vaccination of persons >18 years of age
6
Acellular Pertussis Vaccine Antigens
# Included in all acellular pertussis vaccines: inactivated pertussis toxoid
(PT)
# Variation in inclusion and concentration:
Filamentous hemagglutinin (FHA)
pertactin (PRN)
non-fimbrial protein (69-kd OMP)
2 fimbrial proteins (FIM types 2 and 3)
7
DTP Adverse Events that are Decreased With
DTaP
# Minor Reactions: Local reactions, drowsiness, irritability, anorexia, fever
# Serious Reactions: Hypotonic-hyporesponsive episodes (HHE), persis-
tent crying >3 hrs, temp >40E C, seizures
# The effect of vaccine on the incidence of rare adverse events of immedi-
ate anaphylaxis or encephalopathy within 7 days is unknown.
8
Recommend Use of Pertussis Vaccine
# DTaP is preferred for 5 doses, beginning at 6-8 weeks of age; DTP is an
acceptable alternative in transition
# DTaP can be used to complete regimen in children who received DTP
previously.
# DTaP is recommended if immunization is to be completed in those with a
history of serious DTP event.
# True Contraindications to Pertussis Vaccine
Encephalopathy: DT is recommended
Anaphylaxis: DT should be deferred; consider allergy testing and
desensitization.
9
Pertussis Vaccine: Special Considerations
# Personal or Family History of Seizures
- DTaP is the vaccine of choice for these patients.
- Personal history of seizures: Delay administration until the neuro-
logic condition is stable.
- Family history of seizures is not a contraindication.
- Acetaminophen should be given q4h x 24 hrs after the vaccination.
# # History of Pertussis Disease: DT is given for all; DTaP is recom-
mended by some experts
# 7 years of age: Reformulation is required for adults because diptheria
toxoid content is too high for persons older than 7 years.
10
Combination Vaccines
# Benefit. Minimize number of injections, thereby decreasing associated
pain, costs, provider visits, decreased compliance
# Problems
Need to stock many different products
Potential for extra vaccinations, increased costs,
Decreased reimbursement
Tracking problems, especially with frequently changing health care
providers
11
Combination Vaccine Types
# # Diphtheria, Tetanus, Acellular Pertussis (DTaP)
Tripedia, Infanrix licensed for first 4 doses
ACEL-IMUNE licensed for all 5 doses
TriHIBit (ActHIB reconstituted with Tripedia) licensed only for the 4th
dose of the series
Recommendations: Use same product to complete series whenever
possible; any of the licensed products may be used to complete series
when previous information unavailable
# Hib-Hep B (COMVAX)
Monovalent Pedvax HIB and monovalent RECOMBIVAXHB
.
Most efficient for immunization of infants of HBs Ag negative women
whose Hep B vaccine may safely be deferred until 2 months of age.
Birth dose of Hep B enhances protection in infants of HBs Ag pos
women.
Extra dose (at birth) of Hep B required in absence of screening or if
mother HBs Ag positive.
12
Prevention of Perinatal HBV Infection
# Risk of Perinatal Transmission
- Hb Ag pos 70-90%
e
- Hb Ag neg 10-25%
e
# Sequelae of Perinatal Infection
- Chronic infection in 90%
- Death caused by chronic liver disease in 25%
# Increased risk of horizontal transmission in first 5 years of life
# Universal screening of pregnant women for HBs Ag
Repeat late in pregnancy if high risk
Screen at delivery if HBs Ag unknown
# Infants of HBs Ag positive mothers: HBIG and hep B vaccine within 12
hours of birth.
13
Immunizations at the Adolescent Visit
# Establish visit to provider age 11-12 for immunization and other preven-
tive services
# Vaccines for all adolescents
Hepatitis B, MMR (2nd dose), varicella, Td
Td booster now may be given at 11-12 or 14-16 y
# Vaccines for adolescents at high risk for specific infections
Influenza
Pneumococcal
Hepatitis A
14
Varicella Vaccine
# # Sequelae of Varicella Infection
Complications: 150,000-200,000/yr
Hospitalizations: 5,000-6,500/yr severe GAS, MRSA recently
Deaths: 100/yr
4-15 times higher complication rates, especially in adults
# Efficacy of Vaccination
95% effective against severe disease
70-80% complete protection for 10 yrs
# Vaccine-related Epidemiologic Changes
Persistent immunity has been documented for 20 years in Japan and
for ten years in United States.
