Marasmus Down Syndrome
Diunggah oleh
KURBULDKDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Marasmus Down Syndrome
Diunggah oleh
KURBULDKHak Cipta:
Format Tersedia
1
MALNUTRITION AND DOWN SYNDROME
Presentators Day, Date Supervisor
: Nurtilawati Siregar, Rahmah Khairuna Damanik : Monday, September 9th, 2013 : dr. Pertin Sianturi, Sp.A(K)
CHAPTER 1 INTRODUCTION 1.1. Background Malnutrition is still the main problem in public health especially in developing countries, it contributes more than half death case of children under 5 years. It is one of the main problem of nutrition in Indonesia. Its Prevalence is high especially in children < 5 years. Based on SUSENAS 2002, 26% of children < 5 years having malnutrition, and 8% among them are in severe malnutrition, but in Riskesdas 2007, there prevalence decreases to 13% for moderate-malnutrition and 5.4% for severe malnutrition. 1,2 Severe malnutrition is both a medical and a social disorder. That is, the medical problems of the child result, in part, from the social problems of the home in which the child lives. Malnutrition is the end result of chronic nutritional and, frequently, emotional deprivation by carers who, because of poor understanding, poverty or family problems, are unable to provide the child with the nutrition and care he or she requires. Successful management of the severely malnourished child requires that both medical and social problems be recognized and corrected. If the illness is viewed as being only a medical disorder, the child is likely to relapse when he or she returns home, and other children in the family will remain at risk of developing the same problem.3
Down syndrome occurs due to an excess number of chromosomes in chromosome number 21, which is supposed to be two to three. Chromosomal abnormalities was not heredity. The disorder can cause sufferers experience physical abnormalities such as congenital heart defects, weakened muscles (hypotonia), and mental retardation about development of intelligence and psikomotor delay. Until now, the cause of abnormalities of chromosome number that is not yet known. In patients with Down syndrome chromosome number 21 is not a pair, but 3 pieces so the total number chromosomes to 47.When the baby was growing up, it is necessary to determine the type of IQ examination exercises selected schools. Another examination is an examination that may be required in patients with heart because it often suffer heart defects. There are three types of Down syndrome is Trisomy 21 regular, translocation and mosaic. 4 1.2. Objective The aim of this study is to explore more about the theoritical aspects on severe malnutrition and down syndrome, and to integrate the theory and application of severe malnutrition, in this case marasmus and down syndrome in daily practices.
CHAPTER 2 LITERATUR REVIEW
2.1.
Severe Malnutrition
2.1.1. Definition Malnutrition essentially means bad nourishment. It concerns not enough as well as too much food, the wrong types of food, and the body's response to a wide range of infections that result in malabsorption of nutrients or the inability to use nutrients properly to maintain health. Clinically, malnutrition is characterized by inadequate or excess intake of protein, energy, and micronutrients such as vitamins, and the frequent infections and disorders that result.1,2 2.1.2. Epidemiology Malnutrition is still the main problem in public health especially in developing countries, it contributes more than half death case of children under 5 years. It is one of the main problem of nutrition in Indonesia. Its Prevalence is high especially in children < 5 years. Based on SUSENAS 2002, 26% of children < 5 years having malnutrition, and 8% among them are in severe malnutrition, but in Riskesdas 2007, there prevalence decreases to 13% for moderate-malnutrition and 5.4% for severe malnutrition. 1,2 2.1.3. Aetiology Primarily, it is caused by low in quantity or quality of the food that is consumed, and high in need or output as a secondary causes. Malnutrition is the end result of chronic nutritional and, frequently, emotional deprivation by carers who, because of poor understanding, poverty or family problems, are unable to provide the child with the nutrition and care he or she requires. 2,3
2.1.4. Clinical Manifestation3,5 Marasmus : extreme wasting, old-man face, irritable, subcutaneous fat loss, baggy pant. Kwashiorkor : oedema, moon face, sparse hair with waek roots, apathy, irritable, muscle hypotrofi, hepatomegaly, crazy pavement dermatosis Marasmus-Kwashiorkor : mixed manifestation of marasmus and
kwashiorkor with minimally oedema. Figure 1, Marasmus Figure 2, Kwashiorkor
Others : micronutrient deficiencies (vitamin A deficiency, anemia, stomatitis, skin manifestation) signs and symptomps of co-morbid (diarrhoea, parasitic, tuberculosis, malaria, and pneumonia)
2.1.5. Assesment of Nutritional Status and Criteria for Hospital Admision Table 1, Clasiffication of malnutrion Clasiffication of malnutrition Mild-moderate Severe No Yes -3 SD < 2 < -3 SD (severe wasting) -3 SD < 2 < -3 SD (severe stunting)
Symmetrical oedema Weight for height Height for age
Assesment of severe malnutrition is based on clinical and physical examination (weight for height or length), the result is plotted to CDC NHCS/WHO curve to determine the clasiffication of malnutrition. These are (clinical and physical finding) are summarized in table 1. Children was weight for height is below -3 SD or less than 70% of the median NHCS/WHO reference values (termed severely wasted), or who have symmetrical oedema involving at least the feet (termed oedematous malnutrition) are severely malnourished. They should be admitted to hospital where they can be observed, treated and fed day and night. Another criteria for hospital admission is if there are other signs such as: anorexia, severe pneumonia, anemia, high fever, severe dehydration, lethargy, hypothermia, hypoglicemia.3 2.1.6. Diagnosis1,2,3 a. History : usual diet before current episode of illness, Breastfeeding history, Food and fluids taken in past few days, Recent sinking of eyes, Duration and frequency of vomiting or diarrhoea, Appearance of vomit or diarrhoeal stools, Time when urine was last passed, Contact with people with measles or tuberculosis, Any deaths of siblings, Birth weight, Milestones reached (sitting up, standing, etc., Immunizations. b. Physical Examiination : weight and length or height, Oedema, Enlargement or tenderness of liver, jaundice, Abdominal distension, bowel sounds, abdominal splash (a splashing sound in the abdomen), Severe pallor, Signs of circulatory collapse: cold hands and feet, weak radial pulse, diminished consciousness, Temperature: hypotermia or fever, Thirst, Eyes: corneal lessions indicative of vitamin A deficiency, Ears, mouth, throat : evidence of infection, Skin : evidence of infection or purpura, Respiratory rate and type of respiration: sign of pneumonia or heart failure, Appearance of faeces. c. Other Investigations: Blood Glucose : < 54 mg/dl = hypoglicemia
Blood Smear : malaria Hb or Ht : < 4 g/dl or < 12% = severe anemia Urynalysis/culture : bacteria + or > 10 WBC/ big view = infection Faeces : blood (+) = dysentri, Giardia (+)/ other parasites = infection CXR : Pneumonia, heart failure, fracture Tuberculin Skin Test : often negative
2.1.7. Treatment There are five key-points in management of severe malnutrition, they are : ten main steps, treatment of co-morbid, failure to respond to treatment, education before discharge, and management of emergency condition (such as shock and severe anemia). 2 a. Ten main steps, consists of 3 phase : initial, rehabilitation, and follow-up phase. The time-frame for management of severe malnutrition is shown in table 2.2 Initial Treatment : this phase begins with admission to hospital and lasts until the childs condition is stable (during 1 week). This is divided into stabilitation (day 1-2) and transition (day 3-7). It focuses on lifethreatening condition, spesific deficiencies, and feeding is begun. Rehabilitation (weeks 2-6) : intesive feeding, emotional and physical stimulation, and preperation for discharge. Follow Up (weeks 7-26) : preventing relapse and assure continued physical, mental, and emotional development of the child.
