A Case Report of A Very Late
Diunggah oleh
Fathia RachmatinaJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
A Case Report of A Very Late
Diunggah oleh
Fathia RachmatinaHak Cipta:
Format Tersedia
A Case Report of a Very Late-Onset Systemic Lupus Erythematous Authors: Alice Breining, BS, Anne Sophie Carret-Rebillat, MD,
Nathalie Costedoat-Chalumeau, MD, PhD, Gaelle Leroux, MD, Franois Piette, MD, and Pascal Chaibi, MD Introduction Late-onset systemic lupus erythematous (SLE) is most often a drug-induced SLE, and is usually a benign form. Use of immunosuppressive drugs is rarely necessary. We report an unusual case of a late-onset, drug-induced neuropsychiatric SLE (NPSLE). Case Presentation Mrs. R, an 80-year-old Caucasian woman, was hospitalized in 2006 for fever. Her familial history included a sister who had SLE and a daughter who had Basedow disease and multiple sclerosis. Her past medical history included a diagnosis of coronary heart disease in 2003, which justified an angioplasty with the implementation of two stents and treatment with beta blockers, statins, and platelet antiaggregants. In 2004, the patient had an autoimmune hemolysis without anemia but with positive antinuclear antibody (ANA) (titer 1:320), positive anti-DNA antibodies (titer 1:40), low haptoglobin, and highly positive direct Coombs test. For the 6 months prior to her 2006 hospitalization, Mrs. R had been experiencing a progressive loss of autonomy associated with a cognitive dysfunction. She arrived at a geriatric unit for a urinary tract infection with fever. On examination, she was confused and showed an erythematosquamous eruption of the upper chest and cheeks associated with alopecia. She had no arthritis, serositis, or kidney disease. After the pyelonephritis was treated, the patient remained confused, which triggered further investigations. Biochemistry showed a low sodium level (125 mEq/L) related to a syndrome of inappropriate secretion of anti-diuretic hormone. Mrs. R had a lymphopenia (360/mm), a hemolysis without anemia but with positive direct Coombs test, ANA (titer > 1:640 with a homogene appearance), anti-DNA antibodies (Farr test > 50), anti-nucleosome antibodies, anticardiolipin antibodies, and low complement levels. Anti-beta 2-glycoprotein 1 and antihistone antibodies were negative. Cerebrospinal fluid showed a sterile and acellular liquid.
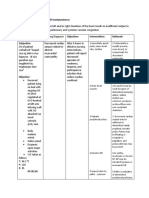
An electroencephalogram denoted a global deterioration evocating an encephalopathy, associated with paroxystic comitiality. Finally, the magnetic resonance imaging (MRI) scan did not reveal any acute vascular lesion. The cutaneous biopsy showed a direct immunofluorescence compatible with a lupic band. Based on the above, Mrs. R met 5 out of 11 SLE criteria from the American College of Rheumatology1 (Table), namely: malar rash, neurological and hematological manifestations, and positive ANA and anti-DNA antibodies. A diagnosis of NPSLE was made. Electrolyte abnormalities were corrected without any influence on the confusion that became even worse. Drugs that may cause SLE, that is beta blockers and statins, were stopped. She was treated with a high oral dose of corticosteroids (prednisone 1 mg/kg/day), and antiepileptic treatment (lamotrigine 75 mg/day). Mrs. R was soon discharged from the acute geriatric unit and went to a convalescent home. All clinical symptoms, except the cognitive dysfunction, and biological abnormalities rapidly began to improve. The autoimmune antibodies decreased (Figure). Mrs. R later presented with numerous complications of corticosteroids: urinary tract infection with recurrence of coronary heart disease after 2 months of treatment, herpes simplex virus pneumopathy and perforated ulcer with peritonitis after 3 months, and tuberculosis and diabetes after 4 months. The dosage of prednisone was reduced gradually to 10 mg/day, and hydroxychloroquine (400 mg/day) was introduced. After 8 months, her cognitive dysfunction had improved, with a Mini-Mental State Examination score that increased from impracticable to 25/30. At last follow-up 2 years later, the patient was doing well and was living at home. Discussion NPSLE in very old persons is difficult to diagnose unless suspected because it is generally considered a disorder of youth and because of its clinical presentation, which is not specific. A review of the literature reveals many cases of late-onset SLE, showing a wide range of clinical manifestations.2-9 Occurrence of neurological manifestations in patients with lateonset SLE varies from 4.8%10 to 90%,11 according to the studies. In elderly persons, neuropsychiatric manifestations due to SLE are nonspecific.12 They include cognitive dysfunction, cerebrovascular manifestations, and encephalopathy. Seizures and parkinsonism have also been described.13 Polyradiculopathy, demyelinating syndrome, headache, cranial