Unknown effect of absence of circulating while varicella virus.
Potential need for adolescent booster.
Universal childhood immunization required to prevent shift.
# The risk of zoster is reduced by vaccination.
# Transmission of Vaccine Virus to Contacts
infection, but not significant disease may be transmitted to close
contacts.
The risk is decreased compared with wild type varicella virus in sus-
ceptible persons.
15
Adverse Effects of Varicella Vaccine
12 months-12 years >13 years
Adverse Effect dose 1 dose 2
Fever 14.7 % 10.2% 9.5%
Injection site pain 19.3% 24.1% 32.5%
Varicella rash at injec- 3.4% 3.0% 1.0%
tion site (8-19 days)
Non-localized varicella 3.8% 5.5% 0.9%
rash (5-26 days)
Febrile seizures <0.1% N.A. N.A.
16
Consequences of Influenza in Children
# The attack rates among healthy children is 10-40%, and hospitalization
occurs in 1%.
# Risk of pneumonia or bronchiolitis is 0.2-25%.
# Other complications include myositis and encephalitis.
# Excessive rates of hospitalization occur for neonates or children with
sickle cell disease, bronchopulmonary dysplasia, asthma, cystic fibrosis,
malignancies, diabetes, chronic renal disease, cyanotic heart disease.
# Children may transmit into influenza to high-risk household members.
# Infection is associated with an increased morbidity in pregnancy after the
first trimester.
17
Influenza Vaccine
# Inactivated whole cell virus vaccine is produced in embryonated eggs.
Subvirion or purified surface antigen vaccines (i.e., split virus vaccines)
are used in children <13 years of age.
# Vaccine strains change each year.
# Efficacy at > six months of age is 70-80%.
# Adverse events
Febrile reactions occur at 6-24 hours most frequently in children < 2
years of age 6.
Local reactions occur in 10 % over 13 years of age.
Guillain-Barre syndrome is not associated with influenza immunization
in children.
18
Influenza Vaccine Recommendations
# Targeted high-risk groups: Asthma, chronic lung disease,
hemodynamically significant cardiac disease, sickle cell anemia,
hemoglobinopathies.
# Other high-risk groups that may be vaccinated: HIV infection/AIDS,
diabetes mellitus, chronic renal disease, metabolic diseases, recipients of
long-term aspirin therapy, members of households with high-risk adults.
# Vaccination may be considered in families who desire to decrease illness
even in no risk factors for severe disease.
19
Hepatitis A Vaccine: Epidemiology
Incidence 1994
- 26,796 cases reported
- estimated 80,000 cases/134,000 infections
# 30% reported cases <15 yrs of age
Serologic evidence of prior infection of U.S. 33%
Source of infection
- household or sexual contact 22-26%
- day care center 14-16%
- international travelers 4-6%
- food/waterborne outbreaks 2-3%
- no identifiable source 50%
# Case fatality rate 0.3%; 1.8% >50 yrs of age
20
Hepatitis A Vaccine Administration
# Inactivated: HAVRIX, VAQTA
# Dosage Schedule 2-18 yrs
- 0, 6-12 mos
- Concentration doubled >17, 18 yrs
# Efficacy: 94-100%
# Effective in chimps post-exposure
# Duration of Protection
Documented 3 years
Estimated to be 20 years or longer
21
Indications for Hepatitis A Vaccine >2 Yrs
# Travel to work in a country with high or intermediate rate of endemic
infection
# Reside in a community with a high rate of infection and periodic out-
breaks
# Recipients of clotting factor concentrates
# Chronic liver disease
# High risk occupation:
Exposure to HAV-infected primates, HAV research
Some food handlers
# High risk behaviors: Illegal drug users, men who have sex with men
22
Immunizations in Individuals With Egg Hyper-
sensitivity
# Vaccines containing egg proteins: Measles, mumps, influenza, yellow
fever
# Anaphylactic reactions following MMR are more likely related to other
antigens (eg, neomycin, gelatin).
# Skin-testing with vaccine is not predictive of allergic reaction to vaccine.
# Children with egg hypersensitivity may receive a routine dose of MMR
without preliminary skin testing; 90 minutes observation in a clinic with
emergency treatment available is recommended.