Table 2, Time Frame for management of severe malnutrition
1) Treat and prevent Hypoglicemia Patients with severe malnutrition are at risk of developing hypoglicemia, its important cause of death during the first 2 days of treatment. Diagnose based on blood glucose level below 54 mg/dl. Signs of hypoglicemia include hypothermia, lethargy, and loss of conscioussness, and often manifests only drowsiness before death. Unlike in common setting, hypoglycemia in severly malnourished children doesnt usually manifest as sweating and pallor. If hypoglicemia is suspected, treatment shoud be given immediately without laboratory confirmation (in setting without laboratory facilities,every severly malnourished children must be suspected and treated as hypoglicemia).3,6 Table 3, signs and treatment of hypoglicemia Signs Conscious, able to drink Treatment Give 50 ml D10%, or sugar 10% solution (by dilute 5 grams of sugar with 50 ml of water) Lethargy Give D10% 5 ml/BW (iv), then give 50 ml D10%,
or sugar 10% solution (bolus) via oral or NG route Shock Give D10% 5 ml/BW (iv), then drip RL and D10% (1:1) 15 ml/BW in 1 hour
2) Treat and prevent Hypothermia Hypothermia is defined as axillary temperature < 36,5 C (measure in 5 minutes) or rectal temperature < 35,5 C. Severly malnourished children are at greater risk of hypothermia than other children and need to be kept warm, and they are probably hypoglicemic also. If those are present, they may have serious systemic infection. All hypotermic children should be treated for hypoglicemia and infection as well. 3,5 Severly malnourished children have difficulty in controlling temperature because of low calories, warming these patients can conserves their energy Following measures are important for all severly malnourished children3,6,7 Cover the child, including his head. Stop draughts in the room. Move the child away from windows. Maintain room temperature of 25 30C (77 86F) if possible. Keep the child covered at night. Warm your hands before touching the child. Avoid leaving the child uncovered while being examined, weighed, etc. Promptly change wet clothes or bedding. Dry the child thoroughly after bathing. In addition to keep the child warm, we can use one of the following : have the mother hold the child with his skin next to her skin when possible (kangaroo technique), and cover both of them. Keep the childs head covered.3,6,7 :
3) Treat and prevent Dehydration
Table 4, Assesment of Dehydration Signs of Dehydration Lethargic Assesment Not awake & alert, drowsy, doesnt show interest in what is happening around him Restless, irritable Happens all the time, especially when he is touched or handled Absence of tears Observe when he cries whether the child has tears or not Sunken Eyes Severly malnourished children may always shows sunken eyes, regardless of the hydration status, so ask the mother if the childs eyes appear unusual Dry mouth and tongue Feel the tounge and inside of the mouth with a clean, dry finger to determine if they are dry Thirsty See if the child reaches out for the cup when we offer the ReSoMal. When its taken away see if the child wants more Skin pinch goes back slowly Use the thumb or first finger to pinch skin on the childs abdomen halfway between umbilicus and the side of abdomen. Pinch the skin for one second and then release, if the skin stays folded for brief time, the skin goes back slowly. Many of these signs of dehydration are unreliable in a child with severe malnutrition, making it difficult to detect and determine the severity of dehydration. Following signs are reliable in a child with severe malnutrition : history of diarrhoea, thirsty, hypothermia, sunken eyes, weak and rapid radial pulse, cold hands and feet, urine flow.3,5
10
Treatment of dehydration in severly malnourished children is different, these children have abnormally hi-sodium and lo-potasium. WHO recomends modified oralit which is called ReSoMal (rehydration solution for malnutrition) that is contained less sodium and more potasium (it is intended for severly malnourished children with diarrhoea). ReSoMal can be made by diluting one-packet standard WHO-ORS, 8 ml mineral mix (one packet dilute in 20 ml water) and 10 gram sugar in 400 ml water. NG tube should be used in all weak or exhausted children. And in those who vomit, have fast breathing, or painful stomatitis.3,6,7 If the severely malnourished child has watery diarrhoea or vomitting, assume dehydration (also ask about dysentry as will affect choice of antibiotics) and give ReSomal as follows : 5 ml/BW every 30 minutes for the first 2 hours (orally or NG tube), then 5-10 ml/BW/hour in alternate hours for up to 10 hours, F-75 is given in alternate hours during this period until the child is rehydrated. These rates are slower than for children who are not severly malnourished. Reassess the child at least every hour. The exact amount of ReSoMal to give should be determined by the eager of drink, amount of going losses (vomit, stool), and also the signs of overhydration especially signs of heart failure. Rehydration is completed when the signs above (table) have disappeared. After rehydration, give 50-100 ml of ReSoMal after each loose stool (< 2 years), and 100-200 ml for > 2 years. This treatment is continued until diarrehoea stops.3,6,7 Be aware the signs of shock during diarrhoea, such as lethargy, unconciousness, cold hands and feet, delayed capillary refill time, diminished urine flow.7
4) Correction of electrolyte imbalances Severe malnutrion patients are at risk having electrolyte imbalance and need to be corrected. ReSoMal consists of glucose, sodium, potasium, chloride, citrate, magnesium, zinc, copper (table 5). Beside ReSoMal when diarrhoea, correction
11
of electrolyte imbalance also got from feeding WHO-formula according to the phase (see next step).3,6,7 Table 5, component of ReSoMal Component Glucose Sodium Potassium Chloride Citrate Magnesium Zinc Copper Osmolarity Consentration (mmol/L) 125 45 40 70 7 3 0.3 0.045 300
5) Treat infections3,6,7 Give all severly malnourished children antibiotics for presumed infection. Give the first dose while other initial treatments are going on, as soon as possible. Selection of antibiotics depends on the presence or absence of complications (like septic shock, hypoglicemia, hypothermia, dermatosis, resp/urinary tract infection, or lethargic/sickly appereance. If no complication : oral cotrimoxazole (25 mg Sulfamethoxazole + 5 mg trimethroprim/kg) every 12 hours for 5 days If there is complications : gentamicin 7.5 mg/kg IM/IV once daily for 7 days + ampicilin 50 mg/kg IM/IV every 6 hours followed by amoxicilin 15 mg/kg every 8 hours for 5 days.
12
If the child fails to improve within 48 hours, add chloramphenicol 25 mg/kg IM/IV every 8 hours for 5 days. And give additional antibiotics if spesific infection are detected.