neuropathy, autonomic central nervous system, and personality or movement disorders are rare. The diagnosis is important to make since the symptoms respond in most cases to corticosteroids, as illustrated in the case patient.12 The classical characteristic of drug-induced SLE14,15 is the combination, to various degrees, of arthralgia, skin involvement, serositis, positive anti-histone antibodies, and negative antiDNA antibodies. On the other hand, malar rash, photosensitivity, alopecia, and renal or neurological dysfunctions are rare. Despite the fact that neurological involvement is rare in drug-induced SLE,14,15 this origin was assumed for the case patient from the facts that very few cases of spontaneous SLE have been described at this age, beta blockers are among the main causes of drug-induced SLE, and from the chronology of events. In this particular case, given the uncertainty of the origin of the disease (ie, drug-induced or not) and the severity of SLE manifestations, the patient was treated with corticosteroids in addition to the withdrawal of potential inducers of SLE. Many studies have compared the severity of SLE depending on the age at onset (after vs before age 50 yr). They are not clearly conclusive, since half of them found that there is no significant difference,16-19 whereas the other half conclude that the severity was lower for late-onset cases.20-24 Additionally, as illustrated by the case patient, four articles emphasize that late-onset SLE can be severe because of the clinical context and complications of treatments, especially corticosteroids.10,12,20,24 This higher mortality was demonstrated in patients with SLE diagnosed both after the age of 50 years20,24 and after the age of 65 years.10,12 Conclusion Even though SLE affects mostly younger persons, it can also be diagnosed in elderly individuals. In such cases, the diagnosis is more difficult, as the clinical presentation may be atypical. Confusion can be the main symptom and, after eliminating the frequent etiologies, rare causes such as SLE must be evoked. Treatment must be adapted to the severity of SLE and to the comorbidities of patients. The authors report no relevant financial relationships. Drs. Breining, Carret-Rebillat, Piette, and Chaibi are from the Department of Internal Medicine, Charles Foix Hospital, Ivry-sur-Seine, France; and Drs. Costedoat-Chalumeau and
Leroux are from the Department of Internal Medicine 2, Piti-Salptrire Hospital, Paris, France. References: 1. Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 1997;40:1725. 2. Beyan E, Uzuner A, Beyan C. An uncommon cause of fever in the elderly: Late-onset systemic lupus erythematosus. Clin Rheumatol 2003;22:481-483. Published Online: November 7, 2003. 3. Takeda N, Teramoto S, Ihn H, et al. A case of very late onset overlap syndrome of systemic sclerosis and systemic lupus erythematosus [article in Japanese]. Nippon Ronen Igakkai Zasshi 2000;37:74-79. 4. Ito H, Nanamiya W, Kuroda N, et al. Chronic lupus peritonitis with massive ascites at elderly onset: Case report and review of the literature. Intern Med 2002;41:1056-1061. 5. Chan KM. Systemic lupus erythematosus--not to be forgotten in the elderly. Singapore Med J 1995;36:105-106. 6. Mirsattari SM, Power C, Fine A, et al. Neuropsychiatric systemic lupus erythematosus and the syndrome of inappropriate secretion of antidiuretic hormone: A case report with very late onset systemic lupus erythematosus. Br J Rheumatol 1998;37:1132-1134. 7. Koga T, Kubota Y, Kiryu H, et al. Late onset systemic lupus erythematosus with lichen planus-like eruption and cardiac tamponade. Eur J Dermatol 2000;10:620-622. 8. Iijima S, Takita T, Otsuka F. Late onset systemic lupus erythematosus diagnosed in an elderly man with unusual skin eruptions and sudden death. J Dermatol 1995;22:943-947. 9. Gordon CD, Lozada CJ. Hydronephrosis and painless ascites: Rare features of late-onset SLE. Clin Exp Rheumatol 2005;23:551. 10. Pu SJ, Luo SF, Wu YJ, et al. The clinical features and prognosis of lupus with disease onset at age 65 and older. Lupus 2000;9:96-100.