23
Vaccine Classification: Live or Inactivated
Live Inactivated
OPV DTP, DTaP, DT, Td
MMR IPV
Varicella HBV
BCG Hib
Typhoid-oral Influenza
Pneumococcal
Meningococcal
Rabies
Cholera
Anda mungkin juga menyukai
- Health Advice and Immunizations for TravelersDari EverandHealth Advice and Immunizations for TravelersBelum ada peringkat
- Pediatric Primary CareDokumen66 halamanPediatric Primary Carefairwoods100% (1)
- Measles and Measles Vaccine Epidemiology and PreventionDokumen18 halamanMeasles and Measles Vaccine Epidemiology and PreventionMar OrdanzaBelum ada peringkat
- Infectious Rubella-4 (Muhadharaty)Dokumen5 halamanInfectious Rubella-4 (Muhadharaty)dr.salam.hassaniBelum ada peringkat
- Iap Guide Book On Immunization Immunization in Special Situations PDFDokumen8 halamanIap Guide Book On Immunization Immunization in Special Situations PDFGirdhari Lal Saini100% (1)
- Pediatric HIV/AIDS: Transmission, Clinical Presentation and ManagementDokumen60 halamanPediatric HIV/AIDS: Transmission, Clinical Presentation and Managementmy Lord JesusBelum ada peringkat
- Immunization and Prophylaxis: Childhood Immunization Has Reduced The Impact - Active Immunization Is TheDokumen18 halamanImmunization and Prophylaxis: Childhood Immunization Has Reduced The Impact - Active Immunization Is TheCabdiBelum ada peringkat
- ImmunizationDokumen60 halamanImmunizationleekabrams11Belum ada peringkat
- CPG on Immunization for WomenDokumen28 halamanCPG on Immunization for WomenYnoli DiosomitoBelum ada peringkat
- Immunization Review GPDokumen46 halamanImmunization Review GPKishore ChandkiBelum ada peringkat
- Dr. Ali's Uworld Notes For Step 2 CKDokumen30 halamanDr. Ali's Uworld Notes For Step 2 CKuyesBelum ada peringkat
- Updates in Iraq national immunization program adds rotavirus vaccineDokumen36 halamanUpdates in Iraq national immunization program adds rotavirus vaccineHusain TamimieBelum ada peringkat
- 1 CombineDokumen726 halaman1 CombineSong Hành Vạn KiếpBelum ada peringkat
- Immunization: Mei Neni S Pediatric Dept. Faculty of Medicine, Gadjah Mada UniversityDokumen35 halamanImmunization: Mei Neni S Pediatric Dept. Faculty of Medicine, Gadjah Mada UniversityadystiBelum ada peringkat
- PAIDSDokumen85 halamanPAIDSw8hxmsvmfzBelum ada peringkat
- DR - Dinesh AgarwalDokumen20 halamanDR - Dinesh AgarwalPushpanjali Crosslay HospitalBelum ada peringkat
- Human Immunodeficiency Virus (Hiv) : Presenter-Dr. Shasidhar ReddyDokumen81 halamanHuman Immunodeficiency Virus (Hiv) : Presenter-Dr. Shasidhar ReddyshravaniBelum ada peringkat
- Malaria & ComorbidDokumen33 halamanMalaria & ComorbidSisilia AlfinaBelum ada peringkat
- Adult ImmunizationDokumen6 halamanAdult ImmunizationAmit GoelBelum ada peringkat
- VaccinationDokumen64 halamanVaccinationnancymhd99Belum ada peringkat
- Vaccination For PregnantDokumen126 halamanVaccination For Pregnantfenan sollanoBelum ada peringkat
- Polio and Polio VaccineDokumen34 halamanPolio and Polio Vaccinevivekmalik420Belum ada peringkat
- Varicella (Chickenpox) Disease: Chananart Yuakyen: IcnDokumen28 halamanVaricella (Chickenpox) Disease: Chananart Yuakyen: IcnKana FajarBelum ada peringkat
- 2 Mumps, RubellaDokumen35 halaman2 Mumps, Rubellaمصطفى رسول هاديBelum ada peringkat
- Pediatric ImmunizationDokumen33 halamanPediatric ImmunizationAlaa Rached Khalid AlmekdadBelum ada peringkat