6) Correction of miconutrient deficiencies Severly malnourished children are at risk having micronutrient deficiencies and its consequences. So give supplemental every day as the following rule : multivitamin supplemental (without iron in the stabilisation & transition phase, with iron in the rehabilitation phase), folic acid 5 mg in the first day then give 1 mg/BW, vitamin A based on age 50.000 IU for < 6 months, 100.000 IU for 6-12 months, and 200.000 IU for > 1 years. Iron should never be given during initial phase because it can lead to free iron in the body and cause : promoting bacterial growth and increasing the risk of infection, formation of free radicals, and increasing the need of calories to be used for converting free iron to ferritin.3,6,7 7) Begin Feeding Feeding is obviously a critical part of managing severe malnutrition, however, feeding must be started cautiously, in frequent, small amounts. If feeding begins too aggressively, or if feeds contain too much protein or sodium, the childs systems may be overwhelmed, and the child may die. To prevent death, feeding should begin as soon as possible with F-75, the starter formula used until the child is stabilized (stabilisation phase). F-75 is specially made to meet the childs needs without overwhelming the bodys systems at this early stage of treatment. F-75 contains 75 kcal and 0.9 g protein per 100 ml. F-75 is low in protein and sodium and high in carbohydrate, which is more easily handled by the child and provides much-needed glucose.3,8,9 The goals to be achieved in this phase are : energy : 80-100 kal/kgBW/day, protein 1-1,5 gr/kg, volume 130 ml/kgBW/day (100 ml if oedema) and the children should also continue to be breastfed between feeding. Appendix A shows the amount of diet at each feed to achieve the goals (dose of F-75 based on BW). For the first 2
13
hours give a quarter of the dose F-75/2 hours every 30 minutes, then for next 10 hours continue F-75/2 hours. If well-tolerated, continue F-75 every 3 and 4 hours. After finishing F-75/4 hours and the children are well-tolerated, continue the feeding in the next phase (transition and rehabilitation).2,3,8 In transition phase the children are given with F-100 but using the F-75 dose (Appendix A) every 4 hours for 2 days, in the third days children are given with F-100 dose (Appendix B) every 4 hours, the dose is up-titrated 10 ml until the children cannot tolerate but not exceed the maximum dose in table. In the fourth day give F100 every 4 hours until the end of transition phase (7-14 days) according to children condition. It is important to note that it is the childs appetite and general condition that determine the phase of treatment and not the length of time since admission.3,8
8) Increase feeding to recover lost weight (Catch-up formula) When the child is stabilized (usually after 2 7 days) and after the appetite has returned, the catch-up formula F-100 is used to rebuild wasted tissues. F-100 contains more calories and protein: 100 kcal and 2.9 g protein per 100 ml. In this phase : energy : 150-220 kal/kgBW/day, protein 4-6 gr/kg. The child should remain in hospital for the first part of rehabilitation phase. The patient can be transferred to nutrition rehabilitation center if all folowing criterias have been met : eating well, mental state has improved (smiles, responds to stimuli, interested in surroundings), sits, crawls, stands or walks (depending on age), normal temperature, no vomitting or diarrhoea, no oedema, gaining weight > 5 g/kgBW per day for 3 successive days.3,8,9,10 9) Stimulate emotional and sensorial development Severly malnourished children have delayed mental and behavioural development, which if not treated can become serious long-term result of malnutrition, emotional and physical stimulation through play programmes that starts during rehabilitation and continue after discharge can substianlly reduce risk of of permanent mental retardation and emotional impairement. Take a look for : the environment, activities (play & physical).2,3
14
10) Prepare for discharge During rehabilitation, preparations should be made to ensure that the child is fully reintegrated into the family and community after discharge. As the childs home is the environment in which severe malnutrition developed, the family must be carefully prepared to prevent its recurrence. Give sugestion to come back to the hospital for evaluation regulary one a week in the first month, one in two weeks in the second month, and one a month in the next three-four months.2,3 The patients are determined as recover from the severe malnutrition if weightlenght > -2 SD and no clinical manifestation. And criteria for discharge as following2,3: b. c. No oedema, awake and active Weigth for lenght > - 3 SD No complications Increase BW 50 g/kgBW/week for 2 weeks Mother given the knowledge about nutrition for her child. Good appetite Treatment of Co-Morbid2,3 Vitamin A Deficiency Dermatosis Parasitic infestation Persisten Diarrhoea Tuberculosis Failure to respond to treatment2,3
15
There are two kinds of failure in this treatment. First when the patient die, for the first 24 hours after admision can be caused by hypoglicemia, hypothermia, dehydration, and sepsis. And for the next 24-72 hours is caused by aggresive feeding (exceed in volume and calories). The next is related to the improvement of body weight, the inadequency of increasing BW may be caused by infection, dietary, and also physicological. So it is important to evaluate the body weight (good if > 10 g/kgBW/day, fair 5-10 f/kgBW/day, and poor < 5 g/kgBW/day) and investigate the cause of the failure of the treatment. d. Discharge before the end of rehabilitation phase2,3 Give education to the parents about dietary (hi-calory and hi-protein, frequency 5 times a day, full portion, multivitamin supplementation, breastfeeding is continued), back to the hospital for evaluation, and vaccination. e. Management of emergency condition 2.2 Down Syndrome
2.2.1 Definition Down syndrome is a genetic disorder known as Trisomy, because individuals who get a Down syndrome have excess chromosome. They have three chromosome 21 where the normal only has two. This will change the excess chromosome genetic balance of the body and result in changes in the characteristics physical and intellectual abilities, as well as disturbances in physiological function body.4 2.2.2 Epidemiology Abnormality is found throughout the world, in all ethnic groups. Estimated incidence of 1.5: 1000 births, and there were 10% among patients with mental retardation. Found statistically more born to mothers over the age of 30 years, although not infrequently also found that babies born to young mothers. In this last group, in the form of a translocation chromosome abnormalities.11
16
2.2.3 Aetiology11 Down syndrome are born to mothers aged older (high risk), women over 35 should be aware of this possibility. The incidence of Down syndrome increases evident in women who gave birth after age 35 years and over. Female egg cell has been established at the time the woman was still in the womb to be cured one by one each month. By the time a woman becomes older, the condition of the egg cells sometimes become less well and at the time the egg is fertilized by the male germ cells undergoing division are less than perfect. The cause of the excess of chromosome 21 could also be due to congenital birth of mother or father who has two pieces of chromosome 21, but it is not in its rightful place, as one of the chromosome 21 attached to another chromosome during cell division so that chromosome 21 does not divide perfectly. Factors that play a role in the occurrence of chromosomal abnormalities are: 1. Maternal age : usually the mother over the age of 30 years, probably due to a hormonal imbalance. 2. Disorders of pregnancy. 3. Endocrine disorders in women : old age can occur relative infertility, thyroid disorders or ovarian.