11. McDonald K, Hutchinson M, Bresnihan B. The frequent occurrence of neurological disease in patients with late-onset systemic lupus erythematosus. Br J Rheumatol 1984;23:186-189. 12. Gaujard S, Broussolle C, Cathebras P, et al. Systemic lupus erythematosus with disease onset after age 65 [article in French]. Rev Med Interne 2003;24:288-294. 13. Mack AH, Fricchione G, Rogers MP. Neuropsychiatric systemic lupus erythematosus, age, and the neurodevelopmental model: Evidence in support of the Weinberger hypothesis. Compr Psychiatry 2002;43:135-141. 14. Vasoo S. Drug-induced lupus: An update. Lupus 2006;15:757-761. 15. de Langen-Wouterse JJ, Bijl AM, van Grootheest AC. Drug-induced systemic lupus erythematosus: Reports to The Netherlands Pharmacovigilance Centre Lareb [article in Dutch]. Ned Tijdschr Geneeskd 2007;151:367-370. 16. Padovan M, Govoni M, Castellino G, et al. Late onset systemic lupus erythematosus: No substantial differences using different cut-off ages. Rheumatol Int 2007;27:735-741. Published Online: December 29, 2006. 17. Sayarlioglu M, Cefle A, Kamali S, et al. Characteristics of patients with late onset systemic lupus erythematosus in Turkey. Int J Clin Pract 2005;59:183-187. 18. Mak SK, Lam EK, Wong AK. Clinical profile of patients with late-onset SLE: Not a benign subgroup. Lupus 1998;7:23-28. 19. Maddison P, Farewell V, Isenberg D, et al; Systemic Lupus International Collaborating Clinics. The rate and pattern of organ damage in late onset systemic lupus erythematosus. J Rheumatol 2002;29:913-917. 20. Boddaert J, Huong DL, Amoura Z, et al. Late-onset systemic lupus erythematosus: A personal series of 47 patients and pooled analysis of 714 cases in the literature. Medicine (Baltimore) 2004;83:348-359. 21. Shaikh SK, Wang F. Late-onset systemic lupus erythematosus: Clinical and immunological characteristics. Med J Malaysia 1995;50:25-31.
22. Ho CT, Mok CC, Lau CS, Wong RW. Late onset systemic lupus erythematosus in southern Chinese. Ann Rheum Dis 1998;57:437-440. 23. Formiga F, Moga I, Pac M, et al. Mild presentation of systemic lupus erythematosus in elderly patients assessed by SLEDAI. SLE Disease Activity Index. Lupus 1999;8:462-465. 24. Bertoli AM, Alarcn GS, Calvo-Alen J, et al; LUMINA Study Group. Systemic lupus erythematosus in a multiethnic US cohort. XXXIII. Clinical [corrected] features, course, and outcome in patients with late-onset disease [published correction appears in Arthritis Rheum 2006;54(7):2320]. Arthritis Rheum 2006;54(5):1580-1587.
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- BreastDokumen38 halamanBreastFathia RachmatinaBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Anggia Dian - AMLDokumen23 halamanAnggia Dian - AMLAzman HakimBelum ada peringkat
- Osteoporosis in Elderly MenDokumen5 halamanOsteoporosis in Elderly MenFathia RachmatinaBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Allergic RhinitisDokumen6 halamanAllergic RhinitisFathia RachmatinaBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- A Case of Scurvy in An Elderly PatientDokumen8 halamanA Case of Scurvy in An Elderly PatientFathia RachmatinaBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Nej M 199512213332508Dokumen8 halamanNej M 199512213332508Fathia RachmatinaBelum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Thypoid Fever + DHF Grade 1Dokumen30 halamanThypoid Fever + DHF Grade 1Fathia RachmatinaBelum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Ulkus Pedis and DM Type 2 Case KarawangDokumen28 halamanUlkus Pedis and DM Type 2 Case KarawangFathia RachmatinaBelum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Journal AmyloidosisDokumen27 halamanJournal AmyloidosisFathia RachmatinaBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Case DR - IrwinDokumen29 halamanCase DR - IrwinFathia RachmatinaBelum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- 60893Dokumen3 halaman60893Salman HabibBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Effect of Hypertension in Patiens With Chronic Kidney DiseaseDokumen17 halamanEffect of Hypertension in Patiens With Chronic Kidney DiseaseFathia RachmatinaBelum ada peringkat