- Influenza (Flu) Vaccine: DR Vineet Jain Pushpanjali Crosslay HospitalDokumen24 halamanInfluenza (Flu) Vaccine: DR Vineet Jain Pushpanjali Crosslay HospitalPushpanjali Crosslay HospitalBelum ada peringkat
- Pediatric Hiv/Aids: Kussia.A (MD)Dokumen62 halamanPediatric Hiv/Aids: Kussia.A (MD)Yemata HailuBelum ada peringkat
- Childhood Immunization ScheduleDokumen59 halamanChildhood Immunization SchedulejaehankimBelum ada peringkat
- Measles, Mumps and RubellaDokumen45 halamanMeasles, Mumps and RubellaKURBULDKBelum ada peringkat
- Herpes ZosterDokumen26 halamanHerpes ZosterFajar AbdurrahmanBelum ada peringkat
- 1-Measles (Rubeola) PDFDokumen37 halaman1-Measles (Rubeola) PDFمصطفى رسول هاديBelum ada peringkat
- Intra-Uterine and Perinatal InfectionDokumen72 halamanIntra-Uterine and Perinatal InfectionsabrinaBelum ada peringkat
- WHO PP Varicella Herpes Zoster June2014 PresentationDokumen29 halamanWHO PP Varicella Herpes Zoster June2014 PresentationMicki TaryanBelum ada peringkat
- Adult Schedule 11x17Dokumen2 halamanAdult Schedule 11x17lcmurilloBelum ada peringkat
- Immunization PDFDokumen9 halamanImmunization PDFwel2332Belum ada peringkat
- Almostadoctor - Co.uk-Vaccination Schedule UKDokumen6 halamanAlmostadoctor - Co.uk-Vaccination Schedule UKIbrahim FoondunBelum ada peringkat
- Types of ImmunizationsDokumen21 halamanTypes of Immunizationsmacmactongos100% (6)
- Hiv/ Human Immunodeficiency Virus/Aids-Acquired Immunodeficiency SyndromeDokumen16 halamanHiv/ Human Immunodeficiency Virus/Aids-Acquired Immunodeficiency SyndromeNiña Ricci MtflcoBelum ada peringkat
- Adult ScheduleDokumen3 halamanAdult SchedulelcmurilloBelum ada peringkat
- Ob 1.05 Clinical Practice Guidelines On Immunization For Filipino WomenDokumen7 halamanOb 1.05 Clinical Practice Guidelines On Immunization For Filipino Womenotartil_niman50% (2)
- Section Only Full Guideline Recommendations Only Tables Only Drug Tables OnlyDokumen4 halamanSection Only Full Guideline Recommendations Only Tables Only Drug Tables OnlyKhadar BashaBelum ada peringkat
- Influenza Bhasa InggrisDokumen11 halamanInfluenza Bhasa InggrisandiniBelum ada peringkat
- MKSAP 16 - Infectious DiseaseDokumen340 halamanMKSAP 16 - Infectious DiseaseBacanator75% (4)
- Adult ScheduleDokumen3 halamanAdult ScheduleerilarchiBelum ada peringkat
- HIV and ChildrenDokumen32 halamanHIV and ChildrenzidabyBelum ada peringkat
- HIV in ChildrenDokumen11 halamanHIV in ChildrenVaibhav KrishnaBelum ada peringkat
- Drug Therapy: Patient EducationDokumen2 halamanDrug Therapy: Patient EducationJustine Bianca NayreBelum ada peringkat
- Community Health Nursing (Learning Feedback Diary (LFD #25)Dokumen3 halamanCommunity Health Nursing (Learning Feedback Diary (LFD #25)Angelica Malacay RevilBelum ada peringkat
- HIV in PregnancyDokumen28 halamanHIV in PregnancyRaja100% (1)
- Salmonellosis: Condes Dela Cruz ZapataDokumen31 halamanSalmonellosis: Condes Dela Cruz ZapatafuriouspauBelum ada peringkat
- Kepi Vaccines (2) - Gi - 1Dokumen30 halamanKepi Vaccines (2) - Gi - 1okwadha simionBelum ada peringkat
- Varicella and Varicella VaccineDokumen37 halamanVaricella and Varicella VaccineAmudhan MurugesanBelum ada peringkat
- Child Health Program OrientationDokumen143 halamanChild Health Program OrientationKayeBelum ada peringkat