2.2.4 Clinical Manifestation11,12 Children with this syndrome are very similar to each other. Mental retardation in addition there is also a very prominent physical retardation. Thinking skills can be classified as an idiot and will not be able to exceed a 7-year-old child. Usually very interested in music. Child's face is very typical. Head rather small and brakisefalik with flat occipital region. Wide face, high cheekbones, flat nose, squinty eyes far apart and tilted upwards and the side (like the Mongols). Ear a bit strange, thick lips and large tongue, rough and fissured-gap. The growth of the teeth are very disturbed. Smooth and loose skin, but the color is normal. In the folds of the neck are excessive. On the pinkie finger looks short and bent inward. Distance between fingers
17
I and II, both on the hands and feet are rather large. Genitals are usually small. Hypotonic muscles and joints from excessive movement. Congenital heart defects such as ventricular septal defect is often found, growth in infancy is sometimes good, but then it became slow. 2.2.5 Diagnosis11 Diagnosis based on: 1. Clinical symptoms 2. Additional examination a. Dermatoglifik b. Chromosome examination 3. Anatomic pathology Brains of children with disorder are usually smaller than normal and bigger children, the growth of the brain growing up. 2.2.6 Treatment No special treatment
CHAPTER III CASE REPORT Name Age Sex Date of Admission Main Complaint : REA : 1 year 3 months : Male : August, 17 th 2013 : vomiting
18
History : It is experienced by patients is approximately 2 days, the frequency of vomiting was not counted. Content of what they eat and drink - Diarrhoea (+) 2 days, 2x/day frequency, consistensi water more than pulp (+), lenders (+), blood (-) - Now this patient's fever, history of recurrent fever (+), fever is up and down, down with fever-reducing medicine. - The body weight decreased since the age of 6 months. - urination (+) normal. History feeding 0.1 years old: ASI 0-6 months: exclusive breastfeeding 6-9 months: cereal + milk 9-12 months: breast + formula (SGM) + cereal History of birth Patient is the second son of the two brothers, was born normal, helped midwife, BW = 2600gr BH = 48cm, immediately cried History of growth and development Now this patient can only prone itself, babbling, imitating the words,smilling, and looking at his hands. Physical Examination BW/Age: < -3SD BH/Age: < -3SD BW/BH: < -3SD Presens status Sens. Compos Mentis, Body temperature: 37,0oC, Pulse: 140 bpm, Respiratory Rate: 40 bpm. Localized status
19
Head : old man face (+),dismortik Face (+) Eye : concave,light reflexes (+/+), isochore pupil, pale conjunctiva palpebra inferior (-/-),icteric sclera (-/-) , Ear : Normal ,Mouth : Normal , Nose: nasal canul O2 attached
1. Neck : Lymph node enlargement (-) 2. Thorax : Symmetrical fusiform, easily seen ribs(+), retraction (-) HR: 140x/i, reguler, sigh (-). RR: 40 x/i, regular, crackles (-/-) 3. Abdomen : Soepel,Peristaltic(+)normal.Liver/Spleen/Renal: undeterminate 4. Extremities: pulse : 140 x/i, regular, adequate pressure and volume, warm acral, CRT <3, baggy pants (+), muscle hypertrophy (+), TD=90/60mmhg. Working Diagnosis -Marasmus type Malnutrition (II condition) + susp.Down syndrome
P: Management - O2 2L / i nasal canul - Inj. ceftriaxone 150 mg / 2 hours / IV -Resomal 50cc alternatif with diet F75 40cc /2hours with mineral mix 0,8cc - When diarrhea (+): Resomal / x diarrhea - Multivitamins without Fe 1 x 1 cth - Folic acid 1x1mg - Vitamin A 1x200.000 IV Planning
20
Complete Blood Count Blood Glucose Electrolite
FOLLOW UP August, 17th 2013 (First day) S: Vomiting (+), Diarrhea (+), shortness of breath(-) O: Sens: GCS 12 (E4V2M6) , Temp: 37 oC, Body weight: 3,4 kg PB = 65cm Head : Old man face (+), dismorfic face (+) eye : concave, light reflexes (+/+), icteric Sclera (-/-), isochoric pupil, pale conjunctiva palpebra inferior (-/-), Ear : Normal, Nose: nasal canul O2 Neck Thorax attached (+),NGT(+), Mouth: normal : Lymph node enlargement (-) : Symmetrical fusiform, easily seen ribs(+),retraction (-) HR: 120x/1, reguler, sigh (-). RR: 32 x/1, regular, crackles (-/-) Abdomen : Soepel, Peristaltic (+) normal. Liver/spleen/renal :undeterminate Extremities : Pulse 140 x/i, regular, adequate pressure and volume, warm acral, CRT < 3, baggy pants (+), muscle hypertrophy (+), TD=90/60 mmgh
A: Marasmus type Malnutrition (II condition) + susp.Down syndrome P: Management - O2 2L / i nasal canul - Inj. ceftriaxone 150 mg / 2 hours / IV - Resomal 50cc alternative with diet F75 40cc/2hours with mineral mix 0,8cc - Multivitamins without Fe 1 x 1 cth - Folic acid 1x1mg - Vitamin A 1x200.000 IV
21
Plan : - Complete Blood Count - Blood Glucose Laboratory Result: 1. August, 17th 2013 g% 106/ mm3 103/ mm3 % 103/ mm3 fL Pg g% % fL % fL % % % % % 103/L 103/L 103/L 103/L 103/L 13.20 4.87 45.00 37.70 736 77.40 27.10 35.00 15.10 9.90 0.73 10.7 83.20 7.40 9.10 0.10 0.200 37.41 3.33 4.11 0.04 0.11 11.3 14.1 4.40 4.48 6.0- 17.5 37 41 217 497 81 95 25 29 29 31 11.6 14.8 7.2 - 10.0 Complete Blood Count Hemoglobin (HGB) Eritrosit (RBC) Leukosit (WBC) Hematokrit Trombosit (PLT) MCV MCH MCHC RDW MPV PCT PDW Diftel Neutrofil Limfosit Monosit Eosinofil Basofil Neutrofil Absolut Limfosit Absolut Monosit Absolut Eosinofil Absolut Basofil Absolut -Electrolite
37 80 20 40 28 16 01 1.9 - 5.4 3.7 - 10.7 0.3 - 0.8 0.20 - 0.50 0 - 0.1
22
Laboratory Result: 1. August, 17th 2013 Clinical Chemistry Blood gas analysis Ph pCO2 Bicarbonate (HC08) Total CO2 Base excess (BE) O2 saturation CARBOHYDRATE METABOLISM Blood glucose (As) ELEKTROLIT Natrium (Na) Kalium (K) Klorida (Cl) Laboratory Result: 2. August, 19th 2013 Clinical Chemistry CARBOHYDRATE METABOLISM Blood glucose (As) IMUNOSEROLOGI TIROID T3 Total T4 Total TSH SATUAN Mg/dL g/mL g/dL U/mL HASIL 129.00 0.67 7.09 1.460 RUJUKAN <200 0.8-2 5-14 0.27-4.2 SATUAN HASIL 7.490 42.8 153.8 31.9 33.2 7.8 331.00/ 123 3.3 87 RUJUKAN 7.35-7.45 38-42 85-100 22-26 19-25 (-2)-(+2) <200 135-155 3.6-5.5 96-106
mmHg mmHg mmol/L mmol/L % mg/dL mEq/L mEq/L mEq/L
23
August, 18th 2013 (Second day) S: Vomiting (+), Diarrhea (+), shortness of breath(-) O: Sens: GCS 12 (E4V2M6) , Temp: 37,6oC, Body weight: 3,4 kg, PB 65cm, LLA : 8cm Head : Old man face (+), dismorfic face (+) Eye :light reflexes (+/+), isochoric pupil, pale conjunctiva palpebra inferior Thorax (-),Ear = normal, Nose = nasal canul O2 (+), NGT (+), Mouth = Normal : Symmetrical fusiformis, easily seen ribs(+), retraction (-).
HR: 120x/1, reguler, sigh (-),RR: 40 x/1, regular, crackles (-/-) Abdomen : Soepel,Peristaltic (+) normal. Liver/Spleen/Renal: undeterminate Extremities : Pulse 140 x/I regular, adequate pressure and volume, CRT < 3 baggy pants (+), muscle hypertrophy (+). A: Marasmus type malnutrition (II condition) + susp. Down syndrome P: management - O2 2L/I - Inj. ceftriaxone 150 mg / 2 hours / IV - Resomal 50cc alternative with diet F75 40cc/2jam with mineral mix 0,8cc - Multivitamins without Fe 1 x 1 cth - Folic acid 1x1mg Plan : consul division nutrition and metabolic diseases
24
August, 19th 2013 (third day) S: vomiting (-), Diarrhea (+), shortness of breath (-) O: Sens: GCS 12 (E4V2M6), Temp: 37oC, Body weight : 3,4 kg, PB: 65cm LLA = 8cm Head Old man face(+),Dismorfic face (+) Eye :light reflexes (+/+),Isochoric pupil, pale conjunctiva palpebra inferior Neck Thorax Abdomen (-),Ear = Normal, Nose= nasal canula O2 (+), NGT (+), Mouth = Normal Lymph node enlargement(-) Symmetrical fusiformis, easily seen ribs(+),retraction (-). HR: 124x/1, reguler, sigh(-),RR: 38 x/1, regular, crackles (-/-) Soepel,Peristaltic (+) normal. Liver/Spleen/Renal : undeterminate < 3, hypotropy muscle (+), baggy pants (+) Extremities Pulse 124 x/1, regular, adequate pressure and volume, warm acral, CRT
A: Marasmus type malnutrition (II condition) + susp.Down syndrome P: management - Resomal 50 cc / x diarrhea - Folat acid 1 x 1 mg - Multivitamin without Fe 1 x1 cth - Diet F75 40cc / 2 hrs with mineral mix 0.8 cc Plan : - Blood Glucose - Tiroid
August, 20th 2013 (Fourth day) S: Vomiting (-), Diarrhea (+), shortness of breath (-)
25