- Thesis Statement For Nicotine AddictionDokumen8 halamanThesis Statement For Nicotine Addictiongbww46x7100% (2)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- West African Journal of Medicine: Volume 40, Number 1 January 2023Dokumen12 halamanWest African Journal of Medicine: Volume 40, Number 1 January 2023ThankGod OgbonnaBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- IMA Monthly Report Form JulyDokumen4 halamanIMA Monthly Report Form JulyInternetStudioBelum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Delivery Room Emergencies: Amanda Louise Du, MD, DPPS, DPSNBM Pediatrician-NeonatologistDokumen44 halamanDelivery Room Emergencies: Amanda Louise Du, MD, DPPS, DPSNBM Pediatrician-NeonatologistLyn LynBelum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Endodontic Treatment PlanDokumen44 halamanEndodontic Treatment Planlinh nguyễnBelum ada peringkat
- Abnormal Illness BehaviorDokumen7 halamanAbnormal Illness Behavioransha2011p0% (1)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- CHF NCPDokumen8 halamanCHF NCPZy Hallasgo100% (1)
- Case Study Severe Depression With Psychosis.: Submitted To:-Submitted ByDokumen33 halamanCase Study Severe Depression With Psychosis.: Submitted To:-Submitted ByPallavi KharadeBelum ada peringkat
- Online Review Exam ISBBDokumen44 halamanOnline Review Exam ISBBRockét PeredoBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Gastric CancerDokumen31 halamanGastric CancerHarleen KaurBelum ada peringkat
- Treatment MGRDokumen12 halamanTreatment MGRMod AntbugBelum ada peringkat
- Systemic Lupus Erythematosus Disease Activity Index 2000: Key Indexing TermsDokumen4 halamanSystemic Lupus Erythematosus Disease Activity Index 2000: Key Indexing TermsRandom PersonBelum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Benign - Malignant Ovarian TumorsDokumen34 halamanBenign - Malignant Ovarian TumorsAhmed AyasrahBelum ada peringkat
- Urn Uvci 01 Ro O0el5r27d48j5197y9nx3vwpgq96km#bDokumen2 halamanUrn Uvci 01 Ro O0el5r27d48j5197y9nx3vwpgq96km#bgrigore sinteanuBelum ada peringkat
- Prescription PsychologyDokumen7 halamanPrescription PsychologyJose LuisBelum ada peringkat
- The Following Resources Related To This Article Are Available Online atDokumen8 halamanThe Following Resources Related To This Article Are Available Online atFerdina NidyasariBelum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (120)
- Perineal Urethrostomy PUDokumen2 halamanPerineal Urethrostomy PUclara FBelum ada peringkat
- 4 Fundamentals of Health Services ManagementDokumen23 halaman4 Fundamentals of Health Services ManagementMayom Mabuong100% (6)
- 1 - Patient Evaluation, Diagnosis and Treatment PlanningDokumen5 halaman1 - Patient Evaluation, Diagnosis and Treatment PlanningMohammed100% (1)
- BSN 3-B (GROUP 2) - CLINICAL CASE ANALYSIS - Arthritis (REVISED)Dokumen7 halamanBSN 3-B (GROUP 2) - CLINICAL CASE ANALYSIS - Arthritis (REVISED)Florence Dumawal FariñasBelum ada peringkat
- Tumors of The Orbit by Dr. Jonathan Del Prado 082708Dokumen3 halamanTumors of The Orbit by Dr. Jonathan Del Prado 082708CitrusBelum ada peringkat
- tmpD824 TMPDokumen12 halamantmpD824 TMPFrontiersBelum ada peringkat
- PleuraDokumen6 halamanPleuraameerabest100% (1)
- Toxicity Review Natural ProductsDokumen5 halamanToxicity Review Natural Productsamino12451Belum ada peringkat
- Borda2018 PDFDokumen48 halamanBorda2018 PDFlarasBelum ada peringkat
- Marijuana and EpilepsyDokumen17 halamanMarijuana and EpilepsyOmar AntabliBelum ada peringkat
- Legal Medicine: Legal Medicine (2011) Antonio Rebosa, LL.B, M.DDokumen6 halamanLegal Medicine: Legal Medicine (2011) Antonio Rebosa, LL.B, M.DarciblueBelum ada peringkat
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Health Education For Patients With Urinary CathetersDokumen2 halamanHealth Education For Patients With Urinary CathetersTriXie SorrillaBelum ada peringkat
- Bates Physical Exam Video NotesDokumen3 halamanBates Physical Exam Video Notesdulcedeleche12359Belum ada peringkat
- The Ivf Pack 2 PDFDokumen11 halamanThe Ivf Pack 2 PDFPaula BošnjakBelum ada peringkat