- Immunisation - 4th Yr Feb2022Dokumen49 halamanImmunisation - 4th Yr Feb2022Omar HamwiBelum ada peringkat
- Dr. Elham Bukhari: Aediatri Nfectious IseaseDokumen56 halamanDr. Elham Bukhari: Aediatri Nfectious IseaseJim Jose AntonyBelum ada peringkat
- Pneumococcal Conjugate: VaccineDokumen2 halamanPneumococcal Conjugate: VaccineJenny TaylorBelum ada peringkat
- Multi Vaccine InfantsDokumen3 halamanMulti Vaccine InfantsRahul MukherjeeBelum ada peringkat
- Typhoid and Paratyphoid FeverDokumen17 halamanTyphoid and Paratyphoid FeverGusti ABBelum ada peringkat
- Peds InfectiousDokumen8 halamanPeds InfectiousMohammad RammalBelum ada peringkat
- VXKVNXKVNXKVNXVDokumen1 halamanVXKVNXKVNXKVNXVAbu Furqan FakhrurraziBelum ada peringkat
- JefjsfbswjhwDokumen1 halamanJefjsfbswjhwAbu Furqan FakhrurraziBelum ada peringkat
- OisgishgiosddDokumen1 halamanOisgishgiosddAbu Furqan FakhrurraziBelum ada peringkat
- KJHDJKHDBSDHVBDHJVBDokumen9 halamanKJHDJKHDBSDHVBDHJVBAbu Furqan FakhrurraziBelum ada peringkat
- KGJDKSKFSJDokumen1 halamanKGJDKSKFSJAbu Furqan FakhrurraziBelum ada peringkat
- Hsvhdlvhfhblbhsdvnik HsvhdlvhfhblbhsdvnikDokumen3 halamanHsvhdlvhfhblbhsdvnik HsvhdlvhfhblbhsdvnikAbu Furqan FakhrurraziBelum ada peringkat
- KGJDKSKFSJDokumen1 halamanKGJDKSKFSJAbu Furqan FakhrurraziBelum ada peringkat
- KJGSKFSKFMSKDokumen1 halamanKJGSKFSKFMSKAbu Furqan FakhrurraziBelum ada peringkat
- KJKXCBKJBKHXGKDokumen3 halamanKJKXCBKJBKHXGKAbu Furqan FakhrurraziBelum ada peringkat
- Learn about wubfasFHEUIFGASVJSOVHSOVDokumen3 halamanLearn about wubfasFHEUIFGASVJSOVHSOVAbu Furqan FakhrurraziBelum ada peringkat
- Hsvhdlvhfhblbhsdvnik HsvhdlvhfhblbhsdvnikDokumen4 halamanHsvhdlvhfhblbhsdvnik HsvhdlvhfhblbhsdvnikAbu Furqan FakhrurraziBelum ada peringkat
- Hsvhdlvhfhblbhsdvnik HsvhdlvhfhblbhsdvnikDokumen3 halamanHsvhdlvhfhblbhsdvnik HsvhdlvhfhblbhsdvnikAbu Furqan FakhrurraziBelum ada peringkat
- Wubfasfheuifgasvjsovhsov WubfasfheuifgasvjsovhsovDokumen4 halamanWubfasfheuifgasvjsovhsov WubfasfheuifgasvjsovhsovAbu Furqan FakhrurraziBelum ada peringkat
- Hsvhdlvhfhblbhsdvnik HsvhdlvhfhblbhsdvnikDokumen8 halamanHsvhdlvhfhblbhsdvnik HsvhdlvhfhblbhsdvnikAbu Furqan FakhrurraziBelum ada peringkat
- The Australian and New Zealand Burn AssociationDokumen97 halamanThe Australian and New Zealand Burn AssociationZarah Alifani Dzulhijjah100% (1)
- Order ReceivedDokumen1 halamanOrder ReceivedAbu Furqan FakhrurraziBelum ada peringkat
- Coping With CaregivingDokumen0 halamanCoping With CaregivingAbu Furqan FakhrurraziBelum ada peringkat
- PediatricsDokumen79 halamanPediatricsapi-3712326Belum ada peringkat
- A Case of Neuromyelitis Optica (Devic's Disease)Dokumen3 halamanA Case of Neuromyelitis Optica (Devic's Disease)Keisha QuinnBelum ada peringkat
- A Case of Neuromyelitis Optica (Devic's Disease)Dokumen3 halamanA Case of Neuromyelitis Optica (Devic's Disease)Keisha QuinnBelum ada peringkat
- Okeechobee County School District 2021-22 Health & Safety ProtocolDokumen3 halamanOkeechobee County School District 2021-22 Health & Safety ProtocolPeterBurkeBelum ada peringkat
- Regents Cells and Human BodyDokumen8 halamanRegents Cells and Human Bodyapi-303120399Belum ada peringkat
- NCM 104 - M6 - DOH Programs Related To Family HealthDokumen4 halamanNCM 104 - M6 - DOH Programs Related To Family HealthJollan Marie Buenvenida0% (1)