O: Sens: GCS 12 (E4V2M6), Temp: 36,8oC, Body weight : 3,4 kg, PB: 65cm LLA = 8cm Head Old man face(+),Dismortic face (+) Eye :light reflexes (+/+),Isochoric pupil, pale conjunctiva palpebra inferior Neck Thorax (-),Ear = Normal, Nose= nasal canula O2 (+), NGT (+), Mouth = Normal Lymph node enlargement(-) Symmetrical fusiformis, easily seen ribs(+),retraction (-)
HR: 124x/1, reguler, sigh (-),RR: 38 x/1, regular, crackles (-/-) Abdomen Soepel. Peristaltic (+) normal. Liver/Spleen/Renal : undeterminate Extremities Pulse 124 x/1, regular, adequate pressure and volume, warm acral, CRT < 3, hypotropy muscle (+), baggy pants (+) A: Marasmus type malnutrition (II condition) + susp.Down syndrome P: management - Resomal 50 cc / x diarrhea - Folat acid 1 x 1 mg - Multivitamin without Fe 1 x1 cth - Diet F75 40cc / 2 hrs /NGT with mineral mix 0.8 cc Plan :-
August, 21st 2013 (fifth day) S: Vomiting (-), Diarrhea (+), shortness of breath (-)
26
O: Sens: GCS 12 (E4V2M6),T: 37.5oC, Body weight : 3,4kg, PB = 65cm, LLA = 8cm Head Old man face(+),Dismorfic face (+) Eye :light reflexes (+/+),Isochoric pupil, pale conjunctiva palpebra inferior (-),Ear = Normal, Nose= nasal canula O2 (+), NGT (+), Mouth = Normal Neck Thorax Lymph node enlargement(-) Symmetrical fusiformis, easily seen ribs(+),retraction (-)
HR: 112x/1, reguler, sigh (-).RR: 38 x/1, regular, crackles (-/-) Abdomen Soepel. Peristaltic (+) normal. Liver/Spleen/Renal : undeterminate Extremities Pulse 112 x/1, regular, adequate pressure and volume, warm acral, CRT < 3, hypotropy muscle (+), baggy pants (+) A: Marasmus type malnutrition (II condition) + susp.Down syndrome P: management - Resomal 50 cc / x diarrhea - Multivitamin without Fe 1 x cth 1 - Folat acid 1 x 1 mg - Contrimoxazole syr 1x 1cth - Diet F75 40cc / 2 hrs/NGT with mineral mix 0,8 cc
Plan : -
August, 22nd 2013 (sixth day) S: Vomiting (-), Diarrhea (-), shortness of breath (-)
27
O: Sens: compos mentis, Temp: 37oC, Body weight : 5,2 kg Head Old man face(+),Dismorfic face (+) Eye :light reflexes (+/+),Isochoric pupil, pale conjunctiva palpebra inferior Neck Thorax (-),Ear = Normal, Nose= nasal canula O2 (+), NGT (+), Mouth = Normal Lymph node enlargement (-) Symmetrical fusiformis, easily seen ribs(+),retraction (-)
HR: 102x/1, reguler, sigh (-). RR: 32 x/1, regular, crackles (-/-) Abdomen Soepel,Peristaltic (+) normal. Liver/Spleen/Renal : undeterminate Extremities Pulse 102 x/1, regular, adequate pressure and volume, warm acral, CRT < 3, hypotropy muscle (+), baggy pants (+). A: Marasmus type malnutrition + susp.Down syndrome P: management - Folat acid 1 x 1 mg - Multivitamin without Fe 1 x 1cth - Cotrimoxazole syr 1x1cth - Diet F100 65cc / 2 hrs/NGT with mineral mix 1,3 cc - Resomal 50 cc / x diarrhea
Plan:-
August, 23rd 2013 (seventh day) S : Vomiting (-), Diarrhea (-)
28
O : Sens: Compos Mentis, Temp: 37oC, Body weight : 5,2 kg Head Old man face(+),Dismorfic face (+) Eye :light reflexes (+/+),Isochoric pupil, pale conjunctiva palpebra inferior Neck Thorax (-),Ear = Normal, Nose= nasal canula O2 (+), NGT (+), Mouth = Normal Lymph node enlargement (-) Symmetrical fusiformis, easily seen ribs(+),retraction (-)
HR: 100x/1, reguler, sigh (-). RR: 30 x/1, regular, crackles (-/-) Abdomen Soepel,Peristaltic (+) normal. Liver/Spleen/Renal : undeterminate Extremities Pulse 100 x/1, regular, adequate pressure and volume, warm acral, CRT < 3, hypotropy muscle (+), baggy pants (+) A : Marasmus type malnutrition + susp.Down syndrome P: Management - Folat acid 1 x 1 mg - Multivitamin without Fe 1 x 1cth - Cotrimoxazole syr 1x1 cth - Diet F100 65cc/3 hours/ NGT with mineral mix 1,3cc Plan: -Blood culture -Thorax photo
August, 24th 2013 (eighth day) S : Vomiting (-), Diarrhea (-)
29
O : Sens: Compos Mentis, Temp: 37oC, Body weight : 5,2 kg Head Old man face(+),Dismorfic face (+) Eye :light reflexes (+/+),Isochoric pupil, pale conjunctiva palpebra inferior Thorax (-),Ear = Normal, Nose= nasal canula O2 (+), NGT (+), Mouth = Normal Symmetrical fusiformis, easily seen ribs(+),retraction(-)
HR: 102x/1, reguler, sigh (-). RR: 24 x/1, regular, crackles (-/-) Abdomen Soepel, Peristaltic (+) normal.Liver/Spleen/Renal: undeterminate Extremities Pulse 102 x/1, regular, adequate pressure and volume, warm acral, CRT < 3, hypotropy muscle (+), baggy pants (+) A : Marasmus type malnutrition + susp.Down syndrome P: Management - Folat acid 1 x 1 mg - Cotrimoxazole syr 1x1 cth - Multivitamin without Fe 1x1 cth - Cotrimoxazole syr 1x1 cth - Diet F100 65cc /3hrs/ NGT with mineral mix 1,3 cc Plan :-
August, 25th 2013 (ninth day) S : Vomiting (-), Diarrhea (-)
30
O : Sens: CM, Temp: 37oC, Body weight : 5,3 kg Head Old man face(+),Dismortic face (+) Eye :light reflexes (+/+),Isochoric pupil, pale conjunctiva palpebra inferior Thorax (-),Ear = Normal, Nose= nasal canula O2 (+), NGT (+), Mouth = Normal Symmetrical fusiform, , easily seen ribs(+) ,retraction (-)
HR : 104 x/1, reguler, sigh (-),RR : 24 x/1, regular,Crackles (-/-) Abdomen Soepel,Peristaltic (+) normal. Liver/Spleen/Renal: undeterminate Extremities Pulse 104 x1, regular, adequate pressure and volume, warm acral, CRT < 3, hypotropy muscle (+), baggy pants (+) A : Marasmus type malnutrition + susp.Down syndrome P:management - Multivitamin without Fe 1x1 cth - Folat acid 1x1mg - Cotrimoxazole syr 1x1 cth - Diet F100 100cc /3hrs/ NGT with mineral mix 2 cc
Plan:-
August, 26th 2013 (tenth day) S : Vomiting (-), Diarrhea (-)
31
O : Sens: Compos Mentis, Temp: 37oC, Body weight : 5,3 kg Head Old man face(+),Dismortic face (+) Eye :light reflexes (+/+),Isochoric pupil, pale conjunctiva palpebra inferior Thorax (-),Ear = Normal, Nose= NGT (+), Mouth = Normal Symmetrical fusiform, easily seen ribs(+),retraction (-)
HR : 102 x/1,reguler,sigh (-),RR : 24 x/1, reguler. Crackles (-/-) Abdomen Soepel Peristaltic (+) normal. Liver/Spleen/Renal: undeterminate Extremities Pulse 102 x/1, regular, adequate pressure and volume, warm acral, CRT < 3, hypotropy muscle (+), baggy pants (+) A : Marasmus type malnutrition + susp.Down syndrome P:Management - Multivitamin without Fe 1x1 cth - Folat acid 1 x 1 mg - Diet F100 100cc/3hours/NGT with mineral mix 2cc
Plan:-
August, 27th 2013 (eleventh day) S : Vomiting (-), Diarrhea (-)
32
O : Sens: Compos Mentis, Temp: 37oC, Body weight : 5,3kg Head Old man face(+),Dismorfic face (+) Eye :light reflexes (+/+),Isochoric pupil, pale conjunctiva palpebra inferior Thorax (-),Ear = Normal, Nose= NGT (+), Mouth = Normal Symmetrical fusiform, easily seen ribs(+),retraction (-)
HR :100 x/1, reguler,sigh (-). RR : 24 x/1, reguler. Crackles (-/-) Abdomen Soepel Peristaltic (+) normal. Liver/Spleen/Renal: undeterminate Extremities Pulse 100 x/1, regular, adequate pressure and volume, warm acral, CRT < 3, hypotropy muscle (+), baggy pants (+) A : Marasmus type malnutrition + susp.Down syndrome P : Management - Multivitamin without Fe 1x1 cth - Folat acid 1 x 1 mg - Diet F100 100cc/3hours/NGT with mineral mix 2cc Plan :-
August, 28th 2013 (twelveth day) S : Vomiting (-), Diarrhea (-)
33
O : Sens: Compos Mentis, Temp: 37oC, Body weight : 5,3 kg Head Old man face(+),Dismorfic face (+) Eye :light reflexes (+/+),Isochoric pupil, pale conjunctiva palpebra inferior Thorax (-),Ear = Normal, Nose= nasal canula O2 (+), NGT (+), Mouth = Normal Symmetrical fusiform, easily seen ribs(+),retraction (-)
HR : 100 x/1, reguler,sigh (-).RR : 24 x/1, reguler. Crackles (-/-) Abdomen Soepel Peristaltic (+) normal. Liver/Spleen/Renal: undeterminate Extremities Pulse 100 x/1, regular, adequate pressure and volume, warm acral, CRT < 3, hypotropy muscle (+), baggy pants (+) A : Marasmus type malnutrition + susp.Down syndrome P : Management - Multivitamin without Fe 1x1 cth - Folat acid 1 x 1 mg - Diet F100 100cc/3hours/NGT with mineral mix 2cc Plan :-
August, 29th 2013 (thirteenth day) S : Vomiting (-), Diarrhea (-)
34
O : Sens: Compos Mentis, Temp: 37oC, Body weight : 5,2 kg Head Old man face(+),Dismorfic face (+) Eye :light reflexes (+/+),Isochoric pupil, pale conjunctiva palpebra inferior Thorax (-),Ear = Normal, Nose= NGT (+), Mouth = Normal Symmetrical fusiform, easily seen ribs(+) , retraction (-).
HR : 102 x/1, reguler, sigh (-). RR : 24 x/1, reguler. Crackles (-/-) Abdomen Soepel Peristaltic (+) normal. Liver/Spleen/Renal: undeterminate Extremities Pulse 102 x/1, regular, adequate pressure and volume, warm acral, CRT < 3, hypotropy muscle (+), baggy pants (+) A : Marasmus type malnutrition + susp.Down syndrome P : Management - Multivitamin without Fe 1x1 cth - Folat acid 1 x 1 mg - Diet F100 100cc/3hours/NGT with mineral mix 2cc Plan :-
August, 30th 2013(fourteenth day) S : Vomiting (-), Diarrhea (-) O : Sens: Compos Mentis, Temp: 37oC, Body weight : 5,3kg
35
Head
Old man face(+),Dismorfic face (+) Eye :light reflexes (+/+),Isochoric pupil, pale conjunctiva palpebra inferior (-),Ear = Normal, Nose= NGT (+), Mouth = Normal Symmetrical fusiform, easily seen ribs(+) , retraction (-)
Thorax
HR : 102 x/1, reguler, sigh (-). RR : 24 x/1, reguler. Crackles (-/-) Abdomen Soepel Peristaltic (+) normal. Liver/Spleen/Renal: undeterminate Extremities Pulse 102 x/1, regular, adequate pressure and volume, warm acral, CRT < 3, hypotropy muscle (+), baggy pants (+) A : Marasmus type malnutrition + susp.Down syndrome P : Management - Multivitamin without Fe 1x1 cth - Folat acid 1 x 1 mg - Diet F100 100cc/3hours/NGT with mineral mix 2cc Plan :-
36
CHAPTER IV DISCUSSION AND SUMMARY Malnutrition essentially means bad nourishment. It concerns not enough as well as too much food, the wrong types of food, and the body's response to a wide range of infections that result in malabsorption of nutrients or the inability to use nutrients properly to maintain health. The clinical manifestation are extreme wasting, old-man face, irritable, subcutaneous fat loss, baggy pant. Down syndrome is a genetic disorder known as Trisomy, because individuals who get a Down syndrome have excess chromosome. They have three chromosome 21 where the normal only has two. REA, male, 1 year 3 month was admitted to RS Haji Adam Malik with the main complaint of vomiting, diarrhea, and fever. On physical examination the patient looks old man face in appereance, dismorfik face, easily seen ribs (+) , hypotropy muscle (+), subcutan lipid decreasing (+) and baggy pants (+), flat nose, smooth and loose skin, thick lips, on the pinkie finger looks short and bent inward, and the growth of the teeth are very disturbed. Laboratory finding shows hyperglicemia, shows leucosytosis, and hyponatremia. Now this patient can only prone itself, babbling, imitating the words, smiling, and looking at his hands.He was diagnosed with marasmus type malnutrition plus suspect down syndrome, and is managed with Folat acid 1x1 mg, Multivitamin without Fe 1x1cth, cotrimoxazole syr 1x1 cth, Diet F100 100 cc/3hrs with mineral mix 2cc, Resomal 50 cc/x diarrhea.
37
REFERENCE 1. IDAI. 2009. Panduan Pelayanan Medik IDAI : Malnutrisi Energi dan Protein. Hal 183-184. 2. Susanto J.C., Mexitalia M., Nasar S.S., Malnutrisi Akut Berat dan Terapi Nutrisi Berbasis Komunitas dalam Buku Ajar Nutrisi Pediatrik dan Penyakit Metabolik Jilid I. 2011. Eds Sjarif D.R., Lestari E.D., Mexitalia M., Nasar S.S. Jakarta: Badan Penerbit IDAI. Hal 128-154. 3. World Health Organization (WHO). 1999. Management of Severe Malnutrition : manual for physicians and other senior health workers. Geneva : WHO. ISBN 92 4 154511 9 4. Davis, A. 2008. Children with Down Syndrome : Implications for Assessment and Intervention in the School. School Psychology Quarterly. Vol. 23 No. 2 (P) 271-281 5. World Health Organization (WHO). 2002. Training Course on management of severe malnutrition : 2. Principles of Care. Geneva : WHO. WHO/NHD/02/.4(P)2 6. World Health Organization (WHO). 2002. Training Course on management of severe malnutrition : 3. Initial Mangement. Geneva : WHO. WHO/NHD/02/.4(P)3 7. World Health Organization (WHO). 2002. Training Course on management of severe malnutrition : 4. Feeding. Geneva : WHO. WHO/NHD/02/.4(P)4 8. Departemen Kesehatan Republik Indonesia. 2011. Petunjuk teknis tata laksana anak gizi buruk : buku I. Jakarta : Depkes. 9. Departemen Kesehatan Republik Indonesia. 2011. Petunjuk teknis tata laksana anak gizi buruk : buku II. Jakarta : Depkes. 10. Kementrian Kesehatan Republik Indonesia. 2011. Pedoman Pelayanan Anak Gizi Buruk. Jakarta : Departemen Kesehatan.