- Pneumovax PiDokumen9 halamanPneumovax PipisucamiBelum ada peringkat
- Medicine Update 2021 Section 12Dokumen161 halamanMedicine Update 2021 Section 12Huda AminBelum ada peringkat
- T 249 - RespondentDokumen49 halamanT 249 - Respondentparth singh pariharBelum ada peringkat
- Notification of Vaccination Letter Template: Vaccines AdministeredDokumen1 halamanNotification of Vaccination Letter Template: Vaccines AdministeredJacob BuckBelum ada peringkat
- Poxviridae: In: A Concise Review of Veterinary Virology, Carter G.R., Wise D.J. and Flores E.F. (Eds.) - A3410.1005Dokumen10 halamanPoxviridae: In: A Concise Review of Veterinary Virology, Carter G.R., Wise D.J. and Flores E.F. (Eds.) - A3410.1005Mestesanu ElisabetaBelum ada peringkat
- Empowerment Technology: Concept Paper ofDokumen2 halamanEmpowerment Technology: Concept Paper ofMary Jane QuijadaBelum ada peringkat
- Global Health Signature Assignment 1Dokumen9 halamanGlobal Health Signature Assignment 1api-534299459Belum ada peringkat
- GCSE Biology - Vaccines - Worksheet AnswersDokumen2 halamanGCSE Biology - Vaccines - Worksheet Answerspangkwan wongprangBelum ada peringkat
- Vaccines - From Concept To Clinic - L. Paoletti, P. McInnes (CRC, 1999) WW PDFDokumen210 halamanVaccines - From Concept To Clinic - L. Paoletti, P. McInnes (CRC, 1999) WW PDFPatriciaBelum ada peringkat
- Reading Practice - 341-408Dokumen68 halamanReading Practice - 341-408El Tea DeeBelum ada peringkat
- MMRDokumen2 halamanMMRShrinivas YuvanBelum ada peringkat
- Emerging Re-Emerging Infectious Disease 2022Dokumen57 halamanEmerging Re-Emerging Infectious Disease 2022marioBelum ada peringkat
- Vaccinations - Dr. Thomas CowanDokumen5 halamanVaccinations - Dr. Thomas Cowanandrogynus71% (7)
- Dr. Ravi MalikDokumen16 halamanDr. Ravi Malikkaabhay8866Belum ada peringkat
- AQA Biol A Unit 3 Jan02Dokumen16 halamanAQA Biol A Unit 3 Jan02woodirocksBelum ada peringkat
- Letter From Doctors To APSDokumen2 halamanLetter From Doctors To APSJustin HinkleyBelum ada peringkat
- Epidemiology and Infection PreventionDokumen32 halamanEpidemiology and Infection Preventionbkbaljeet116131Belum ada peringkat
- Community Medicine GuideDokumen23 halamanCommunity Medicine GuideSohaib Ahmed44% (9)
- HA Drug Formulary - External List v13.4 - 180414Dokumen17 halamanHA Drug Formulary - External List v13.4 - 180414AikBelum ada peringkat
- 980 Final PushDokumen10 halaman980 Final Pushapi-2375055830% (2)
- Protozoa and Fungi Culturing in The LabDokumen7 halamanProtozoa and Fungi Culturing in The LabrorenBelum ada peringkat
- September 9-15, 2012Dokumen24 halamanSeptember 9-15, 2012Bikol ReporterBelum ada peringkat
- Hesc 102Dokumen15 halamanHesc 102Aryansh AryanshBelum ada peringkat
- Jane - Lecture of Typology and Coping IndexDokumen14 halamanJane - Lecture of Typology and Coping IndexArmySapphireBelum ada peringkat
- Assessment of Knowledge, Attitudes and Practices of Mothers in Jos North Regarding ImmunizationDokumen9 halamanAssessment of Knowledge, Attitudes and Practices of Mothers in Jos North Regarding ImmunizationUlil Amri Pramadani100% (1)
- Vaccine PreservationsDokumen2 halamanVaccine PreservationsAlphonsius WongBelum ada peringkat
- Ethical Issues in HIV Vaccine Trial (Notes)Dokumen63 halamanEthical Issues in HIV Vaccine Trial (Notes)Nuur Mursyiidah MuhammadBelum ada peringkat