38
11. Bagian Ilmu Kesehatan Anak FKUI. 2007. Kelainan Kromosom : Buku I. Jakarta : FKUI. Hal 217-219
12. RSCM. 2007. Panduan Pelayanan medis RSCM : Sindrom Down. Hal
347-350
Appendix A (F-75) Appendix B (F-100)
39
40
Anda mungkin juga menyukai
- MarasmusDokumen43 halamanMarasmusCindy PutrianiBelum ada peringkat
- A Guide to Diabetes: Symptoms; Causes; Treatment; PreventionDari EverandA Guide to Diabetes: Symptoms; Causes; Treatment; PreventionBelum ada peringkat
- Conquering Diabetes: Fenugreek Success in Regulating Blood Sugar LevelsDari EverandConquering Diabetes: Fenugreek Success in Regulating Blood Sugar LevelsBelum ada peringkat
- Discover Natural -Alternative Therapies for Managing Type 2 DiabetesDari EverandDiscover Natural -Alternative Therapies for Managing Type 2 DiabetesBelum ada peringkat
- Lapkas Anak (Prof Dr. Hj. Bidasari)Dokumen74 halamanLapkas Anak (Prof Dr. Hj. Bidasari)Maral Bimanti Febrilina100% (1)
- ADA Type 2 Diabetes in ChildrensDokumen10 halamanADA Type 2 Diabetes in ChildrensCho Maharani Rijhigo BaeBelum ada peringkat
- If DIABETESDokumen22 halamanIf DIABETESVictor Jesus Victorsg Siguas GarciaBelum ada peringkat
- User's Guide to Preventing & Reversing Diabetes NaturallyDari EverandUser's Guide to Preventing & Reversing Diabetes NaturallyBelum ada peringkat
- Diabetes Diet: How to improve, manage, and prevent diabetes with the help of food!Dari EverandDiabetes Diet: How to improve, manage, and prevent diabetes with the help of food!Belum ada peringkat
- Eating ProblemsDokumen4 halamanEating ProblemsximerodriguezcBelum ada peringkat
- Rakel: Textbook of Family Medicine, 7th Ed.Dokumen4 halamanRakel: Textbook of Family Medicine, 7th Ed.Nicolás Rojas MontenegroBelum ada peringkat
- Eating ProblemsDokumen4 halamanEating ProblemsNicolás Rojas MontenegroBelum ada peringkat
- How to Manage Diabetes and Cure?: Dr. Alan's Step By Step Guide for Diabetes Management Including General Tips, Diet Plan, Exercise Routine and Much More!Dari EverandHow to Manage Diabetes and Cure?: Dr. Alan's Step By Step Guide for Diabetes Management Including General Tips, Diet Plan, Exercise Routine and Much More!Belum ada peringkat
- Diabetes Ready Reference for Nurse Practitioners: Clear, Concise Guidelines for Effective Patient CareDari EverandDiabetes Ready Reference for Nurse Practitioners: Clear, Concise Guidelines for Effective Patient CareBelum ada peringkat
- Type 2 Diabetes Cookbook for Beginners: Mastering Balanced, Low-Sugar Eating for Enhanced Well-being and Effective Diabetes Control [V EDITION]Dari EverandType 2 Diabetes Cookbook for Beginners: Mastering Balanced, Low-Sugar Eating for Enhanced Well-being and Effective Diabetes Control [V EDITION]Penilaian: 5 dari 5 bintang5/5 (7)
- Metabolic Syndrome Program: How to Lose Weight, Beat Heart Disease, Stop Insulin Resistance and MoreDari EverandMetabolic Syndrome Program: How to Lose Weight, Beat Heart Disease, Stop Insulin Resistance and MorePenilaian: 4.5 dari 5 bintang4.5/5 (2)
- Diabetes Mellitus And Its Complications, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandDiabetes Mellitus And Its Complications, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Assessment and Management of Mild, Moderate, and Severe Dehydration in ChildrenDokumen1 halamanAssessment and Management of Mild, Moderate, and Severe Dehydration in ChildrenMaria Jessica DumdumBelum ada peringkat
- Biology Investigatory Project: Topic - DiabetesDokumen19 halamanBiology Investigatory Project: Topic - Diabetesaditya gollakota84% (38)
- Natural Remedies To Pre-Diabetes: Reverse Type 2 Diabetes Naturally in 90 DaysDari EverandNatural Remedies To Pre-Diabetes: Reverse Type 2 Diabetes Naturally in 90 DaysBelum ada peringkat
- Hypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionDari EverandHypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionBelum ada peringkat
- Food Addiction Denial: False Information and Irrational ThinkingDari EverandFood Addiction Denial: False Information and Irrational ThinkingBelum ada peringkat
- A Project Proposal On Case Study and Management of A Type 1 Diabetes Mellitus ClientDokumen6 halamanA Project Proposal On Case Study and Management of A Type 1 Diabetes Mellitus ClientMichael Kivumbi100% (3)
- Management of The Severely Malnourished Child Perspective FRDokumen6 halamanManagement of The Severely Malnourished Child Perspective FRAshley HumphreyBelum ada peringkat
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesDari EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesPenilaian: 4 dari 5 bintang4/5 (2)
- Diabetes in Children: Student Name Eslam Ashraf Abo El Ftoth Under Supervision: D/ Eman ElsayedDokumen14 halamanDiabetes in Children: Student Name Eslam Ashraf Abo El Ftoth Under Supervision: D/ Eman ElsayedEslam ShamndyBelum ada peringkat
- Diabetes Chapter 1 IntroductionDokumen23 halamanDiabetes Chapter 1 IntroductionHannah CaldinoBelum ada peringkat
- Overview of Diabetes MellitusDokumen7 halamanOverview of Diabetes MellitusIrene InsoBelum ada peringkat
- Eating DisorderDokumen26 halamanEating Disordernoot_onBelum ada peringkat
- Bio Final Investigatory 3334Dokumen28 halamanBio Final Investigatory 3334nokiwiBelum ada peringkat
- Diabetes EducationDokumen5 halamanDiabetes EducationSubramaniam RamanBelum ada peringkat
- Diabetes 1Dokumen67 halamanDiabetes 1Manny HermosaBelum ada peringkat
- Pediatric Type 1 Diabetes MellitusDokumen25 halamanPediatric Type 1 Diabetes MellitusmuhammadferhatBelum ada peringkat
- The Diabetes Code Cookbook: Delicious, Healthy, Low-Carb Recipes to Manage Your Insulin and Prevent and Reverse Type 2 DiabetesDari EverandThe Diabetes Code Cookbook: Delicious, Healthy, Low-Carb Recipes to Manage Your Insulin and Prevent and Reverse Type 2 DiabetesPenilaian: 1 dari 5 bintang1/5 (1)
- Jurnal Nutrisi 4Dokumen16 halamanJurnal Nutrisi 4agung suprasthaBelum ada peringkat
- Spatial Distribution of Type 2 Diabetes and its Geographical PatternsDokumen43 halamanSpatial Distribution of Type 2 Diabetes and its Geographical PatternsHamza FarooqBelum ada peringkat
- Diabetic Ketoacidosis in Toddler With A Diaper RashDokumen4 halamanDiabetic Ketoacidosis in Toddler With A Diaper RashKarl Angelo MontanoBelum ada peringkat
- Praposal DM-1Dokumen117 halamanPraposal DM-1sanjay sabdeBelum ada peringkat
- Bio Project FinalisedDokumen24 halamanBio Project FinalisedLakshmi SenthilkumarBelum ada peringkat
- Smoothies for Diabetics: Reverse Diabetes and Lower Blood Sugar with 36 Quick & Easy Delicious Diabetic Smoothie RecipesDari EverandSmoothies for Diabetics: Reverse Diabetes and Lower Blood Sugar with 36 Quick & Easy Delicious Diabetic Smoothie RecipesPenilaian: 5 dari 5 bintang5/5 (2)
- DM Final PDFDokumen15 halamanDM Final PDFgiftyBelum ada peringkat
- Guideline Screening and Treatment of Malnutrition English July 2012Dokumen30 halamanGuideline Screening and Treatment of Malnutrition English July 2012Putri WibisonoBelum ada peringkat
- 12 Nursing Managment of Childern With Endocarine Disorders 2nd SemesterDokumen27 halaman12 Nursing Managment of Childern With Endocarine Disorders 2nd SemesterFaisal M.AlruwailiBelum ada peringkat
- Immunity in the Midst of Chronic Kidney Disease:A Detailed Guide for Healthcare PractitionersDari EverandImmunity in the Midst of Chronic Kidney Disease:A Detailed Guide for Healthcare PractitionersBelum ada peringkat
- DMDokumen9 halamanDMMiftahul JannahBelum ada peringkat
- Rhinosinusitis Slides 060509Dokumen36 halamanRhinosinusitis Slides 060509KURBULDKBelum ada peringkat
- Reading CT Scan of Human BrainDokumen12 halamanReading CT Scan of Human BrainSumit RoyBelum ada peringkat
- Rash DecisionsDokumen40 halamanRash DecisionsKURBULDKBelum ada peringkat
- Manual/mechanical Activities:: Never Most of The TimeDokumen1 halamanManual/mechanical Activities:: Never Most of The TimeKURBULDKBelum ada peringkat
- Medical GeneticsDokumen12 halamanMedical GeneticsIsmail LubisBelum ada peringkat
- Type and Medical Specialities by Charles MartinDokumen7 halamanType and Medical Specialities by Charles MartinKURBULDKBelum ada peringkat
- Kappa KlarDokumen72 halamanKappa KlarKURBULDKBelum ada peringkat
- Path CH SinsDokumen38 halamanPath CH SinsKURBULDKBelum ada peringkat
- Medical OncologyDokumen12 halamanMedical OncologyKURBULDKBelum ada peringkat
- 6 N MalnutritionDokumen19 halaman6 N MalnutritionSunsong31Belum ada peringkat
- The Secret Doctrine by H. P. BlavatskyDokumen1.477 halamanThe Secret Doctrine by H. P. BlavatskyALDO VILLAMIL100% (28)
- L 3diagnostic UltrasonographyDokumen62 halamanL 3diagnostic UltrasonographyKURBULDKBelum ada peringkat
- Measles, Mumps and RubellaDokumen45 halamanMeasles, Mumps and RubellaKURBULDKBelum ada peringkat
- Stenosis HPI - PMR ClinicsDokumen11 halamanStenosis HPI - PMR ClinicsKURBULDKBelum ada peringkat
- G06 FX Classification JTG Rev 2-3-10Dokumen50 halamanG06 FX Classification JTG Rev 2-3-10KURBULDKBelum ada peringkat
- Why Spiritual Intelligence Is Essential To Mature Leadership Spiritual Intelligence WigglesworthDokumen17 halamanWhy Spiritual Intelligence Is Essential To Mature Leadership Spiritual Intelligence WigglesworthKURBULDKBelum ada peringkat
- The PSX-1,2,3,4: SeriesDokumen10 halamanThe PSX-1,2,3,4: SeriesKURBULDKBelum ada peringkat
- 6 N MalnutritionDokumen19 halaman6 N MalnutritionSunsong31Belum ada peringkat
- Medical GeneticsDokumen12 halamanMedical GeneticsIsmail LubisBelum ada peringkat
- Lumbar SpondylosisDokumen59 halamanLumbar SpondylosisKURBULDKBelum ada peringkat
- Paranasal Sinus 2002 01 SlidesDokumen49 halamanParanasal Sinus 2002 01 SlidesLusia NataliaBelum ada peringkat
- Path CH SinsDokumen38 halamanPath CH SinsKURBULDKBelum ada peringkat
- Anxiety Disorders1Dokumen12 halamanAnxiety Disorders1KURBULDKBelum ada peringkat
- Epos 2007Dokumen137 halamanEpos 2007KURBULDKBelum ada peringkat
- Mental BondageDokumen424 halamanMental BondageRedza92% (12)
- INTPDokumen5 halamanINTPIsmail LubisBelum ada peringkat
- How Islamic Are Islamic CountriesDokumen40 halamanHow Islamic Are Islamic Countriesخير الأنام الحبشىBelum ada peringkat
- The PSX-1,2,3,4: SeriesDokumen10 halamanThe PSX-1,2,3,4: SeriesKURBULDKBelum ada peringkat
- 05 Pulp, Periapical, OsteomyelitisDokumen12 halaman05 Pulp, Periapical, OsteomyelitisKurbulBelum ada peringkat
- Family ApgarDokumen6 halamanFamily ApgarunjyilBelum ada peringkat
- DR-M260 User Manual ENDokumen87 halamanDR-M260 User Manual ENMasa NourBelum ada peringkat
- Ultrasonic Weld Examination ProcedureDokumen16 halamanUltrasonic Weld Examination ProcedureramalingamBelum ada peringkat
- FST Handbook 2014-Final Copy 1 PDFDokumen382 halamanFST Handbook 2014-Final Copy 1 PDFDelvon DownerBelum ada peringkat
- Casio AP-80R Service ManualDokumen41 halamanCasio AP-80R Service ManualEngkiong Go100% (1)
- Acuity Assessment in Obstetrical TriageDokumen9 halamanAcuity Assessment in Obstetrical TriageFikriBelum ada peringkat
- A Study On Customer Satisfaction Towards Honda Bikes in CoimbatoreDokumen43 halamanA Study On Customer Satisfaction Towards Honda Bikes in Coimbatorenkputhoor62% (13)
- Gotham City: A Study into the Darkness Reveals Dangers WithinDokumen13 halamanGotham City: A Study into the Darkness Reveals Dangers WithinajBelum ada peringkat
- Diia Specification: Dali Part 252 - Energy ReportingDokumen15 halamanDiia Specification: Dali Part 252 - Energy Reportingtufta tuftaBelum ada peringkat
- LSUBL6432ADokumen4 halamanLSUBL6432ATotoxaHCBelum ada peringkat
- Detection and Attribution Methodologies Overview: Appendix CDokumen9 halamanDetection and Attribution Methodologies Overview: Appendix CDinesh GaikwadBelum ada peringkat
- Telco XPOL MIMO Industrial Class Solid Dish AntennaDokumen4 halamanTelco XPOL MIMO Industrial Class Solid Dish AntennaOmar PerezBelum ada peringkat
- 2 - Soil-Only Landfill CoversDokumen13 halaman2 - Soil-Only Landfill Covers齐左Belum ada peringkat
- Flexibility Personal ProjectDokumen34 halamanFlexibility Personal Projectapi-267428952100% (1)
- Flood FillDokumen1 halamanFlood FillshubhamBelum ada peringkat
- Are Hypomineralized Primary Molars and Canines Associated With Molar-Incisor HypomineralizationDokumen5 halamanAre Hypomineralized Primary Molars and Canines Associated With Molar-Incisor HypomineralizationDr Chevyndra100% (1)
- Handouts For TLG 3 1Dokumen5 halamanHandouts For TLG 3 1Daniela CapisnonBelum ada peringkat
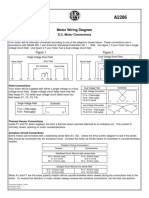
- Motor Wiring Diagram: D.C. Motor ConnectionsDokumen1 halamanMotor Wiring Diagram: D.C. Motor Connectionsczds6594Belum ada peringkat
- Introduction To Finite Element Methods (2001) (En) (489s)Dokumen489 halamanIntroduction To Finite Element Methods (2001) (En) (489s)green77parkBelum ada peringkat
- Smart Note Taker Saves Time With Air WritingDokumen17 halamanSmart Note Taker Saves Time With Air WritingNagarjuna LokkuBelum ada peringkat
- Home Brewing Log Sheet PDFDokumen2 halamanHome Brewing Log Sheet PDFStefanita0% (1)
- EP - EngineDokumen4 halamanEP - EngineAkhmad HasimBelum ada peringkat
- Xii Neet Chemistry Mcqs PDFDokumen30 halamanXii Neet Chemistry Mcqs PDFMarcus Rashford100% (3)
- Artifact and Thingamy by David MitchellDokumen8 halamanArtifact and Thingamy by David MitchellPedro PriorBelum ada peringkat
- ASA 2018 Catalog WebDokumen48 halamanASA 2018 Catalog WebglmedinaBelum ada peringkat
- Effective Time ManagementDokumen61 halamanEffective Time ManagementTafadzwa94% (16)
- Flowing Gas Material BalanceDokumen4 halamanFlowing Gas Material BalanceVladimir PriescuBelum ada peringkat
- Lincoln Pulse On PulseDokumen4 halamanLincoln Pulse On PulseEdison MalacaraBelum ada peringkat
- 24.postpartum Period-Physiological Changes in The MotherDokumen16 halaman24.postpartum Period-Physiological Changes in The MotherHem KumariBelum ada peringkat
- JK Paper Q4FY11 Earnings Call TranscriptDokumen10 halamanJK Paper Q4FY11 Earnings Call TranscriptkallllllooooBelum ada peringkat
- Lec9-Rock Cutting ToolsDokumen35 halamanLec9-Rock Cutting ToolsAmraha NoorBelum ada peringkat



















![Type 2 Diabetes Cookbook for Beginners: Mastering Balanced, Low-Sugar Eating for Enhanced Well-being and Effective Diabetes Control [V EDITION]](https://imgv2-1-f.scribdassets.com/img/word_document/616633879/149x198/173640cf06/1710278044?v=1)